Abstract
Background
Asbestosis and silicosis are progressive pneumoconioses characterized by interstitial fibrosis following exposure to asbestos or silica dust. We evaluated the potential diagnostic biomarkers for these diseases.
Methods
The serum concentrations of Krebs von den Lungen-6 (KL-6), surfactant protein D (SP-D), and matrix metalloproteinase-2 (MMP-2), MMP-7, and MMP-9 were measured in 43 patients with asbestosis, 45 patients with silicosis, 40 dust-exposed workers (DEWs) without pneumoconiosis, and 45 healthy controls (HCs). Chest high-resolution computed tomography (HRCT) images were reviewed by experts blinded to the clinical data. According to the receiver operating characteristic (ROC) curve, the ideal level of each biomarker and its diagnostic sensitivity were obtained.
Results
The serum KL-6 and MMP-2 concentrations were highest in patients with asbestosis, particularly in comparison with those in DEWs and HCs (P<0.05). The serum SP-D concentration was significantly higher in patients with asbestosis than in patients with silicosis, DEWs, and HCs (P<0.01), whereas no significant difference was noted among patients with silicosis, DEWs, and HCs. No significant difference in the serum MMP-7 or -9 concentration was found among patients with asbestosis, patients with silicosis, DEWs, or HCs. Among patients with asbestosis, the serum KL-6 concentration was significantly correlated with the lung fibrosis scores on HRCT and negatively correlated with the forced vital capacity (FVC) % predicted and diffusing capacity of the lung for carbon monoxide (DLCO) % predicted. The serum SP-D and MMP-2 concentrations were negatively correlated with the DLCO % predicted (all P<0.05). The order of diagnostic accuracy according to the ROC curve was KL-6, SP-D, and MMP-2 in patients with asbestosis alone and in the combination of both patients with asbestosis and those with silicosis. The combination of all three biomarkers may increase the possibility of diagnosing asbestosis (sensitivity, 93%; specificity, 57%) and both asbestosis and silicosis (sensitivity, 83%; specificity, 62%).
Conclusions
KL-6, SP-D, and MMP-2 are available biomarkers for the adjuvant diagnosis of asbestosis and silicosis. The combination of all three biomarkers may improve the diagnostic sensitivity for asbestosis and silicosis.
Similar content being viewed by others
Background
Asbestosis and silicosis are progressive pneumoconioses characterized by interstitial fibrosis following exposure to asbestos or silica dust. Disease progression usually leads to irreversible complications and death. Clinical detection and diagnosis of asbestosis and silicosis mainly relies on a history of occupational exposure and radiological abnormalities [1, 2]. China, where the asbestos and silica exposure industries have not been greatly limited, has invariably exhibited a sustained epidemic of asbestosis and silicosis [3, 4]. Biomarkers with which to detect these pneumoconioses other than imaging and lung function testing are warranted [5]. Krebs von den Lungen 6 (KL-6), surfactant protein D (SP-D), and matrix metalloproteinases (MMPs) are potential biomarkers for diagnosing and monitoring progression of various fibrotic lung diseases.
KL-6, classified in humans as mucin, is a circulating high-molecular-weight glycoprotein [6]. KL-6 has served as a useful biomarker in the differential diagnosis of various chronic lung fibroses and pulmonary alveolar proteinosis, evaluation of disease activity, and prediction of disease outcome [6,7,8,9,10]. The regenerating type II pneumocytes can be positively stained by the KL-6 monoclonal antibody in the lung tissue of patients with lung fibrosis [6, 7]. KL-6 is detectable in both the serum and bronchoalveolar lavage fluid of patients with lung fibrosis [6].
SP-D, which belongs to the collecting subgroup of the C-type lectin superfamily, is produced by two types of nonciliated epithelial cells in the peripheral airway (alveolar type II cells and Clara cells) and is secreted into the alveolar space [11]. It functions at the air–liquid interface to reduce surface tension and thereby prevent alveolar collapse and atelectasis; it also plays important roles in the innate immune system of the lungs [12]. The serum concentration of SP-D can reflect the pathological changes of lungs affected by idiopathic pulmonary fibrosis (IPF) by migration from the air space into the bloodstream [11].
In addition to type II pneumocyte-derived biomarkers, MMPs can degrade extracellular matrix components and numerous nonmatrix proteins [13]. MMPs and their inhibitors, tissue inhibitors of MMPs, have been implicated in the pathogenesis of pulmonary fibrosis based upon the results of clinical studies that showed elevated levels of MMPs in both blood and/or lung samples, indicating that they can serve as potential diagnostic and prognostic markers of chronic lung fibrosis [14,15,16,17].
Several biomarkers, such as interleukin-1β, type IV collagen, tumor necrosis factor-α, neopterin, and proteomic profiling, have shown potential significance in patients with lung fibrosis [18,19,20,21]. However, no previous investigations have evaluated the diagnostic values of pneumocyte-derived biomarkers in various pneumoconioses. To clarify the potential diagnostic biomarkers for asbestosis and silicosis, we measured the serum concentrations of KL-6, SP-D, and MMP-2, -7, and -9 in discriminating patients with asbestosis and silicosis from dust-exposed workers (DEWs) without pneumoconiosis and healthy controls (HCs).
Methods
A case–control study of patients with asbestosis, patients with silicosis, DEWs without pneumoconiosis, and HCs was conducted using a sandwich-type electrochemiluminescence immunoassay (ECLIA) or commercially available enzyme-linked immunosorbent assay (ELISA) to detect the serum concentrations of KL-6, SP-D, and MMP-2, -7, and -9. All participants underwent chest X-ray and/or chest high-resolution computed tomography (HRCT) and pulmonary function testing. The study was approved by the Institutional Ethics Committee for Human Research, Beijing Chao-Yang Hospital. Informed consent was obtained from all participants before blood sample collection.
Patients’ characteristics
In total, 43 outpatients with newly diagnosed asbestosis, 45 with silicosis and 40 dust-exposed workers (DEWs) without pneumoconiosis were sequentially recruited from the Department of Occupational Medicine and Toxicology, Beijing Chao-Yang Hospital, during a 2-year period (January 2015 to December 2016). All patients were diagnosed according to the diagnostic criteria of pneumoconiosis based on the 2011 International Labour Organization classification [22]. Patients with bronchial asthma, tuberculosis, autoimmune disease, severe liver and kidney dysfunction, and malignant tumors were excluded.
Forty DEWs, including 19 coal mine workers, 7 sand moulding workers, 5 jade polishers, 4 asbestos textile workers, and 5 boiler maintenance workers, had occupational exposure to silica or asbestos dust. They underwent all examinations without showing evidence of a pneumoconiosis.
The HCs comprised 45 age-, sex-, and smoking status-matched healthy volunteers from the health examination center of Beijing Chao-yang Hospital during the same period of time.
All participants’ smoking status was carefully determined, and they were categorized as non-smokers, ex-smokers (had quit smoking ≥12 months previously), and smokers (currently smoking or had quit smoking <12 months previously). Cigarette smoking is shown by pack-years.
Occupational dust exposure
All participants completed a standardized questionnaire to collect information on their work history. All jobs within the participant’s working life were taken into account. The 43 patients with asbestosis were local residents who had been exposed to chrysotile dust or fibers, including 36 (83.7%) involved in the manufacture of asbestos textiles or asbestos-based products and 7 (16.3%) exposed to asbestos products in a working atmosphere (e.g., heat insulation workers and boiler maintenance workers). The 45 patients with silicosis were local residents who had been exposed to silica dust in the processing of jade. The asbestos product plants were open from the 1950s to 1970s, and the jade-processing factories were open from the 1970s to 1990s. Our hospital is the largest center for evaluation of occupational diseases in the city and is located 20 to 30 km away from the plants.
Because of the absence of atmospheric measurements and the lack of detailed information on the frequency of exposure for each job suspected to be associated with asbestos exposure, the duration of asbestos exposure (number of years) was determined.
Measurements of KL-6, SP-D, and MMP-2, -7, and -9 concentrations
The serum samples were collected from each participant and stored at −80°C until serum analysis. All samples were measured within two weeks of the storage. The serum KL-6 concentration was measured by ECLIA using a Lumipulse G1200 Analyzer (Rebio, Fuji, Japan). The serum SP-D and MMP-2, -7, and -9 concentrations were measured by commercially available ELISA kits (RayBiotech, Norcross, GA, USA).
Pulmonary function tests
Pulmonary function tests were performed according to the guidelines of the hospital physiology laboratory. Parameters used for analysis of the flow–volume curve were the forced vital capacity (FVC), forced expired volume in the first second (FEV1), and FEV1/FVC ratio. Each participant also underwent evaluation of their total lung capacity and diffusing capacity of the lung for carbon monoxide (DLCO SB) (single-breath method, with the values corrected for the present hemoglobin concentration). The results are expressed as percentages of predicted values on the basis of age, height, and sex using equations established by the European Respiratory Society [23]. The forced expiratory maneuvers were repeated until three sequential measurements were obtained. The indices were obtained from the best curve, which was associated with the highest value of FEV1 plus FVC.
Lung fibrosis scores on HRCT
HRCT scans in the patients with asbestosis were performed with 0.625-mm sections, a 1-second scan time, and a 10-mm interval in the apex base scans with inclusion of both lungs in the field of view. The HRCT images were reviewed by two experts blinded to the patients’ clinical data. Two experts scored the HRCT images, which comprised three images taken at the level of the aortic arch, carina, and 1 cm above the diaphragm. Each lung lobe was scored on a scale of 0 to 5 for interstitial abnormalities according to a previously described protocol [24]. The HRCT score for each patient was the sum of the five lung lobes and ranged from 1 to 25. The final score was the mean of the scores from the two experts. The interobserver correlation was good. The kappa coefficient for the correlation between the patterns was 0.742 (P=0.006).
Conventional chest radiographs were performed in each patient with silicosis and independently evaluated by two occupational medicine experts according to the International Labour Organization classification [22]. Briefly, the lung fields were divided into six zones on the posterior chest radiograph. When the highest density of small opacities was ≥1/0 and the distribution affected two or more zones, the patients were classified into Stage I. When the highest density of small opacities was ≥2/1 and the distribution affected more than four zones, or the highest density of small opacities was ≥3/2 and the distribution affected four or more zones, the patients were classified into Stage II. When the highest density of small opacities was ≥3/2 and the distribution affected four or more zones with aggregation of small or large opacities, or the diameter of the largest opacity was ≥20 × 10 mm, the patients were classified into Stage III. The interobserver correlation was good. The kappa coefficient for the correlation between the patterns was 0.653 (P=0.009).
Statistical analysis
The results are expressed as mean ± standard deviation, and the differences among the four groups were tested using the Kruskal–Wallis test or one-way analysis of variance. Counting data were analyzed using the chi-square test. Correlations between parameters were assessed by Pearson’s correlation coefficient. The levels of serum biomarkers were further analyzed by a receiver operating characteristic (ROC) curve to determine the cut-off levels that resulted in the optimal diagnostic accuracy for each marker between the patients and controls. The use of these cut-off levels allowed for calculation of the sensitivity, specificity, and likelihood ratio of the biomarkers for separating the patients from the controls. Statistical analyses were performed using SPSS version 17.0 for Windows (SPSS Inc., Chicago, IL, USA). A P value of <0.05 was considered statistically significant.
Results
Demographics of the participants
The demographics of each participant group are summarized in Table 1. There was no significant difference in sex, age, or smoking status among the groups. However, the pulmonary function values, including the FEV1/FVC ratio, the predicted percentages of FEV1 and DLCO, showed significant differences among the groups.
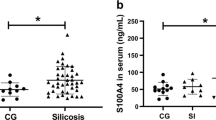
Serum concentrations of KL-6, SP-D, and MMP-2, -7, and -9
As shown in Fig. 1, the serum KL-6 and MMP-2 concentrations were highest in patients with asbestosis and second highest in patients with silicosis; these concentrations were significantly different from those in DEWs and HCs (P<0.05). The serum SP-D concentration was significantly higher in patients with asbestosis than in patients with silicosis, DEWs, or HCs (P<0.01), whereas no significant difference was found among patients with silicosis, DEWs, and HCs. No significant differences were found in the serum MMP-7 or -9 concentration among patients with asbestosis, patients with silicosis, DEWs, and HCs. The serum concentrations of KL-6, SP-D, and MMP-2 were not significantly different among the various stages of silicosis (Table 2).
Correlations between the KL-6, SP-D, and MMP-2 concentrations and clinical parameters in patients with asbestosis
As shown in Fig. 2, the serum KL-6 concentration was positively correlated with the lung fibrosis scores on HRCT in the patients with asbestosis while negatively correlated with the FVC % predicted and DLCO % predicted (P<0.05). The serum SP-D and MMP-2 concentration was also negatively correlated with the DLCO % predicted (P<0.05).
ROC curve analysis for identification of asbestosis or asbestosis and silicosis
ROC curve analysis was used to evaluate the ability of the serum KL-6, SP-D, and MMP-2 concentrations to differentiate patients with asbestosis from patients with silicosis, DEWs and HCs or asbestosis and silicosis from DEWs and HCs (Table 3). The area under the curve (AUC) for KL-6 was larger than that for SP-D and MMP-2 (Fig. 3), indicating that the order of diagnostic accuracy by the ROC curve was KL-6, SP-D, and MMP-2 in patients with asbestosis alone or in both patients with asbestosis and those with silicosis. The sensitivity and specificity of the combination of all three biomarkers for the diagnosis of asbestosis were 93% and 57%, respectively; however, they were 83% and 62% for the diagnosis of both asbestosis and silicosis.
Discussion
In the present study, we showed that the diagnostic value of the serum biomarkers KL-6, SP-D, and MMP-2 was higher in patients with asbestosis or patients with silicosis than in DEWs and HCs. In patients with asbestosis, the serum KL-6 concentration was significantly correlated with the lung fibrosis scores on HRCT while negatively correlated with the FVC % predicted and DLCO % predicted. In addition, the serum SP-D and MMP-2 concentrations were negatively correlated with the DLCO % predicted in patients with asbestosis. The order of diagnostic accuracy according to the ROC curve was KL-6, SP-D, and MMP-2 in patients with asbestosis alone and in patients with asbestosis plus those with silicosis. The combination of KL-6, SP-D, and MMP-2 may improve the diagnostic sensitivity for asbestosis and silicosis.
KL-6 is mainly localized in the cytoplasm and membrane of alveolar type II epithelial cells and bronchial epithelial cells [7]. KL-6 is also expressed in the cytoplasm of Clara cells and in bronchial glands [7]. KL-6 can promote the proliferation and migration of fibroblasts, inhibit cell apoptosis, and increase the development of pulmonary fibrosis [25]. The proliferation of type II alveolar epithelial cells in dust-related lung fibroses such as asbestosis or silicosis may release KL-6 into the peripheral blood, resulting in a significantly elevated serum KL-6 concentration. An increased concentration of KL-6 in the epithelial lining fluid may stimulate fibrotic processes in patients with interstitial lung diseases and raise the possibility of the need for treatment with anti-KL-6 antibodies [26]. The serum KL-6 concentration in patients with interstitial lung diseases reflects the overall extent of interstitial lesions and serves as a powerful predictor of acute exacerbations of IPF [27, 28]. In the present study, KL-6 was higher with diagnostic value in both patients with asbestosis and patients with silicosis than in DEWs and HCs.
SP-D is also a type II pneumocyte-derived biomarker. SP-D plays an important role in lung innate immunity [29], and its serum concentration reflects the severity and prognosis of interstitial lung diseases [30, 31]. SP-A and SP-D are very similar in terms of structure and function. However, evaluation of their hydrophilicity suggests that SP-D migrates into the blood more easily than does SP-A in patients with IPF [11]. SP-D may more easily leak into the bloodstream, whereas SP-A remains bound to surfactant lipids in the alveolar space. Previous data have suggested that the serum SP-D concentration may more accurately reflect pathological changes in IPF-affected lungs than the serum SP-A concentration [11]. The present data show that the SP-D concentrations in patients with asbestosis were significantly higher than those in patients with silicosis, DEWs, or HCs. Our results indicate that the serum SP-D concentration might be an effective biomarker of asbestosis.
MMPs are a family of endopeptidases that can degrade several components of the extracellular matrix and control the activity of several proteins that function in immunity; damage, repair, and remodeling of collagen; and fibrosis [13]. The levels of MMP-7 and MMP-9 in both serum and bronchoalveolar lavage fluid are significantly higher in patients with IPF than in healthy controls [32]. MMP-2, -7, and -9 have also been shown to be upregulated in the lungs in patients with IPF, particularly in alveolar macrophages, hyperplastic epithelial cells, and myofibroblasts [14, 32, 33]. Elevated serum MMP-7 concentrations are correlated with severe lung fibrosis and poorer survival in patients with IPF [34]. Our data failed to show the diagnostic value of the serum MMP-7 and -9 concentrations in patients with asbestosis and in those with silicosis compared with DEWs and HCs, but our data did show the diagnostic value of the MMP-2 concentration. This finding may suggest that MMPs have different roles between dust-related fibrotic lung diseases and IPF.
The typical radiological abnormalities associated with asbestosis are pulmonary fibrosis and pleural plaques [35]. Like other pulmonary fibrotic diseases, asbestosis can be evaluated by the lung fibrosis scores on HRCT to describe the degree of pulmonary fibrosis [36]. As in patients with IPF, our data showed that the serum KL-6 concentration was correlated with the extent of diffuse fibrosis in patients with asbestosis; however, it was not correlated with the density in patients with nodular fibrosis. The serum KL-6 concentration was significantly correlated with lung fibrosis scores on HRCT, indicating the use of KL-6 in the evaluation of pulmonary fibrosis. In the analysis of the KL-6, SP-D, and MMP-2 concentrations and pulmonary function in patients with asbestosis, a higher serum KL-6 concentration was significantly negatively correlated with the FVC % predicted and DLCO % predicted, suggesting that high expression of KL-6 is associated with decreased pulmonary ventilation function and diffusion function in patients with asbestosis. The serum SP-D and MMP-2 concentrations were negatively correlated with DLCO % predicted, indicating impairment of pulmonary diffusion function [37, 38]. The ROC curve analysis showed that the area under the curve of KL-6 was the largest, indicating that it is more effective than SP-D and MMP-2 in the diagnosis of asbestosis or silicosis. The sensitivity of the combination of all three biomarkers was higher than that of any single serum marker. Therefore, the combination of KL-6, SP-D, and MMP-2 can improve the sensitivity of diagnosis of asbestosis and silicosis.
Some limitations of this study should be mentioned. First, we could not continuously monitor the biomarker concentrations in every patient to evaluate the dynamic changes in the progression of asbestosis and silicosis. In addition, other biomarkers may be effective for monitoring and evaluating disease progression and prognosis.
Conclusions
This study showed that KL-6, SP-D, and MMP-2 are readily available biomarkers for the adjuvant diagnosis of asbestosis and silicosis. The combination of all three biomarkers may improve the sensitivity of differentiating patients with asbestosis or silicosis from DEWs or HCs. Further study is warranted to justify KL-6, SP-D and MMP-2 as confirmation of early occupational lung fibrosis in the workers exposure to dusts for the possibility of intervention or prevention of the diseases.
Abbreviations
- AUC:
-
The area under the curve
- DEWs:
-
Dust-exposed workers
- DLCO :
-
Diffusing capacity of the lung for carbon monoxide
- ECLIA:
-
Electrochemiluminescence immunoassay
- ELISA:
-
Enzyme-linked immunosorbent assay
- FEV1 :
-
Forced expired volume in the first second
- FVC:
-
Forced vital capacity
- HCs:
-
Healthy controls
- HRCT:
-
High-resolution computed tomography
- IPF:
-
Idiopathic pulmonary fibrosis
- KL-6:
-
Krebs von den Lungen-6
- MMP:
-
Matrix metalloproteinase
- ROC:
-
Receiver operating characteristic
- SP-D:
-
Surfactant protein D
References
Leong SL, Zainudin R, Kazan-Allen L, Robinson BW. Asbestos in Asia. Respirology. 2015;20(4):548–55.
Castranova V, Vallyathan V. Silicosis and coal workers' pneumoconiosis. Environ Health Perspect. 2000;108(Suppl 4):675–84.
Courtice MN, Lin S, Wang X. An updated review on asbestos and related diseases in China. Int J Occup Environ Health. 2012;18(3):247–53.
Zhang M, Wang D, Zheng YD, XY DU, Chen SY. Analyses on the characteristics and the trends of pneumoconiosis notified between 1997 and 2009 in China. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2013;31(5):321–34.
Pandey JK, Agarwal D. Biomarkers. A potential prognostic tool for silicosis. Indian J Occup Environ Med. 2012;16:101–7.
Takahashi T, Munakata M, Suzuki I, Kawakami Y. Serum and bronchoalveolar fluid KL-6 levels in patients with pulmonary alveolar proteinosis. Am J Respir Crit Care Med. 1998;158, 1294:–8.
Ohnishi H, Yokoyama A, Kondo K, Hamada H, Abe M, Nishimura K, Hiwada K, Kohno N. Comparative study of KL-6, surfactant protein-A, surfactant protein-D, and monocyte chemoattractant protein-1 as serum markers for interstitial lung diseases. Am J Respir Crit Care Med. 2002;165:378–81.
Yokoyama A, Kohno N, Hamada H, Sakatani M, Ueda E, Kondo K, Hirasawa Y, Hiwada K. Circulating KL-6 predicts the outcome of rapidly progressive idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1998;158:1680–4.
Satoh H, Kurishima K, Ishikawa H, Ohtsuka M. Increased levels of KL-6 and subsequent mortality in patients with interstitial lung diseases. J Intern Med. 2006;260:429–34.
Yamakawa H, Hagiwara E, Kitamura H, Yamanaka Y, Ikeda S, Sekine A, Baba T, Okudela K, Iwasawa T, Takemura T, Kuwano K, Ogura T. Serum KL-6 and surfactant protein-D as monitoring and predictive markers of interstitial lung disease in patients with systemic sclerosis and mixed connective tissue disease. J Thorac Dis. 2017;9(2):362–71.
Nishikiori H, Chiba H, Ariki S, Kuronuma K, Otsuka M, Shiratori M, Ikeda K, Watanabe A, Kuroki Y, Takahashi H. Distinct compartmentalization of SP-A and SP-D in the vasculature and lungs of patients with idiopathic pulmonary fibrosis. BMC Pulm Med. 2014;14:196.
Takahashi H, Sano H, Chiba H, Kuroki Y. Pulmonary surfactant proteins A and D: innate immune functions and biomarkers for lung diseases. Curr Pharm Des. 2006;12(5):589–98.
Craig VJ, Zhang L, Hagood JS, Owen CA. Matrix metalloproteinases as therapeutic targets for idiopathic pulmonary fibrosis. Am J Respir Cell Mol Biol. 2015;53(5):585–600.
Selman M, Ruiz V, Cabrera S, Segura L, Ramirez R, Barrios R, Pardo A. TIMP-1, -2, -3, and -4 in idiopathic pulmonary fibrosis: a prevailing nondegradative lung microenvironment? Am J Physiol Lung Cell Mol Physiol. 2000;279:L562–74.
Morais A, Beltrão M, Sokhatska O, Costa D, Melo N, Mota P, Marques A, Delgado L. Serum metalloproteinases 1 and 7 in the diagnosis of idiopathic pulmonary fibrosis and other interstitial pneumonias. Respir Med. 2015;109:1063–8.
Zuo F, Kaminski N, Eugui E, Allard J, Yakhini Z, Ben-Dor A, Lollini L, Morris D, Kim Y, DeLustro B, et al. Gene expression analysis reveals matrilysin as a key regulator of pulmonary fibrosis in mice and humans. Proc Natl Acad Sci USA. 2002;99:6292–7.
Henry MT, McMahon K, Mackarel AJ, Prikk K, Sorsa T, Maisi P, Sepper R, Fitzgerald MX, O’Connor CM. Matrix metalloproteinases and tissue inhibitor of metalloproteinase-1 in sarcoidosis and IPF. Eur Respir J. 2002;20:1220–7.
Prince P, Boulay ME, Pagé N, Desmeules M, Boulet LP. Induced sputum markers of fibrosis and decline in pulmonary function in asbestosis and silicosis: a pilot study. Int J Tuberc Lung Dis. 2008;12:813–9.
Jiang PR, Cao Z, Qiu ZL, Pan JW, Zhang N, Wu YF. Plasma levels of TNF-α and MMP-9 in patients with silicosis. Eur Rev Med Pharmacol Sci. 2015;19:1716–20.
Pingle SK, Tumane RG, Jawade AA. Neopterin: Biomarker of cell-mediated immunity and potent usage as biomarker in silicosis and other occupational diseases. Indian J Occup Environ Med. 2008;12:107–11.
Miao R, Ding B, Zhang Y, Xia Q, Li Y, Zhu B. Proteomic profiling change during the early development of silicosis disease. J Thorac Dis. 2016;8:329–41.
International Labour Office. International Classification of Radiographs of Pneumoconiosis, revised. Occupational Safety and Health Series. 2011;22:Rev 2011.
Cotes JE, Chinn DJ, Quanjer PH, Roca J, Yernault JC. Standardization of the measurement of transfer factor (diffusing capacity), report working party standardization of lung function tests, European Community for steel and coal: official statement of the European Respiratory Society. Eur Respir J. 1993;6:41–53.
Kazerooni EA, Martinez FJ, Flint A, Jamadar DA, Gross BH, Spizarny DL, Cascade PN, Whyte RI, Lynch JP 3rd, Toews G. Thin-section CT obtained at 10-mm increments versus limited three-level thin-section CT for idiopathic pulmonary fibrosis: correlation with pathologic scoring. AJR Am J Roentgenol. 1997;169:977–83.
Ohshimo S, Yokoyama A, Hattori N, Ishikawa N, Hirasawa Y, Kohno N. KL-6, a human MUC1 mucin, promotes proliferation and survival of lung fibroblasts. Biochem Biophys Res Commun. 2005;338:1845–52.
Wakamatsu K, Nagata N, Kumazoe H, Oda K, Ishimoto H, Yoshimi M, Takata S, Hamada M, Koreeda Y, Takakura K, Ishizu M, Hara M, Ise S, Izumi M, Akasaki T, Maki S, Kawabata M, Mukae H, Kawasaki M. Prognostic value of serial serum KL-6 measurements in patients with idiopathic pulmonary fibrosis. Respir Investig. 2017;55:16–23.
Hu Y, Wang LS, Jin YP, Du SS, Du YK, He X, Weng D, Zhou Y, Li QH, Shen L, Zhang F, Su YL, Sun XL, Ding JJ, Zhang WH, Cai HR, Dai HP, Dai JH, Li HP. Serum Krebs von den Lungen-6 level as a diagnostic biomarker for interstitial lung disease in Chinese patients. Clin Respir J. 2017;11(3):337–45.
Kishaba T, Shimaoka Y, Fukuyama H, Yoshida K, Tanaka M, Yamashiro S, Tamaki H. A cohort study of mortality predictors and characteristics of patients with combined pulmonary fibrosis and emphysema. BMJ Open. 2012;15:2(3).
Ariki S, Nishitani C, Kuroki Y. Diverse functions of pulmonary collectins in host defense of the lung. J Biomed Biotechnol. 2012;2012:532071.
Takahashi H, Fujishima T, Koba H, Murakami S, Kurokawa K, Shibuya Y, Hiratori M, Kuroki Y, Abe S. Serum surfactant proteins A and D as prognostic factors in idiopathic pulmonary fibrosis and their relationshipto disease extent. Am J Respir Crit Care Med. 2000;162(3 Pt 1):1109–14.
Greene KE, King TE Jr, Kuroki Y, Bucher-Bartelson B, Hunninghake GW, Newman LS, Nagae H, Mason RJ. Serum surfactant proteins-A and -D as biomarkers in idiopathic pulmonary fibrosis. Eur Respir J. 2002;19(3):439–46.
Rosas IO, Richards TJ, Konishi K, Zhang Y, Gibson K, Lokshin AE, Lindell KO, Cisneros J, Macdonald SD, Pardo A, et al. MMP1 and MMP7 as potential peripheral blood biomarkers in idiopathic pulmonary fibrosis. PLoS Med. 2008;5:e93.
Craig VJ, Polverino F, Laucho-Contreras ME, Shi Y, Liu Y, Osorio JC, Tesfaigzi Y, Pinto-Plata V, Gochuico BR, Rosas IO, et al. Mononuclear phagocytes and airway epithelial cells: novel sources of matrix metalloproteinase-8 (MMP-8) in patients with idiopathic pulmonary fibrosis. PLoS One. 2014;9:e97485.
Song JW, Do KH, Jang SJ, Colby TV, Han S, Kim DS. Blood biomarkers MMP-7 and SP-A: predictors of outcome in idiopathic pulmonary fibrosis. Chest. 2013;143(5):1422–9.
Akira M, Morinaga K. The comparison of high-resolution computed tomography findings in asbestosis and idiopathic pulmonary fibrosis. Am J Ind Med. 2016;59:301–6.
Arakawa H, Kishimoto T, Ashizawa K, Kato K, Okamoto K, Honma K, Hayashi S, Akira M. Asbestosis and other pulmonary fibrosis in asbestos-exposed workers: high-resolution CT features with pathological correlations. Eur Radiol. 2016;26:1485–92.
Yang XL, Zhu XL, Li A, Du XQ, Song YG, Ye Q. Characteristics of lung function in patients with asbestosis of different stages. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2016;34:687–90.
Gothi D, Gahlot T, Sah RB, Saxena M, Ojha UC, Verma AK, Spalgais S. Asbestos-induced lung disease in small-scale clutch manufacturing workers. Indian J Occup Environ Med. 2016;20:95–102.
Acknowledgements
We thank all patients and investigators who were involved in these studies. We express our thanks to our colleagues Yan Yongji and Ma Jing.
Funding
The work was supported by National Major Scientific and Technological Special Project for Significant New Drugs Development (2014ZX09J15104, 2014ZX09303302) and National Natural Science Foundation of China (81370159).
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
XC performed all data collection, collected and processed samples, analyzing the data and wrote the manuscript. WN, LX and QM were responsible for recruiting the patients. DX was responsible for analyzing the data. YQ contributed as primary investigator and was responsible for designing the study, recruiting the patients and writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This work was conducted at Beijing Chao-Yang Hospital with approval from the ethics committee of Beijing Chao-Yang Hospital, Capital Medical University. Informed consent was documented in writing.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Xue, C., Wu, N., Li, X. et al. Serum concentrations of Krebs von den Lungen-6, surfactant protein D, and matrix metalloproteinase-2 as diagnostic biomarkers in patients with asbestosis and silicosis: a case–control study. BMC Pulm Med 17, 144 (2017). https://doi.org/10.1186/s12890-017-0489-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-017-0489-0