Abstract
Background
Abnormal birth weight – small for gestational age (SGA) and large for gestational age (LGA) – are important indicators for newborn health. Due to changes in lifestyle in recent decades, it is essential to keep up-to-date with the latest information on maternal factors linked to abnormal birth weight. The aim of this study is to investigate SGA and LGA in relation to maternal individual, lifestyle and socioeconomic characteristics. .
Methods
This is a register-based cross-sectional study. Self-reported data from Sweden’s Salut Programme maternal questionnaires (2010–2014) were linked with records in the Swedish Medical Birth Register (MBR). The analytical sample comprised 5089 singleton live births. A Swedish standard method using ultrasound-based sex-specific reference curves defines the abnormality of birth weight in MBR. Univariable and multivariable logistic regressions were used to examine crude and adjusted associations between abnormal birth weights and maternal individual, lifestyle and socioeconomic characteristics. A sensitivity analysis, using alternative definitions of SGA and LGA under the percentile method, was undertaken.
Results
In multivariable logistic regression, maternal age and parity were associated with LGA (aOR = 1.05, CI = 1.00, 1.09) and (aOR = 1.31, CI = 1.09, 1.58). Maternal overweight and obesity were strongly associated with LGA (aOR = 2.28, CI = 1.47, 3.54) and (aOR = 4.55, CI = 2.85, 7.26), respectively. As parity increased, the odds of delivering SGA babies decreased (aOR = 0.59, CI = 0.42, 0.81) and preterm deliveries were associated with SGA (aOR = 9.46, CI = 5.67, 15.79). The well-known maternal determinants of abnormal birthweight, such as unhealthy lifestyles and poor socioeconomic factors, were not statistically significant in this Swedish setting.
Conclusions
The main findings suggest that multiparity, maternal pre-pregnancy overweight and obesity are strong determinants for LGA babies. Public health interventions should address modifiable risk factors, especially maternal overweight and obesity. These findings suggest that overweight and obesity is an emerging public health threat for newborn health. This might also result in the intergenerational transfer of overweight and obesity. These are important messages for public health policy and decision making.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Birth weight is a consequence of both foetal and maternal factors and an important indicator of intrauterine growth and newborn health. Abnormal birth weights, such as small for gestational age (SGA) and large for gestational age (LGA), are recognizable risk factors for neonatal morbidity [1, 2]. SGA newborns have subnormal intrauterine growth compared with newborns of the same gestational age and gender, while LGA is a sign of overgrowth [3]. Analysis of maternal causal associations and modifiable risk factors are important from a public health perspective (2). Deviations from expected birth weight have attracted much attention because scientific evidence indicates not only short-term effects, such as neonatal morbidity and mortality, but also adverse long-term effects on subsequent child growth and development, and possibly inter-generational health consequences [4,5,6].
Epidemiological studies on birth weight have reported that the prevalence of large babies (LGA) has increased over the last few decades in some European countries, including Sweden [5, 7, 8]. More importantly, LGA babies are prone to a condition called macrosomia which is excessive growth beyond a birth weight threshold of 4000 g. Macrosomia is a risk factor for several complications such as shoulder dystocia, Erb’s palsy, fractures of the clavicle or humerus, neonatal asphyxia, hypoglycaemia and hyperbilirubinemia, etc. [9]. Moreover, mothers of these babies are at an increased risk of Caesarean section, obstructed labour, haemorrhage, perineal trauma and maternal complications [9].
SGA babies, on the other hand, have a considerably higher risk of morbidity and mortality in neonatal and post-neonatal periods compared to normal weight babies [1, 10, 11]. The risks are even higher if newborns have both preterm and SGA conditions [10]. These babies have a high risk of several neonatal morbidities such as infections, hypothermia, hypoglycaemia, perinatal respiratory depression, and poor feeding. In addition to these adverse health outcomes, SGA babies can develop childhood growth retardation such as stunting and wasting [6].
Previous newborn studies have shown that birth weight is influenced by maternal health, nutrition, genetics, and environmental and lifestyle factors during pregnancy [12]. Thus, the pregnancy period offers a window of opportunity for health interventions which can potentially benefit both maternal and child health. However, in the Swedish setting, little is known about the prevalence of abnormal birth weight, and associations with pre-pregnancy maternal conditions such as lifestyle and socioeconomic factors.
Lifestyle behaviours have changed considerably in recent decades [13]. Hence there is a need to update knowledge regarding associations between maternal characteristics and newborn weight. For example, one Swedish study in 2013 found that the prevalence of overweight and obesity was high among expectant parents, and suggested that this could be associated with over-nutrition related health problems in newborns [14]. Another Swedish study showed that patterns of high body mass index (BMI) are transferred from parents to toddlers [15], thereby indicating that the intergenerational effects of high BMI deserve more attention. On the other hand, preterm and low birth weight is the most common cause of neonatal mortality in Sweden [16]. Our study will investigate both SGA and LGA as outcome measures to capture birth weight deviations at both ends.
Further knowledge of association between maternal characteristics and abnormal birth weight will inform understanding of intergenerational patterns, and ways of preventing child morbidities and mortalities [17,18,19]. The aim of this study is to investigate both SGA and LGA in relation to maternal individual, lifestyle and socioeconomic characteristics. Data analysed here cover the maternal pre-pregnancy stage through to childbirth. The study sample includes five years of birth registry data representative of a regional population in Sweden.
Methods
Study design and participants
This is a registry based cross-sectional study. Data from the Salut Child Health Promotion Programme in Region Västerbotten, northern Sweden, are enriched with individual level data from the National Board of Health and Welfare [14, 20, 21]. The Salut Programme is a multisector, family centred intervention aimed at reaching all children aged 0–18 and their parents, starting with the parents-to-be before the pregnancy. This has resulted in a prospective longitudinal data collection from 2009 to the present-day. As part of this program, all pregnant women in the Region Västerbotten were provided with a self-reported maternal health and lifestyle questionnaire before their first antenatal care visit. The response rate for the antenatal data collection is around 75%. On average women answer the first antenatal questionnaire at about 11 week gestation.
Data structure
The study sample is derived from a merged longitudinal dataset constructed to follow families from pregnancy and through childhood. The Salut antenatal questionnaire which includes important information on lifestyle is enriched by a selection of variables from the MBR hosted by the National Board of Health and Welfare in Sweden. The maternal data from Salut Programme (2010 to 2014) was linked with Swedish Medical Birth Register (using personal identity numbers). A final sample of 5089 singleton newborns and 4683 mothers was obtained for the analysis. Variables selected from the self-reported maternal questionnaire included age at pregnancy, height, pre-pregnancy weight, parity, physical activity, alcohol consumption, employment status and education level. The variables used from the MBR were birth weight, gestational week at birth, maternal smoking and snuffing tobacco at enrolment. See Fig. 1.
The best estimates for dating gestational age at birth were obtained either by the first or second trimester, or the traditional last menstrual period (LMP) method. Gestational dating using ultrasound is offered to all pregnant women in Sweden; about 97% of all pregnant women agree to this. In the final merged dataset, the variables maternal BMI, smoking, and employment had 8.5%, 3.3% and 4.4% of missing data respectively. For the remaining variables missing data was ≤ 2%; maternal age and parity had complete data.
Dependent variables
Two methods were used to calculate SGA and LGA. They are the percentile method (< 10th & >90th percentile) and the standard deviation method (mean ± 2 Standard deviations) [22, 23]. The second method was used in line with the Swedish MBR. This was calculated according to the ultrasound-based sex-specific Swedish reference curve for normal foetal growth [23]. The percentile methods were used in a sensitivity analysis. Both SGA and LGA for both methods (percentile and standard deviation ) were categorised as binary (SGA or non SGA and LGA or non-LGA).
Independent variables
General characteristics
Pregnant women’s age, height and weight were self-reported in the maternal questionnaires just prior to the first antenatal care visit. Maternal pre-pregnancy BMI was calculated by the formula: BMI = kg/m2 = a person’s self-reported weight in kilograms divided by their self-reported height in squared metre. According to WHO’s definition, BMI is classified into underweight (< 18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obesity (≥ 30 kg/m2).
Parity is the number of previous deliveries which is further grouped into primiparity (first pregnancy), multiparity (2nd to 4th pregnancy) and grand multiparity (5th or more). Gestational age at the time of delivery was defined as preterm delivery (< 37 week), term delivery (37–41 week) and post-term delivery (≥ 42week). The offspring’s sex characteristics (male, female) were used in the classification of SGA and LGA, and considered in the data analysis.
Lifestyle characteristics
Data about maternal tobacco smoking and snuffing were extracted from the MBR and coded as yes/no questions at the time of enrolment. Data for physical activity and alcohol consumption originated from the Salut maternal questionnaires. This information reflected women’s lifestyle up to 12 months before their pregnancy.
To estimate individual alcohol risk, the Alcohol Use Disorders Identification Test (AUDIT, approved by WHO) was used in the Salut maternal questionnaires to measure the level of alcohol consumption, drinking behaviours and alcohol-related problems within 12 months before the current pregnancy [24]. The AUDIT score ≤ 5 is categorised as non-risky and a score > 5 as risky alcohol consumption. These variables: smoking, snuffing tobacco and alcohol consumption were encoded as binary variables, i.e., having the risk behaviour or not.
The level of physical activity was measured by total duration spent on physical activities during a week. As per WHO recommendation, at least 150 min of moderate-intensity physical activity throughout the week should be maintained for good health in adults, 18–64 years of age, including pregnant women [25]. The level of physical activity was re-coded as hours per week as a continuous variable.
Socioeconomic characteristics
Post-secondary education or higher (> 12 years of education) was classified as high education and secondary school level or lower (≤ 12 years of education) as medium or low education. Employment status was categorised as unemployed or employed (either full-time or part-time). These socioeconomic variables were also encoded as binary variables for the analysis.
Data analysis
Firstly, maternal characteristics and delivery outcomes were summarised in descriptive tables using numbers and proportions. Secondly, birth weights in relation to maternal pre-pregnancy BMI and parity were illustrated by stacked bar graphs. Thirdly, univariable logistic regressions estimated with Generalized Estimating Equations (to handle correlation between siblings) using an exchangeable correlation structure were performed to identify crude associations between SGA and LGA and each maternal characteristic. Lastly, multivariable logistic regression estimated with Generalized Estimating Equations was executed including those variables for which the p-value < 0.05 in the crude analysis. The statistical associations between variables were reported as odds ratios (OR) with 95% confidence intervals (CI). The statistical threshold for level of significance was set to 0.05. All the statistical analyses were performed using Stata16.0 Software.
Results
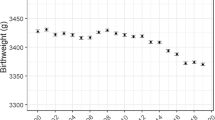
In this sample, the mean birth weights of newborns were 3626 g (Standard deviation (SD): 541 g) for males and 3515 g (SD: 506 g) for females. The median gestational age at delivery was 40 weeks (range 25–43) and male-female ratio was 51.2: 48.8. The median birth weight at 40-weeks were 3747 g and 3590 g for male and female newborns. Newborn with macrosomia (> 4000 g) accounted for 18.8% of the sample but low birth weight (< 2500 g) newborns were only 2.8%. The birth weight for gestational age calculations as per Swedish national standard result in 2.8%, 95.6% and 1.6% for LGA, AGA and SGA, respectively.
Around 86.8% of pregnant women were within the age range of 20–35 years. Teenage pregnancies (< 20 years old) were only 0.9% while pregnancies > 35 years of age accounted for 12.4% of the sample. Primiparity contributed to 44.5% of the sample. Almost 30% of women in this local sample were either overweight or obese (19.7% overweight and 9.0% obese), 67.3% of the women had normal BMI and 4% were underweight. Preterm, term and post-term deliveries comprised 4.3%, 88.0% and 7.7%, of the sample respectively.
Regarding maternal lifestyle characteristics, only 1.5% of the women smoked and 3.8% had snuff (tobacco) using behaviour at the enrolment to AN care. According to the AUDIT score, 6.9% of the pregnant mothers had a risk behaviour regarding alcohol consumption during 12 months before the enrolment to ANC. The recommended physical exercise level (150 min/week) was not achieved by 36.1% of the pregnant mothers; 86.2% of the study population were employed and 61.7% had more than 12 years of education. See Table 1.
The following bar graphs illustrate increasing LGA and decreasing SGA with increasing maternal BMI and parity, as shown in Figs. 2 and 3. Note: missing data may affect the number of observations in each category.
Result from logistic regression analysis
Large for gestational age (LGA)
Older maternal age, parity, high BMI and physical activity showed statistically significant associations with LGA in univariable logistic regression. In the adjusted analysis, a one year increase in maternal age corresponded to an increased odds ratio of 5% for LGA (Adjusted odds ratio (aOR) = 1.05, CI = 1.00, 1.09). The odds for having LGA increased with each pregnancy, (aOR = 1.31, CI = 1.09, 1.58). Overweight and obesity compared with normal BMI group (reference) had significantly higher odds of having LGA, (aOR = 2.28, CI = 1.47, 3.54) and (aOR = 4.55, CI = 2.85, 7.26) respectively. The statistical association with physical activity was attenuated in the adjusted analysis. See Table 2.
Small for gestational age (SGA)
The univariable analysis showed that SGA had significant statistical associations with parity and preterm delivery. In the adjusted analysis, those results remained. The odds decreased for each pregnancy (aOR = 0.59, CI = 0.42, 0.81). The association of preterm birth with SGA was found with wide confidence interval (aOR = 9.46, CI = 5.67, 15.79) compared to normal term deliveries. The interpretation of the high odds ratio should be cautious, given the small number of observations with this criterion. See Table 2.
Sensitivity analysis
The large sample (i.e., 5089 newborns data from regional data collected over 5 years) allowed us to use the percentile method to define SGA and LGA [26]. In this method, SGA and LGA were defined as the newborns weighing < 10th percentile and > 90th percentile of the same gestational week and sex [27, 28]. The calculations were done with a gestational age and weight percentile calculator in Microsoft Excel [29]. This produced the percentile curve of birth weight and cut-off points for respective percentiles of the sample.
For the sensitivity analysis, the logistic regressions were executed with the SGA and LGA determined by the percentile method. The statistical associations with LGA were significant with parity and high BMI, but not with maternal age and physical activity. On the other hand, SGA had statistical association with parity, low BMI, preterm and smoking. Thus, maternal high BMI and parity produced the similar results in the sensitivity analysis. See Tables 3 and 4 for the sensitivity analysis using the WHO percentile method definition of SGA and LGA.
Discussion
The main finding was that the occurrence of LGA (2.8%) was more common than SGA (1.6%) in this sample of Swedish newborns. The high prevalence of macrosomia babies (18.8%) compared to the low birth weight (2.8%) further supports this fact. The international standard of newborn weight in the multinational newborn cross-sectional study of the INTERGROWTH21st Project reported the 50th percentile birth weight of newborns at 40-week gestational age as 3380 g for males and 3260 g for females [28]. The corresponding median values of birth weight at 40-weeks in this local sample were 3747 g and 3590 g for male and females respectively. This means that newborn babies in our sample had, on average, a 349 g higher birth weight than the international standard. But there is need for cautious interpretation because the sample in INTERGROWTH study excluded mothers with extreme age, height and BMI.
In high income countries like Sweden, maternal over-nutrition is more common than under-nutrition. This claim is supported by the percentage of maternal BMI categories which are largely occupied by overweight (19.7%), and obesity (9%) compared to the underweight (4%). It is also reasonable that overweight and obese mothers deliver large babies [30]. Overweight and obesity is one of the top uprising public health concerns due to a global increasing trend in mean BMI since 1980 [31, 32]. Associations between toddlers’ and parents’ BMI is shown in another Swedish study [15]. This is indicative that maternal pre-pregnancy overweight and obesity is increasingly becoming a public health problem in maternal and child health in Sweden.
Maternal overweight and obesity are modifiable risk factors and largely preventable with diet, lifestyle, and weight control measures [33]. Thus, there is a window of opportunity in the pre-conception phase for reducing the attributable risk of LGA through protective lifestyle behaviours, such as eating a healthy diet, promoting physical activity, and weight control measures where appropriate. As a prevention strategy of LGA, weight loss and lifestyle interventions should target overweight and obese women during preconception care, or more ideally before childbearing i.e., promoting healthy eating and physical activity during childhood and adolescence. Since some childhood nutritional status originates in the foetal period, this suggests that public health interventions need to focus on the continuum of maternal and child health care, starting at pre-conception.
The Salut program holds a continuous data collection over decades. This is an advantage for monitoring the lifestyle and socioeconomic conditions of parents-to-be in the Swedish population and the relationship with child health. One of the most important findings was that there was no significant statistical association between abnormal birth weight and the well-known maternal determinants of abnormal birthweight such as unhealthy lifestyle habits and poor socioeconomic factors. This negative finding indicates that these factors are less prominent in the Swedish context. This could be a sign of over nutrition which has become a new challenge re-directing some attention from health problems associated with low socioeconomic status.
There is strong scientific evidence that smoking can cause preterm deliveries and decreased birth weight [34,35,36]. In Sweden daily smoking rates in adults have declined over time according to the latest report from Public Health Agency [37]. The report says 6% of men and women smoked daily in 2021. Snuff use among 16–84-year-old women is estimated at 6% in 2021. In our sample, only a small proportion of respondents (1.5% smoking and 3.8% snuffing) reported these unhealthy lifestyle characteristics. This may explain why no associations between smoking and SGA were found.
In terms of socioeconomic characteristics, abnormal birth weights had no significant statistical association with maternal education level and employment. In general, education is a strong determinant of low-birth-weight outcomes. Most pregnant women in the sample had post-secondary education level or higher (> 12 years of education), and the percentage of women who had less than 9 years of school education in the maternal questionnaire was < 1% (not mentioned in the tables). This might be a reason why education does not determine abnormal birth weight in this Swedish setting.
Indeed, moderate physical exercise is necessary for healthy lifestyle whereas the sedentary lifestyle (low physical activity) is highly associated with overweight and obesity. In our analysis, the physical activity hours per week had a significant association with a decreased LGA in the univariable analysis. Yet the statistical association was diminished in adjusted analysis. This could be due to the strong mediation effect of overweight and obesity in the association pathway. From a public health perspective, unhealthy lifestyles are considered potentially modifiable by means of public health interventions. The health services should continue to provide a good family planning service, adequate preconception care, and proper antenatal care, giving women opportunities to make lifestyle changes, reduce modifiable risk factors and optimise medical conditions [38].
This study further supports relationships between maternal factors and abnormal birth weights. Among the independent variables, the maternal age, parity, pre-pregnancy BMI and preterm deliveries were prominent factors associated with abnormal birth weight in newborns. But recognised health determinants, such as lifestyle and socioeconomic factors, did not have any significant associations with abnormal birth weight in this Swedish population.
Strengths and limitations
This study used a large sample collected over a 5 year period. A wide range of maternal variables were used for analysing abnormal birth weights on both ends (SGA and LGA). The exposure was measured at the early time of pregnancy which reflects the lifestyle of women in reproductive age in a general population, and the outcomes were measured at the time of delivery. However, only a small proportion of the study participants had an unhealthy lifestyle, i.e., 1.5% smoking, 3.8% snuffing tobacco and 6.9% risky alcohol consumption. Thus, the statistical power for analysis of these specific lifestyle characteristics was low. Further research with larger sample sizes, or focused study designs for specific lifestyles, is needed to increase knowledge about maternal lifestyle and the newborn birth weight deviances.
Since the self-reported questionnaires were used in data collection, there was a slight chance of a recall bias from the respondents, for instance, under-reporting of unhealthy lifestyles and women’s body weight. Such conditions could result in an information bias and might lead to an under-estimation of the associations between maternal characteristics and abnormal birth weights. Moreover, pregnant women often make positive lifestyle changes during pregnancy period which might reduce the risk of abnormal birthweight outcomes.
Maternal morbidity during pregnancy and genetic factors have direct relevance for birth weight in addition to maternal lifestyle, social and environmental factors. For instance, maternal health conditions such as gestational diabetes mellitus, and excessive gestational weight gain could lead to over-nutrition of the foetus resulting in a LGA baby at birth [39]. Small-sized newborns and preterm births could be manifested by maternal complications such as pre-eclampsia, pregnancy hypertension and other medical diseases [40]. However, in this study, such maternal morbidity conditions could not be included in the analysis due to data limitations.
Conclusion
The main findings in this research suggest that multiparity, maternal pre-pregnancy overweight or obesity are strong determinants for LGA babies. Public health interventions should address modifiable risk factors especially maternal overweight and obesity. For public health policy level decision making, our study highlights that overweight and obesity is a new public health threat affecting newborn health, and that this might also convey an intergenerational transfer of overweight and obesity.
Data availability
The datasets presented in this article are not readily available because Region Västerbotten originally collected the data for a child health survey (https://www.regionvasterbotten.se/salut). We accessed data for the present study after approval from both the Region Västerbotten and the Ethical Vetting Board. The data are not publicly available but access for replication analyses is possible. Requests to access the datasets should be directed to (https://www.regionvasterbotten.se/salut) or to marie.lindkvist@umu.se.
Abbreviations
- AGA:
-
Average for gestational age
- AUDIT:
-
Alcohol Use Disorders Identification Test
- aOR:
-
Adjusted odds ratios
- BMI:
-
Body Mass Index
- CI 95%:
-
Confidence interval
- LGA:
-
Large for gestational age
- MBR:
-
Medical Birth Register
- SD:
-
Standard deviation
- SGA:
-
Small for gestational age
- WHO:
-
World Health Organisation
References
Ludvigsson JF, Lu D, Hammarstrom L, Cnattingius S, Fang F. Small for gestational age and risk of childhood mortality: a swedish population study.(Research Article)(Report). PLoS Med. 2018;15(12):e1002717.
Mendez-Figueroa H, Truong VTT, Pedroza C, Chauhan SP. Large for gestational age infants and adverse outcomes among uncomplicated pregnancies at term. Am J Perinatol. 2017;34(7):655–62.
Physical status. The use and interpretation of anthropometry: report of a WHO expert committee. Geneva: World Health Organization; 1995.
Sparano S, Ahrens W, Henauw S, Marild S, Molnar D, Moreno L, et al. Being Macrosomic at Birth is an independent predictor of overweight in children: results from the IDEFICS Study. Matern Child Health J. 2013;17(8):1373–81.
José GBD, Fredrik A, Barbro D, Maria L. Obesity rates in two generations of Swedish women entering pregnancy, and associated obesity risk among adult daughters. Sci Rep. 2015;5(1).
Christian P, Lee SE, Donahue Angel M, Adair LS, Arifeen SE, Ashorn P, et al. Risk of childhood undernutrition related to small-for-gestational age and preterm birth in low- and middle-income countries. Int J Epidemiol. 2013;42(5):1340–55.
Ørskou J, Kesmodel U, Henriksen TB, Secher NJ. An increasing proportion of infants weigh more than 4000 grams at birth. Acta Obstet Gynecol Scand. 2001;80(10):931–6.
Surkan PJ, Hsieh C-C, Johansson ALV, Dickman PW, Cnattingius S. Reasons for increasing trends in large for gestational age births. Obstetrics and gynecology (New York 1953). 2004;104(4):720-6.
Najafian M, Cheraghi M. Occurrence of Fetal Macrosomia Rate and Its Maternal and Neonatal Complications: A 5-Year Cohort Study. ISRN Obstet Gynecol. 2012;2012.
Katz J, Lee ACC, Kozuki N, Lawn JE, Cousens S, Blencowe H, et al. Mortality risk in preterm and small-for-gestational-age infants in low-income and middle-income countries: a pooled country analysis. The Lancet (British edition). 2013;382(9890):417–25.
Lee ACC, Kozuki N, Cousens S, Stevens GA, Blencowe H, Silveira MF, et al. Estimates of burden and consequences of infants born small for gestational age in low and middle income countries with INTERGROWTH-21 st standard: analysis of CHERG datasets. BMJ. 2017;358:j3677.
Bennett CJ, Walker RE, Blumfield ML, Ma J, Wang F, Wan Y, et al. Attenuation of maternal weight gain impacts infant birthweight: systematic review and meta-analysis. J Dev origins health disease. 2019;10(4):387–405.
Borodulin K, Laatikainen T, Juolevi A, Jousilahti P. Thirty-year trends of physical activity in relation to age, calendar time and birth cohort in finnish adults. Eur J Pub Health. 2008;18(3):339–44.
Edvardsson K, Lindkvist M, Eurenius E, Mogren I, Small R, Ivarsson A. A population-based study of overweight and obesity in expectant parents: socio-demographic patterns and within-couple associations. BMC Public Health. 2013;13(1):923.
Lindkvist M, Ivarsson A, Silfverdal SA, Eurenius E. Associations between toddlers’ and parents’ BMI, in relation to family socio-demography: a cross-sectional study. BMC Public Health. 2015;15(1):1252.
Hjern A. Children’s health: Health in Sweden: the National Public Health Report 2012. Chapter 2 Scandinavian journal of public health. 2012;40(9suppl):23–41.
Oteng-Ntim E, Varma R, Croker H, Poston L, Doyle P. Lifestyle interventions for overweight and obese pregnant women to improve pregnancy outcome: systematic review and meta-analysis. BMC Med. 2012;10:47.
Moholdt T, Hawley JA. Maternal lifestyle interventions: targeting Preconception Health. Trends in Endocrinology & Metabolism; 2020.
Pfinder M, Kunst AE, Feldmann R, van Eijsden M, Vrijkotte TGM. Preterm birth and small for gestational age in relation to alcohol consumption during pregnancy: stronger associations among vulnerable women? Results from two large western-european studies. BMC Pregnancy Childbirth. 2013;13(1):49.
Edvardsson K, Ivarsson A, Eurenius E, Garvare R, Nyström ME, Small R, et al. Giving offspring a healthy start: parents’ experiences of health promotion and lifestyle change during pregnancy and early parenthood. BMC Public Health. 2011;11(1):936.
Eurenius E, Lindkvist M, Sundqvist M, Ivarsson A, Mogren I. Maternal and paternal self-rated health and BMI in relation to lifestyle in early pregnancy: the Salut Programme in Sweden. Scand J Public Health. 2011;39(7):730–41.
de Onis M, Habicht J-P. Anthropometric Reference Data for International Use: recommendations from a who Expert Committee. FoodNutr Bull. 1997;18(2):1–12.
Maršál K, Persson PH, Larsen T, Lilja H, Selbing A, Sultan B. Intrauterine growth curves based on ultrasonically estimated foetal weights. Acta Paediatr. 1996;85(7):843–8.
Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT: the Alcohol Use Disorders Identification Test: guidelines for use in primary health care. World Health Organization; 2001.
Global recommendations on. physical activity for health, World Health Organisation. 2010.
Mikolajczyk RTMD, Zhang JDP, Betran APMD, Souza JPMD, Mori RMD, Gülmezoglu AMMD, et al. A global reference for fetal-weight and birthweight percentiles. The Lancet (British edition). 2011;377(9780):1855–61.
M.de Onis M, Habicht J-P. Anthropometric reference data for international use: recommendations from a World Health Organization expert committee. Am J Clin Nutr. 1996;64(4):650.
Villar JP, Ismail LCP, Victora CGP, Ohuma EOM, Bertino EP, Altman DGP, et al. International standards for newborn weight, length, and head circumference by gestational age and sex: the newborn cross-sectional study of the INTERGROWTH-21st Project. The Lancet (British edition). 2014;384(9946):857–68.
Mikolajczyk RT, Zhang J, Betran AP, Souza JP, Mori R, Gülmezoglu AM, et al. A global reference for fetal-weight and birthweight percentiles. The Lancet (British edition). 2011;377(9780):1855–61.
Gaudet L, Ferraro ZM, Wen SW, Walker M. Maternal Obesity and Occurrence of Fetal Macrosomia: A Systematic Review and Meta-Analysis. Biomed Res Int. 2014;2014.
Finucane MM, Stevens GA, Farzad Far F, Riley LM, Ezzati M, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. The Lancet (British edition). 2011;377(9765):557–67.
Caman OK, Calling S, Midlöv P, Sundquist J, Sundquist K, Johansson S-E. Longitudinal age-and cohort trends in body mass index in Sweden–a 24-year follow-up study. BMC Public Health. 2013;13(1):893.
Gotthelf L, Chen Y-T, Rajagopalan S, Wu EC-T, Doshi I, Addy C. High intensity lifestyle intervention and long-term impact on weight and clinical outcomes. PLoS ONE. 2018;13(4):e0195794–e.
Wisborg K, Henriksen TB, Hedegaard M, Jergen N. Smoking during pregnancy and preterm birth. BJOG: An International Journal of Obstetrics & Gynaecology. 1996;103(8):800–5.
Ko T-J, Tsai L-Y, Chu L-C, Yeh S-J, Leung C, Chen C-Y, et al. Parental smoking during pregnancy and its Association with Low Birth Weight, Small for Gestational Age, and Preterm Birth offspring: a birth cohort study. Pediatr Neonatology. 2014;55(1):20–7.
Juárez SP, Merlo J. Revisiting the effect of maternal smoking during pregnancy on offspring birthweight: a quasi-experimental sibling analysis in Sweden. PLoS ONE. 2013;8(4):e61734.
Adults’ use of tobacco and nicotine products— The Public Health Authority Sweden. 2022 [cited 2022 27.09.2022]. Available from: https://www.folkhalsomyndigheten.se/livsvillkor-levnadsvanor/andts/utveckling-inom-andts-anvandning-och-ohalsa/anvandning/tobaks--och-nikotinprodukters-utveckling/vuxnas-bruk-av-tobaks--och-nikotinprodukter/.
Grivell RBBM, Dodd JMPFDDUC, Robinson JBMBBBAOFF. The prevention and treatment of intrauterine growth restriction. Best Pract Res Clin Obstet Gynecol. 2009;23(6):795–807.
Yang Y, Wang Z, Mo M, Muyiduli X, Wang S, Li M, et al. The association of gestational diabetes mellitus with fetal birth weight. J Diabetes Complicat. 2018;32(7):635–42.
McCowan LME, Roberts CT, Dekker GA, Taylor RS, Chan EHY, Kenny LC, et al. Risk factors for small-for‐gestational‐age infants by customised birthweight centiles: data from an international prospective cohort study. BJOG: an international journal of obstetrics and gynaecology. 2010;117(13):1599–607.
Acknowledgements
The authors are grateful to all participating women and the healthcare professionals for their efforts with data collection and for the support received from Västerbotten County´s Competence Centre for Maternal and Child health care and the Västerbotten Public Health Unit. We would also like to acknowledge database manager Wolfgang Lohr’s contribution and valuable support.
Funding
The research group has financial support from Region Västerbotten and Umeå University.
Open access funding provided by Umea University.
Author information
Authors and Affiliations
Contributions
MWL and ML designed the study. MV and MWL prepared the data for analysis. EE and AI designed the data collections related to the Salut Programme. MWL analysed and interpreted the data in collaboration with ML. ET and SS provided technical inputs from obstetric and pediatric perspectives. MWL drafted the paper. All authors contributed to interpretation and editing of the manuscript, and all authors have read and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The main part of the study was approved by the Regional Ethical Review Board in Umeå, Sweden (Dnr 2010-63-31 M). A supplementary application for the present study has been approved (2017 / 401 − 32) to expand our regional data with national health data from the Medical Birth Register. The data collection and research methods used were in accordance with the guidelines mentioned in Ethical Review Act, Act (2003: 460). No human or animal experiment was included. Informed consent was obtained from all the participants for further usage of their personal data for research purpose.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lwin, M.W., Timby, E., Ivarsson, A. et al. Abnormal birth weights for gestational age in relation to maternal characteristics in Sweden: a five year cross-sectional study. BMC Public Health 23, 976 (2023). https://doi.org/10.1186/s12889-023-15829-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15829-y