Abstract
Background
The FACED score is an easy-to-use multidimensional grading system that has demonstrated an excellent prognostic value for mortality in patients with bronchiectasis. A Spanish group developed the score but no multicenter international validation has yet been published.
Methods
Retrospective and multicenter study conducted in six historical cohorts of patients from Latin America including 651 patients with bronchiectasis. Clinical, microbiological, functional, and radiological variables were collected, following the same criteria used in the original FACED score study. The vital status of all patients was determined in the fifth year of follow-up. The area under ROC curve (AUC-ROC) was used to calculate the predictive power of the FACED score for all-cause and respiratory deaths and both number and severity of exacerbations. The discriminatory power to divide patients into three groups of increasing severity was also analyzed.
Results
Mean (SD) age of 48.2 (16), 32.9% of males. The mean FACED score was 2.35 (1.68). During the follow up, 95 patients (14.6%) died (66% from respiratory causes). The AUC ROC to predict all-cause and respiratory mortality were 0.81 (95% CI: 0.77 to 0.85) 0.84 (95% CI: 0.80 to 0.88) respectively, and 0.82 (95% CI: 078–0.87) for at least one hospitalization per year. The division into three score groups separated bronchiectasis into distinct mortality groups (mild: 3.7%; moderate: 20.7% and severe: 48.5% mortality; p < 0.001).
Conclusions
The FACED score was confirmed as an excellent predictor of all-cause and respiratory mortality and severe exacerbations, as well as having excellent discriminative capacity for different degrees of severity in various bronchiectasis populations.
Similar content being viewed by others
Background
The multidimensional nature of bronchiectasis means that any analysis of a single variable is insufficient to assess its severity or prognosis [1]. Accordingly, two multidimensional scales have been published in recent years, using several different variables that are easily obtained and have a proven capacity for an accurate prognosis of mortality: the FACED score [2] and the Bronchiectasis Severity Index (BSI) [3]. Both scores have been use to assess the severity of bronchiectasis in several publications [4,5,6,7,8].
The FACED score is a simple score that consists of five dichotomized variables: age, clinical aspects (dyspnea), lung function (FEV1), microbiology (chronic bronchial infection by Pseudomonas aeruginosa), and radiological findings (number of affected lung lobes in computed tomography). This score was developed by a Spanish group in 398 patients and showed excellent internal validity in 411 additional patients. It has demonstrated an excellent power to predict mortality (both all-cause and respiratory) within 5 years of diagnosis [2]. Its longer-term prognostic capacity (up to 15 years) has been confirmed by other series of European patients [9, 10].
However, before a new score can be fully accepted and reliably applied to clinical practice, its validity must be tested in different settings on new data from an appropriately assembled sample of subjects. This process is called external validation. It is further desirable that the sample chosen for external validation is selected with the same criteria as the initial series, while including patients whose characteristics are sufficiently different to enable an evaluation of the score’s breadth of application [11].
Therefore, the primary objective of this study was to perform an external validation of the FACED score for both overall and respiratory mortality in a large group of patients outside Europe from six historical cohorts of several countries in Latin America. The secondary objective was to evaluate the FACED score’s ability to predict exacerbations and hospitalizations.
Methods
Latin America validation sample
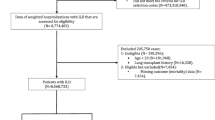
This is a retrospective and multicenter study of historical cohorts that included 672 patients from six cohorts from three different countries from Latin America (Argentina, Brazil, and Chile) with a diagnosis of bronchiectasis confirmed by high resolution computed tomography scan (HRCT scan). All data were collected from specialized bronchiectasis clinics and from patients that had at least 5 years of follow-up after the date of the radiological diagnosis of bronchiectasis. Patients were included starting from January 1, 2005. The inclusion and exclusion criteria were the same as those in the original study that constructed the FACED score, as previously published [2]. Data were also collected in all centers according to the same standardized protocol used in the FACED internal validation. The study was approved by the ethics committees of all the participating centers (Additional file 1: e-Appendix).
Description of the FACED score
The FACED score consists of five dichotomized variables: FEV1, age, presence of chronic colonization by Pseudomonas aeruginosa, dyspnea measured by the modified MRC dyspnea scale (mMRC) and number of pulmonary lobes affected on computed tomography (CT). The possible range of points is 0 to 7, with a higher score indicating greater severity of the disease. The division of the FACED score into three groups makes it possible to define bronchiectasis as mild (0–2 points), moderate (3–4 points), or severe (5–7 points) (Fig. 1).
Variables
As in the study for the construction and internal validation of FACED score, all variables were collected in a standardized manner: general characteristics (age and gender); anthropometric (body mass index [BMI]); smoking habit; symptoms (dyspnea mMRC, appearance of sputum [mucous, mucopurulent, purulent]); presence of chronic respiratory failure (room air oxygen saturation < 90%); radiological findings; etiology of bronchiectasis; colonization by potentially pathogenic microorganisms (PPM), the number of exacerbations and hospitalizations in the year prior to inclusion in the study and during the follow-up; functional variables; and treatments. According to the original FACED paper, chronic colonization was defined as isolation of the same PPM after the diagnosis of bronchiectasis in three consecutive respiratory samples taken at least one month apart within a period of six months. In view of the difference between the care system of patients in Latin America, a less restrictive definition of chronic colonization was used such as at least two isolates of a PPM 3 months apart over 1 year [12]. All the variables were collected as close as possible to the date of the diagnosis of bronchiectasis to avoid interference from different treatments.
Follow-up and end-points
The primary end-points of the study were all-cause and respiratory mortality after 5 years of follow-up from the diagnosis of bronchiectasis. The date and cause of death were confirmed by checking the centers’ digital databases and the relevant death certificates. The numbers of exacerbations and hospitalizations were also recorded during the 5 years of follow-up and these were presented as the ratio of events per year of follow-up.
Statistical analysis
The statistical analysis was the same as that used for the construction and internal validation of the FACED score [2]. Data for the quantitative variables were tabulated as mean ± SD, while the qualitative were tabulated as the percentage of the total subjects. The chi-squared test was used for comparison of qualitative and dichotomic variables. The normality of the variables was confirmed with the Kolgomorov-Smirnov test.
Less than 10% of patients had missing data and were excluded from the analysis. The baseline characteristics of these patients were not different compared with the included ones.
Data from the different centers were compared with one-way ANOVA test. The diagnostic capacity to predict all-cause and respiratory mortality and also exacerbation/hospitalization rates of the FACED score was determined by tracing their corresponding area under ROC curves (AUC-ROC) and 95% confidence interval (CI). The greater the AUC-ROC, the better the predictive value of the FACED score. An AUC-ROC greater than 0.80 was established as excellent [13]. As in the original paper, FACED score was divided into 3 groups (tertiles) with progressively increasing severity (mild, moderate and severe), and each group’s capacity to predict mortality was calculated using Kaplan-Meier method. The two-by-two comparison between the different Kaplan-Meier curves was performed with the log-rank test. Significant difference was considered when p < 0.05.
Results
Data were collected from 672 initial patients but 21 individuals were excluded (3 were under 18 years old and 18 did not present all the required variables). Finally, 651 patients were included in the analysis, and 95 of them (14.6%) died during the 5 years of follow-up. The main cause of death was related to respiratory complications (66% of cases). The general characteristics of these patients are presented in Table 1. The mean ± SD age of the overall sample was 48.2 ± 16.0 years, while 32.9% of the patients were male and 39.8% were chronically colonized by Pseudomonas aeruginosa. The most frequent known etiology of bronchiectasis was post-infective (including post-tuberculosis) in 40.3% of cases, followed by ciliary dyskinesia (9.0%). Thirty-one percent were of unknown etiology.
Table 2 presents the patients’ characteristics according to the six participating centers. Significant differences were observed in relation to their general, etiological, clinical, functional, radiological, and microbiological variables. Mortality rate ranged from 10.1% to 19.4% between centers. Table 2 also presents information about the original Spanish cohort for the FACED score, emphasizing several differences between the initial and international validation cohorts.
Figure 2a shows that the AUC ROC of the final score to predict 5-year all-cause mortality was 0.81 (95% CI: 0.77 to 0.85), p < 0.0001 and 0.84 (95% CI: 0.80 to 0.88), p < 0.0001 to predict respiratory mortality (Fig. 2b). The AUC ROC to predict all-cause mortality was calculated for each Latin American center and the observed values were higher than 0.80 in all except for one (AUC 0.78, range 0.78-0.93).
Figure 3a and b show how the division of the FACED score values into tertiles differentiated bronchiectasis into three distinct groups of increasing all-cause and respiratory mortality respectively according to the results of the Kaplan–Meier curves: mild (3.7% mortality), moderate (20.7% mortality) and severe (48.5% mortality) bronchiectasis.
Kaplan-Meier curves for all-cause mortality (a) and respiratory mortality (b) corresponding to the three bronchiectasis scoring groups. Mild: 0–2 points, Moderate: 3–4 points and Severe 5–7 points. Log-rank test (a): mild bronchiectasis versus moderate bronchiectasis 43.29, p < 0.0001; mild versus severe 138.91; p < 0.0001; and moderate versus severe 23.42, p < 0.0001. Log-rank test (b): mild bronchiectasis versus moderate bronchiectasis 28.29, p < 0.0001; mild versus severe 127.51; p < 0.0001; and moderate versus severe 28.29, p < 0.0001
Finally, to analyze the capacity of the FACED score to predict future exacerbations, we explored several scenarios based on the number and/or severity of exacerbation rates. Table 3 shows that the FACED score can predict those patients with more severe exacerbations (at least 1 hospitalization/year – AUC = 0.82 [95% CI: 0.78–0.87]) and patients with more frequent and relevant exacerbations (at least 2 exacerbations/year or 1 hospitalization/year – AUC = 0.78 [95% CI: 0.74–0.82]).
Discussion
In this study of Latin America validation of the FACED score, using the same methodology for data collection in six large historical cohorts of patients from three countries in Latin America with different clinical features and etiologies from the original cohort, the FACED score maintained an excellent power to predict all-cause and respiratory mortality. The FACED score also maintained its excellent discriminatory power by identifying a profile of increased severity in patients with bronchiectasis that was similar to that seen in the original Spanish study that constructed and internally validated this score. We also demonstrated that the score has a good capacity to predict exacerbations and hospitalizations, especially in those patients who present most severe or frequent exacerbations. These findings endorse the international clinical applicability of the FACED score as a prognostic and severity-assessment tool in patients with bronchiectasis.
There are still large gaps in our knowledge of the epidemiology and pathophysiology of bronchiectasis. The European Multicentre Bronchiectasis Audit and Research Collaboration (EMBARC) recently outlined several research priorities for improving the management of bronchiectasis [14, 15], including greater understanding of its classification and prognosis. Since there is a tendency to manage bronchiectasis based on approaches used for chronic obstructive pulmonary disease (COPD) and cystic fibrosis [16, 17], FEV1 has traditionally been used to define the severity of bronchiectasis. However, other key variables besides FEV1, such as age, quality of life, airway chronic colonization and lung volumes [18,19,20,21], have proved useful in this respect by showing a correlation with mortality in bronchiectasis. As many factors play an important role in the prognosis for bronchiectasis, just one of these on its own is obviously inadequate for predicting an outcome. For example, although CT findings are important and provide substantial information about structural abnormalities in airway diseases, CT scans are not sufficiently sensitive to detect the severity of functional impairment [22,23,24]. Furthermore, CT findings of airway diseases such as bronchial dilation or peribronchial wall thickening are not easily modifiable with treatment. However, decline in lung function also correlates with clinical parameters, the number and severity of exacerbations, and the presence of chronic colonization by P. aeruginosa, and it has been used to predict outcomes in bronchiectasis [18, 25]. Scores covering multiple variables that are validated in different populations of patients can therefore be key tools for assessing patients’ outcomes and their response to treatment. This scenario is even more complex when several comorbidities can coexist and negatively impact the prognosis of patients with bronchiectasis, as recently described by McDonnell et al [26]. Consequently, one of the prerequisites for the applicability of a multivariate score is confirmation of its external validity, i.e., its sustained ability to predict and diagnose regardless of the specific characteristics of the evaluated population. It is therefore essential to test such a score in settings different from the one in which it was first created and validated. One single-center study conducted in London by Ellis et al [9] in a small number of patients (but with a long follow-up of 19 years), and another study in Macedonia [27] both found that the FACED score had excellent predictive power. More recently, McDonnell et al [10] evaluated both the FACED and BSI scores in a large population comprising seven European cohorts and confirmed their discriminatory predictive value for mortality. However, it should be emphasized that all these studies used a European population base. Herein we present the first study to evaluate the FACED score in a group of patients with different ethnic characteristics in various Latin American countries since, as already demonstrated, ethnicity can influence several characteristics in bronchiectasis patients [28].
One of the most striking features of the FACED score is its simplicity. It is very easy to memorize by using the acronym and dichotomization of its variables (Fig. 1). This advantage increases its clinical applicability, making it useful even in the absence of digital equipment. The findings of this study confirm an excellent external validation of the FACED score for predicting both all-cause and respiratory mortality in six cohorts of patients with AUC-ROC above 0.8 from three Latin American countries. Thus, no significant deviations were found from the original prognostic power of the FACED score in the full cohort of 819 patients as regards general mortality (AUC-ROC 0.87 versus 0.81; p = 0.29) or respiratory mortality (AUC-ROC 0.85 versus 0.84; p = 0.88). The results were robust since the AUC-ROC range in the different countries was similar, and excellent in every case (range 0.78–0.93). One important aspect of this study is that the external validation was performed in patients with different characteristics from those of the original cohort. The patients included in the Latin American cohort were younger, with a greater number of affected lobes, and a higher prevalence of purulent sputum. Moreover, the Latin American patients presented worse lung function and a higher rate of chronic colonization by P. aeruginosa– all of which can interfere in bronchiectasis management [29, 30]. The external validation cohort also demonstrated a statistically significant discriminatory power with respect to the three degrees of severity (mild, moderate and severe) in patients with bronchiectasis. In this study, we were able to test an additional important use for the FACED score: its good power to predict exacerbations and hospitalizations (especially those patients with the most severe or frequent exacerbations), which are well recognized as surrogate markers of long-term unfavorable outcomes and potential target endpoints tor new treatments of bronchiectasis [31, 32].
The main limitation of this study is the fact that external validation in three Latin American countries does not guarantee the FACED score’s immediate applicability in countries with very different characteristics, such as Asian countries or the United States, where the frequency of tuberculosis etiology or non-tuberculosis mycobacteria is higher respectively [33, 34]. Validation is still required in other contexts to guarantee the worldwide applicability of the FACED score, although its validation in Latin America in patients with different clinical characteristics, as well as its validation in an English cohort with a long follow-up [9], suggests that it could also be applicable to other countries. A multidimensional score is a useful and easy-to-use tool for predicting and classifying the severity of patients, as well as for allowing comparisons between different cohorts and different treatments. The inclusion of other elements in the score that affect functional deterioration and worsen the quality of life in bronchiectasis, such as exacerbations or hospitalizations, could further strengthen the prognostic power of this instrument. However, it is essential to avoid any undue complication of the FACED score, since its simplicity is probably one of its main virtues and clearly guarantees its wide clinical applicability, especially in out-patient settings with no computers, as in the case of some Latin American centers [35]. In such situations, physicians need a usable tool that is easy to memorize, and the FACED score is ideal for this purpose. It should also be stated that, according to the nature of the retrospective studies, it is possible to occur biases in the collected information by not previous adequately completing of medical records. Such issue could have more impact in variables such as exacerbations, especially mild cases, and may be underestimated in the present study. For this reason, we prioritize hospitalization data for future risk assessment among patients with bronchiectasis in the present study.
Conclusion
In conclusion, the FACED score maintained its excellent ability to predict all-cause and respiratory mortality when tested in a Latin American population. The score’s ability to discriminate between different degrees of bronchiectasis severity was also externally validated and proved similar to the findings in the original cohort. Furthermore, we significantly enhanced the clinical relevance of the FACED score since we also demonstrated its good discriminatory capacity for predicting multiple and severe exacerbations. Further research is also required to assess its ability to predict other important outcomes, such as quality of life or decline in pulmonary function.
Abbreviations
- AUC-ROC:
-
Area under ROC curve
- BSI:
-
Bronchiectasis Severity Index
- CI:
-
confidence interval
- COPD:
-
chronic obstructive pulmonary disease
- CT:
-
computed tomography
- FEV1:
-
forced expiratory volume in 1 s
- FVC:
-
forced vital capacity
- mMRC:
-
modified Medical Research Council
- NA:
-
not applicable
- PPM:
-
potentially pathogenic microorganisms
- SD:
-
standard deviation
References
McShane PJ, Naureckas ET, Tino G, Strek ME. Non-cystic fibrosis bronchiectasis. Am J Respir Crit Care Med. 2013;188(6):647–56.
Martínez-García MA, de Gracia J, Vendrell Relat M, et al. Multidimensional approach to non-cystic fibrosis bronchiectasis: the FACED score. Eur Respir J. 2014;43(5):1357–67.
Chalmers JD, Goeminne P, Aliberti S, et al. The bronchiectasis severity index. An international derivation and validation study. Am J Respir Crit Care Med. 2014;189(5):576–85.
de la Rosa D, Martínez-Garcia MA, Olveira C, Girón R, Máiz L, Prados C. Annual direct medical costs of bronchiectasis treatment: Impact of severity, exacerbations, chronic bronchial colonization and chronic obstructive pulmonary disease coexistence. Chron Respir Dis. 2016;13(4):361–71.
Pinto EH, Longo PL, de Camargo CC, et al. Assessment of the quantity of microorganisms associated with bronchiectasis in saliva, sputum and nasal lavage after periodontal treatment: a study protocol of a randomised controlled trial. BMJ Open. 2016;6(4):e010564.
Dente FL, Bilotta M, Bartoli ML, et al. Neutrophilic Bronchial Inflammation Correlates with Clinical and Functional Findings in Patients with Noncystic Fibrosis Bronchiectasis. Mediators Inflamm. 2015;2015:642503.
Guan WJ, Gao YH, Xu G, et al. Impulse oscillometry in adults with bronchiectasis. Ann Am Thorac Soc. 2015;12(5):657–65.
Guan WJ, Gao YH, Xu G, et al. Bronchodilator response in adults with bronchiectasis: correlation with clinical parameters and prognostic implications. J Thorac Dis. 2015;2015:642503.
Ellis HC, Cowman S, Fernandes M, Wilson R, Loebinger MR. Predicting mortality in bronchiectasis using bronchiectasis severity index and FACED scores: a 19-year cohort study. Eur Respir J. 2016;47(2):482–9.
McDonnell MJ, Aliberti S, Goeminne PC et al. Multidimensional severity assessment in bronchiectasis: an analysis of seven European cohorts. Thorax. 2016
Steyerberg E. Clinical prediction models: a practical approach to development, validation, and updating. New York, NY: Springer; 2010. p. 255–80.
Pasteur MC. Bilton D, Hill AT, British Thoracic Society Bronchiectasis Non-CF Guideline Group. British Thoracic Society guideline for non-CF bronchiectasis. Thorax. 2010;65:i1–i58.
Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36.
Aliberti S, Masefield S, Polverino E, et al. Research priorities in bronchiectasis: a consensus statement from the EMBARC Clinical Research Collaboration. Eur Respir J. 2016;48(3):632–47.
Poppelwell L, Chalmers JD. Defining severity in non-cystic fibrosis bronchiectasis. Expert Rev Respir Med. 2014;8(2):249–62.
Athanazio RA, Rached SZ, Rohde C, Pinto RC, Fernandes FL, Stelmach R. Should the bronchiectasis treatment given to cystic fibrosis patients be extrapolated to those with bronchiectasis from other causes? J Bras Pneumol. 2010;36(4):425–31.
Athanazio R. Airway disease: similarities and differences between asthma COPD and bronchiectasis. Clinics. 2012;67(11):1335–43.
Loebinger MR, Wells AU, Hansell DM, et al. Mortality in bronchiectasis: a long-term study assessing the factors influencing survival. Eur Respir J. 2009;34(4):843–9.
Goeminne PC, Bijnens E, Nemery B, Nawrot TS, Dupont LJ. Impact of traffic related air pollution indicators on non-cystic fibrosis bronchiectasis mortality: a cohort analysis. Respir Res. 2014;15:108.
Sehitogullari A, Bilici S, Sayir F, Cobanoglu U, Kahraman A. A long-term study assessing the factors influencing survival and morbidity in the surgical management of bronchiectasis. J Cardiothorac Sur. 2011;6:161.
Iwagami M, Mansfield K, Quint J, Nitsch D, Tomlinson L. Diagnosis of acute kidney injury and its association with in-hospital mortality in patients with infective exacerbations of bronchiectasis: cohort study from a UK nationwide database. BMC Pulm Med. 2016;16:14.
Edwards EA, Narang I, Li A, Hansell DM, Rosenthal M, Bush A. HRCT lung abnormalities are not a surrogate for exercise limitation in bronchiectasis. Eur Respir J. 2004;24(4):538–44.
Boon M, Vermeulen FL, Gysemans W, Proesmans M, Jorissen M, De Boeck K. Lung structure-function correlation in patients with primary ciliary dyskinesia. Thorax. 2015;70(4):339–45.
Wielpütz MO, Eichinger M, Weinheimer O, et al. Automatic airway analysis on multidetector computed tomography in cystic fibrosis: correlation with pulmonary function testing. J Thorac Imaging. 2013;28(2):104–13.
Martínez-García MA, Soler-Cataluña JJ, Perpiñá-Tordera M, Román-Sánchez P, Soriano J. Factors associated with lung function decline in adult patients with stable non-cystic fibrosis bronchiectasis. Chest. 2007;132(5):1565–72.
McDonnell M, Aliberti S, Goeminne P, et al. Comorbidities and the risk of mortality in patients with bronchiectasis: an international multicentre cohort study. Lancet Respir Med. 2016;4(12):969–79.
Minov J, Karadzinska-Bislimovska J, Vasilevska K, Stoleski S, Mijakoski D. Assessment of the Non-Cystic Fibrosis Bronchiectasis Severity: The FACED Score vs the Bronchiectasis Severity Index. Open Respir Med J. 2015;31(9):46–51.
McShane PJ, Naureckas ET, Strek ME. Bronchiectasis in a diverse US population: effects of ethnicity on etiology and sputum culture. Chest. 2012;142(1):159–67.
29 – Martínez-García MA, Vendrell M, Girón R et al., The Multiple Faces of Non-Cystic Fibrosis Bronchiectasis: A Cluster Analysis Approach. Ann Am Thorac Soc. 2016. In press: doi: 10.1513/AnnalsATS.201510-678OC
Aliberti S, Lonni S, Dore S, et al. Clinical phenotypes in adult patients with bronchiectasis. Eur Respir J. 2016;47(4):1113–22.
Welsh EJ, Evans DJ, Fowler SJ, Spencer S. Interventions for bronchiectasis: an overview of Cochrane systematic reviews. Cochrane Database Syst Rev. 2015;7:CD010337.
Fan LC, Lu HW, Wei P, Ji XB, Liang S, Xu JF. Effects of long-term use of macrolides in patients with non-cystic fibrosis bronchiectasis: a meta-analysis of randomized controlled trials. BMC Infect Dis. 2015;15:160.
Lin JL, Xu JF, Qu JM. Bronchiectasis in China. Ann Am Thorac Soc. 2016;13(5):609–16.
Mirsaeidi M, Hadid W, Ericsoussi B, Rodgers D, Sadikot RT. Non-tuberculous mycobacterial disease is common in patients with non-cystic fibrosis bronchiectasis. Int J Infect Dis. 2013;17(11):e1000–4.
Atun R, de Andrade LO, Almeida G, et al. Health-system reform and universal health coverage in Latin America. Lancet. 2015;385(9974):1230–47.
Acknowledgements
We would like to thank Talita Bianchi Aiello, Alicia Benitez, Andrea Appendino and Javier Castillo for their participation in this study.
Funding
This study has received no funding.
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
RA and MAMG designed the study, contributed to data acquisition and interpretation, supervised the study, wrote the manuscript, and take the responsibility for the integrity of the work as a whole, from inception to published article. MCP, GG, FCL, MFF, SR, DR, LMC, RG, CO and CP contributed to data acquisition and interpretation, critically revised the manuscript, and approved the final version to be published.
Competing interests
No conflicts of interest exist for any of the authors.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by the ethics committees of all the participating centers (Additional file 1: e-Appendix).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
e-Appendix 1 – List of ethical committees and approval numbers. (DOCX 13 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Athanazio, R., Pereira, M.C., Gramblicka, G. et al. Latin America validation of FACED score in patients with bronchiectasis: an analysis of six cohorts. BMC Pulm Med 17, 73 (2017). https://doi.org/10.1186/s12890-017-0417-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-017-0417-3