Abstract
Background
In contrast to high-income countries where physical activity (PA), particularly leisure-time PA, has been shown to be protective against hypertension, few studies have been conducted in low- and middle-income countries. We examined the cross-sectional association between PA and hypertension prevalence among rural residents in Vietnam.
Methods
We used data collected in the baseline survey of a prospective cohort study, among 3000 people aged 40–60 years old residing in rural Khánh Hòa, Vietnam. Hypertension was defined as systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, or the use of antihypertensive medication. We assessed occupational PA and leisure-time PA using the Global Physical Activity Questionnaire. A robust Poisson regression model was used to investigate the associations, with adjustment for covariates.
Results
The prevalence of hypertension was 39.6%. After adjusting for socio-demographic and lifestyle-related variables, leisure-time PA was positively associated with hypertension prevalence (prevalence ratio [PR]: 1.03 per 10 MET-hour/week, 95% confidence interval [CI] 1.01–1.06). Occupational PA was inversely associated with hypertension prevalence (PR: 0.98 per 50 MET-hour/week, 95% CI = 0.96–0.996). After adjusting for BMI and other health-related variables, the association related to occupational PA became statistically non-significant, while the association related to leisure-time PA remained statistically significant.
Conclusion
In contrast to previous studies in high-income countries, we found that leisure-time PA was positively associated with hypertension prevalence and occupational PA was associated with a lower hypertension prevalence. This suggests that the association between PA and hypertension might differ depending on the context.
Similar content being viewed by others
Background
In an effort to mitigate the disease burden associated with hypertension [1], physical activity (PA), particularly leisure-time PA, has been studied extensively. It was identified as a protective factor against hypertension development [2]. For example, a meta-analysis of 29 prospective cohort studies showed that the hypertension risk was reduced by 6% (relative risk [RR]: 0.94; 95% confidence interval [CI]: 0.92–0.96) for each 10 metabolic equivalent of task [MET]-hour/week increase in leisure-time PA [3].
In contrast to the robust inverse associations observed between leisure-time PA and hypertension, findings on the association between occupational PA and hypertension have been conflicting. Meta-analyses by Huai et al. and Liu et al. did not find any evidence of a significant association [3, 4]. Moreover, some studies even reported higher risk/odds of hypertension among those who engaged in heavy occupational PA [5], while other studies have suggested that occupational PA is associated with a lower hypertension risk [6, 7].
This study was designed to extend the previous studies by examining the association between PA and the prevalence of hypertension in rural Vietnam with a special focus on the differential association between leisure-time and occupational PA. There are several reasons we believe this study is important. First, previous evidence on this topic is mostly derived from high-income countries and few studies have been conducted in low- and middle-income countries (LMICs), even though these countries have a high burden of hypertension [8, 9]. For example, in Vietnam, there was a rapid increase in the number of adults with hypertension, from 4.5 million in 1975 to 15.2 million in 2015 [10]. Second, people in LMICs, particularly those living in rural areas, might not engage in leisure-time PA as much as people in high-income countries do while they might engage in occupational PA much more than people in high-income countries. Thus, the PA–hypertension association in LMICs might not be necessarily similar to those observed in high-income countries [11, 12]. Interestingly, in a prospective cohort study in Mexico, higher moderate to vigorous PA (MVPA) at the workplace was associated with a lower hypertension risk [13], which contrasted with the observations in high-income countries.
Therefore, this study aimed to examine the association between PA and the prevalence of hypertension among middle-aged people in a rural area of Khánh Hòa province, Vietnam with a special focus on possible differences between occupational PA and leisure-time PA. We hypothesized that occupational PA is more strongly inversely associated with hypertension prevalence compared to leisure-time PA in our study setting.
Methods
Study setting and design
Khánh Hòa province, situated on the south-central coast of Vietnam, has a population of 1.24 million, with 57.6% of them residing in rural areas. The monthly average income per capita is 3.153 million Vietnamese dong (VND), or approximately 135 USD [14].
The Khánh Hòa Cardiovascular Study (KHCS) is an ongoing prospective cohort study that investigates the determinants of cardiovascular diseases (CVDs) in Vietnam. We selected participants from eight communes in Cam Lâm district, a rural area of Khánh Hòa province, using purposive sampling [15, 16]. The affluence level of these communes was considered average for rural Vietnam.
The baseline survey was conducted between June 2019 and June 2020. The CHC staff members created a list of 6,446 eligible individuals who were aged 40–59 years old at the time of recruitment. Of them, we invited 3,597 individuals to participate in the study until we had recruited 3000 participants (consent rate: 83.4%). We trained staff members of the Pasteur Institute in Nha Trang (PINT) with field survey experience before they collected information on lifestyle and health-related variables using a questionnaire in face-to-face interviews, and anthropometric and biochemical measurements. The detailed information of the study is available elsewhere [17, 18].
The ethical approvals were obtained at the Research Ethics Committee of the National Center for Global Health and Medicine (NCGM) (approval number: NCGM-G-003172-03) and equivalent committees at the University of Tokyo (2021007NI) and the Pasteur Institute in Nha Trang, Vietnam (02/2019/HDDD-IPN). Participants in the study provided their written consent prior to participating in the survey.
Hypertension
Hypertension was defined as either systolic blood pressure (SBP) ≥ 140 mmHg, diastolic blood pressure (DBP) ≥ 90 mmHg, or antihypertensive medication use. Blood pressure was measured twice using an electric sphygmomanometer (Omron, HEM- 1020, Tokyo, Japan), after a 5-minute rest before the first measurement. Participants were seated with their arm supported at the heart level. The mean SBP and DBP were calculated from the two measurements.
Physical activity
PA was assessed using the Global Physical Activity Questionnaire (GPAQ) [19,20,21], which was previously validated in the Vietnamese language [14] and utilized in the WHO STEPS survey in Vietnam in 2015 [22, 23]. Specifically, participants were asked about time spent doing several types of PA in a typical week. We used showcards to help participants understand the level of MVPA [24]. We calculated PA in the form of METs. Following the World Health Organization guidelines [19, 25], we defined 4 METs and 8 METs as moderate and vigorous PA, respectively. The amount of PAs was calculated as the total MET-hours/week. PAs were categorized into occupational and leisure-time activities [3].
Of the three domains that can be assessed with the GPAQ (i.e., activity at work, recreational activities, and travel to and from places), we focused on the first two domains, i.e., occupational PA (such as carrying or lifting heavy loads, digging, or construction work) and leisure-time PA (including playing sports, fitness, walking to and from places, and recreational activities).
Covariates
Socio-demographic information was collected via the questionnaire, including age (in years), sex (male and female), education (primary school or less; secondary school; high school and higher), marital status (currently married/cohabiting or not), current employment (employed by the government/ private sector; self-employed; farmer/fisher; homemaker; others; and unemployed/retired). Information on household income was extracted from the responses by household representatives who were asked to choose a category that best described their monthly household income (VND). Values were then divided by the squared root of the number of household members to compute equivalized income, which was then categorized into tertiles (low, middle, and high). Questionnaire information was also collected on lifestyle parameters, which included smoking (never, former, and current smokers) and alcohol consumption (never, 0.1–0.9 standard drinks, 1–1.9 standard drinks, ≥ 2 standard drinks) [26].
Body mass index (BMI) was computed by dividing measured weight (kg) by the square of measured height (m2), which was then categorized into < 18.5; 18.5–22.9; 23.0–24.9; ≥ 25 kg/m2 [27]. Diabetes Mellitus (DM) was defined as either fasting plasma glucose (FPG) ≥ 126 mg/dL or hemoglobin A1c (HbA1c) ≥ 6.5% or current diabetes medication or insulin use [28]. Dyslipidemia was defined as total cholesterol ≥ 6.2 mmol/L (≥ 240 mg/dL), or low-density lipoprotein (LDL) cholesterol ≥ 4.1 mmol/L (≥ 160 mg/dL), or high-density lipoprotein (HDL) cholesterol < 1.0 mmol/L (< 40 mg/dL), or triglycerides ≥ 2.3 mmol/L (≥ 200 mg/dL), or current cholesterol-control drug use [29]. Previous diagnoses of severe diseases (i.e., diseases of the circulatory system and cancer) were also included in the models (yes or no).
Statistical analysis
Basic characteristics are shown by leisure-time PA (with and without any PA associated with recreational activity) and occupational PA (tertiles: low, middle, and high) categories.
Multiple imputation by chained equation was used to account for missing information on household income (n = 33). Specifically, a linear regression model was used to impute household income with 200 iterations to generate 20 datasets. The estimates were combined using Rubin’s rule [30].
To investigate the association between PA and hypertension, we used a multilevel Poisson regression model with a robust variance estimator with two exposures (i.e., occupational PA and leisure-time PA) simultaneously incorporated into the model [31, 32]. We accounted for possible heterogeneity at the commune level (Level 1: individual; Level 2: commune). Three models were used in the analysis and were adjusted as follows: Model 1 was adjusted for age and sex. Model 2 was further adjusted for income, job categories, educational attainment, marital status, current smoking, and alcohol intake. Model 3 was further adjusted for health-related indicators, including BMI and physical morbidity (i.e., DM, dyslipidemia, history of cancer, or symptoms related to circulatory system diseases). Results are reported as prevalence ratios (PR) and corresponding 95% CIs of hypertension for the occupational (low, middle, and high) and the leisure-time PA categories (yes and no). We also calculated PRs per 10 MET-hour/week-increments in leisure-time PA and PRs per 50 MET-hour/week-increments in occupational PA [3].
To elucidate if a non-linear relationship existed between occupational PA and hypertension prevalence, we used a restricted cubic spline model with three knots set at the 5th, 50th, and 95th percentiles of occupational PA [33, 34] without using multiple imputation [35]. The model was adjusted for the variables included in Model 3, except for household income, which contained missing values. The covariates were rescaled based on average values before calculating the model. The limited variation in leisure-time PA reported in this study did not allow us to apply a restricted cubic spline model to leisure-time PA.
To test the robustness of the study findings, we stratified the analysis by BMI at a 23.0 kg/m2 cut-off, at which overweight is defined for Asian people (< 23.0; ≥ 23.0 kg/m2) [27], and examined whether associations differed by BMI categories (i.e., if BMI was a possible strong mediator linking PA and hypertension) [36]. We also excluded those with antihypertensive medication.
All statistical analyses were conducted using Stata ver. 15.0 (College Station, TX, USA). A restricted cubic spline plot was drawn using the package ‘mskspline2’ in Stata [34]. Statistical significance was set at p < 0.05 (two-tailed).
Results
Table 1 shows the study participants’ basic characteristics. The mean age was 49.9 years (standard deviation [SD] = 5.5 years). Approximately 60% were female, with a higher proportion observed in those with low occupational PA. Those who attained secondary education or higher accounted for 59.5% of all participants, with a higher proportion among those with than among those without leisure-time PA (72.3% vs. 53.2%). About 30% of participants were farmers or fishers. Current smokers occupied 20.5% of all participants, with a higher proportion among those with high than among those with low occupational PA (25.0% vs. 16.4%). The prevalence of overweight/obesity tended to be higher in those with than in those without leisure-time PA (29.4% vs. 24.2%) and higher in those with low than in those with high occupational PA (28.3% vs. 23.2%). Occupational PA tended to be higher in those who did not than in those who did engage in leisure-time PA (139.2 vs. 128.8 MET-hour/week), while leisure-time PA tended to be higher in those in the lowest than in those in the highest tertile of occupational PA (7.0 vs. 5.2 MET-hour/week).
Of the study participants, 39.6% had hypertension. Table 2 shows the results of the multilevel robust Poisson models examining the association between PA and hypertension prevalence. After adjusting for age and sex, those in the highest occupational PA category were less likely to be hypertensive than those in the lowest category (PR 0.89, 95% CI 0.77–1.02), while the PR per 50 MET-hour/week-increment in occupational PA was 0.98 (95% CI 0.96–0.997). Leisure-time PA was positively associated with hypertension prevalence (PR 1.12, 95% CI 1.03–1.22 for those with vs. those without leisure-time PA; PR 1.04 per 10 MET-hour/week-increment, 95% CI 1.01–1.06). These associations were slightly attenuated but did not change markedly when the models were adjusted for educational attainment, household income, job categories, marital status, current smoking, and alcohol intake in Model 2, and for BMI and physical morbidity in Model 3.
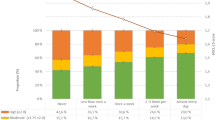
Figure 1 illustrates the non-linear relationship between occupational PA and hypertension prevalence based on the cubic spline model. The OR of hypertension constantly decreased until occupational PA of 300 MET-hour/week, where the OR reached the minimum value, and increased among those with occupational PA at the upper end of the distribution. The coefficients obtained from the models are shown in Supplementary Table 1.
Restricted cubic spline model of odds ratio of hypertension prevalence with Occupational Physical activity (per 50 METs increment)
Panel (a) represents results of restricted cubic spline model adjusting for age, sex and leisure-time PA (Model 1); Panel (b)shows results of restricted cubic spline model further adjusting for educational attainment, marital status, employment, smoking status, and alcohol consumption (Model 2); Panel (c) represents results of restricted cubic spline model further adjusting for body mass index and co-morbidity (i.e., dyslipidemia, diabetes and previous history of serious diseases) (Model 3).
When we stratified the participants by BMI categories, significant positive associations related to leisure-time PA were found among individuals with BMI < 23.0 kg/m2 (Model 2: PR 1.03, 95% CI 1.01–1.06), but not among those with BMI ≥ 23.0 kg/m2 (Table 3). On the other hand, significant inverse associations in relation to occupational PA were observed among those with BMI ≥ 23 kg/m2 (Model 2: PR 0.97, 95% CI 0.93–0.998), while we did not find evidence of a significant association among those with BMI < 23.0 kg/m2.
After excluding those on antihypertensive medication in the sensitivity analysis, we found a significant inverse association with occupational PA, but no evidence of a significant association with leisure-time PA (Supplementary Table 2).
Discussion
Among 3000 rural residents in Khánh Hòa province, Vietnam, we found a positive association between leisure-time PA and hypertension prevalence, while occupational PA was associated with a lower hypertension prevalence. More specifically, every 10 MET-hour/week increment in leisure-time PA was associated with a 2–4% increase in hypertension prevalence, while every 50 MET-hour/week-increment in occupational PA was linked to a 2% reduction in hypertension prevalence. These associations did not materially change after adjusting for socioeconomic status and lifestyle-related variables. Our hypothesis that occupational PA is more strongly inversely associated with hypertension prevalence than leisure-time PA was supported.
The inverse association between occupational PA and hypertension prevalence observed in our study was not consistent with the results of a meta-analysis of 13 cohort studies, the majority of which were conducted in high-income countries, by Huai et al. [4], which did not find any evidence of a significant association between occupational PA and hypertension (RR: 0.93 in high- vs. low-occupational PA groups, 95% CI: 0.81–1.08). However, our finding was in line with several studies conducted in LMICs that reported inverse associations between occupational PA and hypertension [13, 37,38,39]. For example, in an 8-year prospective cohort study among 27 provinces and three megacities in China, by Gu et al., the RR for hypertension was 1.27 (95% CI: 1.10–1.47) among those with low vs. those with high occupational PA [37].
There are some possible interpretations for these discrepant findings between high-income countries and LMICs. First, compared to high-income countries, where a higher occupational PA often indicates a lower socio-economic status (SES), it is possible that there was no such linkage in LMICs, particularly in rural communities where a fair proportion of the population engaged in physically demanding jobs (e.g., farming and fishery), irrespective of their SES [40]. Second, the absolute amount and duration of occupational PA may be larger and longer, respectively, in Vietnam and other LMICs than in high-income countries [41]. In fact, the mean occupational PA in this study population was 135.7 MET-hour/week (SD 110.7 MET-hour/week). This was markedly higher than that in European countries, for example, 47.7 MET-hour/week in Germany [41]. In countries where people do not engage in much occupational PA, it is theoretically not possible to observe the beneficial effects of work-related exercise on blood pressure (e.g., a decrease in vascular resistance caused by decreased sympathetic activity, improving insulin sensitivity, lowering adiposity, and improving energy balance).
Our finding that leisure-time PA was linked to a higher prevalence of hypertension was not in line with the findings of the meta-analyses by Huai et al. and Liu et al. [3, 4] or those of some more recent studies [38, 42]. For example, the pooled RR of hypertension among high vs. low leisure-time PA was 0.81 (95% CI 0.76–0.85) [4]. Our participants lived in rural communities in Vietnam, where people are engaged in agriculture, unstable work, and seasonal jobs [14, 23, 43], and do not typically engage in leisure-time PA. Only a small proportion of the study participants (33.3%) engaged in leisure-time PA and the absolute amount of leisure-time PA was also limited. It is also possible that differences in basic characteristics between those who did and those who did not engage in leisure-time PA differed so markedly that it was not possible to adjust for them fully in a regression model (i.e., residual confounding). For example, those who engaged in leisure-time PA tended to be richer, more educated, and have higher excess body weight than those who did not engage in leisure-time PA.
The restricted cubic spline model applied in this study suggested that a declining trend in the prevalence of hypertension reversed into an increasing trend when occupational PA exceeded 300 MET-hour/week, albeit with large confidence intervals towards the upper end of occupational PA. Given that most participants had occupational PA below this level, we concluded that occupational PA was inversely associated with the prevalence of hypertension. However, this reversal in the association might indicate a possible detrimental effect of occupational PA on hypertension. This suggestive U-shaped association between occupational PA and hypertension agrees with a previous study conducted in China, which found a U-shaped association between occupational PA and the incidence of hypertension [39].
When we stratified participants by BMI at a cut-off of 23.0 kg/m2, we found the inverse association between occupational PA and hypertension only among those with BMI ≥ 23.0 kg/m2. Thus, the protective effect of occupational PA seemed to be more significant among those with obesity. This could be interpreted that, compared to those with BMI < 23.0 kg/m2 who were metabolically healthy irrespective of their occupational PA level, those with higher BMI may develop better cardiorespiratory fitness via occupational PA, which might protect them from developing hypertension [44, 45]. On the other hand, the positive association between leisure-time PA and the prevalence of hypertension was more pronounced among those with BMI < 23 kg/m2. While this suggests that occupational PA and leisure-time PA have different health implications, depending on the BMI of the individuals, it should be considered that this association might have been due to residual confounding [36].
An inconsistency in the direction of the associations between different types of PA and health outcomes within a single study had been reported previously (i.e., the PA paradox). More specifically, occupational PA increased, and leisure-time PA reduced the risk of various negative health outcomes. Our study also reported inconsistency in these associations, but the pattern of inconsistency was not the same as those reported previously (inverse association of hypertension with occupational PA and no association with leisure-time PA).
This study had several limitations. First, as occupational PA and leisure-time PA were both measured using a questionnaire, the responses might have been affected by recall bias. More specifically, using the GPAQ to assess PA could lead to an overestimate or underestimate of PA. For example, it is possible that engaging in housework or taking care of babies were not considered occupational physical activity by rural Vietnamese middle-aged people. Second, the cross-sectional design of the current study could not establish any causal inference. For example, it is possible that those who had developed hypertension chose to engage in leisure-time PA and avoid occupational PA. However, it should also be mentioned that results in relation to occupational PA did not change markedly when we excluded those on antihypertensive medication in our sensitivity analysis. Third, our study participants were not representative of the Vietnamese population as they resided in rural communities of a single province and were all middle-aged. Thus, caution should be exercised when generalizing the study findings to other populations or age groups.
Future research should (1) examine whether the associations observed in this study can also be obtained in a longitudinal design and (2) subjectively measure PA by using accelerometers to reduce misclassification bias in relation to the exposure. In addition, similar studies conducted in other locations (e.g., urban areas of Vietnam or rural areas of other LMICs) will facilitate our understanding of the association between PA and hypertension in a global context.
Conclusion
Among 3000 rural residents in Khánh Hòa Province, Vietnam, we found that a higher level of occupational PA was associated with a lower hypertension prevalence while leisure-time PA was positively associated with hypertension. These findings contrasted with those of previous studies conducted in high-income countries, suggesting that the associations between PA and hypertension might differ depending on the context. Public health researchers and practitioners working in LMICs should be aware of the possible difference in the association between PA and hypertension in such countries.
Data Availability
The data are not publicly available but are available upon reasonable request to the corresponding author (yosuke.yoshi.yosky@gmail.com).
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence intervals
- DBP:
-
Diastolic blood pressure
- DM:
-
Diabetes mellitus
- FPG:
-
Fasting plasma glucose
- GPAQ:
-
Global Physical Activity Questionnaire
- HbA1c:
-
Hemoglobin A1c
- HDL:
-
High-density lipoprotein
- IQR:
-
Interquartile range
- KHCS:
-
Khánh Hòa Cardiovascular Study
- LDL:
-
Low-density lipoprotein
- LMICs:
-
Low- and middle-income countries
- METs:
-
Total metabolic equivalent task
- MICE:
-
Multiple imputation by chained equation
- MVPA:
-
Moderate to vigorous physical activity
- NCGM:
-
National Center for Global Health and Medicine
- OR:
-
Odds ratio
- PA:
-
Physical activity
- PINT:
-
Pasteur Institute in Nha Trang
- PR:
-
Prevalence ratio
- SD:
-
Standard deviation
- SES:
-
Socio-economic status
- SBP:
-
Systolic blood pressure
- USA:
-
The United State of America
- USD:
-
United States dollar
- WHO:
-
World Health Organization
References
Poulter NR, Prabhakaran D, Caulfield M, Hypertension. Lancet. 2015;386:801–12. https://doi.org/10.1016/S0140-6736(14)61468-9.
Diaz KM, Shimbo D. Physical activity and the Prevention of Hypertension. Curr Hypertens Rep. 2013;15:659–68. https://doi.org/10.1007/s11906-013-0386-8.
Liu X, Zhang D, Liu Y, et al. Dose–Response Association between Physical Activity and Incident Hypertension. Hypertension. 2017;69:813–20. https://doi.org/10.1161/HYPERTENSIONAHA.116.08994.
Huai P, Xun H, Reilly KH, et al. Physical activity and risk of hypertension. Hypertension. 2013;62:1021–6. https://doi.org/10.1161/HYPERTENSIONAHA.113.01965.
Korshøj M, Hannerz H, Frikke-Schmidt R, et al. Occupational lifting and risk of hypertension, stratified by use of anti-hypertensives and age - a cross-sectional and prospective cohort study. BMC Public Health. 2021;21:721. https://doi.org/10.1186/s12889-021-10651-w.
Byambasukh O, Snieder H, Corpeleijn E. Relation between Leisure Time, Commuting, and Occupational Physical Activity with blood pressure in 125 402 adults: the Lifelines Cohort. J Am Heart Assoc. 2020;9:e014313. https://doi.org/10.1161/JAHA.119.014313.
Barengo NC, Hu G, Kastarinen M et al. Low physical activity as a predictor for antihypertensive drug treatment in 25-64-year-old populations in Eastern and south-western Finland.J Hypertens2005;23.https://journals.lww.com/jhypertension/Fulltext/2005/02000/Low_physical_activity_as_a_predictor_for.11.aspx
Zhou B, Carrillo-Larco RM, Danaei G, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80. https://doi.org/10.1016/S0140-6736(21)01330-1.
Hayes P, Ferrara A, Keating A, et al. Physical activity and hypertension. Rev Cardiovasc Med. 2022;23:302. https://doi.org/10.31083/j.rcm2309302.
Zhou B, Bentham J, Di Cesare M, et al. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389:37–55. https://doi.org/10.1016/S0140-6736(16)31919-5.
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16:223–37. https://doi.org/10.1038/s41581-019-0244-2.
Shariful Islam M, Rabbani MG, Fardousi A, et al. Effect of leisure-time physical activity in controlling hypertension: a systematic review and meta-analysis protocol. BMJ Open. 2021;11:e056270. https://doi.org/10.1136/bmjopen-2021-056270.
Medina C, Janssen I, Barquera S, et al. Occupational and leisure time physical inactivity and the risk of type II diabetes and hypertension among mexican adults: a prospective cohort study. Sci Rep. 2018;8:5399. https://doi.org/10.1038/s41598-018-23553-6.
Thuy AB, Blizzard L, Schmidt M, et al. Reliability and validity of the global physical activity questionnaire in Vietnam. J Phys Act Heal. 2010;7:410–8. https://doi.org/10.1123/jpah.7.3.410.
Andrade C. The Inconvenient Truth about Convenience and Purposive samples. Indian J Psychol Med. 2020;43:86–8. https://doi.org/10.1177/0253717620977000.
Etikan I. Comparison of Convenience Sampling and Purposive Sampling. Am J Theor Appl Stat. 2016;5:1. https://doi.org/10.11648/j.ajtas.20160501.11.
Inoue Y, Fukunaga A, Stickley A, et al. Association between parental absence during childhood and depressive symptoms in adulthood in rural Vietnam. J Affect Disord. 2022;311:479–85. https://doi.org/10.1016/j.jad.2022.05.102.
Nguyen CQ, Pham TTP, Fukunaga A, et al. Red meat consumption is associated with prediabetes and diabetes in rural Vietnam: a cross-sectional study. Public Health Nutr. 2022;1–8. https://doi.org/10.1017/S1368980022001422.
WHO. Global Physical Activity Questionnaire (GPAQ) Analysis guide. World Heal. Organ. 2006.https://www.who.int/ncds/surveillance/steps/resources/GPAQ_Analysis_Guide.pdf (accessed 15 Dec 2021).
Cleland CL, Hunter RF, Kee F, et al. Validity of the global physical activity questionnaire (GPAQ) in assessing levels and change in moderate-vigorous physical activity and sedentary behaviour. BMC Public Health. 2014;14:1255. https://doi.org/10.1186/1471-2458-14-1255.
Armstrong T, Bull F. Development of the World Health Organization Global Physical Activity Questionnaire (GPAQ). J Public Health (Bangkok). 2006;14:66–70. https://doi.org/10.1007/s10389-006-0024-x.
Bui T, Blizzard C, Luong K, et al. National survey of risk factors for non-communicable disease in Vietnam: prevalence estimates and an assessment of their validity. BMC Public Health. 2016;16. https://doi.org/10.1186/s12889-016-3160-4.
Bui T, Van, Blizzard CL, Luong KN, et al. Physical activity in Vietnam: estimates and measurement issues. PLoS ONE. 2015;10:e0140941. https://doi.org/10.1371/journal.pone.0140941.
Rudolf K, Lammer F, Stassen G, et al. Show cards of the global physical activity questionnaire (GPAQ) - do they impact validity? A crossover study. BMC Public Health. 2020;20:223. https://doi.org/10.1186/s12889-020-8312-x.
WHO. WHO STEPS Surveillance Manual. 2017;:472.https://www.who.int/ncds/surveillance/steps/STEPS_Manual.pdf (accessed 15 Dec 2021).
Bertossi Urzua C, Ruiz MA, Pajak A, et al. The prospective relationship between social cohesion and depressive symptoms among older adults from Central and Eastern Europe. J Epidemiol Community Health. 2019;73:117–22. https://doi.org/10.1136/jech-2018-211063.
WHO. The Asia-Pacific perspective: redefining obesity and its treatment. Sydney: Health Communications Australia 2000. http://iris.wpro.who.int/handle/10665.1/5379
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2011;34(Suppl 1):62–9. https://doi.org/10.2337/dc11-S062.
Teramoto T, Sasaki J, Ishibashi S, et al. Diagnostic criteria for Dyslipidemia. J Atheroscler Thromb. 2013;20. https://doi.org/10.5551/jat.17152.
Rubin DB. Multiple imputation for nonresponse in surveys. 6th ed. New York:: Willey & Sons; 1987. https://doi.org/10.1002/9780470316696.
Greenland S. Model-based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case-control studies. Am J Epidemiol. 2004;160:301–5. https://doi.org/10.1093/aje/kwh221.
Zou G. A modified Poisson Regression Approach to prospective studies with Binary Data. Am J Epidemiol. 2004;159:702–6. https://doi.org/10.1093/aje/kwh090.
Li J, Zhang Z, Si S, et al. Leisure-Time Physical Activity and Cardiovascular Disease Risk among Hypertensive Patients: a longitudinal cohort study. Front Cardiovasc Med. 2021. https://doi.org/10.3389/fcvm.2021.644573. 8.https://www.frontiersin.org/article/.
Orsini N, Greenland S. A Procedure to tabulate and plot results after flexible modeling of a quantitative covariate. Stata J. 2011;11:1–29. https://doi.org/10.1177/1536867X1101100101.
Liu H, Wang Y, Chen W. Three-step imputation of missing values in condition monitoring datasets. IET Gener Transm Distrib. 2020;14:3288–300. https://doi.org/10.1049/iet-gtd.2019.1446.
Hu G, Barengo NC, Tuomilehto J, et al. Relationship of physical activity and body Mass Index to the risk of hypertension: a prospective study in Finland. Hypertension. 2004;43:25–30. https://doi.org/10.1161/01.HYP.0000107400.72456.19.
Gu D, Wildman RP, Wu X et al. Incidence and predictors of hypertension over 8 years among Chinese men and women.J Hypertens2007;25.https://journals.lww.com/jhypertension/Fulltext/2007/03000/Incidence_and_predictors_of_hypertension_over_8.7.aspx
Petermann-Rocha F, Brown RE, Diaz-Martínez X, et al. Association of leisure time and occupational physical activity with obesity and cardiovascular risk factors in Chile. J Sports Sci. 2019;37:2549–59. https://doi.org/10.1080/02640414.2019.1647738.
Li Q, Li R, Zhang S, et al. Occupational physical activity and new-onset hypertension: a Nationwide Cohort Study in China. Hypertension. 2021;78:220–9. https://doi.org/10.1161/HYPERTENSIONAHA.121.17281.
Sebastien FMC, Van Cauwenberg J, Maenhout L, et al. Inequality in physical activity, global trends by income inequality and gender in adults. Int J Behav Nutr Phys Act. 2020;17:142. https://doi.org/10.1186/s12966-020-01039-x.
Nikitara K, Odani S, Demenagas N, et al. Prevalence and correlates of physical inactivity in adults across 28 european countries. Eur J Public Health. 2021;31:840–5. https://doi.org/10.1093/eurpub/ckab067.
MacDonald C, Madika A, Lajous M, et al. Associations between Physical Activity and Incident Hypertension Across Strata of Body Mass Index: a prospective investigation in a large cohort of French Women. J Am Heart Assoc. 2020;9:e015121. https://doi.org/10.1161/JAHA.119.015121.
Trinh OTH, Nguyen N, van der Do HP, et al. Test-retest repeatability and relative validity of the global physical activity questionnaire in a developing country context. J Phys Act Heal. 2009;6:46–53. https://doi.org/10.1123/jpah.6.s1.s46.
Kokkinos P. Cardiorespiratory Fitness, Exercise, and blood pressure. Hypertension. 2014;64:1160–4. https://doi.org/10.1161/HYPERTENSIONAHA.114.03616.
Bakker EA, Sui X, Brellenthin AG et al. Physical activity and fitness for the prevention of hypertension.Curr Opin Cardiol2018;33.https://journals.lww.com/co-cardiology/Fulltext/2018/07000/Physical_activity_and_fitness_for_the_prevention.8.aspx
Acknowledgements
The authors would like to acknowledge the Japan Society for the Promotion of Science for providing funds for the study and NCGM for technical assistance with statistical questions. We are also grateful to the Nha Trang Pasteur Institute for organizing the study protocol and data collection.
Funding
This study was financially supported by the National Center for Global Health and Medicine (19A06, 22A02), the Pfizer Health Research Foundation, and the Japan Society for the Promotion of Science (KAKENHI JP19K20536, JP21J01171, JP21K17301). These funders had no role in the study design, execution of the study, statistical analyses, interpretation of the data, or decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Conceptualization, ADD, TTPP, CQN, and YI; methodology, ADD, SY, and RMS; software, ADD and YI; formal analysis, ADD and YI; writing—original draft preparation, ADD, TTPP, CQN, DVHo, AF; writing—review and editing, DCP, MH, DVHu, HXL, HTD, TM and YI; funding acquisition, HTD, TM and YI. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no competing interests to declare.
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki. The study was approved by the Research Ethics Committee at the National Center for Global Health and Medicine (NCGM) (approval number: NCGM-G-003172) and an equivalent committee at the Pasteur Institute in Nha Trang, Vietnam (02/2019/HDDD-IPN). All participants provided written informed consent before participating in the survey.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Do, A.D., Pham, T.T.P., Nguyen, C.Q. et al. Different associations of occupational and leisure-time physical activity with the prevalence of hypertension among middle-aged community dwellers in rural Khánh Hòa, Vietnam. BMC Public Health 23, 713 (2023). https://doi.org/10.1186/s12889-023-15631-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15631-w