Abstract
Background
In September 2022, a new Ebola outbreak was reported in Uganda, East Africa, and 142 confirmed cases, including 19 Healthcare workers (HCWs) reported. Ebola is not endemic in Somalia, but the country is at a reasonable risk of the virus being introduced due to the direct connection with daily flights from Uganda without border health control and prevention activities. Therefore, evaluating HCWs' Knowledge and attitude is crucial since this is the first time being evaluated in Somalia. The study's objective is to evaluate the HCWs' Knowledge and attitude toward the Ebola virus disease in Somalia.
Method
An online self-administrated cross-sectional survey was conducted among HCWs (n = 1103) in all six federal member states of Somalia using a validated, reliable, well-structured questionnaire. Data we analyzed using descriptive statistics and Logistic regression were used to determine sociodemographic characteristics associated with poor Knowledge and negative attitude.
Result
Over one-third (37.3%) of HCWs had poor Knowledge; the mean knowledge score was 7.97 SD ± 2.15. Almost 40.1% of the HCWs had a negative attitude; the mean attitude was 27.81 SD ± 8.06. Low-income HCWs (AOR = 2.06, 95%CI:1.01–4.19), Married HCWs (AOR = 1.39, 95%CI: 1.110–1.963), Midwives (AOR = 2.76, 95%CI: 1.74–4.39), Lab technicians (AOR = 2.43, 95%CI: 1.43–4.14), HCWs work in Jubaland state of Somalia (AOR = 3.69, 95%CI: 2.39–5.70), Galmudug state (AOR = 8.50, 95%CI: 4.59–15.77), Hirshabelle state (AOR = 3.18, 95%CI: 2.15–4.71) were more likely to have poor Knowledge compared to their counterparts. HCWs who work in Hirshabelle state (AOR = 5.44,95%CI: 3.58–8.27), Jubaland state (AOR = 8.47, 95%CI: 4.69–15.29), and Galmudug state (AOR = 4.43, 95%CI: 3.03–6.48) was more likely to have a negative attitude than those working in the Banadir region administration.
Conclusion
Most Somali healthcare workers showed good Knowledge and a positive attitude toward the Ebola virus. The implementation to enhance Knowledge and attitude must specifically focus on low-income HCWs, Midwives, Lab technicalities, and those who work in Hirshabelle, Jubaland, and Galmudug states of Somalia.
Similar content being viewed by others
Background
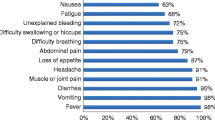
Ebola virus disease (EVD), also known as Ebola hemorrhagic fever, is a severe and often fatal illness caused by the Ebola virus. The virus is transmitted to humans through contact with infected animals, bodily fluids of infected people, or contact with contaminated objects [1]. After 2 to 21 days of its incubation period, symptoms including fever, headache, muscle pain, weakness, fatigue, diarrhea, vomiting, abdominal pain, and unexplained bleeding or bruising can appear [2, 3]. The Ebola virus is highly contagious, often a feral disease, and licensed treatment and vaccines are available in limited numbers to cure and prevent Zaire Ebola virus species. In contrast, Sudan Ebola virus species (SUDV) currently have no licensed treatment and vaccines [4]. However, supportive care, effective prevention strategies, and infection control practices in healthcare settings are vital to improving the chances of survival [2,3,4,5].
WHO recognized a public health threat and numerous vital aspects, including healthcare workers' (HCWs) knowledge and attitude require deep understanding [3,4,5,6,7]. Therefore, enhancing the community's knowledge and attitude is essential to reduce transmission [7,8,9,10,11]. Sub-Saharan African communities over-trust traditional medicine and religious, cultural, and social leaders instead of scientific medical knowledge, which may worsen the outbreaks [12]. Surveying HCWs' knowledge and attitude may help control recurrent outbreaks and support knowledge-building activities [12,13,14].
Previous Ebola outbreaks caused healthcare workers significant mortalities, and healthcare providers were 21 to 32 times greater to be infected Ebola virus than the general adult population [15]. In Sierra Leone, a high number of healthcare workers were infected Ebola virus, with almost 221 death of healthcare workers [15]. In addition, the outbreak affected numerous efforts to strengthen human resources for health, and a weak healthcare system might exacerbate the situation [16, 17]. Around 500 confirmed cases of healthcare workers were reported in Guinea, Liberia, Sierra Leone, and Nigeria [17]. Liberia, Sierra Leone, and Guinea lost 8%, 7%, and 1% of HCWs, respectively [18, 19]. The outbreak also delayed and adversely impacted healthcare delivery; over 50% occurred in the above three countries [20].
In September 2022, a new Ebola outbreak was reported in Uganda, and 142 confirmed and 22 suspected cases with 77 deaths were reported. Almost 19 confirmed cases with 7 deaths were HCWs [4, 21]. The Ebola outbreak is not currently or previously reported in Somalia, but the country is at risk due to the direct connection with daily flights from Uganda, where the disease is endemic without any border health control and prevention activities. Passenger and military flights from Uganda operate daily in Somalia. The Ministry of Health and its partners reported a reasonable risk of introducing the virus into Somalia and enhanced their emergency response plan [22]. Therefore, these efforts become worthless without evaluating HCWs' knowledge and attitude toward the Ebola virus since it has yet to be surveyed in Somalia. This assessment may have a vital role in developing tailored health education programs, supporting public health policymakers and interventions that focus on implementing response to Ebola and strengthening HCWs' awareness. The study aims to evaluate the HCWs' knowledge and attitude toward the Ebola virus disease in Somalia.
Methodology
Study design
A cross-sectional online survey was conducted between 1 December 2022 to 31 January 2023 among healthcare workers across all six federal member states of Somalia. The study invited voluntary, anonymous online surveys to healthcare workers to evaluate KAP toward Ebola.
Inclusion and exclusion criteria
Healthcare professionals who were directly or indirectly involved in healthcare in all six federal member states, including the Banadir administration, older than 18 years were included in the study after excluding those does not have healthcare qualifications, those who are not Somali citizens, and those who do not provide verbal consent.
Study population and sampling techniques
The healthcare workers in this study were qualified medical professionals directly or indirectly involved in providing healthcare for all six federal member states of Somalia. They included nurses (n = 395), medical doctors (n = 362), midwives (n = 132), Lab technicians (n = 89), Pharmacists (n = 38), and other healthcare providers (n = 87). The Ministry of Health and Social Services of the federal republic of Somalia estimated that 19,306 healthcare professionals work in Somalia [23,24,25]. Since there was no similar study in the study area, the sample size calculation was based on a single population proportion formula built on the 50% assumption that the probability of having poor knowledge and attitude toward Ebola virus infection with a 3% of margin of error and, 95% confidence interval (CI) [25, 26]. The total sample study required was 1063 healthcare workers including an additional 5% of a non-response rate. However, this study recruited 1103 respondents after excluding 30 incomplete responses. The probability proportional to size (PPS) sampling technique [27] was used to ensure that the sample was represented in each unit and that samples were distributed as below (Fig. 1).
Development of research tools and variables
A well-structured reliable, validated, self-administered questionnaire was developed from a literature review [8, 13, 28] and discussed by three experts. The questionnaire consists of i) Socio-demographic characteristics (Age, gender, marital status, healthcare profession and experience, monthly income), ii) Twelve true or false simple-dichotomy knowledge statements, and iii) Nine Likert 5-scale attitude statements. All statements are based on Ebola virus infection, epidemiological characteristics, source, signs and symptoms, supportive treatment mode of transmission, risk factors, outbreak prevention, and control strategies.
For the Knowledge section, a 1 score gave a correct response and a 0 for an incorrect response for regular statements and vice-versa for the reverse statements. The maximum expected knowledge score was 12, and all knowledge statements were computed and categorized as poor Knowledge if the score was ≤ 60% (0–7 scores) and good Knowledge if the score was > 60% (8–12 scores) according to the widely adopted modified Bloom's cut-of-point classification [29,30,31,32].
For attitude, nine Likert 5-scale statements were used (1 from strongly disagree to 5 strongly agree), and vice versa reverse statements. All statements were computed; the maximum expected score was 45 and was categorized as a positive attitude if the score was > 60% (28 to 45 score) and a negative attitude if the score was ≤ 60% (0 to 27 scores) according to the widely adopted modified Bloom's cut-of-point classification [33, 34].
The study tool was initially developed in English, and then language experts did forward–backward translations to verify the consistency. The Somali version was used to collect data. The item objective congruence (IOC) method [35] was used for content validity by three external experts (An infectious disease specialist, a Tropical medicine physician, and a clinical epidemiology & public health expert). Consequently, to ensure reliability and respondents' understanding of the questionnaire, a pilot study of 55 respondents (5% of the sample) was conducted for respondents with similar characteristics. An acceptable internal consistency Cronbach's Coefficient alpha of 0.83 and 0.81 for Knowledge and attitude statements were achieved, respectively.
Data collection techniques
The study tool was initially developed in English, and then language experts translated it into Somali to verify the consistency. The Somali version constructed an online electronic form used for data collection. The online tool shared eligible HCWs who met the inclusion criteria and they responded to the self-administered online questionnaire without support. All respondents were informed of the study objective and eligibility criteria, and participation is voluntary and requested to provide verbal consent. The healthcare administrative officials at the healthcare institutions in the six federal member states facilitated the data collection.
Data analysis
Data were cleaned, coded, entered, and kept on the speeded sheet, then imported into the SPSS version 20 (SPSS, Chicago, IL) for analysis. Descriptive statistics were used for general characteristics and knowledge and attitude statements by presenting frequency with percentage for categorical data and mean with standard deviation (SD) for continuous data. The knowledge section, modified Bloom's cut-of-point classification [29,30,31,32], was used by giving 1 score for a correct response and 0 for an incorrect one. All knowledge statements were computed and categorized as poor Knowledge (≤ 60%) and good Knowledge (> 60%). All attitude statements were computed and were categorized as a negative attitude (≤ 60%) and a positive attitude (> 60%) according to modified Bloom's cut-of-point classification [33, 34]. Logistic regression in univariable and multivariable models was used to determine variables associated with poor Knowledge and negative attitude. Variables with a p-value < 0.20 in the univariable logistic regression model were candidates for multivariate logistic regression. Bursac et al. [36] suggest that variables with a p-value < 0.20 in univariate logistic regression may have some reasonable association with the outcome in the final model if they adjust each other due to the possibility of having a confounder in other variables. The Hosmer–Lemeshow goodness of fit test was used to indicate the final model goodness of fit [37]. In Multivariable logistic regression, variables with a p-value < 0.05 were considered statistically significant.
Result
Socio-demographic characteristics
A total of 1103 healthcare workers participated in this study; most of them (28.6%) work in the Banadir region and almost half (46.7%) were aged between 26 to 33 years old with a mean 29.25 SD ± 7.85. More than half (54.4%) were female, 35.8% were nurses, 52.0% had 1–5 years of healthcare work experience, and 51.9% had a monthly income between 201–500 USD (Table 1).
Healthcare workers' knowledge of Ebola virus infection
This study showed that one-third of 411 (37.3%) healthcare workers had poor knowledge, and 692(62.7%) had good knowledge of Ebola virus infections. The mean knowledge score was 7.97 SD ± 2.15 (Table 2).
Healthcare workers' attitude to Ebola virus infection
This study showed that 442 (40.1%) healthcare workers had a negative attitude, while 661(59.9%) had a positive attitude toward Ebola virus infections. The mean attitude was 27.81 SD ± 8.06 mean (Table 3).
Association between demographical characteristics and poor knowledge
In the Univariable logistic regression analytical model, six (6) variables were associated with healthcare workers (HCWs) poor knowledge of Ebola virus infection: These variables were candidates for multivariable logistic regression, and four were associated with poor knowledge. Low-income healthcare workers were 2.06 times more likely to (95% CI;1.01–4.19) have poor knowledge of Ebola virus infections compared to high-income HCWs. The odds of poor knowledge were 1.39 times greater (95% CI; 1.110–1.963) for ever-married HCWs compared to unmarried HCWs. Midwives are 2.76 times more likely (95% CI; 1.74–4.39), and Lab technicians are 2.43 times more likely (95% CI; 1.43–4.14) to have poor knowledge compared to Nurses. Healthcare workers working in Jubaland state were 3.69 times more likely (95% CI; 2.39–5.70), Galmudug state was 8.50 times more likely (95% CI; 4.59–15.77), and Hirshabelle state 3.18 times more likely (95% CI; 2.15–4.71) to be poor knowledge compared to those working Banadir region administration (Table 4).
Association between demographical characteristics and negative attitude
In the univariable logistic regression analysis, six (6) variables were associated with negative attitudes: These variables were candidates for multivariable logistic regression, and only one variable was found to be significantly associated with negative attitudes toward Ebola virus infection. Healthcare workers working in Hirshabelle state were 5.44 times (95%CI; 3.58–8.27) more likely to have negative attitudes than those working in Banadir region administration. Those who work in Jubaland state 8.47 times (95%CI; 4.69–15.29) greater of have a negative attitude compared to those who work in Banadir region administration. Those who work in Galmudug state were 4.43 times greater (95%CI; 3.03–6.48) to have a negative attitude compared to those who work in the Banadir region administration (Table 5).
Discussion
The Ebola virus disease (EVD) outbreak is not currently or previously reported in Somalia. However, the country is at risk due to the direct connection with daily flights from Uganda, where the disease is endemic without meaningful border health control and prevention activities. Passenger and military flights from Uganda operate daily in Somalia [22]. The Ministry of Health (MOH) and its partners reported a reasonable risk of introducing the virus into Somalia. They enhanced their emergency response plan by strengthening capacities following the 2005 international health regulation (IHR) to protect vulnerable populations against emergency health threats. In addition, they strengthened surveillance and alerts systems for any cluster of unexplained fever, bleeding, deaths, or other main EVD clinical features, implemented access to advanced diagnostic laboratories for the Ebola virus, established primary infection prevention and control (IPC) measurements in any health center and provided healthcare workers training to prevent infections from themselves and the community. In addition, a rapid response team was nominated and trained to conduct contact tracing and investigate if suspected case report [22].
Furthermore, in November 2018, the infectious hazard management and control unit of the World Health Organization's Eastern Mediterranean regional office implemented sequenced activities to scale up Ebola preparedness and response due to the risk of importation of cases from the democratic republic of Congo was high where the Ebola outbreak is ongoing at that time. Somalia actively participated in these activities launched by WHO to help these countries prepare for early detection of any possible outbreak, enhancing surveillance capacity, sample collection, and laboratory tests. A rapid response team from Somalia, Libya, and Pakistan received additional training [38]. Similar preparedness efforts helped ensure that all these countries remained free from Ebola between 2014 to 2015 [38]. Before the covid-19 pandemic, Somalia faced numerous man-made and natural disasters and infectious disease outbreaks, including tuberculosis, malaria, measles, viral hepatitis, parasitic infections, diarrhea, and HIV, which is uncommon [39,40,41,42,43,44,45].
This study recruited 1103 healthcare workers (HCWs) from Somalia's six federal member states. The study revealed that over one-third of the HCWs lack basic knowledge of Ebola (EVD). In addition, half of HCWs do not know the mode of the disease transmission. In general, poor EVD knowledge is a risk factor; HCWs' poor knowledge has a high impact on the disease spread with severe consequences for the HCWs and the entire community. HCWs with insufficient knowledge may not take the necessary precautions to protect themselves from infection leading to excessive disease spread. A similar study in the Demographic Republic of Congo (DRC) is in line and reported high disease transmission among HCWs, reasoned due to poor transmission knowledge [46].
This study discovered that one-six of the HCWs do not know they are in the frontline risk groups. It may lead HCWs to neglect and not implement infection control practices such as avoiding touching the body of a suspected or confirmed patient or dead body, regular hand washing, using personal protective equipment, and increasing the disease transmission to other healthcare providers and the community. A previous study reported that over 2,127 HCWs confirmed Ebola cases, including 1145 deaths during the EVD outbreak between 2014 and 2015 [16, 17]. It was the worst hazard that African healthcare workers faced [18, 19].
Over a quarter of this study participants do not know the sign and symptoms of the disease and even the incubation period. Hence, only one-quarter knew the mode of disease treatment. HCWs' poor signs and symptoms knowledge may delay disease diagnosis. It might prevent on-time treatment and early action, enhancing the outbreak since the disease is highly contagious and has high mortality rates. A low-income setting like sub–Saharan Africa usually has a healthcare worker shortage that may exacerbate the situation. A similar study is inline [47].
In addition, a similar study in Sub–Saharan Africa reported that previous Ebola outbreaks delayed and adversely impacted healthcare delivery [20]. Healthcare workers' poor knowledge may erode trust in the healthcare system, making outbreak control difficult. Therefore, this study re-emphasizes implementing healthcare educational programs and comprehensive training on EVD, including infection prevention and control, to enhance HCWs' access to up-to-date information and resources to help them provide safe and effective care to themselves and their patients. This study revealed that over 40% of the participating healthcare workers had a negative attitude toward the Ebola virus. Furthermore, many of them cannot believe their active participation in hospital infection control programs can reduce EVD prevalence. That can substantially impact the management and containment of the disease. Healthcare workers' negative attitudes interlink to Ebola patients' stigma and discrimination that discourage patients from seeking medical care and complying with public health measures which ultimately contribute to the spread of the disease and make it more difficult to control. A similar study concluded that healthcare workers' negative attitudes are highly associated with patient stigma. Those with negative attitudes may abuse Ebola patients verbally or/or behaviorally, worsening the situation [48].
In addition, almost one-third of the HCWs do not recognize the importance of following advice regarding the Ebola virus disease can reduce the risk of Ebola. Subsequently, over one-half need to recognize that full healthcare facilities preparedness is required to manage the Ebola outbreak. Poor knowledge can affect HCWs' ability to provide compassionate and effective care to Ebola patients. Without HCWs' preparedness, it might lead to medical treatment errors, compromise the safety of healthcare workers themselves, and may promote treatment misconceptions. Consequently, it can also undermine the healthcare system's trust and make implementing effective public health interventions difficult. Similar studies supported and stated that HCWs' negative attitudes and beliefs lead to ignoring healthcare instruction and addicting inappropriate practices [46, 49]. HCWs' practical training, support, providing needed resources, addressing negative attitudes, and promoting a culture of compassion and respect can become a buffer and valuable solution.
Conclusion
This study recruited healthcare workers (n = 1103) from all six federal member states of Somalia. It concluded that around one-third of the HCWs lack basic knowledge of the Ebola virus disease (EVD), and almost 40% of the HCWs' showed a negative attitude towards the Ebola virus disease (EVD). Therefore, the study re-emphasizes implementing healthcare educational programs and comprehensive training on EVD, including infection prevention and control, to enhance HCWs' access to up-to-date information and resources to help them provide safe and effective care to themselves and their patients. The implementation to enhance knowledge and attitude must specifically focus on low-income HCWs, Midwives, Lab technicalities, and HCWs that work in Hirshabelle, Jubaland, and Galmudug states of Somalia.
Strengths and limitations of the study
The study has numerous strengths; first, to the best of our knowledge, it is the first similar study assessing healthcare providers' knowledge and attitude toward Ebola virus disease conducted in Somalia; second, it is a multicenter nationwide survey sampled and survived all Somali federal member states (n = 1103) so the finding acts as nationally representative data that might help policymakers, healthcare educational programs, and comprehensive training on Ebola. A self-administered questionnaire was used to collect the information, so the respondents' intention and seriousness to the questions responses were difficult to access.
Availability of data and materials
All data collected and generated during the study are included in this paper.
References
Ebola virus disease, Fact sheet N°103, Updated September 2014". World Health Organization (WHO). September 2014. Archived from the original on 14 December 2014. Retrieved 15 Dec 2014.
Kishore S, Singh R. Ebola virus disease–an update. Indian J Community Health. 2014;26(4):443–5.
Vetter P, Kaiser L, Schibler M, Ciglenecki I, Bausch DG. Sequelae of Ebola virus disease: the emergency within the emergency. Lancet Infect Dis. 2016;16(6):e82-91.
World Health Organization. Ebola disease caused by Sudan ebolavirus – Uganda. 2023 [cited 8 Jan 2023]. Available from: https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON433.
Clark DV, Kibuuka H, Millard M, Wakabi S, Lukwago L, Taylor A, Eller MA, Eller LA, Michael NL, Honko AN, Olinger GG. Long-term sequelae after Ebola virus disease in Bundibugyo, Uganda: a retrospective cohort study. Lancet Infect Dis. 2015;15(8):905–12.
Mate SE, Kugelman JR, Nyenswah TG, Ladner JT, Wiley MR, Cordier-Lassalle T, Christie A, Schroth GP, Gross SM, Davies-Wayne GJ, Shinde SA. Molecular evidence of sexual transmission of Ebola virus. N Engl J Med. 2015;373(25):2448–54.
Awah PK, Boock AU, Kum KA. Ebola virus diseases in Africa: a commentary on its history, local and global context. Pan Afr Med J. 2015;22(Suppl 1):18.
Gray N, Stringer B, Bark G, Heller Perache A, Jephcott F, Broeder R, Kremer R, Jimissa AS, Samba TT. ‘When Ebola enters a home, a family, a community’: a qualitative study of population perspectives on Ebola control measures in rural and urban areas of Sierra Leone. PLoS Negl Trop Dis. 2018;12(6):e0006461.
Leach M. Time to put Ebola in context. Bull World Health Organ. 2010;88(7):481–560.
Roca A, Afolabi MO, Saidu Y, Kampmann B. Ebola: a holistic approach is required to achieve effective management and control. Allergy Clin Immunol. 2015;135(4):856–67.
Coltart CE, Lindsey B, Ghinai I, Johnson AM, Heymann DL. The Ebola outbreak, 2013–2016: old lessons for new epidemics. Philos Trans R Soc Lond B Biol Sci. 2017;372(1721):20160297.
Hersey S, Martel LD, Jambai A, Keita S, Yoti Z, Meyer E, Seeman S, Bennett S, Ratto J, Morgan O, Akyeampong MA. Ebola virus disease—sierra leone and guinea, August 2015. Morb Mortal Wkly Rep. 2015;64(35):981–4.
Muzembo BA, Ntontolo NP, Ngatu NR, Khatiwada J, Ngombe KL, Numbi OL, Nzaji KM, Maotela KJ, Ngoyi MJ, Suzuki T, Wada K. Local perspectives on Ebola during its tenth outbreak in DR Congo: a nationwide qualitative study. PLoS ONE. 2020;15(10):e0241120.
United States Agency for International Development (USAID). The KAP Survey Model (Knowledge, Attitudes, and Practices). Available online: https://www.spring-nutrition.org/publications/toolsummaries/kap-survey-model-knowledge-attitudesand-practices (Accessed on 22 May 2020).
Raven J, Wurie H, Witter S. Health workers’ experiences of coping with the Ebola epidemic in Sierra Leone’s health system: a qualitative study. BMC Health Serv Res. 2018;18:1–9.
Ansumana R, Keitell S, Roberts GM, Ntoumi F, Petersen E, Ippolito G, Zumla A. Impact of infectious disease epidemics on tuberculosis diagnostic, management, and prevention services: experiences and lessons from the 2014–2015 Ebola virus disease outbreak in West Africa. Int J Infect Dis. 2017;56:101–4.
World Health Organization. WHO: Ebola response roadmap update 26 September 2014.
World Health Organization. WHO: Ebola situation report 4 November 2015.
Evans DK, Goldstein M, Popova A. Health-care worker mortality and the legacy of the Ebola epidemic. Lancet Glob Health. 2015;3(8):e439–40.
Parpia AS, Ndeffo-Mbah ML, Wenzel NS, Galvani AP. Effects of response to 2014–2015 Ebola outbreak on deaths from malaria, HIV/AIDS, and tuberculosis, West Africa. Emerg Infect Dis. 2016;22(3):433.
Okamoto F, Nishikawa Y, Twalla Y, Nakayama T, Masai S. Ebola outbreak in Uganda: patient values and preferences. Lancet. 2022;400(10367):1925–6.
Somali Government, Ministry of Health (2022), Somalia National Ebola Preparedness and Response Plan. https://reliefweb.int/report/somalia/somalia-national-ebola-preparedness-and-response-plan.
Tulenko, K.; Bile, K.; Dlima, N. Somali Health Regulatory Landscape Report; MOH: Mogadishu, Somalia, 2021. Health-Sector-Strategy-Plan-III.pdf
MoH Somali Service Availability and Readiness Assessment Report. Somali Health Authority online:https://www.humanitarianresponse.info/sites/www.humanitarianresponse.info/files/documents/files/somali_country_report_final_draft_30dec2016-.pdf.
Dahie HA, Mohamoud JH, Adam MH, Garba B, Dirie NI, Sh. Nur MA, Mohamed FY. COVID-19 vaccine coverage and potential drivers of vaccine uptake among healthcare workers in Somalia: a cross-sectional study. Vaccines. 2022;10(7):1116.
Feleke BT, Wale MZ, Yirsaw MT. Knowledge, attitude and preventive practice towards COVID-19 and associated factors among outpatient service visitors at Debre Markos compressive specialized hospital, north-west Ethiopia, 2020. PLoS ONE. 2021;16(7):e0251708.
Skinner CJ. Probability proportional to size (PPS) sampling. Wiley StatsRef: Statistics Reference Online. 2014:1-5.
Ahmad A, Khan MU, Jamshed SQ, Kumar BD, Kumar GS, Reddy PG, Ajmera S. Are healthcare workers ready for Ebola? An assessment of their knowledge and attitude in a referral hospital in South India. J Infect Dev Ctries. 2016;10(07):747–54.
Dauda Goni M, Hasan H, Naing NN, Wan-Arfah N, Zeiny Deris Z, Nor Arifin W, Abubakar BA. Assessment of knowledge, attitude and practice towards prevention of respiratory tract infections among Hajj and Umrah Pilgrims from Malaysia in 2018. Int J Environ Res Public Health. 2019;16(22):4569.
Kanu S, James PB, Bah AJ, Kabba JA, Kamara MS, Williams CE, Kanu JS. Healthcare workers’ knowledge, attitude, practice and perceived health facility preparedness regarding COVID-19 in Sierra Leone. J Multidiscip Healthc. 2021;14:67–80.
Kassie BA, Adane A, Tilahun YT, Kassahun EA, Ayele AS, Belew AK. Knowledge and attitude towards COVID-19 and associated factors among health care providers in Northwest Ethiopia. PLoS ONE. 2020;15(8):e0238415.
Salman M, Mustafa Z, Asif N, Zaidi HA, Shehzadi N, Khan TM, Saleem Z, Hussain K. Knowledge, attitude and preventive practices related to COVID-19 among health professionals of Punjab province of Pakistan. J Infect Dev Ctries. 2020;14(07):707–12.
Yu PL, Ab Ghafar N, Adam M, Goh HC. Understanding the human dimensions of recycling and source separation practices at the household level: an evidence in Perak, Malaysia. Sustainability. 2022;14(13):8023.
Nguyen HB, Nguyen THM, Tran TTT, Vo THN, Tran VH, Do TNP, et al. Knowledge, attitudes, practices, and related factors towards COVID-19 prevention among patients at University Medical Center Ho Chi Minh City, Vietnam. Risk Manag Healthc Policy. 2021;14:2119–32. https://doi.org/10.2147/RMHP.S305959.
Turner RC, Carlson L. Indexes of item-objective congruence for multidimensional items. Int J Test. 2003;3(2):163–71.
Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3(1):1–8.
Hosmer Jr DW, Lemeshow S, Sturdivant RX. Applied logistic regression. Hoboken, New Jersey: John Wiley & Sons; 2013.
Eastern Mediterranean Regional Office World Health Organization. https://www.emro.who.int/pandemic-epidemic-diseases/news/ramping-up-ebola-preparedness-to-ensure-early-detection-and-response.html. 2018. Ramping up Ebola preparedness to ensure early detection and response.
Mohamud AK, Ahmed OA, Mohamud AA, Dirie NI. Magnitude of opportunistic infections and associated factors among adult people living with human immune deficient virus on art at selected public hospital, mogadishu somalia: cross-sectional study. Ann Med Surg. 2023;85(7):3364.
Rock RB, Sutherland WM, Baker C, Williams DN. Extrapulmonary tuberculosis among Somalis in Minnesota. Emerg Infect Dis. 2006;12(9):1434.
Jeele MO, Addow RO, Adan FN, Jimale LH. Prevalence and risk factors associated with hepatitis B and hepatitis C infections among patients undergoing hemodialysis: a single-centre study in Somalia. Int J Nephrol. 2021;2021:1555775.
Dirie AM, Çolakoğlu S, Abdi BM, Shire AM, Abdinur AH. The prevalence of HIV among tuberculosis patients in Benadir, Somalia. Retrospective multi-center study. Ann Med Surg. 2022;78:103793.
Mohamud AK, Ahmed OA, Mohamud AA, Dirie NI. Prevalence of and factors associated with depression among adult patients living with HIV/AIDs undergoing ART unit in Banadir hospital, Mogadishu Somalia. BMC Psychiatry. 2023;23(1):1–8.
Hassan-Kadle MA, Osman MS, Ogurtsov PP. Epidemiology of viral hepatitis in Somalia: systematic review and meta-analysis study. World J Gastroenterol. 2018;24(34):3927.
Mohamud AK, Ahmed OA, Ali IA, Dirie NI. Demographical, clinical, and complication differences between vaccinated and unvaccinated hospitalized children with measles in Mogadishu Somalia: a hospital-based retrospective cohort study. Ann Med Surg. 2023;85(5):1550.
Cénat JM, Rousseau C, Dalexis RD, Bukaka J, Derivois D, Balayulu-Makila O, Birangui JP. Knowledge and misconceptions related to the Ebola virus disease among adults in the democratic republic of the congo: the venomous snake under the table of prevention. Public Health in Practice. 2021;2:100178.
Iliyasu G, Ogoina D, Otu AA, Dayyab FM, Ebenso B, Otokpa D, Rotifa S, Olomo WT, Habib AG. A multi-site knowledge attitude and practice survey of Ebola virus disease in Nigeria. PLoS ONE. 2015;10(8):e0135955.
James PB, Wardle J, Steel A, Adams J. An assessment of Ebola-related stigma and its association with informal healthcare utilisation among Ebola survivors in Sierra Leone: a cross-sectional study. BMC Public Health. 2020;20(1):1–2.
Adongo PB, Tabong PT, Asampong E, Ansong J, Robalo M, Adanu RM. Beyond knowledge and awareness: addressing misconceptions in Ghana’s preparation towards an outbreak of Ebola virus disease. PLoS ONE. 2016;11(2):e0149627.
Acknowledgements
The paper acknowledges all healthcare workers participating in the study and health administration officials for their facilitation.
Funding
N/A.
Author information
Authors and Affiliations
Contributions
All authors developed the study design and data collection tool by reviewing previous literature. Khalif has a research idea, analyzed the data, wrote a report, and arranged data collection of Puntland state and time frame. Diriye arranged the data collection of the Banadir region. Pamansiri drafted a manuscript and supported the time frame. Ikran arranged the data collection of Jubaland state, Omar arranged the data collection of Galmudug state, Abdulrahman arranged the data collection of Hirshabelle state, and Ahmed arranged the data collection of Southwest state.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study aligns with the rules and regulations of the World Medical Association Declaration of Helsinki. Ethical approval was obtained from the Human Research review board of the Somali Ministry of Health and Human Service. The Human Research review board of the Somali Ministry of Health and Human Service approved the survey procedure including obtaining informed verbal consent with approval IRB number: (MOH&HS/DGO/1931/NOV2022). All eligible respondents explained the study objective and requested participation, and informed verbal consent was obtained from participating healthcare workers (HCWs). Consequently, all participants were informed that they had a full right to discontinue the interview without penalty. Confidentiality was kept, the online questionnaire was anonymous, and data was presented without reflecting individual information.
Consent for publication
Not applicable.
Competing interests
All authors declared that they do not have any compensation.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mohamud, A.K., Ali, I.A., Ali, A.I. et al. Assessment of healthcare workers' knowledge and attitude on Ebola virus disease in Somalia: a multicenter nationwide survey. BMC Public Health 23, 1650 (2023). https://doi.org/10.1186/s12889-023-16562-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-16562-2