Abstract
Background
Despite inhaled medications that decrease exacerbation risk, some COPD patients experience frequent exacerbations. We determined prospective risk factors for exacerbations among subjects in the COPDGene Study taking inhaled medications.
Methods
2113 COPD subjects were categorized into four medication use patterns: triple therapy with tiotropium (TIO) plus long-acting beta-agonist/inhaled-corticosteroid (ICS ± LABA), tiotropium alone, ICS ± LABA, and short-acting bronchodilators. Self-reported exacerbations were recorded in telephone and web-based longitudinal follow-up surveys. Associations with exacerbations were determined within each medication group using four separate logistic regression models. A head-to-head analysis compared exacerbation risk among subjects using tiotropium vs. ICS ± LABA.
Results
In separate logistic regression models, the presence of gastroesophageal reflux, female gender, and higher scores on the St. George’s Respiratory Questionnaire were significant predictors of exacerbator status within multiple medication groups (reflux: OR 1.62–2.75; female gender: OR 1.53 - OR 1.90; SGRQ: OR 1.02–1.03). Subjects taking either ICS ± LABA or tiotropium had similar baseline characteristics, allowing comparison between these two groups. In the head-to-head comparison, tiotropium users showed a trend towards lower rates of exacerbations (OR = 0.69 [95 % CI 0.45, 1.06], p = 0.09) compared with ICS ± LABA users, especially in subjects without comorbid asthma (OR = 0.56 [95 % CI 0.31, 1.00], p = 0.05).
Conclusions
Each common COPD medication usage group showed unique risk factor patterns associated with increased risk of exacerbations, which may help clinicians identify subjects at risk. Compared to similar subjects using ICS ± LABA, those taking tiotropium showed a trend towards reduced exacerbation risk, especially in subjects without asthma.
Trial registration
ClinicalTrials.gov NCT00608764, first received 1/28/2008.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
The frequency of exacerbations defines a distinct phenotype of COPD and has implications for prognosis and possibilities for intervention [1]. COPD exacerbations impact the morbidity, mortality, and clinical course of COPD [2–7]. Previous studies examined the association of COPD severity and the frequency of acute exacerbations in an effort to accurately characterize this subset of patients [1]. Additionally, chest computed tomography (CT) features such as bronchial wall thickness [8], emphysema percentage [8], and ratio of pulmonary artery diameter to aortic diameter [9] identify patients susceptible to exacerbations. These studies did not consider differences in medication use and the relationship to exacerbation frequency.
Some commonly prescribed medications have been shown to decrease the rate of exacerbations in randomized clinical trials, including tiotropium (TIO) [10] and long-acting beta-agonists/inhaled corticosteroid (ICS ± LABA) combinations [11]. The relative merits of these two therapies have been compared through a meta-analysis [12] as well as a randomized trial [13]. Although these studies have provided evidence regarding COPD treatment, there still remains a subset of patients who experience frequent exacerbations despite appropriate therapy. It is unclear what factors separate medication non-responders from those who respond more favorably to inhaled medications such as short-acting bronchodilators (SAB), ICS ± LABA, long-acting muscarinic antagonists, or combinations of these medications.
The Genetic Epidemiology of COPD Study (COPDGene, clinicaltrials.gov identifier NCT00608764) is a large observational study of smokers with and without COPD [14]. We examined the differences between COPD subjects with and without exacerbations stratified by common medication use patterns using four separate logistic regression models, analyzing risk factors within each medication usage group to minimize confounding by indication. The primary hypothesis was that unique risk factor profiles for the exacerbator phenotype would exist for subjects on different inhaled medications. In a separate head-to-head analysis, we examined the effect of tiotropium vs. long-acting beta-agonist/inhaled corticosteroids on exacerbation risk.
Methods
COPDGene is an observational study of COPD conducted at 21 clinical centers in the U.S. (see Additional file 1: Supplementary Data and Methods) designed to discover epidemiologic and genetic risk factors for COPD [8, 14, 15]. It consists of 10,192 current and former Non-Hispanic white or African-American smokers with and without COPD. Each subject underwent spirometry, inspiratory and expiratory chest CT scans, and questionnaires related to demographics, medical history, symptoms and quality of life, in addition to blood samples for genetic analysis. The Longitudinal Follow-Up (LFU) program is a prospective follow-up program [16] in COPDGene using automated telephone and web-based surveys every 3–6 months to monitor incident exacerbations, comorbidities, and death [15]. The LFU dataset (version Oct 12, 2013) used for this investigation included 8465 subjects with a mean follow-up time of 3.35 years. An exacerbation was defined as an episode of increased cough, phlegm, or shortness of breath that lasted >48 h and required treatment with antibiotics, systemic steroids, or both. Severe exacerbations required an emergency room visit or hospitalization. Asthma was defined by self-report of a doctor’s diagnosis of asthma before age 40, as previously reported [17]. The COPDGene Study was approved by Partners Healthcare institutional review board (Protocol # 2007P000554) and institutional review boards at all study sites, and written informed consent was obtained from all subjects. This study was conducted in accordance with the amended Declaration of Helsinki. The St. George's Respiratory Questionnaire was used with permission.
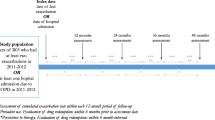
This analysis included subjects with COPD defined by a forced expiratory volume in one second (FEV1) to forced vital capacity (FVC) ratio <0.7 (GOLD stages 1–4) [18]. Subjects without LFU data and subjects not using inhaled medications were excluded, leaving 2543 subjects. Four medication usage patterns (Fig. 1) were defined at the baseline study visit: 1) Triple therapy with long-acting beta-agonist/inhaled corticosteroid and tiotropium (TIO/LABA/ICS, N = 863); 2) tiotropium alone (TIO, N = 256); 3) long-acting beta-agonists/inhaled corticosteroid or inhaled corticosteroid alone (ICS ± LABA, N = 628); 4) short-acting bronchodilator medications only (SAB, N = 366), including albuterol or ipratropium alone or in combination.
Study subjects. The COPDGene cohort was narrowed to those with LFU data available, then narrowed to subjects with a diagnosis of COPD by GOLD criteria, then to those taking medications. These subjects were divided into four exclusive groups based on medication use, as defined in the Methods section. Exacerbators had one or more exacerbations per year, non-exacerbators had zero exacerbations per year, subjects with between 0 and 1 exacerbations per year were not classified. LFU = Longitudinal follow-up; FEV1/FVC = ratio of forced expiratory volume in one second to forced vital capacity
Subjects with an exacerbation rate of one or more per year in the LFU were considered exacerbators, those with no exacerbations were considered non-exacerbators, and those with between zero and one exacerbation per year were not classified. The previously described threshold of greater than two exacerbations per year [1] resulted in an insufficient sample size for the subgroup analyses (Fig. 2). Statistical analysis was performed using R software [19].
Frequency of COPD exacerbations within the four medication groups. Medication groups are mutually exclusive. TIO/LABA/ICS indicates triple therapy with tiotropium, long-acting beta-agonist/inhaled corticosteroid, TIO indicates tiotropium alone, ICS ± LABA indicates long-acting beta-agonist/inhaled corticosteroid combination therapy, and SAB indicates short-acting bronchodilators alone
Additional methods are available in the online supplement (see Additional file 1: Supplementary Data and Methods).
Within medication group analysis
We compared exacerbators versus non-exacerbators within each medication group for differences in imaging characteristics, symptoms, comorbidities, pulmonary function tests, and demographics. Univariate analysis of binary variables was performed using chi-square statistics and continuous variables using Student's T-test. Significant prospective univariate risk factors were used to build multivariable logistic regression models including a group of common covariates (age, race, gender, FEV1 % predicted).
Head-to-head analysis
We examined the effect of tiotropium vs long-acting beta-agonist/inhaled corticosteroid on exacerbator phenotype in a logistic regression model using a combined subject pool of the TIO and ICS ± LABA medication groups, who were shown to have similar baseline characteristics. Covariates included baseline differences between the groups. The analysis was repeated after stratification for comorbid asthma.
Results
Baseline characteristics
The TIO/LABA/ICS group showed a higher percentage of subjects on oxygen therapy, shorter six minute walk test (6MWT) distance, lower FEV1, higher Modified Medical Research Council dyspnea (MMRC) score, higher total SGRQ score, higher BODE (body mass index, airflow obstruction, dyspnea, and exercise capacity) score, and greater percent emphysema and gas trapping compared to the other groups (Table 1), similar to data previously published by Park et al. [20]. In addition, they showed higher rates of exacerbations/year (1.1) and severe exacerbations/year (0.4) in LFU. These features describe a sicker population with worse functional measures, higher symptom scores, and more disease on chest CT scans.
The ICS ± LABA and TIO groups showed broad similarities in baseline characteristics (Table 2). They did not significantly differ in functional measures such as 6MWT distance and FEV1, rates of comorbidities such as GERD, nor in imaging characteristics such as emphysema and gas trapping. Several of the variables, including MMRC score, SGRQ score, and BODE score, showed small statistically significant differences that may not be clinically significant based on accepted standards. The differences in TLC (101.9 % in TIO vs. 104.3 % in ICS ± LABA) and SRWA-Pi10 (3.70 mm in TIO vs. 3.73 mm in ICS ± LABA) are also small. However, there were differences in the proportion of subjects with asthma (16.0 % in TIO vs. 39.3 % in ICS ± LABA) and the mean exacerbation rates (0.5 per year in TIO vs. 0.7 per year in ICS ± LABA). When subjects with asthma were removed, the differences in exacerbation rates, SRWA-Pi10, and SGRQ were no longer significant (see Additional file 1: Supplementary Data and Methods 1, Table S1 and S2).
The SAB group contained 366 subjects (Table 1), with the best lung function (FEV1 56.1 % predicted) and one of the lowest exacerbation rates (0.6 per year). Despite this, 148 (40 %) of SAB subjects had GOLD stage 3 or 4 disease. In addition, 80 (22 %) SAB subjects had greater than one exacerbation per year, while 31 (8.5 %) had two or more exacerbations per year. There was a higher proportion of African-Americans than in other groups, and the SAB group had the highest proportion with chronic bronchitis. Functional measurements such as 6MWT were better compared with other groups, and they had the least emphysema.
The 174 subjects on chronic oral steroids tended to have lower lung function (FEV1 39.3 % predicted) and an exacerbation rate (1.6 per year) that was comparable to other groups despite use of chronic systemic steroids. Subjects on chronic oral steroids in COPDGene have been described previously [21].
Within medication group analysis
In univariate analysis, risk factors for the exacerbator phenotype were discovered within each medication group (see Additional file 1: Supplementary Data and Methods 1, Table S3). Notable risk factors consistent across all medication groups were frequent cough symptoms and higher TLC. GERD, asthma, and higher SGRQ score were statistically significant risk factors of exacerbator status in the TIO/LABA/ICS, TIO, and ICS ± LABA groups, but not in the SAB group. The presence of chronic bronchitis and of daily phlegm symptoms were not significant predictors in subjects taking tiotropium (TIO/LABA/ICS and TIO groups), but were predictors in subjects not taking tiotropium (ICS ± LABA and SAB groups). Similarly, emphysema on CT was predictive of exacerbator phenotype only in subjects not receiving tiotropium. Bronchodilator (BD) responsiveness as measured by absolute change in FEV1 was not a significant risk factor in subjects receiving ICS ± LABA combinations (with or without TIO), but was a significant risk factor in subjects without ICS ± LABA (TIO and SAB groups). Prior venous thromboembolism, obstructive sleep apnea, higher body mass index (BMI), and congestive heart failure were not associated with exacerbator phenotype. Current smoking status was not a risk factor in any medication group, nor was lifetime smoking exposure, measured in pack-years (Additional file 1: Supplementary Data and Methods, Table S3).
Logistic regression was performed within each medication group using the significant univariate risk factors as covariates, in addition to age, race, sex, and FEV1 (Table 3). Risk factors of female gender, higher SGRQ score, prior pneumonia, and GERD remained significant in the TIO/LABA/ICS group, while the presence of co-morbid asthma showed a trend towards significance. Younger age, asthma, greater gas-trapping by CT, and GERD were statistically significant risk factors in the TIO group, while female gender and African-American race approached significance. Female gender, higher SGRQ score, and GERD were risk factors in the ICS ± LABA group, while history of pneumonia, hay fever, and cardiovascular disease all approached statistical significance. In the SAB group, female gender, home oxygen therapy, and frequent cough symptom were all statistically significant risk factors, while higher FEV1 change post-BD approached statistical significance. Statistically significant results are summarized in Table 4.
Head-to-head analysis
In the analysis of each group’s baseline characteristics, we determined that the TIO and ICS ± LABA groups represented broadly similar populations of subjects in terms of severity, imaging characteristics, and symptoms. These similarities allowed us to combine these groups to analyze exacerbation risk factors in a head-to-head fashion while limiting confounding by indication. We compared the effects of tiotropium vs. ICS ± LABA therapy on prospective exacerbations in a logistic regression model combining subjects in the TIO and ICS ± LABA groups (Table 5) adjusted for the baseline differences between the groups, including age, asthma, MMRC score, SGRQ score, BODE score, and TLC. There was a trend towards a reduction in exacerbation risk for tiotropium (OR 0.69, p = 0.09). The logistic regression models were repeated after stratifying by asthma status. In subjects without a history of comorbid asthma, there was a stronger trend toward reduction in exacerbation risk from tiotropium (OR 0.56, p = 0.05). In only the subjects with comorbid asthma, this association disappeared (OR 1.03, p = 1.0).
Discussion
Using prospective observational data from the COPDGene Study, we identified risk factors for exacerbations within four groups of subjects with common medication use patterns. While comparison across medication groups is confounded by indication, we found substantial similarities between the subjects using ICS ± LABA and those using TIO. Controlling for baseline differences in a head-to-head analysis, we saw a trend towards an association with reduced exacerbation risk for tiotropium compared to ICS ± LABA, especially in subjects without the diagnosis of asthma. We also demonstrated the feasibility of using self-reported medication data from an observational study to generate hypotheses regarding drug treatment effects.
The interplay of comorbid conditions with COPD exacerbations has been previously described [22, 23], and the influence of comorbidities on COPD exacerbations is also shown in our study. Respiratory comorbidities such as asthma and prior pneumonia were risk factors in some groups. GERD has previously been described as a risk factor for more frequent COPD exacerbations [24] and our data showed a similar effect in all medication groups except for those using only short-acting agents. Notably, other cardiopulmonary comorbidities such as prior venous thromboembolism, obstructive sleep apnea, higher BMI, and congestive heart failure did not show an association. Previous studies have shown an association between ongoing smoking and exacerbation risk [25–27]. However, current smoking and cumulative pack-year exposure were not risk factors in any group within our study, despite the acute [28] and chronic inflammatory effects of cigarette smoke on airways [29] and the immune system [30].
The baseline characteristics of the TIO and ICS ± LABA groups were similar across many clinical parameters. Although SGRQ and MMRC scores were statistically different between the two groups, these did not exceed thresholds for minimal clinically important differences [31, 32]. The similarities between these baseline characteristics make possible comparison between the two groups with less concern of confounding by indication. The similarity between the two groups was more clearly seen among the non-asthmatic subjects. These findings reflect current clinical practice guidelines, in which administration of a long-acting beta-agonist/inhaled corticosteroid or long-acting muscarinic-antagonist are both recommended for patients with FEV1 < 60 % predicted and stable symptoms [33]. The overall rate of exacerbations among this population was lower than previously published randomized controlled trials data of TIO [3, 13] or ICS ± LABA [13], however those trials enrolled patients with more severe airflow obstruction.
The number of subjects with asthma in the ICS ± LABA group was higher than in the TIO group. It is plausible that concurrent asthma may lead a provider to prescribe ICS ± LABA combinations [34] given the prominent role of inhaled corticosteroids as anti-inflammatory therapy in asthma [35]. Alternatively, subjects with asthma and COPD may have had greater symptomatic response to ICS ± LABA, creating a preference for this medication among asthma-COPD overlap patients. In previous COPDGene publications, the asthma-COPD overlap syndrome has been shown to be a relevant clinical entity, associated with worse health-related quality of life and more frequent exacerbations [17, 36]. These findings were recapitulated in our analysis, with subjects with asthma-COPD overlap taking either TIO or ICS ± LABA showing a higher rate of exacerbations than their non-asthmatic counterparts, as well as a trend towards higher SGRQ scores.
In this observational study, we observed a trend towards an association with reduction in exacerbation risk in subjects taking tiotropium compared to ICS ± LABA. The trend was stronger in subjects without asthma. Conflicting randomized trial literature exists on the choice of tiotropium or long-acting beta-agonist/inhaled corticosteroid in advanced stage COPD. The INSPIRE trial [13] showed no difference in rates of exacerbations among COPD subjects randomized to ICS ± LABA vs. TIO, and subjects were excluded from INSPIRE if they had significant bronchodilator response or asthma [37]. However INSPIRE subjects had more severe airflow obstruction (mean FEV1 39.3 % predicted vs. 48.3 % predicted in our study), so their comparison of TIO and ICS/LABA may not generalize to COPDGene. Conversely, a recent meta-analysis of randomized controlled trials comparing tiotropium vs. long-acting beta-agonist (with 35–56 % of patients taking inhaled corticosteroid as well) in stable COPD showed a reduction in exacerbations with tiotropium.
Previous literature comparing COPD medication regimens with and without inhaled corticosteroids have largely focused on comparisons of LABA alone versus ICS + LABA, without comparisons of long-acting muscarinics versus an ICS ± LABA regimen. A randomized trial conducted in Canada in subjects with moderate to severe COPD showed a decreased exacerbation rate in subjects receiving fluticasone as part of a triple therapy regimen of tiotropium/fluticasone/salmeterol compared with those receiving tiotropium alone or tiotropium/salmeterol [38]. The TORCH trial [11] showed a decreased annual exacerbation rate in subjects with moderate to severe COPD receiving fluticasone/salmeterol therapy compared with those receiving salmeterol alone. More recently, the WISDOM trial [39] demonstrated that the time to first moderate or severe COPD exacerbation was similar in subjects with severe and very severe COPD continuing triple therapy with tiotropium/salmeterol/fluticasone or undergoing controlled withdrawal of inhaled corticosteroid therapy, which cast doubt on the added benefit of corticosteroids for those with stable COPD. Finally, the longitudinal cohort study by Gershon et al. from 2014 [40] reviewed database information in elderly COPD subjects without asthma starting LABA or ICS ± LABA therapy and showed that those subjects using LAMAs did not have a better outcome on the composite outcome of hospitalization or death. Given the conflicting evidence regarding the optimal choice of inhaled therapy for patients with moderate to severe COPD, we contend that our data adds to the debate questioning the added benefit of inhaled corticosteroids in these patients, and is hypothesis-generating for additional investigation comparing ICS ± LABA versus tiotropium alone.
Our study has several limitations. The medication usage data is based upon subject report at the initial study visit, and was not updated during the longitudinal follow-up. Because of the lack of follow-up medication data, we are unable to account for medication changes that might influence inclusion and analysis of a subject in a particular medication group. Self-report of exacerbations could introduce bias, however this self-reported definition has been used in previous work in COPDGene as well as other COPD studies such as ECLIPSE [1]. LFU calls were completed every 3 to 6 months, so some exacerbation events may have been missed. Therefore we dichotomized subjects into exacerbators and non-exacerbators, rather than analyzing exacerbation counts. Our definition of exacerbators used a threshold of ≥1 exacerbation per year, which differs from previous studies which used ≥2 exacerbations per year [1] and may limit direct comparison of results. COPDGene subjects had a lower overall rate of exacerbations than other study populations. Using a threshold of ≥2 exacerbations per year led to small sample sizes in the medication groups (see Fig. 2) that would have limited our power to detect associations. The definition of asthma in this study was based on self-reported diagnosis by a clinician, which has been previously used in COPDGene [17]. The diagnosis of asthma may have influenced a prescriber’s choice of inhaled corticosteroids as a controller medication. In order to minimize confounding by indication, we compared exacerbation risk factors within subjects reporting the same medication usage pattern. The characteristics of subjects using TIO and ICS ± LABA were similar, so we were able to compare these medications in a prospective observational design. Our results suggest that tiotropium may be associated with decreased exacerbations compared with ICS ± LABA among patients without concurrent asthma. However a randomized clinical trial would be needed to confirm this hypothesis.
Conclusions
In summary, this study examined risk factors for future exacerbations in COPD subjects using common medications, which may help providers identify individuals at higher risk of exacerbations and influence treatment strategies or discussions of action plans. We confirmed previous associations of GERD and female gender with exacerbation risk in certain subsets, and found that previous pneumonia, higher SGRQ scores, and gas trapping on CT scans were risk factors for exacerbations in subjects using certain medications. The head-to-head analysis also showed a trend towards a reduced exacerbation risk with tiotropium compared to ICS ± LABA in COPD subjects without concurrent asthma, which could be viewed as hypothesis-generating for a clinical trial. This study may also add to the body of literature questioning the added benefit of ICS in moderate to severe COPD.
Ethics approval and consent to participate
The COPDGene Study was approved by Partners Healthcare institutional review board (Protocol # 2007P000554) and institutional review boards at all study sites, and written informed consent was obtained from all subjects.
Consent for publication
Not Applicable
Availability of data and materials
COPDGene data is available on dbGAP (http://www.ncbi.nlm.nih.gov/gap, accession number phs000179.v4.p2)
Abbreviations
- 6MWT:
-
six minute walk test
- BD:
-
bronchodilator
- BMI:
-
body mass index
- BODE:
-
body mass index, airflow obstruction, dyspnea, and exercise capacity score
- COPD:
-
chronic obstructive pulmonary disease
- COPDGene:
-
The Genetic Epidemiology of COPD Study
- CT:
-
computed tomography
- FEV1:
-
forced expiratory volume in one second
- FVC:
-
forced vital capacity
- GERD:
-
gastroesophageal reflux disease
- GOLD:
-
Global Initiative for Obstructive Lung Disease
- ICS ± LABA:
-
long-acting beta-agonist/inhaled corticosteroid
- LFU:
-
COPDGene biannual telephone- and web-based longitudinal follow-up program
- MMRC:
-
Modified Medical Research Council Scale for Dyspnea
- OR:
-
odds ratio
- SAB:
-
short-acting bronchodilator
- SGRQ:
-
St. George's Respiratory Questionnaire
- SRWA-Pi10:
-
square root of wall area of a hypothetical 10 mm internal perimeter airway
- TIO:
-
tiotropium
- TLC:
-
total lung capacity
References
Hurst JR, Vestbo J, Anzueto A, Locantore N, Mullerova H, Tal-Singer R, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128–38.
Anzueto A. Impact of exacerbations on COPD. Eur Respir Rev. 2010;19(116):113–8.
Anzueto A, Leimer I, Kesten S. Impact of frequency of COPD exacerbations on pulmonary function, health status and clinical outcomes. Int J Chron Obstruct Pulmon Dis. 2009;4:245–51.
Spencer S, Calverley PM, Sherwood Burge P, Jones PW. Health status deterioration in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;163(1):122–8.
Connors Jr AF, Dawson NV, Thomas C, Harrell Jr FE, Desbiens N, Fulkerson WJ, et al. Outcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments). Am J Respir Crit Care Med. 1996;154(4 Pt 1):959–67.
Seemungal TA, Donaldson GC, Paul EA, Bestall JC, Jeffries DJ, Wedzicha JA. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157(5 Pt 1):1418–22.
Cote CG, Dordelly LJ, Celli BR. Impact of COPD exacerbations on patient-centered outcomes. Chest. 2007;131(3):696–704.
Han MK, Kazerooni EA, Lynch DA, Liu LX, Murray S, Curtis JL, et al. Chronic obstructive pulmonary disease exacerbations in the COPDGene study: associated radiologic phenotypes. Radiology. 2011;261(1):274–82.
Wells JM, Washko GR, Han MK, Abbas N, Nath H, Mamary AJ, et al. Pulmonary arterial enlargement and acute exacerbations of COPD. N Engl J Med. 2012;367(10):913–21.
Tashkin DP, Celli B, Senn S, Burkhart D, Kesten S, Menjoge S, et al. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008;359(15):1543–54.
Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356(8):775–89.
Welsh EJ, Cates CJ, Poole P. Combination inhaled steroid and long-acting beta2-agonist versus tiotropium for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2013;5:CD007891.
Wedzicha JA, Calverley PM, Seemungal TA, Hagan G, Ansari Z, Stockley RA. The prevention of chronic obstructive pulmonary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromide. Am J Respir Crit Care Med. 2008;177(1):19–26.
Regan EA, Hokanson JE, Murphy JR, Make B, Lynch DA, Beaty TH, et al. Genetic epidemiology of COPD (COPDGene) study design. COPD. 2010;7(1):32–43.
Bowler RP, Kim V, Regan E, Williams A, Santorico SA, Make BJ, et al. Prediction of acute respiratory disease in current and former smokers with and without COPD. Chest. 2014;146(4):941–50.
Stewart JI, Moyle S, Criner GJ, Wilson C, Tanner R, Bowler RP, et al. Automated telecommunication to obtain longitudinal follow-up in a multicenter cross-sectional COPD study. COPD. 2012;9(5):466–72.
Hardin M, Silverman EK, Barr RG, Hansel NN, Schroeder JD, Make BJ, et al. The clinical features of the overlap between COPD and asthma. Respir Res. 2011;12:127.
Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163(5):1256–76.
Team RDC. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2008.
Park SJ, Make B, Hersh CP, Bowler RP. Significance of Medication History at the Time of Entry into the COPDGene Study: Relationship with Exacerbation and CT Metrics. COPD. 2014;12(4):366–73.
Swift I, Satti A, Kim V, Make BJ, Newell J, Steiner RM, et al. Demographic, physiologic and radiographic characteristics of COPD patients taking chronic systemic corticosteroids. COPD. 2012;9(1):29–35.
Miravitlles M, Guerrero T, Mayordomo C, Sanchez-Agudo L, Nicolau F, Segu JL. Factors associated with increased risk of exacerbation and hospital admission in a cohort of ambulatory COPD patients: a multiple logistic regression analysis. The EOLO Study Group. Respiration. 2000;67(5):495–501.
Divo M, Cote C, de Torres JP, Casanova C, Marin JM, Pinto-Plata V, et al. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;186(2):155–61.
Rascon-Aguilar IE, Pamer M, Wludyka P, Cury J, Coultas D, Lambiase LR, et al. Role of gastroesophageal reflux symptoms in exacerbations of COPD. Chest. 2006;130(4):1096–101.
Godtfredsen NS, Vestbo J, Osler M, Prescott E. Risk of hospital admission for COPD following smoking cessation and reduction: a Danish population study. Thorax. 2002;57(11):967–72.
Garcia-Aymerich J, Farrero E, Felez MA, Izquierdo J, Marrades RM, Anto JM. Risk factors of readmission to hospital for a COPD exacerbation: a prospective study. Thorax. 2003;58(2):100–5.
Beeh KM, Glaab T, Stowasser S, Schmidt H, Fabbri LM, Rabe KF, et al. Characterisation of exacerbation risk and exacerbator phenotypes in the POET-COPD trial. Respir Res. 2013;14:116.
van der Vaart H, Postma DS, Timens W, ten Hacken NH. Acute effects of cigarette smoke on inflammation and oxidative stress: a review. Thorax. 2004;59(8):713–21.
Tamimi A, Serdarevic D, Hanania NA. The effects of cigarette smoke on airway inflammation in asthma and COPD: therapeutic implications. Respir Med. 2012;106(3):319–28.
Sopori M. Effects of cigarette smoke on the immune system. Nat Rev Immunol. 2002;2(5):372–7.
Jones PW. Interpreting thresholds for a clinically significant change in health status in asthma and COPD. Eur Respir J. 2002;19(3):398–404.
Jones PW. St. George's Respiratory Questionnaire: MCID. COPD. 2005;2(1):75–9.
Qaseem A, Wilt TJ, Weinberger SE, Hanania NA, Criner G, van der Molen T, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179–91.
Kesten S, Chapman KR. Physician perceptions and management of COPD. Chest. 1993;104(1):254–8.
Chung KF, Wenzel SE, Brozek JL, Bush A, Castro M, Sterk PJ, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43(2):343–73.
Hardin M, Cho M, McDonald ML, Beaty T, Ramsdell J, Bhatt S, et al. The clinical and genetic features of COPD-asthma overlap syndrome. Eur Respir J. 2014;44(2):341–50.
Seemungal T, Stockley R, Calverley P, Hagan G, Wedzicha JA. Investigating new standards for prophylaxis in reduction of exacerbations--the INSPIRE study methodology. COPD. 2007;4(3):177–83.
Aaron SD, Vandemheen KL, Fergusson D, Maltais F, Bourbeau J, Goldstein R, et al. Tiotropium in combination with placebo, salmeterol, or fluticasone-salmeterol for treatment of chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med. 2007;146(8):545–55.
Magnussen H, Disse B, Rodriguez-Roisin R, Kirsten A, Watz H, Tetzlaff K, et al. Withdrawal of inhaled glucocorticoids and exacerbations of COPD. N Engl J Med. 2014;371(14):1285–94.
Gershon AS, Campitelli MA, Croxford R, Stanbrook MB, To T, Upshur R, et al. Combination long-acting beta-agonists and inhaled corticosteroids compared with long-acting beta-agonists alone in older adults with chronic obstructive pulmonary disease. JAMA. 2014;312(11):1114–21.
Acknowledgements
ᅟ
Funding
This study was supported by NIH grants T32 HL007427, R01HL094635, R01NR013377, P01HL105339, R01HL089897 and R01HL089856. The COPDGene Study is also supported by the COPD Foundation through contributions made to an Industry Advisory Board comprised of AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Novartis, Pfizer, Siemens and Sunovion.
Role of the funding body
The funding sources were not directly involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Collaborators
We would like to acknowledge and thank the COPDGene Investigators listed below.
Administrative Core: James Crapo, MD (PI), Edwin Silverman, MD, PhD (PI), Barry Make, MD, Elizabeth Regan, MD, PhD
Genetic Analysis Core: Terri Beaty, PhD, Nan Laird, PhD, Christoph Lange, PhD, Michael Cho, MD, Stephanie Santorico, PhD, John Hokanson, MPH, PhD, Dawn DeMeo, MD, MPH, Nadia Hansel, MD, MPH, Craig Hersh, MD, MPH, Peter Castaldi, MD, MSc, Merry-Lynn McDonald, PhD, Emily Wan, MD, Megan Hardin, MD, Jacqueline Hetmanski, MS, Margaret Parker, MS, Marilyn Foreman, MD, Brian Hobbs, MD, Robert Busch, MD, Adel El-Boueiz, MD, Peter Castaldi, MD, Megan Hardin, MD, Dandi Qiao, PhD, Elizabeth Regan, MD, Eitan Halper-Stromberg, Ferdouse Begum, Sungho Won, Sharon Lutz, PhD
Imaging Core: David A Lynch, MB, Harvey O Coxson, PhD, MeiLan K Han, MD, MS, MD, Eric A Hoffman, PhD, Stephen Humphries MS, Francine L Jacobson, MD, Philip F Judy, PhD, Ella A Kazerooni, MD, John D Newell, Jr., MD, Elizabeth Regan, MD, James C Ross, PhD, Raul San Jose Estepar, PhD, Berend C Stoel, PhD, Juerg Tschirren, PhD, Eva van Rikxoort, PhD, Bram van Ginneken, PhD, George Washko, MD, Carla G Wilson, MS, Mustafa Al Qaisi, MD, Teresa Gray, Alex Kluiber, Tanya Mann, Jered Sieren, Douglas Stinson, Joyce Schroeder, MD, Edwin Van Beek, MD, PhD
PFT QA Core, Salt Lake City, UT: Robert Jensen, PhD
Data Coordinating Center and Biostatistics, National Jewish Health, Denver, CO: Douglas Everett, PhD, Anna Faino, MS, Matt Strand, PhD, Carla Wilson, MS
Epidemiology Core, University of Colorado Anschutz Medical Campus, Aurora, CO: John E. Hokanson, MPH, PhD, Gregory Kinney, MPH, PhD, Sharon Lutz, PhD, Kendra Young PhD, Katherine Pratte, MSPH, Lindsey Duca, M
Ann Arbor VA: Jeffrey L. Curtis, MD, Carlos H. Martinez, MD, MPH, Perry G. Pernicano, MD
Baylor College of Medicine, Houston, TX: Nicola Hanania, MD, MS, Philip Alapat, MD, Venkata Bandi, MD, Mustafa Atik, MD, Aladin Boriek, PhD, Kalpatha Guntupalli, MD, Elizabeth Guy, MD, Amit Parulekar, MD, Arun Nachiappan, MD
Brigham and Women’s Hospital, Boston, MA: Dawn DeMeo, MD, MPH, Craig Hersh, MD, MPH, George Washko, MD, Francine Jacobson, MD, MPH
Columbia University, New York, NY: R. Graham Barr, MD, DrPH, Byron Thomashow, MD, John Austin, MD, Belinda D’Souza, MD, Gregory D.N. Pearson, MD, Anna Rozenshtein, MD, MPH, FACR
Duke University Medical Center, Durham, NC: Neil MacIntyre, Jr., MD, Lacey Washington, MD, H. Page McAdams, MD
Health Partners Research Foundation, Minneapolis, MN: Charlene McEvoy, MD, MPH, Joseph Tashjian, MD
Johns Hopkins University, Baltimore, MD: Robert Wise, MD, Nadia Hansel, MD, MPH, Robert Brown, MD, Karen Horton, MD, Nirupama Putcha, MD, MHS,
Los Angeles Biomedical Research Institute at Harbor UCLA Medical Center, Torrance, CA: Richard Casaburi, PhD, MD, Alessandra Adami, PhD, Janos Porszasz, MD, PhD, Hans Fischer, MD, PhD, Matthew Budoff, MD, Harry Rossiter, PhD
Michael E. DeBakey VAMC, Houston, TX: Amir Sharafkhaneh, MD, PhD, Charlie Lan, DO
Minneapolis VA: Christine Wendt, MD, Brian Bell, MD
Morehouse School of Medicine, Atlanta, GA: Marilyn Foreman, MD, MS, Gloria Westney, MD, MS, Eugene Berkowitz, MD, PhD
National Jewish Health, Denver, CO: Russell Bowler, MD, PhD, David Lynch, MD
Reliant Medical Group, Worcester, MA: Richard Rosiello, MD, David Pace, MD
Temple University, Philadelphia, PA: Gerard Criner, MD, David Ciccolella, MD, Francis Cordova, MD, Chandra Dass, MD, Gilbert D’Alonzo, DO, Parag Desai, MD, Michael Jacobs, PharmD, Steven Kelsen, MD, PhD, Victor Kim, MD, A. James Mamary, MD, Nathaniel Marchetti, DO, Aditi Satti, MD, Kartik Shenoy, MD, Robert M. Steiner, MD, Alex Swift, MD, Irene Swift, MD, Maria Elena Vega-Sanchez, MD
University of Alabama, Birmingham, AL: Mark Dransfield, MD, William Bailey, MD, J. Michael Wells, MD, Surya Bhatt, MD, Hrudaya Nath, MD
University of California, San Diego, CA: Joe Ramsdell, MD, Paul Friedman, MD, Xavier Soler, MD, PhD, Andrew Yen, MD
University of Iowa, Iowa City, IA: Alejandro Cornellas, MD, John Newell, Jr., MD, Brad Thompson, MD
University of Michigan, Ann Arbor, MI: MeiLan Han, MD, Ella Kazerooni, MD, Carlos Martinez, MD
University of Minnesota, Minneapolis, MN: Joanne Billings, MD, Tadashi Allen, MD
University of Pittsburgh, Pittsburgh, PA: Frank Sciurba, MD, Divay Chandra, MD, MSc, Joel Weissfeld, MD, MPH, Carl Fuhrman, MD, Jessica Bon, MD
University of Texas Health Science Center at San Antonio, San Antonio, TX: Antonio Anzueto, MD, Sandra Adams, MD, Diego Maselli-Caceres, MD, Mario E. Ruiz, MD
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Competing interests
The authors (RB, MKH, RPB, MTD, JMW, EAR, CPH) assert that they have no conflicts of interest to disclose directly pertaining to the content of this study. Robert Busch, and Elizabeth Regan declare that they have no conflicts of interest. Russell Bowler has served on the Advisory Board to Boehringer-Ingelheim. MeiLan Han has served as a consultant for Regenerson, Glaxo-Smith-Kline, and Boehringer-Ingelheim. Mark Dransfield has served as a consultant for Glaxo-Smith-Kline, Boehringer-Ingelheim, and Ikaria. J Michael Wells and Mark Dransfield both declare that their institution has received research grant support from the American Heart Association, National Heart Lung and Blood Institute, Glaxo-Smith-Kline, and Forest and has received contracted support for enrollment in clinical trials from Aeris, AstraZeneca, Boehringer-Ingelheim, Boston Scientific, Centocor, Glaxo-Smith-Kline, Forest, Otsuka, Pearl, Pfizer, PneumRx, and Pulmonx. Craig Hersh has received lecture fees from Novartis and consulting fees from CSL Behring.
Authors’ contributions
All of the authors listed have contributed sufficiently to the project to be included as authors by BMC Pulmonary Medicine/ICMJE guidelines, and all those who are qualified to be authors are listed in the author byline. RB was responsible for the study conception and design, data analysis, manuscript drafting, and critical revision of the manuscript for important intellectual content. CPH contributed substantially to the study design, data analysis and interpretation, the writing and revising of the manuscript, agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved, and provided final approval of the version to be published. RPB was responsible for data acquisition, contributed to the writing and revising of the manuscript for important intellectual content, and provided final approval of the version to be published. CPH, MKH, RPB, MTD, JMW, and EAR contributed substantially to the data analysis and interpretation, the writing and revising of the manuscript, and have provided final approval of the version to be published.
Additional file
Additional file 1:
Supplementary Data and Methods. (DOCX 38 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Busch, R., Han, M.K., Bowler, R.P. et al. Risk factors for COPD exacerbations in inhaled medication users: the COPDGene study biannual longitudinal follow-up prospective cohort. BMC Pulm Med 16, 28 (2016). https://doi.org/10.1186/s12890-016-0191-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-016-0191-7