Abstract
Background
The critical management of advanced non-small-cell lung carcinoma (NSCLC), especially when complicated by severe airway stenosis, is difficult and often leads to high clinical risks and medical costs.
Case presentation
A 51-year-old previously healthy male was admitted to the Department of Respiratory and Critical Care Medicine, Taizhou People’s Hospital, in November 2018 for haemoptysis and difficulty breathing during a 15-d period. Following admission, chest computed tomography (CT) showed a large mass in the left hilum with atelectasis in the left upper lobe and obstructive pneumonia in the left lower lobe. Bronchoscopy revealed that the lesions occurred in the distal segment of the left main trachea, with occlusion of the left upper bronchus and significant narrowing of the lower bronchus. A basal mucosal biopsy of the lump tissue was performed after haemostasis treatment with sub-plasma coagulation (APC), and squamous lung carcinoma was confirmed. Following the final diagnosis, the patient was successfully treated with implantation of 125I radioactive seeds via transbronchial needle aspiration (c-TBNA) combined with chemotherapy.
Conclusion
We believe that implantation of 125I radioactive seeds via c-TBNA is an effective treatment for patients with advanced lung cancer and those presenting with severe and mixed main bronchus stenosis.
Similar content being viewed by others
Background
Non-small-cell lung carcinoma (NSCLC) is the most common type of cancer worldwide. Almost 70–75% of patients with NSCLC have advanced stage IIIB or IV disease when first diagnosed [1]. Advanced NSCLC, particularly at the time where the central airway is involved, which often leads to severe airway stenosis, is a dangerous disease that is challenging to manage and has a poor prognosis [2]. Although substantial progress has been made in terms of bronchoscopy interventional techniques, such as electrocoagulation, sub-plasma coagulation (APC), airway stenting, laser therapy and balloon dilatation in recent years [3], the critical management of some patients with airway stenosis is difficult and remains a focus of attention. The choice of therapy depends on the type of airway stenosis, pulmonary function and life expectancy of the patient. In recent years, studies have examined 125I radioactive seed implantation performed under CT or ultrasound guidance for the treatment of lung cancer, and many patients have been reported to benefit from this alternative technique [4]. However, central bronchogenic carcinoma patients cannot benefit from this alternative technique because of a high risk of haemorrhage or pneumothorax [5, 6]. To the best of our knowledge, reports of 125I radioactive seed implantation via transbronchial needle aspiration (c-TBNA) are rare [7]. The present study reports the diagnosis of an advanced NSCLC patient with severe airway stenosis and the outcomes of treatment with 125I radioactive seed implantation combined with chemotherapy.
Case presentation
This case report was carried out in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Taizhou People’s Hospital, Jiangsu, China. Written informed consent was obtained from the patient. A 51-year-old previously healthy male was admitted to the Department of Respiratory and Critical Care Medicine, Taizhou People’s Hospital, in November 2018 for haemoptysis and difficulty breathing during a 15-d period. Following admission, physical examinations revealed that vital signs were stable. Left-side respiratory movement was weakened and left upper lung tremor was significantly enhanced. Expiratory wheezing was heard throughout the left lung, and no moist rales were noted. The patient had a regular heart rhythm, and no oedema was observed in the lower extremities.
A complete blood test revealed a white blood cell count of 6.84 × 109/l and a large white blood cell ratio (percentage of white blood cells that are neutrophils) of 82.8%. A blood gas analysis demonstrated a pH of 7.38, 90 mmHg PaO2, 35 mmHg PaCO2 and 29 mmol/l HCO3−. Serum tumour markers demonstrated 3.56 ng/ml of CEA, 18.75 ng/ml of Cyfra21–1 and 1.2 ng/ml of SCC. No obvious abnormalities in liver or kidney function were observed. CT showed 4.1 × 7.1 cm lesions with irregular, thick-walled, hollow and unclear boundaries in the left hilum, as well as atelectasis in the left upper lobe, obstructive pneumonia in the left lower lobe and a mass in the mediastinum and left hilar lymph node. Bronchoscopy revealed that the lesions occurred in the distal segment of the left main trachea, with occlusion of the left upper bronchus and significant narrowing of the lower bronchus (Fig. 1a). A basal mucosal biopsy of the lump tissue was performed after haemostasis treatment with APC, and squamous lung carcinoma was confirmed. The patient was eventually diagnosed with left upper lung squamous cell carcinoma, with stage IIIB (cT3N2M0) and ECOG’s PS1.
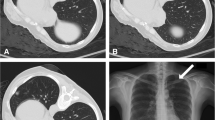
a Bronchoscopy revealed that the lesions occurred in the distal segment of the left main trachea, with occlusion of the left upper bronchus and significant narrowing of the lower bronchus. b, c 125I radioactive seeds were pushed into the tumour via the core of the needle after the puncture needle was passed through the wall of the externally compressed trachea or into the tumour. d Bronchoscopy at the second cycle after chemotherapy revealed disappearance of the lesions in the distal segment of the left main trachea, with no obstruction of the left upper lobe or the left lower lobe
Following confirmation, the patient was treated with 125I radioactive seed implantation via c-TBNA combined with chemotherapy. The implantation of 0.7 mCi 125I radioactive seeds (catalogue no., CIAE-6711; Chinese Atomic Energy Science Institution, Beijing, China) was used for this patient. The dose of the radioactive seeds was determined according to the following empirical formula: total dose (mCi) = (length + width + height) / 3 × 5. The number of seeds was calculated as follows: number of seeds = total dose/0.7. The prescription dose determined from this formula was expected to reach 100–130 Gy [7]. The endoscope was obtained from Olympus (BF-1 T260; Olympus Corporation, Tokyo, Japan). The technique used for 125I radioactive seed implantation was, overall, the same as that used for the regular c-TBNA examination and was performed under general anaesthesia of the airway with the use of a laryngeal mask and monitoring of the heart (via an electrocardiogram), pulse, blood pressure and blood oxygen saturation. Prior to implantation, 2–3 seeds were placed in the biopsy channel of the endoscope biopsy sampling needles (Changzhou Detan Medical Devices Co., Ltd., Changzhou, Jiangsu, China) (Fig. 2). The channel port was blocked with sterile glucose agar after the placement of the seeds. 125I radioactive seeds were pushed into the tumour via the core of the needle after the puncture needle passed through the wall of the externally compressed trachea or into the tumour (Fig. 1b, c). Based on chest CT and bronchoscopy, the size of the lesions in the left hilum was approximately 1.8*2.1*2.6. Eighteen seeds were implanted via c-TBNA in the patient. The distance between each puncture point was controlled at approximately 0.5 cm, and the puncture needle was placed perpendicular to the lesion during the puncture in order to ensure an even radiation dose in the lesion. To avoid unnecessary radiation pollution, the operation was carried out in the DSA operating room with adequate protective covering for the operators. The operation was successfully performed, and the vital signs of the patient were stable during and after the operation. Post-operative CT 3 days later confirmed that high-density 125I radioactive seeds were observed in the tumour (Fig. 3a, b). After the implantation of the 125I radioactive seeds, the patient received chemotherapy with GP (gemcitabine: 1000 mg/m2, i.v., days 1 and 8; cisplatin: 80 mg/m2, i.v., day 1), which was repeated every 21 days. At the first cycle after chemotherapy, the patient demonstrated a distinctly improved mental condition with no further activity haemoptysis attacks, as well as a distinct improvement of left chest tightness. Compared with the previous chest CT scan, a chest CT scan at the second cycle after chemotherapy revealed disappearance of atelectasis and obstructive pneumonia in the left upper lung, as well as evident improvement of the lesions in the left hilum (Fig. 3c, d). A follow-up bronchoscopy at the second cycle after chemotherapy revealed disappearance of the lesions in the distal segment of the left main trachea, with no obstruction of the left upper lobe or the left lower lobe (Fig. 1d). Following two rounds of chemotherapy, the patient’s disease was controlled, and partial remission of lung cancer was achieved.
Endoscope biopsy sampling needles: The inner tube of the tissue needles consisted of a hose with a steel wire directly connected to the syringe, which could be automatically moved during suction. 2–3 125I radioactive seeds were placed in the biopsy channel of the endoscope biopsy sampling needles after suction of the syringe to the specified scale. The channel port of the needles was blocked with sterile glucose agar after the placement of the seeds. 125I radioactive seeds were pushed into the tumour by using the steel wire
a, b Post-operative CT 3 days later confirmed that high-density 125I radioactive seeds were observed in the tumour (a: lung window, b: mediastinal window). c, d Compared with the previous chest CT scan, the chest CT scan at the second cycle after chemotherapy revealed disappearance of atelectasis and obstructive pneumonia in the left upper lung, as well as evident improvements in the lesions of the left hilum (a: lung window, b: mediastinal window)
Discussion and conclusions
The critical management of advanced NSCLC, especially when complicated by severe airway stenosis, is difficult and often leads to high clinical risks and medical costs. Opening of the narrow trachea as soon as possible is one of the key factors affecting the prognosis of the disease [8]. Although there has been considerable progress in recent years in terms of the development of bronchoscopy interventional techniques, including electrocoagulation, APC, airway stenting, balloon dilatation, laser therapy and cryoablation, the critical management of some patients with obstruction of the distal section of the central airway caused by intraluminal tumour growth or extrinsic compression is difficult and remains a focus of attention [9].
Radioactive seeds are implanted directly into the lesion as a kind of brachytherapy, and these seeds kill the tumour cells by consistently releasing rays [10]. 125I radioactive seeds represent the most common type of permanently implanted seed, which can continuously release low-power γ-rays, with a half-life of 59.6 days and an available irradiation range of 17 mm, thus continuously inhibiting cell proliferation and angiogenesis as well as inducing apoptosis and killing tumour cells [11]. Percutaneous 125I radioactive seed implantation is usually performed under computed tomography (CT) or ultrasound guidance, and this technique has demonstrated effectiveness in local control and improvements of the OS time and rate [12,13,14,15]. However, for central-type lung cancer, the technique of percutaneous puncture is associated with a great risk of haemorrhage and pneumothorax [7].
With the development of endoscopic interventional diagnosis and treatment techniques, trans-bronchoscopy 125I radioactive seed implantation has been reported for the treatment of central airway stenosis [7]. This technique is mainly guided by bronchoscopy; 125I radioactive seeds are implanted into the tumour tissue via c-TBNA or EBUS-TBNA technology [16]. After implantation, the 125I radioactive seeds inhibit cell proliferation and angiogenesis, induce apoptosis, and kill tumour cells [11]. This technology provides a new and effective palliative treatment for patients with central lung cancer; it can permanently destroy tumour cells, maximize the patient’s lung function, improve the patient’s tracheal patency, and improve the patient’s quality of life.
The lesions in the reported patient occurred in the distal segment of the left main bronchus, with occlusion of the left upper bronchus and significant narrowing of the lower bronchus. To the best of our knowledge, traditional respiratory endoscopic intervention techniques, such as laser ablation and stent placement, which are considered the gold-standard treatments for narrowing of the trachea and main bronchus, were not effective and thus were not preferred methods for the specific site of bronchus narrowing in the presented patient. The site of bronchus narrowing was the real problem for the patient; thus, there was a need for a different type of therapy. Fortunately, the patient was successfully treated with trans-bronchoscopy with 125I radioactive seed implantation combined with chemotherapy. We believe that the treatment strategy used for this patient may have opened the respiratory tract in a short period of time, reduced the clinical symptoms, and thus improved the patient’s quality of life and survival time.
In conclusion, the majority of patients with advanced central lung cancer eventually require palliative treatment and individualized treatment strategies. Trans- bronchoscopy with 125I radioactive seed implantation combined with chemotherapy may be a potential and alternative treatment for some patients. It has been reported that 3 to 4 days after 125I radioactive seed implantation may be the best time for initial chemotherapy because the radioactive effect of the 125I radioactive seeds at this time result in an increase in vascular permeability and a facilitation of drug penetration [17]. However, due to the limitation of the number of patients, a mature and feasible radioactive particle-based comprehensive program for these patients still requires further large-scale clinical research.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- APC:
-
Sub-plasma coagulation
- CT:
-
Computed tomography
- c-TBNA:
-
transbronchial needle aspiration
- NSCLC:
-
Non-small-cell lung carcinoma
References
Ettinger DS, Aisner DL, Wood DE, Akerley W, Bauman J, Chang JY, et al. NCCN guidelines insights: non-small cell lung Cancer, version 5.2018. J Natl Compr Cancer Netw. 2018;16(7):807–21. https://doi.org/10.6004/jnccn.2018.0062.
Govindan R, Bogart J, Vokes EE. Locally advanced non-small cell lung cancer: the past, present, and future. J Thorac Oncol. 2008;3(8):917–28. https://doi.org/10.1097/JTO.0b013e318180270b.
Guibert N, Mazieres J, Marquette CH, Rouviere D, Didier A, Hermant C. Integration of interventional bronchoscopy in the management of lung cancer. Eur Respir Rev. 2015;24(137):378–91. https://doi.org/10.1183/16000617.00010014.
Zhang F, Wang J, Guo J, Li Y, Huang X, Guan Z, et al. Chinese expert consensus workshop report: guideline for permanent iodine-125 seed implantation of primary and metastatic lung tumors. Thorac Cancer. 2019;10(2):388–94. https://doi.org/10.1111/1759-7714.12912.
Niu L, Zhou L, Xu K, Mu F. Combination of cryosurgery and Iodine-125 seeds brachytherapy for lung cancer. J Thorac Dis. 2012;4(5):504–7. https://doi.org/10.3978/j.issn.2072-1439.2012.09.03.
Zhang S, Zheng Y, Yu P, Yu F, Zhang Q, Lv Y, et al. The combined treatment of CT-guided percutaneous 125I seed implantation and chemotherapy for non-small-cell lung cancer. J Cancer Res Clin Oncol. 2011;137(12):1813–22. https://doi.org/10.1007/s00432-011-1048-3.
Lu M, Pu D, Zhang W, Liao J, Zhang T, Yang G, et al. Trans-bronchoscopy with implantation of 125I radioactive seeds in patients with pulmonary atelectasis induced by lung cancer. Oncol Lett. 2015;10(1):216–22.
Jiang AG, Gao XY, Lu HY. Diagnosis and management of an elderly patient with severe tracheomalacia: a case report and review of the literature. Exp Ther Med. 2013;6(3):765–8.
Scarlata S, Fuso L, Lucantoni G, Varone F, Magnini D, Antonelli Incalzi R, et al. The technique of endoscopic airway tumor treatment. J Thorac Dis. 2017;9(8):2619–39. https://doi.org/10.21037/jtd.2017.07.68.
Mao Y, Yang X, Li M, Guo W, Zhang W. Treating cancerous large airway stenosis with staging radioactive particle implantation guided by computed tomography and fiber bronchoscopy: a clinical study. World J Surg Oncol. 2017;15(1):149. https://doi.org/10.1186/s12957-017-1216-2.
Xiang GL, Zhu XH, Lin CZ, Wang LJ, Sun Y, Cao YW, et al. 125I seed irradiation induces apoptosis and inhibits angiogenesis by decreasing HIF-1α and VEGF expression in lung carcinoma xenografts. Oncol Rep. 2017;37(5):3075–83. https://doi.org/10.3892/or.2017.5521.
Wang ZM, Lu J, Liu T, Chen KM, Huang G. Liu FJ.CT-guided interstitial brachytherapy of inoperable non-small cell lung cancer. Lung Cancer. 2011;74(2):253–7. https://doi.org/10.1016/j.lungcan.2011.03.006 Epub 2011 Apr 21.
Zhang FJ, Li CX, Wu PH, Wu YX, Jiao DC, Liu J, et al. CT guided radioactive 125I seed implantation in treating localized advanced pulmonary carcinoma. Zhonghua Yi Xue Za Zhi. 2007;87(46):3272–5 (In Chinese).
Zhang T, Lu M, Peng S, Zhang W, Yang G, Liu Z, et al. CT-guided implantation of radioactive 125I seed in advanced non-small-cell lung cancer after failure of first-line chemotherapy. J Cancer Res Clin Oncol. 2014;140(8):1383–90. https://doi.org/10.1007/s00432-014-1655-x Epub 2014 Apr 11.
Huang Q, Chen J, Chen Q, Lai Q, Cai S, Luo K, et al. Computed tomographic- guided iodine-125 interstitial implants for malignant thoracic tumors. Eur J Radiol. 2013;82(11):2061–6.
Xiao DJ, Li CY, Yuan GB, Wang YC. Ultrasound bronchoscopy-guided implantation of 125I seed in the treatment of lung cancer. J Shanxi Med Univ. 2017;48(5):467–70. https://doi.org/10.13753/j.issn.1007-6611 (In Chinese).
Cron GO, Beghein N, Crokart N, Chavée E, Bernard S, Vynckier S, et al. Changes in the tumor microenvironment during low-dose-rate permanent seed implantation iodine-125 brachytherapy. Int J Radiat Oncol Biol Phys. 2005;63(4):1245–51.
Acknowledgements
Not applicable.
Funding
This work was supported by the “Six One Project” Top Talent Research Project of Jiangsu Commission of Health (GY2018033).
Author information
Authors and Affiliations
Contributions
AGJ contributed to study design,data collection, and preparation of the manuscript. ZQD and HYL contributed to study design and data collection. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This case report was approved by the Ethics Committee of Taizhou People’s Hospital, Jiangsu, China. Written informed consent was obtained from the patient.
Consent for publication
The patient provided written informed consent for the publication of any associated data and accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Jiang, AG., Lu, HY. & Ding, ZQ. Implantation of 125I radioactive seeds via c-TBNA combined with chemotherapy in an advanced non-small-cell lung carcinoma patient. BMC Pulm Med 19, 205 (2019). https://doi.org/10.1186/s12890-019-0974-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-019-0974-8