Abstract
Background
To forecast the human immunodeficiency virus (HIV) incidence and mortality of post-neonatal population in East Asia including North Korea, South Korea, Mongolia, Japan and China Mainland and Taiwan province.
Methods
The data on the incidence and mortality of HIV in post-neonatal population from East Asia were obtained from the Global Burden of Diseases (GBD). The morbidity and mortality of post-neonatal HIV population from GBD 2000 to GBD 2013 were applied as the training set and the morbidity and mortality from GBD 2014 to GBD 2019 were used as the testing set. The hybrid of ARIMA and LSTM model was used to construct the model for assessing the morbidity and mortality in the countries and territories of East Asia, and predicting the morbidity and mortality in the next 5 years.
Results
In North Korea, the incidence and mortality of HIV showed a rapid increase during 2000–2010 and a gradual decrease during 2010–2019. The incidence of HIV was predicted to be increased and the mortality was decreased. In South Korea, the incidence was increased during 2000–2010 and decreased during 2010–2019, while the mortality showed fluctuant trend. As predicted, the incidence of HIV in South Korea might be increased and the mortality might be decreased during 2020–2025. In Mongolia, the incidence and mortality were slowly decreased during 2000–2005, increased during 2005–2015, and rapidly decreased till 2019. The predicted incidence and mortality of HIV showed a decreased trend. As for Japan, the incidence of HIV was rapidly increased till 2010 and then decreased till 2015. The predicted incidence of HIV in Japan was gradually increased. The mortality of HIV in Japan was fluctuant during 2000–2019 and was slowly decreased as predicted. The incidence and mortality of HIV in Taiwan during 2000–2019 was increased on the whole. The predicted incidence of HIV during was stationary and the mortality was decreased. In terms of China Mainland, the incidence and mortality of HIV was fluctuant during 2000–2019. The predicted incidence of HIV in China Mainland was stationary while the mortality was rapidly decreased.
Conclusion
On the whole, the incidence of HIV combined with other diseases in post-neonatal population was increased before 2010 and then decreased during 2010–2019 while the mortality of those patients was decreased in East Asia.
Similar content being viewed by others
Background
Human immunodeficiency virus (HIV) is a tremendous challenge to the society with 37.7 million people living with HIV, 1.5 million new HIV infections and 680,000 deaths from AIDS-related causes that occurred in 2020 all over the world [1, 2]. HIV has many routes of transmission including mother-to-child transmission (MTCT) [3]. Women with HIV infection at childbearing age are associated with a risk of MTCT during pregnancy and breastfeeding [4]. Most children were infected with HIV via MTCT and the Joint United Nations Program on HIV/AIDS (UNAIDS) estimated that there were 160,000 new HIV infections among children in 2018 [5]. It is well documented that the MTCT rate during pregnancy or postpartum period varies from 15 to 45% without prophylaxis [6]. Maternal HIV infection is associated with a significantly increased risk of infant death with 20% of untreated perinatally infected infants dying within 3 months and 48% dying within 1 year [7]. This indicated the high mortality rate due to HIV in the post-neonatal (1 month to 1 year) population. Effective surveillance and accurate prediction of HIV are essential for the control and outcome improving in post-neonatal population with HIV. Previously, growing numbers of researchers conducted studies on forecasting the incidence of HIV [8,9,10]. But these studies were performed in all individuals. To date, there was no data on forecasting the HIV incidence and mortality of post-neonatal population.
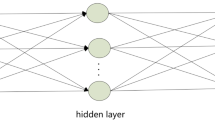
Recently, various machine learning (ML) and deep learning (DL) were extensively proposed and applied for various aspects including ground water storage change [11], climate [12, 13], permafrost distribution [14], air pollution [15], weed detection [16], botnet detection [17]. Disease forecasting is vital for the prevention of diseases and mathematical models are important tools for understanding of epidemics [18]. Previously, several mathematical models were also applied in forecasting the incidence of infection diseases including HIV [18, 19]. The autoregressive integrated moving average (ARIMA) model proposed by Box and Jenkins in the early 1970s, is a classical model based on linear theory to predict future tendency using the past and present data of time series [20]. The ARIMA model comprehensively considers the change of time trend, periodicity and other factors to achieve better prediction effect, and it is widely applied in predicting the incidence of diseases [21, 22]. The long short-term memory (LSTM) model is a novel prediction tool and a kind of Recurrent Neural Networks (RNN) using the multi-layer and complex neural networks close to the real values and a backward propagation algorithm to continually shrink the fitting error [23]. LSTM can skip the complex mathematical modelling and solving processes, which is suitable to solve the problem of correlation in time series [24]. Increasing evidence suggested that the LSTM model is a useful method for forecasting the incidence of diseases [25, 26].
In this study, we planned to forecast the HIV incidence and mortality of post-neonatal population in East Asia including North Korea, South Korea, Mongolia, Japan and China Mainland and Taiwan via constructing ARIMA and LSTM prediction model based on the data from the Global Burden of Disease (GBD) Study 2000–2019.
Methods
Data source
The data on the incidence of HIV in post-neonatal population from East Asian were obtained from the GBD 2000-GBD 2019 (https://www.healthdata.org/gbd/2019). The GBD is a multinational collaborative research study estimating the disease burden of 204 countries and territories [27]. It is an ongoing study updated annually including the incidence, prevalence, mortality, years of life lost (YLLs), years lived with disability (YLDs), and disability-adjusted life-years (DALYs) of 369 diseases and injuries, for two sexes in 204 countries and territories from 1990 to 2019 [27]. The GBD provides information for researchers and clinicians in discovering the latest knowledge and the current status of health for populations and countries worldwide [28]. In this study, HIV burden from 2000 to 2019 in post-neonatal population from East Asian was selected to analyze the time trends of incidence and mortality during 2010–2019 as well as the predicted trends of incidence and mortality in these patients.
Construction of the hybrid of ARIMA and LSTM model
The hybrid of ARIMA and LSTM model was constructed as follows: ARIMA time series model was employed to predict the morbidity and mortality of post-neonatal HIV population using the Statsmodels package in Python. The formula of the model was Φ(B)(1 − B) dXτ = θ(B)ετ. For construction of the model, firstly, time-series data were collected from the GBD, and the data were plotted to identify whether the time series was stationary. The d order difference operation was conducted in non-stationary time series to convert them into a stationary time series. The autocorrelation function analysis and the partial autocorrelation function analyses were used to identify the possible values of P. The parametric tests not statistically significant (P > 0.05) in the model were excluded, and the residual tests showed the non-white noise sequence using the Box–Jenkins Q test.
LSTM model was used to train and predict the residual values of ARIMA model using the Torch package in Python. For the construction of LSTM model, the raw data were divided into the testing set (data from 2014 to 2019), and the training set (data from 2000 to 2013). The training samples were used to build the model and to discover potential relationships in the data, and the test samples were used to evaluate the predictive power of the model constructed by the training set. The series of LSTM models were constructed using N values which were the time steps. The model with the lowest mean square error (MSE) was considered the optimal model. Finally, the incidence and mortality of HIV in post-neonatal population from East Asian were predicted by the optimal model for the assignment of the lowest MSE.
The final hybrid of ARIMA and LSTM model was calculated by adding the results of residual values of ARIMA time series model and ARIMA model predicted by LSTM model. The time complexity of the model was O (n2), and the space complexity was O (1).
Statistical analysis
The annual percent changes (APC) for morbidity and mortality were calculated using the Joint Point. The morbidity and mortality of post-neonatal HIV population from 2000 to 2013 were applied as the training set and the morbidity and mortality from 2014 to 2019 were used as the testing set. The hybrid of ARIMA and LSTM model was used to construct the model for assessing the morbidity and mortality in the countries and territories of East Asia, and predicting the morbidity and mortality in the next 5 years. The hybrid of ARIMA and LSTM model was constructed using Python V3.7.4. The performance of the model was evaluated by measuring its persistence including mean absolute error (MAE), the mean squared error (MSE), and root mean square error (RMSE).
Results
The incidence of HIV in post-neonatal population from East Asia during 2000–2019
In post-neonatal population from North Korea, the incidences of HIV were increased during 2000–2002, 2002–2006, and 2006–2010, and decreased during 2010–2019. The respective APCs were 14.7 (95%CI: 11.8–17.6), 9.8 (95%CI: 8.4–11.2), 4.4 (95%CI: 3.1–5.8) and − 0.7 (95%CI: − 0.9--0.5). As for HIV with extensive drug-resistant tuberculosis (XDR-TB), the incidence was increased during 2000–2004 (APC = 20.3, 95%CI: 18.9–21.8), 2004–2011 (APC = 3.2, 95%CI: 2.5–3.9) and 2011–2019 (APC = 7.0, 95%CI: 6.6–7.4). The incidences of HIV combined with other diseases were increased during 2000–2002 (APC = 14.7, 95%CI: 11.8–17.6), 2002–2006 (APC = 9.8, 95%CI: 8.4–11.2) and 2006–2010 (APC = 4.4, 95%CI: 3.1–5.8). The incidences of HIV with multidrug-resistant TB (MDR-TB) were increased during 2000–2005 (APC = 6.3, 95%CI: 5.5–7.1), 2010–2015 (APC = 0.6, 95%CI: − 0.5-1.6) and 2015–2019 (APC = 3.5, 95%CI: 2.4–4.6). The incidences of HIV with drug-susceptible TB (DS-TB) were increased during 2000–2004 (APC = 4.2, 95%CI: 3.9–4.5) and 2011–2017 (APC = 2.0, 95%CI: 1.8–2.2) (Fig. 1) (Table 1).
In post-neonatal population from South Korea, the incidences of HIV were increased during 2000–2003 (APC = 82.6, 95%CI: 70.5–95.5) and 2003–2011 (APC = 10.3, 95%CI: 8.3–12.4). In terms of HIV with XDR-TB, the incidences were increased during 2000–2004 (APC = 17.1, 95%CI: 15.9–18.2) and 2014–2017 (APC = 5.1, 95%CI: 1.8–8.5). As for HIV combined with other diseases, the incidences were increased during 2000–2003 (APC = 82.6, 95%CI: 70.5–95.5) and 2003–2011 (APC = 10.3, 95%CI: 8.3–12.4). With regard to HIV with MDR-TB, the incidences were increased during 2000–2005 (APC = 3.4, 95%CI: 2.3–4.6), and decreased during 2005–2013 (APC = -7.2, 95%CI: − 7.8--6.5), 2013–2017 (APC = -0.3, 95%CI: − 2.8-2.2) and 2017–2019 (APC = -6.7, 95%CI: − 11.3--1.9). The incidences of HIV with DS-TB were increased during 2005–2009 (APC = 14.3, 95%CI: 12.9–15.8), and decreased during 2000–2005 (APC = -2.4, 95%CI: − 2.9--1.8), 2009–2017 (APC = -0.4, 95%CI: − 0.8--0.1) and 2017–2019 (APC = -5.3, 95%CI: − 7.7--2.9) (Fig. 2) (Table 1).
In post-neonatal population from Mongolia, the incidences of HIV were increased during 2006–2015 (APC = 7.7, 95%CI: 1.2–14.7), and decreased during 2000–2006 (APC = -6.6, 95%CI: − 15.3-3) and 2015–2019 (APC = -26.6, 95%CI: − 38.8--12). The incidences of HIV with XDR-TB were increased during 2000–2004 (APC = 9.0, 95%CI: 4.7–13.4), 2004–2010 (APC = 1.6, 95%CI: − 1.3-4.5) and 2010–2016 (APC = 16.4, 95%CI: 13.1–19.7), and decreased during 2016–2019 (APC = -14.4, 95%CI: − 19.7--8.8). The incidences of HIV with combined with other diseases were increased during 2000–2003 (APC = 8.8, 95%CI: 2.5–15.5) and 2006–2016 (APC = 8.1, 95%CI: 6.9–9.3), and decreased during 2003–2006 (APC = -9.6, 95%CI: − 19.8-1.9) and 2016–2019 (APC = -32.7, 95%CI: − 36.6--28.5). The incidences of HIV with MDR-TB were increased during 2010–2014 (APC = 11.3, 95%CI: 5.8–17.1) and 2014–2017 (APC = 1.3, 95%CI: − 8.4-12.1), and decreased during 2000–2010 (APC = -4.8, 95%CI: − 5.6--4.1) and 2017–2019 (APC = -23.6, 95%CI: − 31--15.5). The incidences of HIV with DS-TB were increased during 2010–2017 (APC = 1.9, 95%CI: 0.8–3), and decreased during 2000–2002 (APC = -7.6, 95%CI: − 13.2--1.7), 2002–2010 (APC = -17.2, 95%CI: − 17.9--16.5) and 2017–2019 (APC = -26.3, 95%CI: − 30.8--21.5) (Fig. 3) (Table 1).
In post-neonatal population from Japan, the incidences of HIV were increased during 2004–2012 (APC = 8.1, 95%CI: 7.2–9.1) and 2016–2019 (APC = 1.3, 95%CI: − 2-4.7), and decreased during 2000–2004 (APC = -0.5, 95%CI: − 2.5-1.6) and 2012–2016 (APC = -15.8, 95%CI: − 18.5--12.9). In HIV with XDR-TB, the incidences were increased during 2010–2015 (APC = 4.7, 95%CI: 3.8–5.7), and decreased during 2000–2002 (APC = -6.3, 95%CI: − 9.1--3.6), 2002–2010 (APC = -13.2, 95%CI: − 13.5--12.9) and 2015–2019 (APC = -18.4, 95%CI: − 19.1--17.6). For HIV accompanied with other diseases, increased incidences were observed during 2004–2012 (APC = 8.1, 95%CI: 7.2–9.1) and 2016–2019 (APC = 1.3, 95%CI: − 2-4.7) while decreased incidences were observed during 2000–2004 (APC = -0.5, 95%CI: − 2.5-1.6) and 2012–2016 (APC = -15.8, 95%CI: − 18.5--12.9). In terms of HIV with MDR-TB and DS-TB, the incidences were decreased during 2000–2019 (Fig. 4) (Table 1).
In post-neonatal population from Taiwan, the increased incidences of HIV were found during 2000–2012 (APC = 11.1, 95%CI: 9.8–12.4), and 2015–2019 (APC = 2.1, 95%CI: − 4-8.7), and decreased incidences were identified during 2012–2015 (APC = -12.8, 95%CI: − 28.3-6). The increased incidences of HIV with XDR-TB were observed during 2000–2005 (APC = 6.4, 95%CI: 5.8–7), 2010–2017(APC = 0.8, 95%CI: 0.3–1.2) and 2017–2019 (APC = 4.2, 95%CI: 1.5–7). The incidences of HIV combined with other diseases were increased during 2000–2012 (APC = 11.1, 95%CI: 9.8–12.4) and 2015–2019 (APC = 2.1, 95%CI: − 4-8.7). The incidences of HIV with MDR-TB were increased during 2017–2019 (APC = 0.5, 95%CI: − 0.8-1.8), and decreased during 2000–2017. For HIV with DS-TB, the incidence was decreased during 2000–2019 (APC = -2.3, 95%CI: − 3.1--1.4) (Fig. 5) (Table 1).
As for the incidence of different types of HIV in post-neonatal population from China Mainland, increased incidences of HIV were identified during 2000–2007 (APC = 5.9, 95%CI: 4.8–7) and 2013–2016 (APC = 0.8, 95%CI: − 6.9-9.1), and decreased during 2007–2013 (APC = -4.2, 95%CI: − 5.9--2.5) and 2016–2019 (APC = -12.6, 95%CI: -16--9). The incidences of HIV with XDR-TB were elevated during 2000–2006 (APC = 0.1, 95%CI: − 0.7-0.9) and 2014–2019 (APC = 6.3, 95%CI: 5.1–7.4), and declined during 2006–2014. In terms of HIV combined with other diseases, the incidences were increased during 2000–2007 (APC = 5.9, 95%CI: 4.8–7) and 2013–2016 (APC = 0.8, 95%CI: − 6.9-9.1), and decreased during 2007–2013 (APC = -4.2, 95%CI: − 5.9--2.5) and 2016–2019. Decreased incidence of HIV with MDR-TB was found during 2000–2014, and then increased during 2014–2019 (APC = -12.6, 95%CI: -16--9). The incidence of HIV with DS-TB was decreased during 2000–2019 (Fig. 6) (Table 1).
The mortality of HIV in post-neonatal population from East Asia during 2000–2019
In post-neonatal population from North Korea, the mortalities of HIV, HIV with XDR-TB, and HIV combined with other diseases were increased during 2000–2019. The mortality of HIV with MDR-TB was decreased during 2013–2019 (APC = -2.9, 95%CI: − 4.1--1.8) and HIV with DS-TB was decreased during 2012–2019 (APC = -4.2, 95%CI: − 4.6--3.8) (Fig. 1) (Table 1).
In terms of the mortality of post-neonatal population from South Korea, decreased mortality of HIV was observed during 2010–2019 (APC = -4.7, 95%CI: − 7.9--1.3). For HIV with XDR-TB, the mortality was decreased during 2004–2019 (APC = -2.9, 95%CI: − 4.2--1.5). The mortality of HIV combined with other diseases showed a decline during 2011–2019 (APC = -3.6, 95%CI: − 5.1--2.2). The mortality of HIV with MDR-TB was decreased during 2004–2009 (APC = -13.7, 95%CI: − 22.2--4.4) and 2009–2019 (APC = -6.0, 95%CI: − 8.3--3.6) while the mortality of HIV with DS-TB was decreased during 2010–2019 (APC = -4.5, 95%CI: − 7.5--1.4) (Fig. 2) (Table 1).
In post-neonatal population from Mongolia, the mortality of HIV was decreased during 2000–2007 and 2016–2019 (APC = -32.6, 95%CI: − 36.4--28.6). With regard to HIV with XDR-TB, the mortality was decreased during 2000–2010 (APC = -1.6, 95%CI: − 2.8--0.5) and 2016–2019 (APC = -28.3, 95%CI: − 33.7--22.6). Decreased mortality of HIV combined with other diseases was observed during 2003–2006 and 2016–2019 (APC = -32.7, 95%CI: − 36.6--28.5). The mortality of HIV with MDR-TB and HIV with DS-TB presented a decline during 2000–2010 and 2016–2019 (Fig. 3) (Table 1).
For post-neonatal population from Japan, during 2007–2019 (APC = -3.2, 95%CI: − 4.6--1.8), the mortality of HIV was decreased. During 2000–2011 (APC = -2.4, 95%CI: − 4.4--0.4), the mortality of HIV with XDR-TB was decreased, and during 2007–2019 (APC = -3.2, 95%CI: − 4.7--1.7), the mortality of HIV combined with other diseases were decreased. For HIV with MRD-TB and DS-TB, the mortality was decreased during 2000–2019 (Fig. 4) (Table 1).
In Taiwan, the mortality of HIV and HIV combined with other diseases in post-neonatal population was decreased during 2011–2019 (APC = -3.1, 95%CI: − 6.8-0.8). For HIV with XDR-TB, MDR-TB and DS-TB, a decline of mortality was observed during 2000–2019 (Fig. 5) (Table 1).
With regard to HIV in post-neonatal population from China Mainland, decreased mortality of HIV was found during 2008–2019 (APC = -0.6, 95%CI: − 1.6-0.3). As for the mortality of HIV with XDR-TB, the mortality showed a decline during 2007–2014 (APC = -11.2, 95%CI: − 13--9.3) and 2014–2019 (APC = -2.9, 95%CI: − 5.6--0.2). The mortality of HIV with MDR-TB and DS-TB was decreased during 2000–2019 (Fig. 6) (Table 1).
The prediction of the incidence and mortality of HIV in post-neonatal population during 2020–2025
As for post-neonatal population in North Korea, the incidence of HIV was slowly increased from 2020 to 2025 while the mortality was decreased. For HIV with XDR-TB, both the incidence and mortality were rapidly increased during 2020–2025. The incidence of HIV combined with other diseases were increased during 2020–2024, but decreased in 2025. The mortality of HIV combined with other diseases was slowly decreased during 2020–2025. Increased incidence of HIV with MDR-TB was found during 2020–2025. The mortality of HIV with MDR-TB was slowly decreased during 2020–2025. The incidence and mortality of HIV with DS-TB was decreased in the next 5 years (Fig. 1) (Table 2).
As shown in Table 2, the incidence of HIV in post-neonatal population from South Korea was rapidly increased and the mortality was decreased during 2020–2025. The incidence of HIV with XDR-TB was decreased during 2020–2025 while the mortality was stationary during 2020–2021, and increased during 2022 and then stationary to 2025. A rapid increase of incidence and slowly decrease of mortality in HIV with other diseases were observed during 2020–2025. Both the incidence and mortality in HIV with MDR-TB and DS-TB presented a declined trend (Fig. 2) (Table 2).
In terms of the predicted incidence and mortality in post-neonatal population from Mongolia, decreased incidence and mortality of HIV, HIV with XDR-TB, HIV combined with other diseases, HIV with MDR-TB and DS-TB was observed during 2020–2025 (Fig. 3) (Table 2).
In Japan, the predicted incidence of HIV was increased during 2020–2021 and then slowly decreased during 2022–2025. The mortality was decreased during 2020–2025. A decreased incidence and increased mortality of HIV with XDR-TB was identified during 2020–2025. The incidence of HIV combined with other diseases was decreased during 2020–2024 but increased in 2025. The mortality of HIV combined with other diseases showed rapid decline during 2020–2025. The incidence of HIV with MDR-TB showed a slow decrease while the mortality of HIV with MDR-TB exhibited a slow increase. In terms of DS-TB, the incidence was slowly decreased while the mortality was increased during 2020–2021 and decreased during 2022–2025 (Fig. 4) (Table 2).
With regard to the post-neonatal population from Taiwan, the incidence of HIV showed a decreased trend during 2020–2024 and was increased slowly in 2025 while the mortality of HIV was quickly decreased during 2020–2025. Rapid increase of the incidence and mortality of HIV with XDR-TB was observed during 2020–2025. As for the incidence and mortality of HIV combined with other diseases, a slow increase was identified during 2020–2025. The incidence and morality of HIV with MDR-TB was gradually declined during 2020–2025. In terms of HIV with DS-TB, the incidence presented a quickly increase trend while the mortality displayed a gradual decreased trend during 2020–2025 (Fig. 5) (Table 2).
In China mainland, the incidence of HIV in post-neonatal population was similar while the mortality of HIV decreased slowly during 2020–2025. Rapid increase was observed in the incidence of HIV with XDR-TB during 2020–2022. The incidence and mortality of HIV combined with other diseases, HIV with MDR-TB and HIV with DS-TB exhibited a decreased trend during 2020–2025 (Fig. 6) (Table 2).
Discussion
In the present study, we evaluated the incidence and mortality of HIV in post-neonatal population from East Asia during 2000–2019 based on the data from GBD and predicted the incidence and mortality of HIV in the population during 2020–2025. In North Korea, the incidence and mortality of HIV showed a rapid increase during 2000–2010 and a gradual decrease during 2010–2019. The incidence of HIV was predicted to be increased and the mortality was decreased. In South Korea, the incidence during 2000–2010 was increased and decreased during 2010–2019, while the mortality showed fluctuant trend. As predicted, the incidence of HIV in South Korea might be increased and the mortality might be decreased during 2020–2025. In Mongolia, the incidence and mortality were slowly decreased during 2000–2005, increased during 2005–2015, and then rapidly decreased till 2019. The predicted incidence and mortality of HIV showed a decreased trend. As for Japan, the incidence of HIV was rapidly increased till 2010 and then decreased till 2015. The predicted incidence of HIV in Japan was gradually increased. The mortality of HIV in Japan was fluctuant during 2000–2019 and was slowly decreased as predicted. The incidence and mortality of HIV in Taiwan during 2000–2019 was increased on the whole. The predicted incidence of HIV during was stationary and the mortality was decreased. In terms of China Mainland, the incidence and mortality of HIV was fluctuant during 2000–2019. The predicted incidence of HIV in China Mainland was stationary while the mortality was rapidly decreased.
According to the results in this study, the incidence of HIV in post-neonatal population was increased on the whole in East Asia during 2000–2019. This may be due to the remarkable progress achieved in the diagnosis of HIV, especially the increase for the diagnosis of HIV infection in 20s and 30s women who at reproductive age [29]. During 2010–2015, the incidence of HIV showed a decreased trend. The World Health Organization (WHO) provided and updated the recommendations on the regimens of antiretrovirals (ARVs) for pregnant women infected with HIV [30,31,32]. Additionally, some East Asia countries launched the prevention of mother-to-child transmission for HIV program and spread more knowledge of HIV transmission means from mother to child among women [33, 34]. The predicted incidence of HIV in post-neonatal population showed a decreased trend in East Asia, except North Korea and South Korea. This might because in South Korea, the incidence of HIV has been steadily on the rise, especially among adolescents (ages 10–19 years) and young adults (ages 20–29 years) [29, 35]. As antiretroviral therapy (ART) has increased the life expectancy of HIV patients, women HIV patients are now more frequently considering becoming pregnant [36]. The live birth rate in women HIV patients is nearly as high as women without HIV infection with the application of ART [37]. Additionally, the repeated pregnancies among women with HIV was also increased in recent years [38, 39]. These factors might be the reason for the increase of HIV incidence post-neonatal population. In the current study, the mortality of HIV in post-neonatal population in East Asia was decreased since 2010 and the predicted mortality during 2020–2025 was continued to decline. This maybe because the improved prevention, screening, and treatment strategies including ART for HIV [40, 41]. Early HIV screening tests, avoid breastfeeding, and health care were provided in post-neonatal population with HIV, which might also help decrease the mortality of these patients [33]. In general, the incidence of HIV with XDR-TB in South Korea, North Korea, Mongolia, and Taiwan was increased during 2000–2019. According to the data from Zhang et al., the incidence rate of HIV with XDR-TB in all population from East Asia were increased from 1990 to 2017 [42]. The increased number of women HIV infection might be associated with the elevated incidence of post-neonatal HIV infection. As for North Korea, China Mainland and Taiwan, the increased incidence trend of HIV with XDR-TB was found during 2020–2025, and more effective measures should be taken to prevent the occurrence of HIV with XDR-TB. Meanwhile, the mortality of post-neonatal HIV in most East Asia countries and territories were decreased from 2000 to 2019 except North Korea in our study. The decreasing tendency of mortality indicates the great improvements in HIV treatments due to the introduction of ART [43]. It is worth noting that the mortality of post-neonatal HIV in North Korea and Japan during 2020–2025 presented an increasing tendency. The management of HIV with XDR-TB is more complicated and early use of ART and early testing to the drug resistance status should be provided to improve the outcomes of these patients.
On the whole, the trend of incidence of HIV combined with other diseases in post-neonatal population was increased before 2010 followed by decrease during 2010–2019. Infants who infected with HIV through MTCT have high possibility of combining with other diseases since born. A previous study on evaluating the outcomes of neonates whose mother were infected with HIV, and the results demonstrated that most neonates were born prematurely and associated with low birth weight [44]. This was supported by several studies in other countries, including a preterm birth rate of 13.0% in the United Kingdom and a 23.7% preterm birth rate, and an 18.4% small for gestational age rate in Botswana [45, 46]. Preterm or low birth weight neonates were reported to combine with many diseases [47, 48]. The predicted incidence of HIV combined with other diseases in post-neonatal population was increased in North Korea, South Korea and Taiwan during 2020–2025. Increased incidence of HIV in post-neonatal population might result in a higher rate of those patients combined with other diseases. More care should be provided on puerpera infected with HIV and their infants to prevent the occurrence of HIV or other diseases on the babies. The overall mortality of HIV combined with other diseases in post-neonatal population began to decrease in recent years from East Asia. As the increase of the knowledge on HIV, timely diagnosis and treatments were provided to infants with HIV, which helped improve the outcomes of those patients. On the whole, the incidence and mortality of HIV with MDR-TB and DS-TB in post-neonatal population from East Asia showed a decreased trend. A mathematical model constructed by Cho et al. for predicting the TB burden in South and North Korea delineated that the control strategies of TB including latent TB infection treatment, rapid diagnosis, active case-finding and improvement of the treatment success rate would reduce the burden of TB [49]. Zhang et al. identified that the overall mortality in all population with HIV and TB co-infection was decreased in East Asia in recent years [42]. These gave evidence to the finding of our study.
In previous studies, multiple evidence exhibited that the establishment of a single model presented a good effect when dealing with a single time series forecasting problem, but limitations existed when facing the complex problems [50, 55
Artificial intelligence (AI) is novel method to solve complex problems using computer engineering and software development [56]. As one of the applications of AI, ML provide output to almost any given input based on training, which ultimately improves the predictive value for a given task and/or acquire new skills over time when trained with more data [15]. In recent years, multiple ML, and AI methods were applied for helping predict ground water storage change [11], climate [12, 13] et al., and more and more studies indicated that artificial neural networks were more robust than linear regression as they more efficiently processed large datasets, worked with incomplete data, handled both linear and nonlinear processes and identified more relationships not inputted by the user [57]. In our study, we used LSTM to predict the HIV incidence and mortality of post-neonatal population in East Asia. Dropouts and callbacks were used to prevent the overfitting in the LSTM model. The results might help guide the clinicians and governments to make further policies for HIV prevention and treatment in both adults and neonatal.
This study evaluated the incidence and mortality of HIV in post-neonatal population based on the data from GBD, the data from GBD are authoritative and reliable. We were focused on HIV in post-neonatal population, and the results of our study might help decrease the occurrence of HIV and improve the outcome in those population, which might decrease the burden of society. There were several limitations of our study. Firstly, the data from GBD was updated to 2019, the recent data on 2020 was still unavailable to validate the results in the present study. Secondly, the prediction of incidence and mortality was only evaluated according to the time series, if other variables were included, the results of our study might be more reliable. In the future, we will update our prediction through using the recent data on 2020–2022, and the actual incidence and mortality of HIV in post-neonatal population could be compared with the predicting results in our study to validate the prediction value of our model. Also, we will apply more ML and DL methods to improve the predictive accuracy for the incidence and mortality of HIV in post-neonatal population, and hope to provide a reference for the government and clinicians to make future polices in the prevention and treatments of HIV.
Conclusions
The incidence and mortality of HIV in post-neonatal population from East Asia during 2000–2019 was evaluated and the incidence and mortality of HIV in the population during 2020–2025 was predicted in the current study. On the whole, the incidence of HIV combined with other diseases in post-neonatal population was increased before 2010 and then decreased during 2010–2019 while the mortality of those patients was decreased in East Asia. Strategies should be applied in respective countries to decrease the incidence and mortality of HIV in those population.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- HIV:
-
Human immunodeficiency virus
- MTCT:
-
Mother-to-child transmission
- UNAIDS:
-
The Joint United Nations Program on HIV/AIDS
- ARIMA:
-
Autoregressive integrated moving average
- LSTM:
-
Long short-term memory
- GBD:
-
Global Burden of Disease
- YLLs:
-
Years of life lost
- YLDs:
-
Years lived with disability
- DALYs:
-
Disability-adjusted life-years
- APC:
-
Annual percent changes
- XDR-TB:
-
Extensive drug-resistant tuberculosis
- DS-TB:
-
Drug-susceptible TB
References
Campbell EM, Jia H, Shankar A, Hanson D, Luo W, Masciotra S, et al. Detailed transmission network analysis of a large opiate-driven outbreak of HIV infection in the United States. J Infect Dis. 2017;216:1053–62.
HIV JUNPo. Availabe from: https://www.unaids.org/en/resources/documents/2021/2021_unaids_data.
Chi BH, Mbori-Ngacha D, Essajee S, Mofenson LM, Tsiouris F, Mahy M, et al. Accelerating progress towards the elimination of mother-to-child transmission of HIV: a narrative review. J Int AIDS Soc. 2020;23:e25571.
Mayaphi SH, Martin DJ, Quinn TC, Stoltz AC. Vertical transmission of HIV among pregnant women who initially had false-negative rapid HIV tests in four south African antenatal clinics. Plos One. 2019;14:e0226391.
UNAIDS. Global HIV and AIDS Statistics. Available from: https://www.unaids.org/en/resources/fact-sheet. 2019 Fact Sheet 2019.
Drake AL, Wagner A, Richardson B, John-Stewart G. Incident HIV during pregnancy and postpartum and risk of mother-to-child HIV transmission: a systematic review and meta-analysis. Plos Med. 2014;11:e1001608.
Lilian RR, Kalk E, Technau KG, Sherman GG. Birth diagnosis of HIV infection in infants to reduce infant mortality and monitor for elimination of mother-to-child transmission. Pediatr Infect Dis J. 2013;32:1080–5.
Liu Y, Ji W, Yin Y, Yang Z, Yang S, Zhou C, et al. An analysis on the trend of AIDS/HIV incidence in Chongqing and Shenzhen, China from 2005-2015 based on age-period-cohort model. Math Biosci Eng. 2021;18:6961–77.
Li Z, Li Y. A comparative study on the prediction of the BP artificial neural network model and the ARIMA model in the incidence of AIDS. BMC Med Inform Decis Mak. 2020;20:143.
Billock RM, Powers KA, Pasquale DK, Samoff E, Mobley VL, Miller WC, et al. Prediction of HIV transmission cluster growth with statewide surveillance data. J Acquir Immune Defic Syndr. 1999;2019(80):152–9.
Mohd Anul Haq AKJ, Prabul P. Deep learning BasedModeling of groundwater storage change. Comput Mater Contin. 2022;(70):4599–4611.
Mohd Anul Haq, Baral P, Yaragal S, Pradhan B. Bulk processing of multi-temporal Modis data, Statistical analyses and machine learning algorithms to understand climate variables in the Indian Himalayan region. Sensors (Basel, Switzerland). 2021;21(21):7416.
Mohd Anul Haq. CDLSTM: a novel model for climate change forecasting. Comput Mater Contin. 2021.
Mohd Anul Haq PB. Study of permafrost distribution in Sikkim Himalayas using Sentinel-2 satellite images and logistic regression modelling. Geomorphology. 2019;333:123–36.
Haq MA. SMOTEDNN: a novel model for air pollution forecasting and AQI classification. Comput Mater Contin. 2022;(77):1403–25.
Haq MA. CNN based automated weed detection system using UAV imagery. Comput Syst Sci Eng. 2022(42):837–49.
Haq MA, MARK. DNNBoT: deep neural network-based botnet detection and classification. Comput Mater Contin. 2022;(71):1729–50.
Blaizot S, Riche B, Maman D, Mukui I, Kirubi B, Etard JF, et al. Estimation and Short-term prediction of the course of the HIV epidemic using demographic and health survey methodology-like data. Plos One. 2015;10:e0130387.
Yin L, Zhao Y, Peratikos MB, Song L, Zhang X, Xin R, et al. Risk prediction score for HIV infection: development and internal validation with cross-sectional data from men who have sex with men in China. AIDS Behav. 2018;22:2267–76.
Adeyinka DA, Muhajarine N. Time series prediction of under-five mortality rates for Nigeria: comparative analysis of artificial neural networks, Holt-winters exponential smoothing and autoregressive integrated moving average models. BMC Med Res Methodol. 2020;20:292.
Cheng Y, Yuan J, Chen Q, Shen F. Prediction of nosocomial infection incidence in the Department of Critical Care Medicine of Guizhou Province with a time series model. Ann Transl Med. 2020;8:758.
Saba AI, Elsheikh AH. Forecasting the prevalence of COVID-19 outbreak in Egypt using nonlinear autoregressive artificial neural networks. Process Saf Environ Prot. 2020;141:1–8.
Kim Y, Choi A. EEG-based emotion classification using long Short-term memory network with attention mechanism. Sensors (Basel, Switzerland). 2020;20(23):6727.
Hochreiter S, Schmidhuber J. Long short-term memory. Neural Comput. 1997;9:1735–80.
Zhao D, Chen M, Shi K, Ma M, Huang Y, Shen J. A long short-term memory-fully connected (LSTM-FC) neural network for predicting the incidence of bronchopneumonia in children. Environ Sci Pollut Res Int. 2021;28:56892–905.
Zhang R, Guo Z, Meng Y, Wang S, Li S, Niu R, et al. Comparison of ARIMA and LSTM in forecasting the incidence of HFMD combined and uncombined with exogenous meteorological variables in Ningbo, China. Int J Environ Res Public Health. 2021:18(11):6174.
Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet (London, England). 2020;396:1204–22.
Smith L, Shin JI, Hwang SY, Tizaoui K, Dragioti E, Jacob L, et al. Global burden of disease study at the World Health Organization: research methods for the most comprehensive global study of disease and underlying health policies. Life Cycle. 2022;2:e8.
Danforth K, Granich R, Wiedeman D, Baxi S, Padian N. Global mortality and morbidity of HIV/AIDS. In: Holmes KK, Bertozzi S, Bloom BR, Jha P, editors. Major infectious diseases. Washington (DC): The International Bank for Reconstruction and Development / The World Bank International Bank for Reconstruction and Development / The World Bank; 2017.
WHO. Antiretroviral drugs for treating pregnant women and preventing HIV infection in infants. Guidelines on care, treatment and support for women living with HIV/AIDS and their children in resource-constrained settings. Geneva: World Health Organization; 2004.
WHO. Antiretroviral drugs for treating pregnant women and preventing HIV infection in infants. Recommendations for a public health approach. Geneva: World Health Organization; 2010.
WHO. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. Recommendations for a public health approach. Geneva: World Health Organization; 2013.
Choi H, Kim MH, Lee SJ, Kim EJ, Lee W, Jeong W, et al. Pregnancy rates and outcomes of HIV-infected women in Korea. J Korean Med Sci. 2018;33:e296.
Vo Hoang L, Nguyen Si Anh H, Tran Minh H, Tran Nhu P, Nguyen HT, Affarah WS, et al. Trends and changes in the knowledge of mother-to-child transmission means of HIV among Vietnamese women aged 15-49 years and its associated factors: findings from the multiple Indicator cluster surveys, 2000-2014. AIDS Care. 2020;32:445–51.
Yoo M, Seong J, Yoon JG, Cha JO, Chung YS, Kim K, et al. Characteristics of adolescents and young adults with HIV in the Republic of Korea from 2010 through 2015. Sci Rep. 2020;10(1):9384.
Harris K, Yudin MH. HIV infection in pregnant women: a 2020 update. Prenat Diagn. 2020;40(13):1715–21.
Haddad LB, Wall KM, Mehta CC, Golub ET, Rahangdale L, Kempf MC, et al. Trends of and factors associated with live-birth and abortion rates among HIV-positive and HIV-negative women. Am J Obstet Gynecol. 2017;216:71.e1–e16.
Floridia M, Tamburrini E, Masuelli G, Martinelli P, Spinillo A, Liuzzi G, et al. Rate, correlates and outcomes of repeat pregnancy in HIV-infected women. HIV Med. 2017;18:440–3.
Kang JS, Lee SH, Lee S, Lee JE, Lee SO, Kim SC, et al. Changing trends in pregnancy and childbirth among women living with human immunodeficiency virus at a tertiary Hospital in Korea: a 28-year experience. Infect Chemother. 2019;51:28–34.
Zhang R, Chen L, Cui YD, Li G. Achievement of interventions on HIV infection prevention among migrants in China: a meta-analysis. SAHARA J. 2018;15:31–41.
Yen-Hao Chu I, Wen-Wei KS, Li CW, Toh HS, Yang CJ, Wu KS, et al. Taiwan guideline on oral pre-exposure prophylaxis for HIV prevention - 2018 update. Journal of microbiology, immunology, and infection =. Wei mian yu gan ran za zhi. 2020;53:1–10.
Zhang J, Kern-Allely S, Yu T, Price RK. HIV and tuberculosis co-infection in East Asia and the Pacific from 1990 to 2017: results from the global burden of disease study 2017. J Thorac Dis. 2019;11:3822–35.
Mutembo S, Mutanga JN, Musokotwane K, Alisheke L, Whalen CC. Antiretroviral therapy improves survival among TB-HIV co-infected patients who have CD4+ T-cell count above 350cells/mm (3). BMC Infect Dis. 2016;16:572.
Benali G, Ramdin T, Ballot D. An audit of mother to child HIV transmission rates and neonatal outcomes at a tertiary hospital in South Africa. BMC Res Notes. 2019;12:586.
Wedi CO, Kirtley S, Hopewell S, Corrigan R, Kennedy SH, Hemelaar J. Perinatal outcomes associated with maternal HIV infection: a systematic review and meta-analysis. Lancet HIV. 2016;3:e33–48.
Short CE, Douglas M, Smith JH, Taylor GP. Preterm delivery risk in women initiating antiretroviral therapy to prevent HIV mother-to-child transmission. HIV Med. 2014;15:233–8.
Martín-Calvo N, Goni L, Tur JA, Martínez JA. Low birth weight and small for gestational age are associated with complications of childhood and adolescence obesity: Systematic review and meta-analysis. Obes Rev. 2021;23(Suppl 1):e13380.
Saad H, Sinclair M, Bunting B. Maternal sociodemographic characteristics, early pregnancy behaviours, and livebirth outcomes as congenital heart defects risk factors - Northern Ireland 2010-2014. BMC Pregnancy Childbirth. 2021;21:759.
Cho H, Park Y, Seok J, Yeom JS, Choi JY, Kim HJ, et al. Predicting the impact of control strategies on the tuberculosis burden in south and North Korea using a mathematical model. BMJ Glob Health. 2021:6(10):e005953.
Zheng A, Fang Q, Zhu Y, Jiang C, Jin F, Wang X. An application of ARIMA model for predicting total health expenditure in China from 1978-2022. J Glob Health. 2020;10:010803.
Maragatham G, Devi S. LSTM model for prediction of heart failure in big data. J Med Syst. 2019;43:111.
Tung WC, Ding K, Farmer S. Knowledge, attitudes, and behaviors related to HIV and AIDS among college students in Taiwan. J Assoc NursAIDS Care. 2008;19:397–408.
Olakunde BO, Pharr JR, Adeyinka DA. HIV testing among pregnant women with prenatal care in the United States: an analysis of the 2011-2017 National Survey of family growth. Int J STD AIDS. 2020;31:680–8.
Chi BH, Stringer JS, Moodley D. Antiretroviral drug regimens to prevent mother-to-child transmission of HIV: a review of scientific, program, and policy advances for sub-Saharan Africa. Curr HIV/AIDS Rep. 2013;10:124–33.
Dunkley E, Ashaba S, Burns B, O'Neil K, Sanyu N, Akatukwasa C, et al. “I beg you … breastfeed the baby, things changed”: infant feeding experiences among Ugandan mothers living with HIV in the context of evolving guidelines to prevent postnatal transmission. BMC Public Health. 2018;18:188.
Lin Z, Chou WC. Machine learning and artificial intelligence in toxicological sciences. Toxicol Sci. 2022;189(1):7–19.
Lin Z, Chou WC, Cheng YH, He C, Monteiro-Riviere NA, Riviere JE. Predicting nanoparticle delivery to tumors using machine learning and artificial intelligence approaches. Int J Nanomedicine. 2022;17:1365–79.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
YC and MW designed the study. YC wrote the manuscript. JH collected, analyzed and interpreted the data. MW critically reviewed, edited and approved the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our data are from a public research database. Since all subjects in the database were anonymous, informed consent and ethical approval were not required. All methods were carried out in accordance with relevant guidelines and regulations (declaration of Helsinki). All individuals provided written informed consent before participating in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, Y., He, J. & Wang, M. A hybrid of long short-term memory neural network and autoregressive integrated moving average model in forecasting HIV incidence and morality of post-neonatal population in East Asia: global burden of diseases 2000–2019. BMC Public Health 22, 1938 (2022). https://doi.org/10.1186/s12889-022-14321-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-14321-3