Abstract
Purpose
Smoking cessation in patients with diagnosed lung cancer has positive effects on cancer therapy and overall prognosis. Despite this, knowledge on smoking cessation in lung cancer patients is sparse.
Methods
This is an observational single centre, 12-week, prospective, single-arm trial at a tertiary lung cancer centre. Responsive patients were enrolled following confirmed lung cancer diagnosis. Smoking cessation intervention included counselling as well as pharmacotherapy. The primary endpoint was the point prevalence abstinence rate at week 12 based on biochemical verification. Secondary endpoints were the abstinence rate at week 26, quality of life and side effects.
Results
80 patients were enrolled. Mean age was 62.6 ± 7.9 years. Most patients (63%) were treated with chemotherapy or radiochemotherapy. 39 patients used nicotine replacement therapy, 35 varenicline whereas six patients did not use pharmacotherapy. During the study period 13 patients died. Data were available in 72 patients after 12 weeks and 57 patients at week 24. Point prevalence abstinence rates were 37.5% (95% CI 26.4–49.7%) at week 12 and 32.8% (95% CI 21.8–45.4%) at week 26, respectively. Quality of life and side effects were not significantly affected by pharmacotherapy.
Conclusion
In conclusion, our results suggest that smoking cessation is feasible in patients with newly diagnosed lung cancer. The observed abstinence rate is comparable to other patient cohorts. Furthermore, pharmacotherapy in addition to cancer therapy was safe and did not show novel side effects in these seriously ill patients. Thus, smoking cessation should be an integral part of lung cancer treatment.
Trial registration The study was conducted in accordance with good clinical practice standards (GCP) and approved by the local ethics committee (16/3/14), the European PAS registry (EUPAS8748) and the German BfArM (NIS-Studien-Nr. 5508). All patients provided written informed consent before study enrollment.
Similar content being viewed by others
Background
Tobacco smoking increases mutational burden and quitting fosters replenishment of the bronchial epithelium with cells that have avoided tobacco mutagenesis [1]. Thus, not surprisingly, smoking cessation is not only paramount in the prevention but also in the treatment of lung cancer. Indeed, quitting smoking clearly improves lung cancer survival. Recent studies show that smoking cessation after the diagnosis of lung cancer had an influence on overall prognosis [2, 3], effectiveness of chemotherapy [4] and on morbidity after curative surgery [5, 6]. Smoking cessation has therefore become a part of current treatment guidelines for lung cancer [7, 8]. The majority of lung cancer patients is willing to stop smoking. Due to their long smoking history and high nicotine dependence, the ability to reach this aim is low. Recent data show a still high smoking rate in smoking-related cancer survivors [7].
Concerning hospitalized patients mainly with cardiovascular disease a meta-analysis demonstrated that high-intensity behavioral interventions (preferable with pharmacologic therapy) beginning during a hospital stay promote smoking cessation [9, 10].
Despite the above mentioned, clinicians often hesitate to actively encourage patients to quit smoking once lung cancer is diagnosed. Reasons for this might be ignorance of the clinical benefits and medical options for smoking cessation, lack of time for smoking cessation counselling, and fear of side effects of available drugs for smoking cessation during cancer treatment [11].
Until now, data on smoking cessation in lung cancer patients are sparse. In a metaanalysis there was insufficient evidence to determine whether smoking cessation interventions are effective for people with lung cancer [8]. In a recent large retrospective study investigating patients with current cancer an intensive cessation treatment resulted in an overall self reported abstinence rate of 45% at 3 months. The subgroup of patients with lung cancer demonstrated similar results as compared to the overall group [12]. To investigate whether smoking cessation could be implemented in the daily routine of a lung cancer centre we conducted this single arm, uncontrolled feasibility study. The primary endpoint was the point prevalence abstinence rate at week 12 based on biochemical verification. Quality of life and side effects were also prospectively evaluated.
Methods
Study design and outcome
This is an observational, single center, 12-week, prospective, single-arm trial of a smoking cessation intervention performed at a large university lung cancer centre. The primary endpoint was the point abstinence rate at week 12 based on biochemical verification. Secondary endpoints were the point abstinence rate at week 26, quality of life and abstinence phenomena as evaluated by questionnaire (see study procedures). Patients were enrolled after confirmed lung cancer diagnosis. Every patient with a new diagnosis of lung cancer was screened, unless the study team was not available.
Inclusion criteria were as follows:
-
Newly diagnosed lung cancer stages I–IV within 14 days preceding study enrollment
-
Current smoking or smoking up to 4 weeks before study enrollment
-
Age ≥ 18 years
-
Providing written informed consent
Exclusion criterion was severe comorbidity, making study participation unlikely.
The study was conducted in accordance with good clinical practice standards (GCP) and approved by the local ethics committee (Ethikkommission der Universitätsmedizin Göttingen, 16/3/14), the European PAS registry (EUPAS8748) and the Bundesinstitut für Arzneimittel und Medizinprodukte (BfArM) (NIS-Studien-Nr. 5508) before enrolment. All patients provided written informed consent before study related procedures.
Study procedures
After enrollment, each patient received smoking cessation counselling by trained physicians or a social worker. Counselling was based on the technique of motivational interviewing. It also included counselling on pharmacotherapy. Following counselling, patients could decide whether they wanted to use pharmaceutical support or not. Pharmacotherapy offered was nicotine replacement therapy in form of patches and/or nicotine gums/lozenges according to the daily number of cigarettes smoked or varenicline for 12 weeks each. Patients received verbal and written instructions on how to use pharmacotherapy.
The intervention was conducted in accordance with the German procedure code (OPS) for in hospital smoking cessation (OPS 9-501 “Multimodale stationäre Behandlung zur Tabakentwöhnung” [13]. However, the duration of the intervention was at least 30 min and thus shorter as stated in the OPS. Physicians and the social worker were trained and certified according to the curriculum of the Bundesärztekammer. This curriculum comprises 28 h of structured learning in small groups and is constructed to address the four main active ingredients according to behavior change technique taxonomy [14].
At study entry, carbon monoxide (CO)-Concentration in exhaled air was measured using a Senko® BMC 2000 device (SENKO Co., Ltd.). CO-Concentration in exhaled air of more than 8 ppm was considered as current smoking.
Cigarette Dependence was measured by the Fagerström Test for Cigarette Dependence [15,16,17]. Quality of life was assessed at the beginning and week 12 by the EORTC QLQ C30 and [18] the lung-specific EORTC QLQ LC13 questionnaire [19] as well as the EQ VAS [18]. In addition, we assessed psychological distress by the Hospital Anxiety and Depression Scale (HADS) and abstinence phenomena by the latest version of the Mood and physical symptoms scale (MPSS) [20, 21].
After 6 weeks, patients were asked about their smoking status, withdrawal symptoms, the use of the medication (if chosen) and any side effects. After 12 weeks, they were also asked about quality of life and the CO concentration in exhaled air was measured again. After 26 weeks CO concentration was measured. Study flow and investigations are shown in Fig. 1.
Statistical analysis
Baseline characteristics of analyzed patients are reported by summary statistics such as mean (standard deviation) for continuous data and frequencies (percentages) for categorical data overall and by intervention. Patients who withdrew their consent or were lost to follow up were counted as smokers according to the intention to treat protocol. Patients who died during the study period were censored after their last documented visit.
Tobacco abstinence was defined as CO concentration in exhaled air below or equal to 8 ppm. Missing values were considered as non-abstinent. The primary endpoint tobacco abstinence after 12 weeks was estimated with 95% Clopper–Pearson confidence intervals. Differences between the treatment groups, albeit not randomized, were tested using the t-test.
Since this was not a controlled efficacy study no formal power calculation was performed. Nevertheless, we planned that 80 patients could be enrolled in 2–3 years based on previous experience [22, 23]. With a 10% drop out rate 72 patients would be available for calculation of tobacco abstinence.
The funding source had no influence on the study design, the data analysis and interpretation of the study.
Results
Study enrollment ran from March 2015 to June 2018. Baseline characteristics of the study population are shown in Table 1. Of 80 patients enrolled, 39 decided for nicotine replacement therapy, 35 for varenicline whereas six patients chose no pharmacotherapy.
Of the 80 patients, 66% had non-small cell lung cancer and 34% small cell lung cancer. During the study period 13 patients died (nine due to worsening of lung cancer, 1 due to myocardial infarction, 1 due to renal failure, 1 due to stroke, one patient committed suicide after receiving the message of cancer progress). Four patients were lost to follow up and 7 patients withdrew their consent. One patient was diagnosed as non-small cell lung cancer and received nicotine replacement therapy. A few days following study enrollment, the final diagnosis was urothelial cancer and the patient was subsequently excluded. Some patients responded to a call for visit 4 but not for visit 3. Thus, data are available of 72 patients after 12 weeks and of 67 patients at week 26.
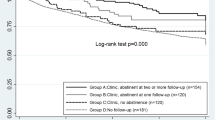
Overall verified tobacco point abstinence rate for patients alive was 37.5% (95% CI 26.4–49.7%) at week 12 and 32.8% (95% CI 21.8–45.4%) at week 26, respectively. Point abstinence rates according to medical treatment are shown in Table 2.
Withdrawal symptoms evaluated by MPSS-Scores of the treatment groups are shown in Fig. 2. There was no increase in MPSS-Scores during the treatment period. There was a significant difference in withdrawal symptoms between patients in the no medication group and patients in the NRT or varenicline group. Patients in the no medication group showed significantly fewer withdrawal symptoms than others right from the beginning up to week 12. There were no significant differences in abstinence phenomena between the NRT and varenicline group (for details see Tables 3, 4). Most patients of the no medication group had already stopped smoking within four weeks before study entry (5 out of 6 patients) and showed a low Fagerström score.
HADS scores for each treatment are shown in Fig. 3. There was no increase in HADS total score during the treatment period. There was a tendency to a difference in symptoms between patients in the no medication group and patients in the NRT or varenicline group at week 6 and week 12 (Additional file 1: HADS).
There was no group difference in EQ VAS, EORTC QLQ C30 and EORTC LC13 subscales. For further details, see Additional file 2: EORTC.
Side effects
Each patient was asked at visit 2 (week 6) and visit 3 (week 12) if adverse events of medication occurred. Hospitalization due to lung cancer therapy or lung cancer therapy complications was not considered an adverse event as predefined in the study protocol.
Nicotine replacement therapy
Patients receiving nicotine replacement therapy were, amongst others, asked at visit 2 and 3 about skin irritation, flu-like symptoms and coughing due to the therapy. Furthermore, they were asked about neurological, cardiovascular and endocrinological symptoms. None of the 39 patients receiving nicotine replacement therapy reported any of these symptoms at visit 2 and visit 3, respectively.
One patient suffered a myocardial infarction four weeks after visit 3 and died of cardiogenic shock two days later. At that time, the patient had already stopped nicotine replacement therapy.
Varenicline
Patients who received varenicline were, amongst others, questioned about psychological effects such as abnormal dreams, insomnia, anxiety, and hallucinations. Furthermore, they were asked about gastrointestinal side effects such as nausea, vomiting, obstipation, and chest pain. Six patients reported nausea at week 6, 3 also reported vomiting. All these patients stopped varenicline without further symptoms. One patient switched to nicotine replacement therapy. Of note, all patients reporting nausea received chemotherapy or radiochemotherapy, respectively. When comparing EORTC QLQ C30 subscales nausea and vomiting as well as fatigue and insomnia, there was no difference at week 12 between treatment groups (Additional file 2: EORTC).
In one patient a transient ischemic attack led to a hospitalization after 10 days on varenicline. The patient showed a transient hemiparesis on the left side. Symptoms dissolved within hours. The patient previously has had a stroke. The same patient reported mild hallucinations after increasing varenicline dose to 1 mg twice daily. As the patient was further interested in pharmacological support, dosage was reduced but symptoms reoccurred, and the patient decided to switch to nicotine replacement therapy.
One patient receiving varenicline, who stopped the medication due to nausea after 4 weeks, suffered renal failure about 3 weeks later due to chemotherapy-associated diarrhea. The patient finally died due to renal failure.
One patient receiving varenicline died by suicide after receiving the message of progress of lung cancer. The patient was a hunter. He received only one package of varenicline, which was taken until 4 weeks before his dead. The patient never received a further package of varenicline. There was no suggestion that the medication was responsible for his decision to commit suicide.
Discussion
This prospective study evaluated a comprehensive smoking cessation program including pharmacotherapy in smokers with newly diagnosed lung cancer. Achieved smoking abstinence rate was 37.5% after 12 and 32.8% after 24 weeks and thus comparable to results in other patient groups or healthy subjects [15, 16, 24]. A recent unblinded study randomly assigned 303 patients with newly diagnosed cancer to an intensive treatment group, with 11 smoking cessation telephone counselling sessions coupled with 12 weeks of free cessation medication or to standard therapy [25]. The 7-day abstinence rates at 6-month were 35% in the intensive treatment versus 22% in the standard group. A study using only brief advice in cancer patients reported a biochemically validated quit rate at 6 months of 6% [26]. When comparing these and other studies, it should be kept in mind that comparison is difficult because of diversities in enrolled patients, assessment of abstinence and intensity of the cessation intervention.
There is only limited evidence on smoking cessation in lung cancer patients. Previous studies were retrospective [27] and included only a limited number of patients (15–49 patients) [9, 10, 28]. Importantly, side effects of pharmacotherapy were not systematically evaluated. Thus, a recent Cochrane review stated insufficient evidence for smoking cessation in patients with lung cancer mainly due to the limited number of patients with lung cancer included and the uncontrolled design [8].
Smoking abstinence was numerically higher in the varenicline group as compared to the nicotine replacement group, but this observational study was not designed to show differences between different forms of treatment. In persons trying to quit smoking varenicline is known to be more effective as compared to nicotine replacement therapy [16, 29].
Most of the patients chose pharmacotherapy following smoking cessation counselling. Only six patients decided against any medication. Among these, most patients had already stopped smoking within the 4 weeks before enrollment into the study and the score of the Fagerström-test was lower than in the other patients, indicating lesser nicotine addiction. Thus, our study revealed that intense cessation counselling during hospitalization for diagnosis and subsequent treatment of lung cancer leads to a high proportion of patients using pharmacotherapy as an aid for smoking cessation. In a prospective, representative German survey of over 10.000 smokers, cessation attempts only 7.6% used nicotine replacement therapy and 0.4% used varenicline [30]. A high proportion of patients using pharmacotherapy is important since this nearly doubles the success rate [31].
We included not only current smokers but also patients smoking up to 4 weeks before study enrollment. This was done because quitting just before the diagnosis of lung cancer is common [32], often due to acute lung cancer associated symptoms and may thus indicate a less favorable abstinence rate [33]. Accordingly, cessation intervention is endorsed in these patients [34].
Side effects
Side effects of medication are important when treating lung cancer patients with a high symptom burden and a limited prognosis. The side effects observed in the present study were keeping within the previously published data in persons trying to quit smoking. There were no solicited adverse events reported in patients using nicotine replacement therapy. Nausea while taking varenicline was reported by six patients. Of note, all of these patients received concurrent chemotherapy or radiochemotherapy, respectively. There was no difference in the subscale “nausea and vomiting” on the EORTC QLQ C30 questionnaire between the patients receiving varenicline or nicotine replacement therapy. Also, in these groups nausea and vomiting were associated with lung cancer therapy. Thus, the study revealed no novel side effects in the cohort of patients with life-limiting disease often undergoing systemic therapy including chemotherapy and immunotherapy. As the study included patients with all lung cancer stages, among them many patients with advanced disease, most patients who died did so due to progression of lung cancer. Accordingly, mortality was high during the study period.
Symptoms of nicotine withdrawal were lowest in patients who did not opt for additional pharmacological treatment. This might be explained by the low rate of current smokers in this group at study entry as discussed above. Correspondingly, the abstinence rate was highest in this group (60% of patients were abstinent at week 12). The significant difference of nicotine withdrawal symptoms at week 12 between patients receiving NRT or varenicline and patients without medication might also be explained by the disparity of the groups at baseline. The small number of patients in this group hampers interpretation of the data. There were no significant group differences for global health status, and cognitive as well as emotional functioning.
Limitations
A limitation of the present study is that not all smokers with a new diagnosis of lung cancer were included in the study since some patients were reluctant to participate and the study team was absent for distinct periods of time. Furthermore, the study is rather small and the lack of randomization precludes any formal comparison between the different pharmacologic treatments. Finally, qualitative data from patients and clinicians on their experiences might have helped to identify barriers. A strength of the study is the prospective evaluation of side effects and the real life setting in a tertiary lung cancer center.
Conclusion
Our results indicate that smoking cessation is feasible in patients with newly diagnosed lung cancer. The observed cessation rate is comparable to other patient cohorts or healthy subjects. Furthermore, pharmacotherapy using nicotine replacement therapy or varenicline in addition to cancer therapy was safe and did not show novel side effects in these seriously ill patients. Given the known positive effects of smoking cessation in lung cancer patients, smoking cessation should be integral part of lung cancer treatment [35].
Availability of data and materials
The datasets used and analysed during the current study is available from the corresponding author on reasonable request.
Abbreviations
- CO:
-
Carbon monoxide
- BfArM:
-
Bundesinstitut für Arzneimittel und Medizinprodukte
- EORTC QLQ:
-
European Organization Research Treatment Cancer—Quality of Life Questionnaire
- EQ VAS:
-
European Quality of Life—visual analog scale
- GCP:
-
Good clinical practice
- HADS:
-
Hospital Anxiety and Depression Scale
- MPSS:
-
Mood and Physical Symptoms Scale
- NM:
-
No medication
- NRT:
-
Nicotine replacement therapy
- STD:
-
Standard deviation
References
Yoshida K, Gowers KHC, Lee-Six H, Chandrasekharan DP, Coorens T, Maughan EF, et al. Tobacco smoking and somatic mutations in human bronchial epithelium. Nature. 2020;578(7794):266–72.
Dobson Amato KA, Hyland A, Reed R, Mahoney MC, Marshall J, Giovino G, et al. Tobacco cessation may improve survival lung cancer patients survival. J Thorac Oncol. 2015;10:1014–9.
Hanna N, Mulshine J, Wollins DS, Tyne C, Dresler C. Tobacco cessation and control a decade later: American society of clinical oncology policy statement update. J Clin Oncol. 2013;31:3147–57.
Parsons A, Daley A, Begh R, Aveyard P. Influence of smoking cessation after diagnosis of early stage lung cancer on prognosis: systematic review of observational studies with meta-analysis. BMJ. 2010;340:b5569.
Mason DP, Subramanian S, Nowicki ER, Grab JD, Murthy SC, Rice TW, et al. Impact of smoking cessation before resection of lung cancer: a Society of Thoracic Surgeons General Thoracic Surgery Database study. Ann Thorac Surg. 2009;88(2):362–70 (discussion 370-1).
Jiménez-Ruiz CA, Andreas S, Lewis KE, Tonnesen P, van Schayck CP, Hajek P, et al. Statement on smoking cessation in COPD and other pulmonary diseases and in smokers with comorbidities who find it difficult to quit. Eur Respir J. 2015;46(1):61–79.
Gritz ER, Talluri R, Fokom Domgue J, Tami-Maury I, Shete S. Smoking behaviors in survivors of smoking-related and non-smoking-related cancers. JAMA Netw Open. 2020;3(7):e209072.
Zeng L, Yu X, Yu T, Xiao J, Huang Y. Interventions for smoking cessation in people diagnosed with lung cancer. Cochrane Database Syst Rev. 2019;6:CD0011751.
Lai DT, Cahill K, Qin Y, Tang JL. Motivational interviewing for smoking cessation. Cochrane Database Syst Rev. 2010;(1):CD006936.
Rigotti NA, Clair C, Munafò MR, Stead LF. Interventions for smoking cessation in hospitalised patients. Cochrane Database Syst Rev. 2012;(5):CD001837.
Andreas S, Rittmeyer A, Hinterthaner M, Huber RM. Smoking cessation in lung cancer-achievable and effective. Dtsch Arztebl Int. 2013;110(43):719–24.
Cinciripini PM, Karam-Hage M, Kypriotakis G, Robinson JD, Rabius V, Beneventi D, et al. Association of a comprehensive smoking cessation program with smoking abstinence among patients with cancer. JAMA Netw Open. 2019;2(9):e1912251.
Andreas S, Jany B, Hering T, Rustler C, Grah C, Pfeifer M. OPS 9–501 Multimodale stationäre Behandlung zur Tabakentwöhnung. Pneumologie. 2018;72(2):103–5.
Michie S, Hyder N, Walia A, West R. Development of a taxonomy of behaviour change techniques used in individual behavioural support for smoking cessation. Addict Behav. 2011;36(4):315–9.
Tashkin DP, Rennard S, Hays JT, Ma W, Lawrence D, Lee TC. Effects of varenicline on smoking cessation in patients with mild to moderate COPD: a randomized controlled trial. Chest. 2011;139(3):591–9.
Anthenelli RM, Benowitz NL, West R, St Aubin L, McRae T, Lawrence D, et al. Neuropsychiatric safety and efficacy of varenicline, bupropion, and nicotine patch in smokers with and without psychiatric disorders (EAGLES): a double-blind, randomised, placebo-controlled clinical trial. Lancet. 2016;387(10037):2507–20.
Fagerström K. Determinants of tobacco use and renaming the FTND to the Fagerstrom test for cigarette dependence. Nicotine Tob Res. 2012;14(1):75–8.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–76.
Bergman B, Aaronson NK, Ahmedzai S, Kaasa S, Sullivan M. The EORTC QLQ-LC13: a modular supplement to the EORTC Core Quality of Life Questionnaire QLQ-C30 for use in lung cancer clinical trials EORTC Study Group on Quality of Life. Eur J Cancer. 1994;30(5):635–42.
West R, Hajek P, Stead L, Stapleton J. Outcome criteria in smoking cessation trials: proposal for a common standard. Addiction. 2005;100(3):299–303.
West, R. Mood and Physical Symptoms Scale (MPSS) Questionnaire. 2012 [cited 2021 19.08.]; Available from: https://www.ncsct.co.uk/usr/pub/Mood%20and%20physical%20symptoms%20scale%20(MPSS).pdf.
Schuette WH, Gröschel A, Sebastian M, Andreas S, Müller T, Schneller F, et al. A randomized phase II study of pemetrexed in combination with cisplatin or carboplatin as first-line therapy for patients with locally advanced or metastatic non-small-cell lung cancer. Clin Lung Cancer. 2013;14(3):215–23.
Rittmeyer A, Barlesi F, Waterkamp D, Park K, Ciardiello F, von Pawel J, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet. 2017;389(10066):255–65.
Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, et al. A Randomized Trial of E-Cigarettes versus Nicotine-Replacement Therapy. N Engl J Med. 2019;380(7):629–37.
Park ER, Perez GK, Regan S, Muzikansky A, Levy DE, Temel JS, et al. Effect of sustained smoking cessation counseling and provision of medication vs shorter-term counseling and medication advice on smoking abstinence in patients recently diagnosed with cancer: a randomized clinical trial. JAMA. 2020;324(14):1406–18.
Li WHC, Wang MP, Ho KY, Lam KKW, Cheung DYT, Cheung YTY, et al. Helping cancer patients quit smoking using brief advice based on risk communication: a randomized controlled trial. Sci Rep. 2018;8(1):2712.
Griebel B, Wewers ME, Baker CA. The effectiveness of a nurse-managed minimal smoking-cessation intervention among hospitalized patients with cancer. Oncol Nurs Forum. 1998;25(5):897–902.
Cahill K, Stead LF, Lancaster T. Nicotine receptor partial agonists for smoking cessation. Cochrane Database Syst Rev 2011; (2): CD006103.
Mills EJ, Wu P, Lockhart I, Thorlund K, Puhan M, Ebbert JO. Comparisons of high-dose and combination nicotine replacement therapy, varenicline, and bupropion for smoking cessation: a systematic review and multiple treatment meta-analysis. Ann Med. 2012;44(6):588–97.
Kotz D, Batra A, Kastaun S. Smoking cessation attempts and common strategies employed. Dtsch Arztebl Int. 2020;117(1–2):7–13.
Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Database Syst Rev 2013; (5): CD009329.
Ferketich AK, Niland JC, Mamet R, Zornosa C, D’Amico TA, Ettinger DS, et al. Smoking status and survival in the national comprehensive cancer network non-small cell lung cancer cohort. Cancer. 2013;119(4):847–53.
Sanderson Cox L, Patten CA, Ebbert JO, Drews AA, Croghan GA, Clark MM, et al. Tobacco use outcomes among patients with lung cancer treated for nicotine dependence. J Clin Oncol. 2002;20(16):3461–9.
Cox LS, Africano NL, Tercyak KP, Taylor KL. Nicotine dependence treatment for patients with cancer. Cancer. 2003;98(3):632–44.
Croyle RT, Morgan GD, Fiore MC. Addressing a core gap in cancer care—the NCI Moonshot Program to help oncology patients stop smoking. N Engl J Med. 2019;380(6):512–5.
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. The study was supported by an unrestricted grant supplied by Pfizer in 2016. The funding company had no influence on the study design, medical treatment, data analysis and interpretation of the study. It had no influence on writing this report either.
Author information
Authors and Affiliations
Contributions
CR participated in protocol writing and patient inclusion, participated in data analysis and drafted the manuscript. MH carried out data analysis and drafted the result section. CHL participated in data interpretation and manuscript writing. AR participated in patient inclusion, participated in data analysis and drafted the manuscript. SA conceived the study participated in coordination and data analysis and finalized the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with good clinical practice standards (GCP) and approved by the local ethics committee (Ethikkommission der Universitätsmedizin Göttingen, 16/3/14), the European PAS registry (EUPAS8748) and the Bundesinstitut für Arzneimittel und Medizinprodukte (BfArM) (NIS-Studien-Nr. 5508) before enrolment. All patients provided written informed consent before study related procedures.
Consent for publication
Not applicable.
Competing interests
CR reports personal fees from Boehringer, Roche, BerlinChemie, Jansen, Astra Zeneca und GSK outside the submitted work. AR reports grants from EliLilly, BMS, Boehringer Ingelheim, AstraZeneca, MSD, Pfizer, AbbVie, Novartis and Roche, outside the submitted work. SA reports grants and personal fees from Boehringer Ingelheim, personal fees from Novartis, AstraZeneca, GSK, Chiesi and Merini, outside the submitted work. The other authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Comparison of Mean Total HADS during treatment period.
Additional file 2.
Comparison of Mean EORTC-QLQ C30 3.0 subscale nausea and vomiting. Comparison of Mean EORTC-QLQ C30 3.0 subscale fatigue and insomnia.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Reinhardt, C., Harden, M., Herrmann-Lingen, C. et al. Smoking cessation by combined medication and counselling: a feasibility study in lung cancer patients. BMC Pulm Med 22, 252 (2022). https://doi.org/10.1186/s12890-022-02048-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-022-02048-1