Abstract
Introduction
Men have higher rates of morbidity and mortality across nearly all top ten causes of mortality worldwide. Much of this disparity is attributed to men’s lower utilization of routine health services; however, little is known about men’s general healthcare utilization in sub-Saharan Africa.
Methods
We analyze the responses of 1,116 men in a community-representative survey of men drawn from a multi-staged sample of residents of 36 villages in Malawi to identify factors associated with men’s facility attendance in the last 12 months, either for men’s own health (client visit) or to support the health care of someone else (caregiver visit). We conducted single-variable tests of association and multivariable logistic regression with random effects to account for clustering at the village level.
Results
Median age of participants was 34, 74% were married, and 82% attended a health facility in the last year (63% as client, 47% as caregiver). Neither gender norm beliefs nor socioeconomic factors were independently associated with attending a client visit. Only problems with quality of health services (adjusted odds ratio [aOR] 0.294, 95% confidence interval [CI] 0.10—0.823) and good health (aOR 0.668, 95% CI 0.462–0.967) were independently associated with client visit attendance. Stronger beliefs in gender norms were associated with caregiver visits (beliefs about acceptability of violence [aOR = 0.661, 95% CI 0.488–0.896], male sexual dominance [aOR = 0.703, 95% CI 0.505–0.978], and traditional women’s roles [aOR = 0.718, 95% CI 0.533–0.966]). Older age (aOR 0.542, 95% CI 0.401–0.731) and being married (aOR 2.380, 95% CI 1.196–4.737) were also independently associated with caregiver visits.
Conclusion
Quality of services offered at local health facilities and men’s health status were the only variables associated with client facility visits among men, while harmful gender norms, not being married, and being younger were negatively associated with caregiver visits.
Similar content being viewed by others
Introduction
Men experience disproportionately high rates of morbidity and mortality compared to women across nearly all top ten causes of disease worldwide. [1] In southern and eastern Africa, gender disparities in HIV and tuberculosis (TB) outcomes are particularly stark – in 2016, men accounted for only 40% of people living with HIV but represented 54% of those who died of AIDS. [2].
Regular engagement with health systems can improve poor health outcomes for men. Routine facility visits may increase men’s comfort level with health systems [3] and can provide critical entry points for men to access screening services (such as for HIV, TB, or various non communicable diseases [NCDs]), preventative care, or early-stage care for illness. [4] While men in sub-Saharan Africa are not generally encouraged nor expected to attend health facilities except for HIV testing, [5] a growing number of studies show that men do attend facilities frequently, although their attendance is less visible than women’s. [6, 7] A recent study from Malawi showed that over 80% of men visited a health facility in the past 12 months, most attending outpatient departments for acute needs. Interestingly, the majority had attended facilities as both clients and caregivers during this time period. Over 45% of men attended a health facility to support friends’ or family members’ use of health services (caregiver visits). [6] Such facility visits could provide key entry points for key non-acute services, although such integrated care is poorly implemented to date. [8, 9].
While the majority of men appear to attend facilities for acute care, it is unclear if certain sub-populations of men do not attend general facility visits and what factors are associated with men’s general facility attendance (either for their own health or as caregivers). This question is important both for ensuring equity in men’s health and determining if men’s routine facility visits can be used to as an entry point for other priority services. For example, if facility services systematically reach all men, facility visits could be optimized as a primary entry point for improving population-level coverage for HIV, TB, and NCD screening among men. However, if facility services systematically exclude sub-populations of men, outreach services will likely be required to achieve population-level coverage. Both client and caregiver visits are potential entry points for additional services. [10, 11] Throughout the region, caregiver visits have been a critical entry point for women’s health education and screening services. [12, 13] The same could be done for men if a large portion of men attend facilities as caregivers. [14].
Research from HIV and TB services examines factors associated with service utilization and offers a useful system for categorizing potential factors that might also influence men’s general facility attendance. [15, 16] Demographic characteristics, such as education, age, marital status, income, and dependence on day labor, are all associated with use of HIV testing. [7, 17,18,19,20,21,22] Harmful gender norms regarding masculinity are also found to negatively influence men’s use of HIV and TB services, although most of the literature relies on qualitative data. [23, 24] Finally, health system factors such as quality of services, length of time required to receive services, and days/times when services are offered are associated with men’s use of reproductive health services. [25, 26] There is evidence that these same factors may dissuade men from attending as caregivers. [27 ] However, the above factors might not be associated with men’s general facility attendance. Most men attend facilities for curative care for non-stigmatized illnesses [6] – the acute and non-stigmatized nature of illness for most curative services may mitigate barriers traditionally experienced for HIV and TB services.
We assessed individual- and facility-level factors associated with men’s attendance to a health facility in the past 12 months, using data from a cross-sectional, community representative survey with men in rural Malawi. We examined factors associated with client visits (seeking care for men’s own health) and caregiver visits (providing support for someone else’s health).
Methods
Setting
Malawi is a predominantly rural country in southern Africa with an HIV prevalence of 13.2% in the Southern region and 5.7% in the Central region. [28] Basic primary health services, including sexual and reproductive health care, HIV services, and TB care, are free at all Ministry of Health and mission facilities. Acute care and other outpatient services are free at Ministry of Health facilities, but at mission facilities are offered at cost. Health insurance plays a negligible role in health access in Malawi; it comprises less than 5% of total health expenditures and, without a national health insurance scheme, typically only formally employed Malawians have insurance. [29].
Design
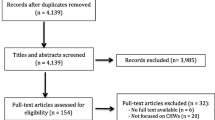
We use data from a large cross-sectional, community representative survey with men in central and southern Malawi collected from 15 August to 18 October 2019. The parent study examined the frequency with which men attend health facilities (for any reason) and coverage of HIV testing services at these visits. Detailed information of the parent study has been published elsewhere. [6] Briefly, the study used a multi-staged sampling design. First, we purposively selected two of Malawi’s most populous districts in the central and southern regions and three mid-size health facilities per district. Second, we randomly selected 6 villages within each facility catchment area (36 villages in total) and roughly 45 male respondents per village. Household census listings from each village were used to randomly select respondents using randomized number generation. Random selection within each village was stratified by age categories: young men (15-24-years, n = 300); middle-aged men (25-39-years, n = 425); and older men (40+-years, n = 425).
Eligibility criteria for individual men were: (1) aged 15–64 years; (2) current resident of the participating village; and (3) spent > 15 nights within the village in the past 30 days. Exclusion criteria included: (1) men who did not meet eligibility criteria, (2) men who were drunk, disabled, or otherwise unable to consent, and (3) men who did not match randomization identifiers. For this secondary analysis, we also exclude men who self-report as ever testing HIV-positive, because their health service utilization would not represent the general population and we would anticipate increased facility visits for HIV treatment services.
Data collection
Surveys were conducted with all randomly selected men, with the assistance of community health workers and village chiefs for identification. Survey domains included: (1) recent facility visits, including quality-related experience during the visit like wait time and privacy; (2) sociodemographic characteristics and health status; (3) gender norms; and (4) HIV testing history. The survey tool was developed in English and translated into the local language (Chichewa). It was piloted with approximately 25 men who met eligibility criteria and modified as needed for clarity. Surveys lasted approximately 55 min on average.
Variables
For this secondary analysis, our primary outcome of interest was facility visit in the past 12 months. Participants were asked to describe their four most recent visits to a health facility, including who received the primary health service at that visit. We created a dichotomous variable for having at least one facility visit (not for HIV treatment) within the past 12 months, distinguishing between client visits and caregiver visits.
We drew from HIV and TB literature to identify potential factors associated with men’s general facility attendance to include in the model. [17,18,19,20,21] Sociodemographic characteristics included ever attending secondary school (yes/no), currently having children living at home (yes/no), having financial savings at the time of the survey (yes/no), currently employed (yes/no), mobility (yes/no), and a household wealth index scale. We defined employment as either formally employed or self-employed over the past 12 months, while unemployment included both unemployment and ganyu work, a form of daily wage labor without long-term predictability. Mobility was defined as spending more than 3 nights away from home in the past 6 months. For the household wealth index, we used the first dimension of a principal component analysis of 22 household assets including items such as a chair, a radio, and a bicycle. [30] To make the index more easily interpretable, we linearly transformed it to a scale of 0 to 10, with a resulting mean of 1.88.
Men’s acceptance of harmful gender norms has been identified as a barrier to HIV and TB services in qualitatively studies. [24,25,26] To measure men’s acceptance of harmful gender norms, we use 12 questions from the Gender Equitable Men (GEM) survey, a validated tool used widely throughout sub-Saharan Africa. [31,32,33] While the tool has not been fully validated in Malawi, it has been validated in the region and has been used in other studies in Malawi. [32, 34] Questions were asked on a 5-point Likert scale from “strongly agree” to “strongly disagree.” We collapsed questions responses into 4 distinct measures, with 3 questions in each measure: measure 1: violence is permissible; measure 2: male sexual dominance is acceptable; measure 3: women’s roles should be confined to the household; and measure 4: men control household decisions, which was not scored on a Likert scale, with participants receiving scores of 1 for “male only,” 2 for “joint decision,” and 3 for “female only” on questions regarding who made decisions within respondents’ own household (see Appendix A for specific questions). We summed participant scores for each question in the construct (based on the Likert scale). We then created a dichotomous variable to measure respondents’ relative acceptance of harmful gender norms as compared to other study participants, separating the 20% of respondents with the highest degree of gender bias from the remaining 80% in each category. We found no concerning evidence of multicollinearity between the four gender norm constructs using variance inflation factors (all VIF < 2.0).
Quality of health services is associated with service utilization across numerous disease categories and conditions. [35,36,37] We included a composite measure for quality of services offered at respondents’ closest public facility. Participants were asked about their satisfaction with services received, using questions from the Service Provision Assessment (SPA) [38] that covered service availability (wait time and opening hours), privacy (ability to discuss concerns and privacy of their discussion and of the examination), medicine availability, and cleanliness. Participants were asked about whether they experienced problems during the visit in each domain (see Appendix B for all satisfaction questions). There were six major health facilities within the survey catchment area, with an average of 115 respondents reporting on the quality of health services at each facility (range 61–163 respondents). We generated a composite quality score (maximum of 7 problems) by averaging the problems reported within each domain for all men who described a visit to that facility. Facility scores were then applied to each respondent living in the catchment area of that respective facility, regardless of whether they reported visiting that facility.
Analysis
We used Wilcoxon rank sum tests, t-tests, and Chi-square tests to examine factors associated with facility attendance. Factors that had a p-value of < 0.10 in univariable analysis were included in our multivariable model. For client visits, we also included two control variables, age and self-reported health status, regardless of their association in the single-variable analyses, because we believe those to be intrinsically related to the need for a clinic visit. The multivariable model was a logistic regression with random effects to account for clustering at the village level, and we report results at the p < 0.05 significance level. Clustering at facility level (n = 6) did not notably changes results. Analyses were completed in Stata v.14. [39].
Human subjects
The parent study was approved by the National Health Sciences Review Committee (NHSRC) of Malawi and the University of California Los Angeles (UCLA) Institutional Review Board. Written, informed consent was ascertained from all respondents; written, informed assent was attained from respondents and written, informed consent was obtained from parents or legal guardians for participants between 15 and 17 years.
Results
Our analysis included 1,116 respondents after excluding men who reported being HIV-positive. Over 74% (824/1116) of participants were married, 88% (983/1116) owned land (not shown), and 20% (228/1116) attended at least some secondary school. A total of 82% (919/1116) of participants attended at least one facility visit in the past 12 months: 63% (701/1116) had at least one client visit, while 47% (524/1116) attended at least one visit as a caregiver in the past year (see Table 1). Interestingly, 25% of participants attended a health facility besides their local Ministry of Health facility, meaning they either had to travel a longer distance or had to pay user fees for a private facility (analysis not shown). The mean distance from facilities to village was 5.11 km with a standard deviation of 3.46 km.
There were few significant differences between participants who attended client visits in the last year and those who did not. Within sociodemographic and gender norms variables, only household assets trended toward significance (mean household asset score of 1.95 among those who attended a client visit versus 1·76 among those who did not; p = 0.09). The participant’s distance from facility was associated with the likelihood of a client visit in single-variable analysis (p < 0.001).
Perceived quality of services offered at local health facilities was significantly associated with attending a client visit in the past 12 months. Men who lived in catchment areas of health facilities with more frequently reported quality problems were less likely to attend client visits (problem score of 1.19 among those who attended a visit versus 1.26 among those who did not, out of a maximum of 7; p < 0.001).
Factors associated with facility attendance differed for caregiver visits. Scoring in the top quintile of respondents on each of the four beliefs regarding harmful gender norms was negatively associated with men’s attendance to caregiver visits: participants who believed men should assert violence to get their way (19% of men who attended a caregiver visit were in the top 20th percentile on the violence measure versus 29% among those who did not attend caregiver visits; p = 0.002), participants who believed men have natural sexual dominance (17% versus 24%; p = 0.006), and participants who believed household or childcare duties were strictly women’s roles (24% versus 32%; p = 0.004) were all less likely to attend caregiver visits. The male participant’s control over household financial decisions was associated with a higher likelihood of attending a caregiver visit (30% versus 25%; p = 0.054). Being formally employed or self-employed, versus being unemployed or relying on piece work, was associated with men attending a caregiver visit in the past 12 months (65% versus 55%; p = 0.001). Unlike client visits, attending caregiver visits was not associated with local facility quality of care metrics.
In our multivariable model for client visits (see Table 2), none of the wealth or demographic characteristics were associated with client visits, including distance from facility. Quality of health services offered at local facilities was significantly associated with visits: problems with overall quality was negatively associated with men’s likelihood of attending a client visit in the past 12 months (adjusted odds ratio [aOR] 0.294, 95% confidence interval [CI] 0.105–0.823) when controlling for wealth, demographics, self-rated health, and mixed effects from village level clustering. Self-rated good health was also negatively associated with client visits (aOR 0.668, 95% CI 0.462–0.967).
For caregiver visits, men with the most strongly-held harmful beliefs regarding three of the four gender norm measures remained significantly less likely to attend a caregiver visit (violence [aOR = 0.661, 95% CI 0.488–0.896], sexual dominance [aOR = 0.703, 95% CI 0.505–0.978], and women’s roles [aOR = 0.718, 95% CI 0.533–0.966]). Tests for collinearity showed no evidence that the gender norms were highly collinear. Age and marital status were also significantly associated with caregiver visits, with men over age 50 less likely to make caregiver visits than younger men (aOR 0.542, 95% CI 0.401–0.731) and married men more likely to make caregiver visits than non-married men (aOR 2.380, 95% CI 1.196–4.737). Employment status was not significant in the multivariable model.
The same analysis was conducted to understand factors associated with any visit (either client or caregiver) and no new independent factors were observed in the model (see Appendix C).
Discussion
We used data from a community-representative, cross-sectional survey with men in Malawi to understand factors associated with men’s attendance to health facilities within the past 12 months. Understanding which men are missed by general facility visits is critical to understand the role of integrated services for bridging the gap in men’s health care. We find that for client visits (whereby men access services for their own health), poor quality health services at local health facilities and feeling healthy at the time of the survey were negatively associated with facility visits; sociodemographic factors and harmful gender norms were not associated with client visits. For caregiver visits (whereby men support the health care of others), ascribing to harmful gender norms, being ≥ 50 years of age, and being unmarried were negatively associated with facility visits. Findings suggest that men’s general facility attendance as clients is, on the whole, equitable across a broad range of rural Malawian men. Men’s client visits could provide an equitable venue for increasing access to key services (such as HIV and TB screening) among men at the population level, without missing key sub-populations.
The lack of association between client visits and demographic and individual-level characteristics (such as age, economic status, or gender norms) is in contrast to the HIV and TB literature that shows poverty, low educational attainment, and harmful beliefs about gender norms are all negatively associated with men’s use of high-priority services. [18, 21, 24] Previous findings from Malawi using the same dataset found that 83% of men’s client visits are to outpatient departments for acute or curative care services, [6] suggesting that curative care may not have the same barriers as HIV and TB screening services. Divergent findings between men’s general facility attendance and HIV / TB services may also be impacted by how health services and HIV services are often organized around women’s and children’s health, which can create additional barriers to care that may not be present within outpatient departments. [3].
We found that poor quality health services at local health facilities was negatively associated with men’s general facility attendance for client visits. This finding highlights the importance of the clinic experience for continued use of care. Other research shows how quality is associated with utilization of services such as facility deliveries, [36] primary care, [35] and HIV care. [37] Future studies should include metrics on service quality when studying men’s use of health services in order to further understand this relationship.
This is one of the few studies to our knowledge to assess factors associated with men’s caregiver visits, outside of studies exclusively focused on prevention of mother-to-child transmission. Interestingly, we found very different factors associated with client versus caregiver visits. Client visits are motivated by men’s own health, often by an acute illness or injury. [6] Most men, regardless of demographics or beliefs about gender norms, may choose to seek curative care to receive immediate relief. Caregiver visits, however, are for the well-being of others, [40, 41] and men are rarely the only available caregivers – other family members may be able to perform the role of a caregiver so men can continue other activities. It is therefore unsurprising that the men who do choose to serve as caregivers have less restrictive views of gender norms and may value caregiving as a reasonable priority over income generation. [42, 43] Though our results show that caregiver visits are not made equally by all men, the result that 47% of participants had made a caregiver visit in the last year suggests these events may provide opportunities to familiarize men with the health care system and offer screening services.
Our findings challenge the notion that harmful beliefs regarding gender norms universally discourage men’s use of health services. [23, 24] The fact that gender norms were not associated with client visits, but were associated with caregiver visits, suggests that gender norms do not constrain all health-seeking behavior. Our results highlight that masculinity is one component among many in men’s dynamic decision-making process regarding engagement with health facilities. [26].
Our study has several limitations. First, our data relies on self-report and may be sensitive to social desirability and recall bias. Social desirability bias could affect men’s report of gender norm beliefs and health-seeking behavior, reducing our ability to detect relationships between gender norms and health-seeking behavior. However, because there was a clear and strong association between gender norm beliefs and caregiver visits, we are more confident in our null result for client visits. Recall bias may affect men’s recollection of the quality of services, though the effect should be minor for activities in the last 12 months and should affect all groups of men similarly. Second, and perhaps most importantly given our conclusions, our quality-of-care metrics are based on reports of respondents in this study. We considered alternative data sources, such as the Demographic Health Surveys Program’s Service Provision Assessment (SPA) data, but we felt that community perceptions of quality would be at least as relevant (if not more so) than official measures. In total, our respondents described an average of 115 visits per facility (range 61–163), many more than the SPA is able to observe. Third, our sampling frame was not designed for varying village size or population age distribution. The parent study conducted a sensitivity analysis using weights for village size and found no difference. [6] Finally, we did not ask about presence of pregnant people or older adult dependents living in respondents’ household, which may be positively associated with men making caregiver visits.
Conclusion
Factors associated with men’s facility attendance are nuanced and vary by the type of visit made – men’s facility attendance for their own health was only associated with quality of services available to them (and by their self-reported health), whereas men’s attendance as caregivers was associated with men’s strong acceptance of harmful gender norms. These findings suggest that client visits could be an entry point to reach the general male population. Our analysis also suggests that health system improvements may be the best tool to engage men in general health care.
Data Availability
Data is not currently available in a repository due to the sensitive information included in survey responses. Data is available to individuals by request via email to the corresponding author.
References
Global Health Observatory. In: Organization WH, ed. Geneva2018.
Roser M, Ritchie H. HIV/AIDS. In. Our World In Data. Online at OurWorldInData.org2018.
Dovel K, Dworkin SL, Cornell M, Coates TJ, Yeatman S. Gendered health institutions: examining the organization of health services and men’s use of HIV testing in Malawi. J Int AIDS Soc. 2020;23(Suppl 2(Suppl 2):e25517.
Kennedy CE, Fonner VA, Sweat MD, Okero FA, Baggaley R, O’Reilly KR. Provider-initiated HIV testing and counseling in low- and middle-income countries: a systematic review. AIDS Behav. 2013;17(5):1571–90.
Yeatman S, Chamberlin S, Dovel K. Women’s (health) work: A population-based, cross-sectional study of gender differences in time spent seeking health care in Malawi. PLoS One. 2018;13(12):e0209586.
Dovel K, Balakasi K, Gupta S, et al. Frequency of visits to health facilities and HIV services offered to men, Malawi. Bulletin of the World Health Organization. 2021;99(9).
Musoke D, Boynton P, Butler C, Musoke MB. Health seeking behaviour and challenges in utilising health facilities in Wakiso district, Uganda. Afr Health Sci. 2014;14(4):1046–55.
Balakasi K, Nichols BE, Mphande M, et al. Individual- and Facility-Level Factors Associated with Facility Testing among Men in Malawi: Findings from a Representative Community Survey. Diagnostics (Basel). 2021;11(6).
McNaghten AD, Schilsky Mneimneh A, Farirai T, et al. Implementation and Operational Research: Strengthening HIV Test Access and Treatment Uptake Study (Project STATUS): A Randomized Trial of HIV Testing and Counseling Interventions. J Acquir Immune Defic Syndr. 2015;70(4):e140–6.
Banda J. Willingness to Accept HIV Testing among Caretakers with a Child Attending the University Teaching Hospital in Lusaka, Zambia. Med J Zambia. 2013;40:55–9.
Dovel K, Shaba F, Offorjebe OA, et al. Effect of facility-based HIV self-testing on uptake of testing among outpatients in Malawi: a cluster-randomised trial. Lancet Glob Health. 2020;8(2):e276–87.
Rosser JI, Njoroge B, Huchko MJ. Changing knowledge, attitudes, and behaviors regarding cervical cancer screening: The effects of an educational intervention in rural Kenya. Patient Educ Couns. 2015;98(7):884–9.
Onono M, Blat C, Miles S, et al. Impact of family planning health talks by lay health workers on contraceptive knowledge and attitudes among HIV-infected patients in rural Kenya. Patient Educ Couns. 2014;94(3):438–41.
Onono M, Guzé MA, Grossman D, et al. Integrating family planning and HIV services in western Kenya: the impact on HIV-infected patients’ knowledge of family planning and male attitudes toward family planning. AIDS Care. 2015;27(6):743–52.
Ditekemena J, Koole O, Engmann C, et al. Determinants of male involvement in maternal and child health services in sub-Saharan Africa: a review. Reproductive Health. 2012;9(1):32.
Colvin CJ. Strategies for engaging men in HIV services. Lancet HIV. 2019;6(3):e191–200.
Hensen B, Lewis JJ, Schaap A, et al. Factors Associated with HIV-Testing and Acceptance of an Offer of Home-Based Testing by Men in Rural Zambia. AIDS and Behavior. 2015;19(3):492–504.
Quinn C, Kadengye DT, Johnson CC, Baggaley R, Dalal S. Who are the missing men? Characterising men who never tested for HIV from population-based surveys in six sub-Saharan African countries. J Int AIDS Soc. 2019;22(10):e25398.
Staveteig S, Head SK, Croft TN, Kampa KT. Factors associated with prior testing among HIV-positive adults in Sub-Saharan Africa. Rockville. Maryland: ICF International; 2016.
Kirakoya-Samadoulougou F, Jean K, Maheu-Giroux M. Uptake of HIV testing in Burkina Faso: an assessment of individual and community-level determinants. BMC Public Health. 2017;17(1):486.
Ante-Testard PA, Benmarhnia T, Bekelynck A, et al. Temporal trends in socioeconomic inequalities in HIV testing: an analysis of cross-sectional surveys from 16 sub-Saharan African countries. The Lancet Global Health. 2020;8(6):e808–18.
Omotoso D. Health Seeking Behaviour among the Rural Dwellers in Ekiti State, Nigeria. African Research Review. 2010;4(2).
Barker G, Ricardo C, Nascimento M, Olukoya A, Santos C. Questioning Gender Norms with Men to Improve Health Outcomes: Evidence of Impact. Global public health. 2009;5:539–53.
Chikovore J, Hart G, Kumwenda M, Chipungu GA, Corbett L. ‘For a mere cough, men must just chew Conjex, gain strength, and continue working’: the provider construction and tuberculosis care-seeking implications in Blantyre, Malawi. Glob Health Action. 2015;8:26292.
Leichliter JS, Paz-Bailey G, Friedman AL, et al. ‘Clinics aren’t meant for men’: sexual health care access and seeking behaviours among men in Gauteng province, South Africa. Sahara j. 2011;8(2):82–8.
Nzama N. Masculinity and Men’s health seeking behaviours amongst Black/African men: The case of Durban, KwaZulu-Natal, South Africa. School of Built Environment and Development Studies, University of KwaZulu-Natal; 2013.
Ganle JK, Dery I. ‘What men don’t know can hurt women’s health’: a qualitative study of the barriers to and opportunities for men’s involvement in maternal healthcare in Ghana. Reprod Health. 2015;12:93.
Nutor JJ, Duah HO, Agbadi P, Duodu PA, Gondwe KW. Spatial analysis of factors associated with HIV infection in Malawi: indicators for effective prevention. BMC Public Health. 2020;20(1):1167.
Mchenga M, Manthalu G, Chingwanda A, Chirwa E. Developing Malawi’s Universal Health Coverage Index. Frontiers in Health Services. 2022;1.
Filmer D, Pritchett LH. Estimating wealth effects without expenditure data–or tears: an application to educational enrollments in states of India. Demography. 2001;38(1):115–32.
Pulerwitz J, Segundo M, Nascimento M, Barker G. Promoting more gender-equitable norms and behaviors among young men as an HIV/AIDS prevention strategy. 2006.
Azad AD, Charles AG, Ding Q, Trickey AW, Wren SM. The gender gap and healthcare: associations between gender roles and factors affecting healthcare access in Central Malawi, June-August 2017. Arch Public Health. 2020;78(1):119.
Levtov RG, Barker G, Contreras-Urbina M, Heilman B, Verma R. Pathways to gender-equitable men: Findings from the international men and gender equality survey in eight countries. Men and Masculinities. 2014;17(5):467–501.
Ruark A, Chase R, Hembling J, Davis VR, Perrin PC, Brewster-Lee D. Measuring couple relationship quality in a rural African population: Validation of a Couple Functionality Assessment Tool in Malawi. PLOS ONE. 2017;12(11):e0188561.
Gage AD, Leslie HH, Bitton A, et al. Does quality influence utilization of primary health care? Evidence from Haiti. Global Health. 2018;14(1):59.
Kruk ME, Rockers PC, Mbaruku G, Paczkowski MM, Galea S. Community and health system factors associated with facility delivery in rural Tanzania: a multilevel analysis. Health Policy. 2010;97(2–3):209–16.
McCarthy EA, Subramaniam HL, Prust ML, et al. Quality improvement intervention to increase adherence to ART prescription policy at HIV treatment clinics in Lusaka, Zambia: A cluster randomized trial. PLoS One. 2017;12(4):e0175534.
SPA Questionnaires (ANC Client Exit Interview, FP Client Exit Interview, Sick Child Exit Interview). Available at https://dhsprogram.com/publications/publication-SPAQ6-SPA-Questionnaires-and-Manuals.cfm.
StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP. [computer program].
Manjate Cuco RM, Munguambe K, Bique Osman N, Degomme O, Temmerman M, Sidat MM. Male partners’ involvement in prevention of mother-to-child HIV transmission in sub-Saharan Africa: A systematic review. SAHARA-J: J Social Aspects HIV/AIDS. 2015;12(1):87–105.
Nkwonta CA, Messias DKH. Male Participation in Reproductive Health Interventions in Sub-Saharan Africa: A Scoping Review. Int Perspect Sex Reproductive Health. 2019;45:71–85.
Ditekemena J, Koole O, Engmann C, et al. Determinants of male involvement in maternal and child health services in sub-Saharan Africa: a review. Reprod Health. 2012;9:32.
Greenspan JA, Chebet JJ, Mpembeni R, et al. Men’s roles in care seeking for maternal and newborn health: a qualitative study applying the three delays model to male involvement in Morogoro Region, Tanzania. BMC Pregnancy and Childbirth. 2019;19(1):293.
Acknowledgements
The study authors would like to acknowledge the time and insight of the nearly 1,500 original participants surveyed for this dataset, the expertise of biostatistician Holly Wilhalme of the UCLA Department of Medicine, and the geocoding work of Vania Wang of UCSB.
Funding
The study was funded by the Foreign, Commonwealth and Development Office of the United Kingdom of Great Britain and Northern Ireland (grant #300380). Additional, individual support during the analysis phase included funding from the Fogarty International Center (K01-TW011484-01, UCLA CFAR grant AI028697), the Bill & Melinda Gates Foundation (grant #001423), and the National Institutes of Health (T32MH080634). The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Contributions
Conceptualization, MT and KD; methodology, KB, BEN, and KD; formal analysis, MT and KB; data verification, KD; writing—original draft preparation, MT; writing—reviewing and editing, KD, BEN, ND, KB, MM, IR, SK, and CS; supervision, MM, CS, and IR; funding acquisition, KD and BEN.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The parent study was approved by the National Health Sciences Review Committee (NHSRC) of Malawi and the University of California Los Angeles (UCLA) Institutional Review Board. All methods were performed in accordance with the guidelines of the two approving IRBs. Written, informed consent was ascertained from all respondents; written, informed assent was attained from respondents and written, informed consent was attained from parents or legal guardians for respondents between 15 and 17 years of age.
Consent for publication
Not applicable.
Competing interests
None of the authors have any competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Thorp, M., Balakasi, K., Mphande, M. et al. Factors associated with men’s health facility attendance as clients and caregivers in Malawi: a community-representative survey. BMC Public Health 22, 1904 (2022). https://doi.org/10.1186/s12889-022-14300-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-14300-8