Abstract
Background
The presence of emphysema on computed tomography (CT) is associated with an increased frequency of lung cancer, but the postoperative outcomes of patients with pulmonary emphysema are not well known. The objective of this study was to investigate the association between the extent of emphysema and long-term outcomes, as well as mortality and postoperative complications, in early-stage lung cancer patients after pulmonary resection.
Methods
The clinical records of 566 consecutive lung cancer patients who underwent pulmonary resection in our department were retrospectively reviewed. Among these, the data sets of 364 pathological stage I patients were available. The associations between the extent of lung emphysema and long-term outcomes and postoperative complications were investigated. Emphysema was assessed on the basis of semiquantitative CT. Surgery-related complications of Grade ≥ II according to the Clavien-Dindo classification were included in this study.
Results
Emphysema was present in 63 patients. The overall survival and relapse-free survival of the non-emphysema and emphysema groups at 5 years were 89.0 and 61.3% (P < 0.001), respectively, and 81.0 and 51.7%, respectively (P < 0.001). On multivariate analysis, significant prognostic factors were emphysema, higher smoking index, and higher histologic grade (p < 0.05). Significant risk factors for poor recurrence-free survival were emphysema, higher smoking index, higher histologic grade, and presence of pleural invasion (P < 0.05). Regarding Grade ≥ II postoperative complications, pneumonia and supraventricular tachycardia were more frequent in the emphysema group than in the non-emphysema group (P = 0.003 and P = 0.021, respectively).
Conclusion
The presence of emphysema affects the long-term outcomes and the development of postoperative complications in early-stage lung cancer patients.
Similar content being viewed by others
Background
Lung cancer is the most common malignancy and the leading cause of cancer-related death in men worldwide [1]. Tobacco smoking is the most common risk factor for developing not only lung cancer, but also chronic obstructive pulmonary disease (COPD) [2, 3]. It has been shown that oxidants in cigarette smoke cause chronic biological damage, including DNA injury [4,5,6], which then results in a predisposition to these pulmonary diseases.
A mixture of small airway disease and emphysema causes airflow limitation in COPD [7]. Pulmonary emphysema is defined as abnormal permanent enlargement of the airspaces distal to the terminal bronchioles accompanied by destruction of their walls without obvious fibrosis [8]. A previous study showed that the severity of emphysema did not reflect the COPD disease stage well [9]. Some severe COPD patients also have terrible emphysema, whereas there are other patients with very little evidence of emphysema. Therefore, one cannot easily classify the COPD phenotypes, such as “pink puffers” and “blue bloaters”, using the severity of emphysema as a criterion. Thus, to assess emphysematous change in the lung and its implications for lung cancer is meaningful. Recent reports have shown that the extent of emphysema on computed tomography (CT) is associated with an increased frequency of lung cancer [10, 11], but the postoperative outcomes of pulmonary emphysema have not been studied in depth [12,13,14].
Therefore, this study was conducted to investigate the associations between the extent of emphysema detected semiquantitatively on CT scans and long-term outcomes, as well as mortality and postoperative complications, of stage I lung cancer patients after pulmonary resection.
Methods
Patients
Of 566 patients with non-small cell lung cancer (NSCLC) admitted from 2009 to 2015 to the Division of Thoracic and Cardiovascular Surgery at Niigata University Hospital, 392 had pathological stage I disease. Because the purpose of this study was to identify whether the extent of emphysema could be a prognostic factor, the exclusion criteria were: 1) neoadjuvant therapy (chemotherapy and/or radiation therapy); 2) the presence of interstitial pneumonia (IP); and 3) incomplete resection with macroscopic or microscopic residual disease. After exclusion of 28 cases, a consecutive series of 364 of these patients who had pathological stage I disease and had undergone lung resection were retrospectively reviewed in the present study. The institutional review board approved this study (Niigata University, 2018–0133) and waived the requirement for informed consent because the study was a retrospective review.
The preoperative patient data included age, sex, body mass index (BMI), smoking habit, spirometric variables, tumor size, surgical procedure (lobectomy or sublobar resection), and the extent of emphysema. The patients with lung cancer located within the outer one-third of the lung field and diameter of ≤2 cm as measured on CT underwent intentional sublobar resection, especially segmentectomy. However, the patients with compromised pulmonary reserve underwent wedge resection. Pulmonary emphysema was diagnosed by visual semiquantitative CT, as described later. Spirometric variables included forced vital capacity (FVC) and forced expiratory volume in 1 s (FEV1). Pathologic data obtained after surgery included histologic subtype, histologic grade, and pleural invasion. The tumors were classified histologically as adenocarcinoma, squamous cell carcinoma, and others and graded as well, moderately, or poorly differentiated carcinoma according to the WHO classification [15]. Pathological stage was determined according to the 7th edition of the TNM classification for lung cancer proposed by the International Association for the Study of Lung Cancer (IASLC) [16].
Diagnosis of emphysema
CT images, 1 to 2-mm-thick, were obtained using window levels appropriate for lung (level, − 910 Hounsfield units (HU); width, 1500 HU) from the apex to the diaphragm at full inspiration with the patient in the supine position. All CT scans at 1-cm intervals from each case were coded and masked for identifiable information and then evaluated by one thoracic radiologist (H. I.) and two thoracic surgeons (S.S. and Y.S.) who were blinded to the clinical data.
The system used to score the extent of emphysema on the CT scans was adapted from prior work by Goddard et al. [17] and Bergin et al. [18]. A brief summary was as follows. Each slice was assessed individually, and the right and left lungs were graded separately according to the percentage area that demonstrated changes suggestive of emphysema. Areas of low attenuation and vascular disruption were considered suggestive of emphysema. A grade of 0 was given if there was no abnormality. If less than 25% of the pulmonary parenchyma in a slice was considered to show vascular disruption and low attenuation compared with remaining lung parenchyma, the score was 1; between 25 and 50%, the score was 2; between 50 and 75%, the score was 3; and if more than 75% of the lung parenchyma on 1 side suggested emphysema, the maximum score of 4 was given. This gave a maximum possible of 4 for the right lung and 4 for the left lung or a total of 8 for 1 slice. All slices from the apex to the diaphragm at 1-cm intervals were assessed in each patient (14 to 29 slices per patient). The maximal possible score in a patient in whom 20 slices were taken was 8 × 20 = 160. The final score for each patient was calculated as a percentage of the maximal possible CT score.
The percentage of voxels with attenuation values lower than − 910 HU among the total number of voxels in the entire lung was considered to be the low attenuation area (LAA) [19, 20]. Emphysema was defined as being present if LAAs occupied more than 10% of the lung, according to past reports [11, 12].
Postoperative complications
Surgery-related complications were graded according to the Clavien-Dindo classification [21, 22] as follows: grade 0, no complications; grade I, some deviation from the normal postoperative course; grade II, complications requiring management not exceeding intravenous medications, total parenteral nutrition, enteral nutrition, or blood transfusion; grade III, complications requiring surgical, endoscopic, or radiologic intervention; grade IV, life-threatening complications requiring intensive care; and grade V, complications causing the death of the patient. Complications of Grade ≥ II were included in this study.
Postoperative follow-up
After the patients were discharged from hospital, they were followed in our outpatient clinic at intervals of 3 months during the first 5 years postoperatively and then every 6 months. During follow-up, at intervals of 6 to 12 months, the patients were routinely evaluated for tumor recurrence or metastasis by chest CT and, if necessary, head and abdominal CT and positron emission tomography with 18F-fluoro-2-d-glucose/computed tomography (FDG-PET/CT).
Statistical analysis
The characteristics of the patients are shown as counts and proportions. The categorical variables were compared using the chi-squared test or Fisher’s exact test when there were ≤ 5 observations in a cohort. The unpaired Student’s t-test was used to compare quantitative parameters. The relationship between two continuous variables was tested by linear regression analysis. A univariate Cox regression model was used for survival analysis. Using a threshold of P < 0.05 on univariate analysis, variables were then entered in a stepwise Cox regression analysis to identify independent factors, with the criterion for retention of factors in the final model being P = 0.05. Recurrence-free survival (RFS) was defined as the time from surgery to documented clinical recurrence or death, with overall survival (OS) defined as the time from surgery to death. The Kaplan-Meier method was used to prepare survival curves, which were then compared using the log-rank test. Differences with a P value < 0.05 were considered significant. SPSS for Windows Version 25.0 (SPSS, Inc., Chicago, IL, USA).
Results
Perioperative patient characteristics
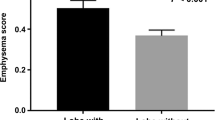
Emphysema was diagnosed in 63 (17.3%) and COPD was diagnosed in 94 (25.8%) of the 364 patients. Perioperative patient characteristics are summarized in Table 1. The median follow-up period was 45.8 months (range, 2.4–105 months). The following were more frequent in the emphysema group than in the non-emphysema group: male sex, thinner patients, higher smoking index, squamous cell carcinoma, pleural invasion-positive, and higher histologic grade. On pulmonary function testing, FEV1/FVC was significantly worse, but VC was significantly better in the emphysema group than in the non-emphysema group. Figure 1 shows the linear relationship between FEV1/FVC and %LAA; a weak relationship was noted between these parameters (r = 0.351, P < 0.001).
Survival analysis
During the study period, there were 32 deaths (10.6% of patients) in the non-emphysema group and 20 deaths (31.7% of patients) in the emphysema group. Primary lung cancer recurrence was seen in 36 patients (12.0%) in the non-emphysema group and 18 patients (28.6%) in the emphysema group. Five-year overall survival was 89.0 and 61.3% in the non-emphysema and emphysema groups, respectively (P < 0.001; Fig. 2a), with 5-year relapse-free survivals of 81.0 and 51.7%, respectively (P < 0.001; Fig. 2b).
Univariate and multivariate analyses of risk factors for long-term surgical outcomes
Using the univariate Cox regression model, male sex, higher age, lower BMI, higher smoking index, lower %VC, lower FEV1/FVC, presence of COPD, histology, higher histologic grade, presence of pleural invasion, and the presence of emphysema were significantly associated with overall survival (Table 2), whereas male sex, higher smoking index, lower %VC, lower FEV1/FVC, presence of COPD, tumor size, histology, higher histologic grade, presence of pleural invasion, and the presence of emphysema were significantly associated with relapse-free survival (Table 3).
Using the stepwise Cox regression analysis, the presence of emphysema [hazard ratio (HR), 1.927; 95% confidence interval (95% CI), 1.050–3.537; P = 0.034], higher smoking index [HR, 1.000; 95% CI, 1.000–1.001; P = 0.013], and higher histologic grade [moderately differentiated: HR, 2.205; 95% CI, 1.115–4.360; P = 0.023, and poorly differentiated: HR, 2.990; 95% CI, 1.388–6.442; P = 0.005, respectively] were considered independent predictors of poor overall survival (Table 2), whereas the presence of emphysema [HR, 2.122; 95% CI, 1.173–3.829; P = 0.013], higher smoking index [HR, 1.000; 95% CI, 1.000–1.001; P = 0.006], lower %VC [HR, 0.985; 95% CI, 0.971–0.999; P = 0.032], higher histologic grade [moderately differentiated: HR, 1.934; 95% CI, 1.111–3.367; P = 0.020, and poorly differentiated: HR, 2.026; 95% CI, 1.048–3.915; P = 0.036, respectively], and presence of pleural invasion [HR, 1.845; 95% CI, 1.154–2.951; P = 0.011] were considered independent predictors of poor recurrence-free survival (Table 3).
Postoperative morbidity and mortality
Table 4 summarizes postoperative grade ≥ II cardiopulmonary complications and mortality. The emphysema group had significantly more episodes of pneumonia requiring antibiotic therapy (P = 0.003) and of supraventricular tachycardia requiring medication (P = 0.021) than the non-emphysema group. No patients underwent mechanical ventilation and died within 30 days after surgery, but one patient died of pneumonia during the hospital stay in the non-emphysema group.
Discussion
In this study, emphysematous lung was found to be the critical predictor of long-term survival in stage I lung cancer patients undergoing pulmonary resection. Furthermore, lung cancer patients with emphysema developed more postoperative cardiopulmonary complications requiring treatment, such as pneumonia and supraventricular tachycardia, than those without emphysema.
The extent of abnormal inflammatory responses in small airways and parenchymal destruction of the lungs promotes airflow limitation in COPD [7]. Several studies have shown that COPD diagnosed on the basis of functional limitation by spirometry worsened the prognosis of early-stage neoplasms [23,24,25,26,27]. However, the clinicopathological characteristics and postoperative outcomes of early-stage lung cancer patients with pulmonary emphysema have not well been studied [13].
With regard to the characteristics of patients with emphysema, some studies have addressed this point. Patients with emphysematous lungs had a higher prevalence of male sex and a smoking history [12, 14]. Regarding histology, emphysema lung was associated with a risk of small cell lung carcinoma (SCLC) and squamous cell carcinoma [28, 29]. In the present study, male sex, thinner patients, higher smoking index, squamous cell carcinoma, high histologic grade, and pleural invasion-positive were more frequent in patients with emphysema, similar to previous reports.
In this study, the correlation between FEV1/FVC and %LAA was found to be significant but weak overall (r = 0.351, P < 0.001). This finding was consistent with that of previous studies [9, 30,31,32], which suggested that the cause of airflow limitation in COPD was not mainly pulmonary emphysema.
In the present study, 5-year overall survival and relapse-free survival rates were 61.3 and 51.7%, respectively. Patients with emphysema in pathological stage I had poorer OS and RFS than those without emphysema. Ueda et al. defined emphysema as the presence of LAAs that occupied more than 5% of the lung based on objective quantification using CT densitometry and reported 5-year OS and RFS rates of 39.4 and 44.0% after pulmonary resection in lung cancer patients with emphysema [13]. In the present study, emphysema was defined as the presence of LAAs that occupied more than 10%, because this was thought to reflect emphysema more strongly. Nevertheless, the reason for the better results of the present study might be due to differences in patient background characteristics. Ueda et al. recruited patients who were all smokers, and 28 (28%) had pathologic stage II or higher [13]. In contrast, the present study included a consecutive series of 364 patients who underwent lung resection for pathological stage I lung cancer. In addition, a few studies investigated the outcomes of lung cancer with emphysema. Zulueta et al. showed that the presence of emphysema was a significant predictor of death from lung cancer, and as for the extent of emphysema, marked emphysema, in which discrete areas of decreased attenuation could be identified in more than one-half of the lung parenchyma, was an independent risk factor for death from lung cancer [33]. Gullon et al. showed that emphysema, which occupied > 10% of the lung, was an independent prognostic factor, but not COPD, in patients with advanced-stage lung cancer [12].
The mechanism of the association between emphysema and a poor prognosis in lung cancer patients has not been fully clarified. Both emphysema and lung cancer are affected by reactive oxidant species caused by tobacco smoking, which induce chronic inflammatory changes in the lungs [34, 35]. Chronic inflammation, through the production of inflammatory cells and inflammatory mediators, including chemokines, cytokines, prostaglandins, and so on, facilitates the survival and proliferation of malignant cells and promotes angiogenesis and metastasis [36]. Various inflammatory mediators, such as tumor necrosis factor-α (TNF-α), transforming growth factor β (TGF-β), interleukin-1 (IL-1), and IL-6, have been reported to promote circulating tumor cell survival and the epithelial-mesenchymal transition, which play an important role in cellular proliferation, migration, invasion and immunosurveillance of NSCLC [37, 38]. Lourenco et al. reported that the extent of emphysema impair the mucociliary function, so carcinogens tend to pool in the emphysematous lung with impaired mucociliary clearance, leading to lung cancer development [39]. Genetically, Yang et al. showed that the patients who carry an α1-antitrypsin deficiency allele may have an increased risk for developing lung squamous cell or bronchoalveolar carcinoma [40]. The protein that cannot inhibit neutrophil elastase are regularly polymerized by the α1-antitrypsin deficiency. Under the α1-antitrypsin deficiency, these protein polymers are chemotactic for neutrophils and produce the inflammatory change in the lung, and lead to early-onset and emphysema [41]. Muller et al. showed that the percentage of fibroblasts positive for senescence-associated β-galactosidase was significantly higher in emphysematous lung than in non-emphysematous lung [42]. They suggested that lung fibroblasts in emphysematous lung were associated with premature aging and therefore predisposed to cancer.
The postoperative complications graded according to the Clavien-Dindo classification in the present study showed that emphysema lung was closely associated with pneumonia and supraventricular tachycardia. Previous studies have suggested that postoperative pulmonary complications were linked to several preoperative variables including obesity [43], COPD [26, 44], smoking habit [43], and so on. Takahashi et al. showed that emphysema based on high-resolution CT (HRCT) was independently associated with pulmonary complications after single lobectomy [45]. Several studies reported that emphysema, bronchiectasis, and bronchial wall thickness on HRCT are predictors of COPD severity [46, 47]. It has been assumed that as COPD is impaired from the alveolar surface to the capillary endothelium region, a decrease in gas exchange space and capillary area occurs. Then, atelectasis due to increased sputum and altered mucociliary clearance also occurs more frequently in patients with emphysema [48].
The risk of supraventricular tachycardia (SVT) following pulmonary resection has been reported in several papers, with an incidence ranging between 10 and 28% [49,50,51]. In patients with emphysema lung, 6 (9.5%) of 63 had postoperative SVT, and this incidence rate was lower than in previous reports, but only patients with postoperative SVT grade ≥ 2 could be included in the present study. It has remained unclear why SVT develops more frequently in patients with emphysema. A previous study reported that the decrease of elastic recoil induced by emphysema produces a decrease in maximal expiratory airflow and an increase in residual volume, contributing to shortness of breath during exertion and at rest [52]. Emphysema is associated with pulmonary hypertension not only at rest, but also during exercise in patients compared with general subjects [53]. Thus, right heart strain following right ventricular dilatation could occur with an increase in pulmonary artery pressures. Therefore, patients with emphysema might have a higher incidence of SVT than those without emphysema. However, pulmonary artery pressures have not been routinely examined using Swan-Ganz catheters or echocardiograms in our patients, and further study will be required to address this issue.
Our study has several strengths. First, a detailed visual score of the extent of emphysema could be obtained because CT images were viewed from the apex to the diaphragm at 1-cm intervals in each patient. Thus, CT images of 14 to 29 slices were assessed for each patient. Second, postoperative complications were assessed objectively based on the Clavien-Dindo classification. Only complications of Grade ≥ II, which required management, were included in this study. Thus, the subjects with postoperative complications seemed to represent clinically relevant patients in this study. Third, surgical outcomes were reported based on the extent of emphysema in patients with early-stage lung cancer, but so far there have been few reports about this issue [13].
Limitations
This study has several limitations. First, it was a retrospective, single-institute study with a small sample size. In particular, of the 63 patients in the emphysema group, there were only 9 women. Thus, it would be difficult to generalize these results to all patients, especially women with emphysema. Second, although quantitative standardized assessment with computer algorithms could be used, visual assessment of emphysema based on CT images, which is a subjective task known to be prone to observer variability [54, 55], was also used to assess the presence and extent of emphysema. However, previous studies have shown the validity of this approach [28, 56]. The visual emphysema score has been described as highly correlated with objective volume-based computerized assessment of the whole lung [9]. Third, this study did not evaluate the outcomes of all patients with resected stage I lung cancer because patients with interstitial pneumonia (IP) and combined pulmonary fibrosis and emphysema were excluded. Although Li et al. suggested that the visual emphysema score could distinguish the lesion of emphysema from UIP more accurately than objective volume-based computerized assessment [28], it has been difficult to accurately distinguish emphysema lung from interstitial pneumonia lung. Fourth, the number of patients with advanced lung cancer was too small in our database to make any definitive conclusions about the effect of emphysema. Thus, whether the impact of emphysema on cancer behavior was strong only in early-stage lung cancer remains unknown. To clarify this issue, a larger series of patients with advanced-stage lung cancer would be required.
Conclusions
The extent of emphysema affects long-term outcomes and the development of postoperative cardiopulmonary complications in surgically resected early-stage lung cancer patients. Thus, it is possible that assessment of emphysema in lung cancer patients using CT before therapeutic intervention could be meaningful to decide the appropriate treatment strategy, such as surgery (lobectomy or sublobar resection), radiotherapy, and so on.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- CT:
-
Computed tomography
- FDG-PET/CT:
-
Positron emission tomography with 18F-fluoro-2-d-glucose/computed tomography
- FEV1:
-
Forced expiratory volume in 1 s
- FVC:
-
Forced vital capacity
- HR:
-
Hazard ratio
- HRCT:
-
High-resolution computed tomography
- HU:
-
Hounsfield units
- IL:
-
Interleukin
- IP:
-
Interstitial pneumonia
- LAA:
-
Low attenuation area
- NSCLC:
-
Non-small cell lung cancer
- OS:
-
Overall survival
- RFS:
-
Recurrence-free survival
- SCLC:
-
Small cell lung carcinoma
- SVT:
-
Supraventricular tachycardia
- UIP:
-
Usual interstitial pneumonia
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2224–60.
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2095–128.
Kodama M, Kaneko M, Aida M, Inoue F, Nakayama T, Akimoto H. Free radical chemistry of cigarette smoke and its implication in human cancer. Anticancer Res. 1997;17(1A):433–7.
Pryor WA. Cigarette smoke radicals and the role of free radicals in chemical carcinogenicity. Environ Health Perspect. 1997;105(Suppl 4):875–82.
Cao C, Lai T, Li M, Zhou H, Lv D, Deng Z, Ying S, Chen Z, Li W, Shen H. Smoking-promoted oxidative DNA damage response is highly correlated to lung carcinogenesis. Oncotarget. 2016;7(14):18919–26.
Hogg JC. Pathophysiology of airflow limitation in chronic obstructive pulmonary disease. Lancet. 2004;364(9435):709–21.
American Thoracic Society. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1995;152(5 Pt 2):S77–121.
Makita H, Nasuhara Y, Nagai K, Ito Y, Hasegawa M, Betsuyaku T, Onodera Y, Hizawa N, Nishimura M, Hokkaido CCSG. Characterisation of phenotypes based on severity of emphysema in chronic obstructive pulmonary disease. Thorax. 2007;62(11):932–7.
de Torres JP, Bastarrika G, Wisnivesky JP, Alcaide AB, Campo A, Seijo LM, Pueyo JC, Villanueva A, Lozano MD, Montes U, et al. Assessing the relationship between lung cancer risk and emphysema detected on low-dose CT of the chest. Chest. 2007;132(6):1932–8.
Wilson DO, Weissfeld JL, Balkan A, Schragin JG, Fuhrman CR, Fisher SN, Wilson J, Leader JK, Siegfried JM, Shapiro SD, et al. Association of radiographic emphysema and airflow obstruction with lung cancer. Am J Respir Crit Care Med. 2008;178(7):738–44.
Gullon JA, Suarez I, Medina A, Rubinos G, Fernandez R, Gonzalez I. Role of emphysema and airway obstruction in prognosis of lung cancer. Lung Cancer. 2011;71(2):182–5.
Ueda K, Jinbo M, Li TS, Yagi T, Suga K, Hamano K. Computed tomography-diagnosed emphysema, not airway obstruction, is associated with the prognostic outcome of early-stage lung cancer. Clin Cancer Res. 2006;12(22):6730–6.
Ueda K, Murakami J, Sano F, Hayashi M, Suga K, Hamano K. Similar radiopathological features, but different postoperative recurrence rates, between stage I lung cancers arising in emphysematous lungs and those arising in nonemphysematous lungs. Eur J Cardiothorac Surg. 2015;47(5):905–11.
Travis W, Brambilla E, Burke A, Marx A, Nicholson A. World Health Organization classification of tumours of the lung, pleura, Thymus and heart. Lyon: IARC Press; 2015.
Detterbeck FC, Boffa DJ, Tanoue LT. The new lung cancer staging system. Chest. 2009;136(1):260–71.
Goddard PR, Nicholson EM, Laszlo G, Watt I. Computed tomography in pulmonary emphysema. Clin Radiol. 1982;33(4):379–87.
Bergin C, Muller N, Nichols DM, Lillington G, Hogg JC, Mullen B, Grymaloski MR, Osborne S, Pare PD. The diagnosis of emphysema. A computed tomographic-pathologic correlation. Am Rev Respir Dis. 1986;133(4):541–6.
Lamers RJ, Thelissen GR, Kessels AG, Wouters EF, van Engelshoven JM. Chronic obstructive pulmonary disease: evaluation with spirometrically controlled CT lung densitometry. Radiology. 1994;193(1):109–13.
Park KJ, Bergin CJ, Clausen JL. Quantitation of emphysema with three-dimensional CT densitometry: comparison with two-dimensional analysis, visual emphysema scores, and pulmonary function test results. Radiology. 1999;211(2):541–7.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Katayama H, Kurokawa Y, Nakamura K, Ito H, Kanemitsu Y, Masuda N, Tsubosa Y, Satoh T, Yokomizo A, Fukuda H, et al. Extended Clavien-Dindo classification of surgical complications: Japan clinical oncology group postoperative complications criteria. Surg Today. 2016;46(6):668–85.
Bugge A, Lund MB, Brunborg C, Solberg S, Kongerud J. Survival after surgical resection for lung Cancer in patients with chronic obstructive pulmonary disease. Ann Thorac Surg. 2016;101(6):2125–31.
Qiang G, Liang C, Xiao F, Yu Q, Wen H, Song Z, Tian Y, Shi B, Guo Y, Liu D. Impact of chronic obstructive pulmonary disease on postoperative recurrence in patients with resected non-small-cell lung cancer. Int J Chron Obstruct Pulmon Dis. 2016;11:43–9.
Sekine Y, Suzuki H, Yamada Y, Koh E, Yoshino I. Severity of chronic obstructive pulmonary disease and its relationship to lung cancer prognosis after surgical resection. Thorac Cardiovasc Surg. 2013;61(2):124–30.
Shibazaki T, Odaka M, Noda Y, Tsukamoto Y, Mori S, Asano H, Yamashita M, Morikawa T. Effect of comorbidities on long-term outcomes after thoracoscopic surgery for stage I non-small cell lung cancer patients with chronic obstructive pulmonary disease. J Thorac Dis. 2018;10(2):909–19.
Zhai R, Yu X, Shafer A, Wain JC, Christiani DC. The impact of coexisting COPD on survival of patients with early-stage non-small cell lung cancer undergoing surgical resection. Chest. 2014;145(2):346–53.
Li Y, Swensen SJ, Karabekmez LG, Marks RS, Stoddard SM, Jiang R, Worra JB, Zhang F, Midthun DE, de Andrade M, et al. Effect of emphysema on lung cancer risk in smokers: a computed tomography-based assessment. Cancer Prev Res (Phila). 2011;4(1):43–50.
Wang W, Xie M, Dou S, Cui L, Zheng C, Xiao W. The link between chronic obstructive pulmonary disease phenotypes and histological subtypes of lung cancer: a case-control study. Int J Chron Obstruct Pulmon Dis. 2018;13:1167–75.
Gelb AF, Hogg JC, Muller NL, Schein MJ, Kuei J, Tashkin DP, Epstein JD, Kollin J, Green RH, Zamel N, et al. Contribution of emphysema and small airways in COPD. Chest. 1996;109(2):353–9.
Gelb AF, Schein M, Kuei J, Tashkin DP, Muller NL, Hogg JC, Epstein JD, Zamel N. Limited contribution of emphysema in advanced chronic obstructive pulmonary disease. Am Rev Respir Dis. 1993;147(5):1157–61.
Hogg JC, Wright JL, Wiggs BR, Coxson HO, Opazo Saez A, Pare PD. Lung structure and function in cigarette smokers. Thorax. 1994;49(5):473–8.
Zulueta JJ, Wisnivesky JP, Henschke CI, Yip R, Farooqi AO, McCauley DI, Chen M, Libby DM, Smith JP, Pasmantier MW, et al. Emphysema scores predict death from COPD and lung cancer. Chest. 2012;141(5):1216–23.
Brody JS, Spira A. State of the art. Chronic obstructive pulmonary disease, inflammation, and lung cancer. Proc Am Thorac Soc. 2006;3(6):535–7.
Gwilt CR, Donnelly LE, Rogers DF. The non-neuronal cholinergic system in the airways: an unappreciated regulatory role in pulmonary inflammation? Pharmacol Ther. 2007;115(2):208–22.
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–44.
Punturieri A, Szabo E, Croxton TL, Shapiro SD, Dubinett SM. Lung cancer and chronic obstructive pulmonary disease: needs and opportunities for integrated research. J Natl Cancer Inst. 2009;101(8):554–9.
Qian Q, Shi X, Lei Z, Zhan L, Liu RY, Zhao J, Yang B, Liu Z, Zhang HT. Methylated +58CpG site decreases DCN mRNA expression and enhances TGF-beta/Smad signaling in NSCLC cells with high metastatic potential. Int J Oncol. 2014;44(3):874–82.
Lourenco RV, Loddenkemper R, Carton RW. Patterns of distribution and clearance of aerosols in patients with bronchiectasis. Am Rev Respir Dis. 1972;106(6):857–66.
Yang P, Wentzlaff KA, Katzmann JA, Marks RS, Allen MS, Lesnick TG, Lindor NM, Myers JL, Wiegert E, Midthun DE, et al. Alpha1-antitrypsin deficiency allele carriers among lung cancer patients. Cancer Epidemiol Biomark Prev. 1999;8(5):461–5.
Marciniak SJ, Lomas DA. What can naturally occurring mutations tell us about the pathogenesis of COPD? Thorax. 2009;64(4):359–64.
Muller KC, Welker L, Paasch K, Feindt B, Erpenbeck VJ, Hohlfeld JM, Krug N, Nakashima M, Branscheid D, Magnussen H, et al. Lung fibroblasts from patients with emphysema show markers of senescence in vitro. Respir Res. 2006;7:32.
Tisi GM. Preoperative evaluation of pulmonary function. Validity, indications, and benefits. Am Rev Respir Dis. 1979;119(2):293–310.
Sekine Y, Behnia M, Fujisawa T. Impact of COPD on pulmonary complications and on long-term survival of patients undergoing surgery for NSCLC. Lung Cancer. 2002;37(1):95–101.
Takahashi Y, Matsuda M, Aoki S, Dejima H, Nakayama T, Matsutani N, Kawamura M. Qualitative analysis of preoperative high-resolution computed tomography: risk factors for pulmonary complications after major lung resection. Ann Thorac Surg. 2016;101(3):1068–74.
Bafadhel M, Umar I, Gupta S, Raj JV, Vara DD, Entwisle JJ, Pavord ID, Brightling CE, Siddiqui S. The role of CT scanning in multidimensional phenotyping of COPD. Chest. 2011;140(3):634–42.
Kim SS, Seo JB, Lee HY, Nevrekar DV, Forssen AV, Crapo JD, Schroeder JD, Lynch DA. Chronic obstructive pulmonary disease: lobe-based visual assessment of volumetric CT by using standard images--comparison with quantitative CT and pulmonary function test in the COPDGene study. Radiology. 2013;266(2):626–35.
Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007;370(9589):786–96.
Asamura H, Naruke T, Tsuchiya R, Goya T, Kondo H, Suemasu K. What are the risk factors for arrhythmias after thoracic operations? A retrospective multivariate analysis of 267 consecutive thoracic operations. J Thorac Cardiovasc Surg. 1993;106(6):1104–10.
Curtis JJ, Parker BM, McKenney CA, Wagner-Mann CC, Walls JT, Demmy TL, Schmaltz RA. Incidence and predictors of supraventricular dysrhythmias after pulmonary resection. Ann Thorac Surg. 1998;66(5):1766–71.
Harpole DH, Liptay MJ, DeCamp MM Jr, Mentzer SJ, Swanson SJ, Sugarbaker DJ. Prospective analysis of pneumonectomy: risk factors for major morbidity and cardiac dysrhythmias. Ann Thorac Surg. 1996;61(3):977–82.
Fry DL, Hyatt RE. Pulmonary mechanics. A unified analysis of the relationship between pressure, volume and gasflow in the lungs of normal and diseased human subjects. Am J Med. 1960;29:672–89.
Schulman LL, Lennon PF, Wood JA, Enson Y. Pulmonary vascular resistance in emphysema. Chest. 1994;105(3):798–805.
Bankier AA, De Maertelaer V, Keyzer C, Gevenois PA. Pulmonary emphysema: subjective visual grading versus objective quantification with macroscopic morphometry and thin-section CT densitometry. Radiology. 1999;211(3):851–8.
Hersh CP, Washko GR, Jacobson FL, Gill R, Estepar RS, Reilly JJ, Silverman EK. Interobserver variability in the determination of upper lobe-predominant emphysema. Chest. 2007;131(2):424–31.
Maisonneuve P, Bagnardi V, Bellomi M, Spaggiari L, Pelosi G, Rampinelli C, Bertolotti R, Rotmensz N, Field JK, Decensi A, et al. Lung cancer risk prediction to select smokers for screening CT--a model based on the Italian COSMOS trial. Cancer Prev Res (Phila). 2011;4(11):1778–89.
Acknowledgements
Not applicable.
Funding
The authors declare that no funding was received for this study.
Availability of data and materials
Datasets analyzed for this study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
SS has been involved in collection and assembly of data, data analysis and interpretation, and manuscript writing. MN, YS, TG, TK, and TM have been involved in collection and assembly of data and data analysis. SS, YS, and HI have been involved in analysis of the CT examinations. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures were performed in accordance with Helsinki declaration. This study was approved by the ethics committee of Niigata University on August 2nd, 2018 and is known under reference number 2018–0133. Written informed consents were obtained from all patients before surgery. In this study, the requirement for informed consent was waived because this was a retrospective study according to the Ethical Guidelines for Medical and Health Research Involving Human Subjects of Ministry of Health, Labour and Welfare of Japan. All participants were provided opportunities to decline participation in the study prior to the present investigation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Sato, S., Nakamura, M., Shimizu, Y. et al. The impact of emphysema on surgical outcomes of early-stage lung cancer: a retrospective study. BMC Pulm Med 19, 73 (2019). https://doi.org/10.1186/s12890-019-0839-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-019-0839-1