Abstract
Background
Despite recent progress in rural economic development and food production, the prevalence of household food insecurity (FI) and use of unimproved toilet facilities are widespread in Bangladesh. Evidence regarding the consequencs of household FI and poor sanitation on child morbidity is scarce. This study aimed to understand the association of FI and unimproved toilet facility with morbidity status of under-5 children in Bangladesh.
Methods
We used data from a cross-sectional survey that was conducted as part of an evaluation of the Maternal, Infant and Young Child Nutrition (MIYCN) Program in 9 districts of Bangladesh. The study population included children aged 6–59 months and their caregivers, identified using a two-stage cluster-sampling procedure. Child morbidity status was the outcome variable, and household FI status and type of toilet used were considered the main exposure variables in this study. We performed logistic regression, calculated adjusted odds ratios (AOR) to assess the association of child morbidity with household FI and unimproved toilet facility after adjusting for potential confounders.
Results
A total of 1,728 households were eligible for this analysis. About 23% of the households were food-insecure, and a large number of households had improved toilet facilities (93.4%). In the multivariable logistic regression model, we found that children in food-insecure households with unimproved toilet facility had 5.88 (AOR: 5.88; 95% CI 2.52, 13.70) times more chance, of being morbid compared to the children of food-secure households with improved toilet facility. A similar association of FI and toilet facilities with each of the morbidity components was observed, including diarrhea (AOR:3.6; 95% CI 1.79, 7.89), fever (AOR:3.47; 95% CI 1.72, 6.99), difficult or fast breathing with cough (AOR:3.88; 95% CI 1.99, 7.59), and difficult or fast breathing with blocked or running nose (AOR:1.29; 95% CI 0.56, 2.95).
Conclusions
Our study shows that household FI and unimproved toilet facility jointly have more deteriorative effects on child morbidity than either of these conditions alone. Therefore, it is recommended to consider these two critical factors while designing a public health intervention for reducing morbidity among under-five children.
Similar content being viewed by others
Background
Household food insecurity (FI) is a measure of the availability of food in households and lack of access to an adequate amount of safe and nutritious food to fulfill dietary requirements for an active and healthy life [1]. FI is a multi-dimensional phenomenon that occurs in most countries at all income levels [2, 3], in 2020 globally 2.37 billion people remain food-insecure [3]. In 2020, the prevalence of experiencing severe FI was estimated at 60% in Africa, 26% in Asia, 50% in Latin America, and 9% in North America [3]. In Bangladesh, about 25% of the population remained FI in 2019 [4], despite the country making some progress in achieving food self-sufficiency through agricultural improvement, food production, as well as reducing under-five mortality [4]. According to the Global Food Security Index 2017, Bangladesh was ranked 89th out of 113 countries for prevalence of food insecurity [5].
Previous studies have identified several adverse consequences of household FI among infants and young children [6], including long-term impacts on children’s health [7]. Studies conducted in low-income settings [6,7,8,9,10] observed significant associations between household FI and childhood illness. For example, a study in Ethiopia observed household FI as a significant risk factor for increasing morbidity. FI increased the risk of childhood diarrhea 1.44 times, cough 1.42 times and fever 1.53 times compared to children in food-secure households [8]. Children in FI households are also at risk of poor development, impaired performance in school and depression and poor health in adulthood, and are more likely to be stunted and suffer from undernutrition [11,12,13]. FI in children plays out through nutritional and non-nutritional pathways that lead to poor-quality diet (higher consumption of energy, fat, sugar, and fiber), less physical activity and their developmental consequences [14]. FI in children was significantly associated with iron deficiency anemia among infants and young children which indicate deleterious health, social, behavirorial and cognitive consequences for children [15].
As well, measuring FI alone may not be sufficient in assessing child morbidity-outcome risks if the other major driver of such morbidity, in terms of sanitation, is not considered [16]. Despite consistent improvement in rural economic development in Bangladesh, national survey data shows 57% of households were using unimproved toilet facilities in 2017 [17] and elsewhere a study showed not owning a toilet increased the likelihood of being a food insecure household [18]. The effect of unimproved toilet facilities on child undernutrition and childhood morbidity have been well established [19, 20]. A study conducted in rural northern Bangladesh observed that the use of unimproved toilet facilities increased the risk of childhood acute respiratory infection by 31% [21]. A study in India showed that access to an improved toilet can reduce childhood diarrhea by more than 2% [20]. Another recent study conducted in Myanmar observed children in the household with unimproved toilet facility were at significantly higher risk of suffering from cough and fever compared to households with improved toilets [22].
Although numerous studies have assessed the independent effect of household FI and unimproved toilet facilities on child morbidities [6,7,8,9,10], to our knowledge, no study has measured the combined effect of household FI and unimproved toilet facility on the morbidity status of children. This paper aimed to understand the association of FI and unimproved toilet with morbidities of under-5 children in Bangladesh. We expect that the findings of this study will inform the development of programs to improve child health outcomes through consideration of combinations of risk factors.
Methods
Data source
In this paper, we used the data from a cross-sectional survey that was conducted as part of an evaluation of the Maternal, Infant and Young Child Nutrition (MIYCN) Program of BRAC (formerly known as Bangladesh Rural Advancement Committee), an international non-governmental organization based in Bangladesh. Data was collected during April–May 2016.
Study area
The study area comprised nine districts including Barguna, Bogra, Chittagong, Comilla,Cox’s Bazar, Dinajpur, Feni, Jessore, Meherpur of Bangladesh where BRAC was implementing its MIYCN program (Fig. 1). BRAC has selected these districts considering the availability BRAC programme-delivery infrastructures including the availability of its community health workers who were trained to implement the MIYCN interventions at the community level.
Study population
The study population included children aged 6–59 months and their caregivers. The caregiver was defined as the child’s biological mother or the person who takes care of or looks after and gives the child most meals on most days in the past seven days before the survey. Inclusion criteria allowed selection of the households of caregivers who had at least one child of 6–59 months and where the caregivers had resided in that household for at least one year. We excluded households if the caregiver was unable to attend an interview during the day of the survey due to illness or was unable to give consent to participate in the survey. If the household has more than one eligible child, we randomly selected one child for the survey.
Sample-size and sampling
We calculated sample-size for a district-level estimation; we considered 50% prevalence, the precision of ± 10%, Zα value of 1.96, and a design effect of 2. The use of the standard sample-size calculation formula yielded the minimum sample-size of 192 households per district. Thus, the total sample-size was 1,728.
We followed a two-stage cluster-sampling procedure. In the first stage, systematic random- sampling was applied to select 16 Primary Sampling Units (PSUs) from the complete list of BRAC communities in a district. This procedure helped to ensure the equal chance of being included in the sample, and the resulting sample was close to an even spatial sample of BRAC’s target areas. In the second stage, the survey team ensured the population-size, total approximate households, and the boundaries of the PSU on arrival at the selected PSU and in consultation with and assistance of the local people (Union Parishad Chairman, Member, Counselor, school teacher, elderly person, and the relevant personnel of the locality). A physical map-segment sample approach was exercised to segment the selected community or PSU. The detailed sampling procedures have been reported elsewhere [23].
Outcome variable
Child morbidity status was the outcome variable for this study. We considered children to be experiencing morbidity if their caregivers reported that their child had been sick either due to ailments, such as diarrhea (diarrhea with 3 or more loose or watery, bloody, pussy or mucous stools in a 24 h period), fever (illness with fever), illness with cough and had difficulty in breathing or fast breathing, difficult or fast breathing with blocked or runny nose in the last 14 days before the survey. In addition to the caregivers recall, we also collected child’s morbidity related information from the doctor’s prescriptions/medicines if the child received any treatment from a doctor during the last episode of illness. If caregivers reported any of the illnesses being present in their child, or if medical records indicated a sickness episode, then we considered them as experiencing morbidity.
Exposure variable and covariates
Household FI status (categorized as food-insecure, food-secure) was considered the main exposure variable in this study. We assessed households FI status based on 9 questions (Additional file 1) from the Household Food Insecurity Access Scale (HFIAS) developed by the Food and Nutrition Technical Assistance (FANTA) group in collaboration with Tufts University and Cornell University [24]. The response to each question ranges from 0 to 30. We made scoring of these responses as 0 = 0, 1–2 = 1, 3–10 = 2, and 11–30 = 3. The total score ranged from 0 to 27 for 9 questions. We then categorized as score 0–1 = food-secure household and 2–27 = food-insecure household. Other exposure variables included toilet availability, categorized as: Improved toilet (flush or pour flush to a piped sewer system, septic tank, pit latrine, Kumasi Ventilated Improved Pit latrine, pit latrine with slab), unimproved toilet (pit latrine without a slab, hanging latrine or defecate in bush or field). We also combined food security and toilet facilities of households to see the combined effects in regression analysis and we categorized them as: Food-secure and improved toilet, Food-secure and unimproved toilet, Food-insecure and improved toilet, Food-insecure and unimproved toilet.
Other covariates included household-size (categorized as: < 5, ≥ 5), number of 6–59 months old children in the household (categorized as: one, two, or more), child’s age (6–23 months, 24–59 months), any children in the household aged 5–14 year who were attending school, caregiver’s age (< 25 years, ≥ 25 years), caregiver’s education (< 5 years, ≥ 5 years), father’s age (categorized as: < 30 years, ≥ 30 years), caregiver’s religion (categorized as: Muslim, Hindu/Other religion), caregiver’s occupation (categorized as: other, housewife), wealth index (categorized as: poor, middle, rich), and monthly household income [categorized as: < 11,000 BDT (Bangladeshi taka), ≥ 11,000 BDT (83 BDT = 1 USD)]. A supplementary file on response categories and variable description has been described about the variables used in this study (Supplementary table 1).
Data collection
The study was conducted in accordance with the National/International human ethics guidelines and regulations. Before data collection all participants provided written informed consent. To collect data, we formed a survey team of four members, including two interviewers, a medical technologist, and a supervisor. At the time of recruitment of team members, priority was given to the members who were experienced and/or involved in the previous surveys. The supervisor was mainly responsible for selection of the study participants, using the mentioned sampling methods, monitoring the data-collection activities, and ensuring the quality of the data by spot-checking and re-interviewing.
We measured the level of anxiety and uncertainty of the participants about household food supply, insufficient quality of food, and insufficient food intake by following the HFIAS that comprises a brief survey instrument to assess whether households have experienced problems with accessing food during the last 30 days of survey. The questionnaire used a nine-item household hunger scale questionnaire [(i) worry about food, (ii) unable to eat preferred foods, (iii) eat just a few kinds of foods, (iv) eat foods they really do not want to eat, (v) eat a smaller meal, (vi) eat fewer meals in a day, (vii) no food of any kind in the household, (viii) go to sleep hungry, and (ix) go a whole day and night without eating)].
Before finalizing the questionnaire, a field test was conducted in a real-field setting in the non-survey areas, and the feedback from the field test was incorporated into the final version of the questionnaire. It was then submitted to the Institutional Review Board (IRB) of icddr,b for review and approval. A Standard Operating Procedure (SOP) was developed for the interviewers. This SOP was a guide for the interviewers on how to ask each of the questions to the participants. The electronic data-collection procedures used an Android-based Smartphone program of survey questionnaire. To support the Android operating system, Open Data Kit (ODK) software was used for developing the program. TABs/Smartphones were used and both Bangla and English versions questionnaire were used in the ODK software.
Data analysis
Weighted and cluster (PSU)-adjusted descriptive statistics were estimated and presented in percentages with respective 95% confidence intervals. Bivariate analysis using a chi-square test was performed to measure the association between the outcome variable (morbidity status of the children) and main exposure variables (household FI and toilet facilities). We performed multivariable logistic regression analysis to measure the association between outcome variables and other independent variables. At first, we performed unadjusted logistic regression to find the significant variables for the final multivariable regression model; p-value of < 0.05 was considered for the significance level. Finally, multivariable logistic regression was performed to assess the association of child morbidity with household FI and unimproved toilet facility after adjusting for potential confounders and presented in adjusted odds ratios with a 95% confidence interval. All analyses were performed using statistical software STATA (Version 13).
Results
Socio-demographic and background characteristics of the study participants have been presented in Table 1. A total of 1,728 households were eligible for this analysis. Around 61% of households had ≥ 5 members, and about 85% had one child aged 6–59 months of age. Most of the selected respondents were biological mothers (97%) of the eligible children. Caregivers aged > 25 years were 55 and 76.2% of the caregivers had completed ≥ 5 years of schooling. About 68% of fathers of the eligible children completed five or more years of schooling.
Sixty percent of the children belonged to the age-group of 24–59 months. Around 97% of the children aged 5 to 14 years were attending school. The ratio of boys and girls was 53:47. Fifty-six percent of caregivers of under-5 children reported that their children had been sick in the last two weeks prior to the day of the interview. Results showed that about 23% of the households were food-insecure, and a large number of households had improved toilet facilities (93.4%).
Table 2 presents the association of morbidity status with food security and toilet facility status of the households. There was a significant (p < 0.001) association between morbidity status and either FI or unimproved toilet facility in the household. In food-secure households, 52.8% of children were found with morbidity but, in food-insecure households, child morbidity prevailed among 66.5% of households (p < 0.001). About 55% of children from households that had improved toilet facility had morbidity whereas this figure was about 75% in the households that had unimproved toilet facilities (p < 0.001). In the unadjusted logistic regression model, we found that the children of food-insecure households had 77% (OR: 1.77; 95% CI 1.27–2.47) more likelihood of being morbid compared to children of food-secure households. Children of households with unimproved toilet facilities had 2.44 (OR: 2.44; 95% CI 1.46–4.06) times higher chances to be morbid compared to children of households with improved toilet facilities (Table 2).
In multivariable logistic regression, we adjusted the model with caregiver’s education, caregiver’s religion, number of children aged 6–59 months in the household, household income, household food security status, and toilet facility of the household; it was found that children of food-insecure households were 60% (AOR: 1.60; 95% CI 1.15, 2.22) more likely to be morbid compared to children of food-secure households (Table 2). Furthermore, children of households with unimproved toilet facilities had 2.08 (AOR: 2.08; 95% CI: 1.24, 3.48) times higher likelihood of being morbid compared to children of households with improved toilet facilities (Table 2).
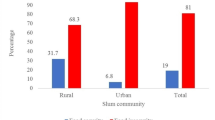
The simple and multivariable logistic regression model to explore the associated factors of morbidity status is presented in Table 3. In the unadjusted logistic regression model, we found age of children, household income, and combination of food security and toilet facility to be significantly associated with morbidity status of under-five children. In the multivariable logistic regression model, we considered all significant variables of the simple logistic regression model and found that children of food-insecure households with improved toilet facility had 53% (AOR: 1.53; 95% CI 1.09, 2.15) more chance, and food-insecure children with unimproved toilet facility had 5.88 (AOR: 5.88; 95% CI 2.52, 13.70) times more chance, of being morbid compared to the children of food-secure households with improved toilet facility (Table 3). A similar association of food security and toilet facilities with each of the morbidity components was observed, including diarrhea (AOR:3.6; 95% CI 1.79, 7.89), fever (AOR:3.47; 95% CI 1.72, 6.99), difficult or fast breathing with cough (AOR:3.88; 95% CI 1.99, 7.59), and difficult or fast breathing with blocked or running nose (AOR:1.29; 95% CI 0.56, 2.95) (Fig. 2).
Discussion
The findings of this study revealed that household FI and unimproved toilet facility have independent effects on child morbidity. However, FI and unimproved toilet facility combined can have a more severe effect than either alone. These findings have important implications for the development of programmes to alleviate common childhood diseases. Some other studies have reported the association between FI and general health consequences [25,26,27]; studies also have shown that poor general health, mental and physical health have a relationship with FI [28, 29]. Studies conducted in Brazil and Colombia found that household FI and child morbidity, such as diarrheal disease among the children, were significantly associated [3, 9] corresponding to the findings of our study.
The interventions or programs taken so far in low- and middle-income countries are vertical and specific to address one particular problem: either FI or child morbidity. Their relationship is often overlooked while designing an intervention. Nevertheless, an integrated program could be cost-effective targeting both improving food security and sanitation status of the households, and, thus, to reduce child morbidity. A prevous study considered both household FI and adequate access to water and sanitation behaviour suggesting the consideration of integrated interventions to reduce acute malnutrition and childhood morbidity among children [30]. A study in Ethiopia showed that Integration of WASH and nutrition was associated with less stunting and disease in children 0–59 months in a setting with poor WASH conditions [31]. That was also supported by the recent analysis showing integrating antihelminth treatement with the home fortification with micornutrients powders reduced anaemia among children in Bangladesh [32].
It is very likely that the food-insecure households have poor living conditions. The unimproved toilet is one of the dimensions of poor living conditions. Studies indicate that the use of unimproved toilets increases the burden of diseases, like diarrhea among poor children [10, 33]. A recent study conducted in Cameroon suggested that children from households practicing open defecation and/or having poor hygiene practices had higher chance of developing diarrhea [30].Our study also found that the children belonging to food-insecure households having unimproved toilet facilities are more likely to suffer from diarrhoea, fever, and fast breathing with cough. Therefore, the study corroborates with the suggested potential nutrition-sensitive interventions such as social protection and safety net program to improve food security and living conditions of the households leading to improvement of child health [34].
Other studies also show that younger children are more susceptible to morbidity when compared to their older counterparts [35]. Apart from household FI and unimproved toilet facility, child’s age is also found to be associated with morbidity in our study. Childhood morbidity, particularly diarrheal diseases, are more prevalent among the younger children compared to the older ones [36]. Since child’s age is a non-modifiable factor, the study suggests undertaking of interventions targeting the younger children for reducing morbidity, irrespective of household food security and living conditions.
Limitations and strengths
Being a community-based study; the participation rate was considerably high as the respondents were at the households during the day of the interview. The survey was cross-sectional and, so, it was difficult to assess the causality between the outcome and exposure variables. Morbidity assessments were self-reported by children caregivers through recall of the preceding two weeks from the date of the interview; so, there was a possibility of recall bias. FI data were collected through recall, and the situation prevailed in the past 30 days. The accuracy of data depended on the respondent’s memory and honesty. To overcome this, the interviewers were given special training to increase the ability to understand the questions to be asked to the respondents. Self-reported family income and expenditure could also be subject to bias. In the multiple regression model, we didn't include the wealth index variable. We included only three variables, child's age, household income and combined food security and toilet facilities of households, which were found significant in the simple regression model. However, we also checked the multicollinearity among these three variables and found the mean VIF (variance inflation factor) is 1.07 and the individual VIF ranges from 1.00 to 1.10, which indicating the negligible collinearity among the independent variables.
Conclusions
Our study shows that household FI and unimproved toilet facility jointly have more deteriorative effects on child morbidity than either of these conditions alone. Unlike other studies, this illustrates the independent and combined effects of household FI and unimproved toilet facility on child morbidity. Taking measures on food security at the household level may not be sufficient to develop the nutritional status of children, rather an integrated programme on food security and sanitation is recommended to improve the overall health outcomes of the children. This evidence could show the pathway for the implementers and policy-makers that intervention targeting the improvement of the health status of children should not only consider the food security status of the households but also the sanitation condition of the households.
Availability of data and materials
The data that support the findings of this study are available from corresponding author (HS) upon reasonable request and with permission of icddr,b IRB.
Abbreviations
- FI:
-
Food insecurity
- MIYCN:
-
Maternal, Infant and Young Child Nutrition
- AOR:
-
Adjusted odds ratios
- BRAC:
-
Bangladesh Rural Advancement Committee
- PSU:
-
Primary Sampling Units
- HFIAS:
-
Household Food Insecurity Access Scale
- FANTA:
-
Food and Nutrition Technical Assistance
- BDT:
-
Bangladeshi taka
References
Napoli, M., Muro, P. De & Mazziotta, M. Towards a food insecurity Multidimensional Index (FIMI). Romatre: Universita Degli Studi. 2011. http://www.fao.org/fileadmin/templates/ERP/uni/FIMI.pdf. Last accessed on 22 Aug 2021.
Norhasmah S, Zalilah MS, Mohd Nasir MT, Kandiah M, Asnarulkhadi AS. A Qualitative Study on Coping Strategies among Women from Food Insecurity Households in Selangor and Negeri Sembilan. Malays J Nutr. 2010;16(1):39–54.
FAO, IFAD, UNICEF, WFP and WHO. 2021. The State of Food Security and Nutrition in the World 2021. Transforming food systems for food security, improved nutrition and affordable healthy diets for all. Rome, FAO. https://doi.org/10.4060/cb4474en
USAID. 2019, May 21. Agriculture and Food Security. Accesssed https://www.usaid.gov/bangladesh/agriculture-and-food-security.
Global Food Security Index (2017). Report from Economist Intelligence Unit. Retrieved from: https://foodsecurityindex.eiu.com/Home/DownloadResource?fileName=EIU%20Global%20Food%20Security%20Index%20-%202017%20Findings%20%26%20Methodology.pdf. Last accessed 22 August 2021.
Haque MA, Farzana FD, Sultana S, Raihan MJ, Rahman AS, Waid JL. Factors associated with child hunger among food insecure households in Bangladesh. BMC Public Health. 2017;17(1):205.
Kirkpatrick SI, McIntyre L, Potestio ML. Child hunger and long-term adverse consequences for health. Arch Pediatr Adolesc Med. 2010;164(8):754–62.
Anderson LC, Tegegn A, Tessema F, Galea S, Hadley C. Food insecurity, childhood illness and maternal emotional distress in Ethiopia. Public Health Nutr. 2011;15(4):648–55.
Gubert MB, Spaniol AM, Bortolini GA, Pérez-Escamilla R. Household food insecurity, nutritional status and morbidity in Brazilian children. Public Health Nutr. 2016;19(12):2240–5.
Ohemeng A, Marquis GS, Lartey A. Household food insecurity is associated with respiratory infections among 6–11-Month old infants in rural ghana. Pediatr Infect Dis J. 2015;34(8):821–5.
Chilton M, Rose D. A rights-based approach to food insecurity in the United States. Am J Public Health. 2009;99(7):1203–11.
Sarma H, Khan JR, Asaduzzaman M, Uddin MF, Tarannum S, Hasan MM, Rahman AS, Ahmed T. Factors influencing the prevalence of stunting among children aged below five years in Bangladesh. Food Nutr Bull. 2017;38(3):291–301.
Ali D, Saha KK, Nguyen PH, Diressie MT, Ruel MT, Menon P, Rawat R. Household food insecurity is associated with higher child undernutrition in Bangladesh, Ethiopia, and Vietnam, but the effect is not mediated by child dietary diversity. J Nutr. 2013;143(12):2015–21.
Fram MS, Ritchie LD, Rosen N, Frongillo EA. Child experience of food insecurity is associated with child diet and physical activity. J Nutr. 2015;145(3):499–504. https://doi.org/10.3945/jn.114.194365.
Skalicky A, Meyers AF, Adams WG, Yang Z, Cook JT, Frank DA. Child food insecurity and iron deficiency anemia in low-income infants and toddlers in the United States. Matern Child Health J. 2006;10(2):177–85. https://doi.org/10.1007/s10995-005-0036-0.
Iram U, Muhammad S, Butt. Determinants of household food security: an empirical analysis for Pakistan. Int J Soc Econ. 2004;31:8753–66. https://doi.org/10.1108/03068290410546011.
National Institute of Population Research and Training (NIPORT). Bangladesh demographic and health survey 2017–18: Key indicators. https://dhsprogram.com/pubs/pdf/PR104/PR104.pdf. Last accessed on 2 Aug 2021.
Rukundo PM, Rukooko B, Andreassen BA, Iversen PO. Housing, water and sanitation implications on food insecurity and diet diversity in landslide affected communities: a cross-sectional survey of two districts in Uganda. Clin Nutr ESPEN. 2019;33:47–56. https://doi.org/10.1016/j.clnesp.2019.07.010.
Mesagan PE, Adeniji-Ilori OM, Fudan J. Household environmental factors and childhood morbidity in South-Western Nigeria. Hum Soc Sci. 2018;11:411. https://doi.org/10.1007/s40647-017-0204-9.
Kumar S, Vollmer S. Does access to improved sanitation reduce childhood diarrhea in rural India? Health Econ. 2013;22(4):410–42.
Ullah MB, Mridha MK, Arnold CD, Matias SL, Khan MS, Siddiqui Z, Hossain M, Paul RR, Dewey KG. Factors associated with diarrhea and acute respiratory infection in children under two years of age in rural Bangladesh. BMC Pediatr. 2019;19(1):1–1.
Naz L, Ghimire U. 2020. Unimproved water, sanitation, and hygiene (WASH) and common childhood illness in Myanmar: evidence from a nationally representative survey. https://doi.org/10.21203/rs.3.rs-36037/v1
Sarma H, Mbuya MN, Tariqujjaman M, Rahman M, Askari S, Khondker R, Sultana S, Shahin SA, Bossert TJ, Banwell C, Neufeld LM. Role of home visits by volunteer community health workers: to improve the coverage of micronutrient powders in rural Bangladesh. Public Health Nutr. 2021;24(S1):s48-58.
Coates J, Swindale A, Bilinsky P. Household food insecurity access scale (HFIAS) for measurement of household food access: Indicator guide (v. 3). Washington, DC: food and nutrition technical assistance project, academy for educational Development. 2007 Aug:1–36. http://www.fao.org/fileadmin/user_upload/eufao-fsi4dm/doc-training/hfias.pdf. Last accessed on 22 Aug 2021.
Stuff JE, Casey PH, Szeto KL, Gossett JM, Robbins JM, et al. Household food insecurity is associated with adult health status. J Nutr. 2004;134(9):2330–5.
Casey PH, Szeto KL, Robbins JM, Stuff JE, Connell C, Gossett JM, et al. Child health-related quality of life and household food security. Arch Pediatr Adolesc Med. 2005;159(1):51–6.
Sharkey JR, Johnson CM, Dean WR. Relationship of household food insecurity to health-related quality of life in a large sample of rural and urban women. Women Health. 2011;51(5):442–60.
Huddleston-Casas C, Charnigo R, Simmons LA. Food insecurity and maternal depression in rural, low-income families: a longitudinal investigation. Pub Health Nutr. 2009;12(8):1133–40.
Leung CW, Epel ES, Willett WC, Rimm EB, Laraia BA. Household food insecurity is positively associated with depression among low income supplemental nutrition assistance program participants and income-eligible nonparticipants. J Nutr. 2015;145(3):622–7.
Nounkeu CD, Teta I, Dharod JM, Saha Foudjo BU, Ntentie FR, Boris AK, et al. Limited water access is associated with food insecurity and diarrheal episodes among children suffering from moderate acute malnutrition in Far-North Cameroon. J Water Sanit Hyg Dev. 2022;12(1):68–79.
Head JR, Freeman MC. Integration of water, sanitation, hygiene and nutrition programming is associated with lower prevalence of child stunting and fever in oromia, Ethiopia. African J Food, Agric Nutr Dev. 2019;19(4):1480–83.
Sarma H, Wangdi K, Tariqujjaman M, Das R, Rahman M, Kelly M, et al. The effects of deworming and multiple micronutrients on anaemia in preschool children in bangladesh: analysis of five cross-sectional surveys. Nutrients. 2022;14(1):150.
Cook JT, Frank DA, Levenson SM, Neault NB, Heeren TC, Black MM, et al. Child food insecurity increases risks posed by household food insecurity to young children’s health. J Nutr. 2006;136(4):1073–6.
Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S, et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet. 2013;382(9890):452–77. https://doi.org/10.1016/s0140-6736(13)60996-4.
Kamal MM, Hasan MM, Davey R. Determinants of childhood morbidity in Bangladesh: evidence from the demographic and health survey 2011. BMJ Open. 2015;5:e007538. https://doi.org/10.1136/bmjopen-2014-007538.
Woldemicael G. Diarrhoeal morbidity among young children in eritrea: environmental and socioeconomic determinants. J Health Popul Nutr. 2001;19(2):83–90.
Acknowledgements
All authors and icddr,b acknowledge with gratitude the commitment of CIFF to its research efforts; icddr,b is also grateful to the core donors: the Governments of the People’s Republic of Bangladesh, Canada, Sweden, and the UK for providing core/unrestricted support. The authors thank BRAC and GAIN for their assistance in conducting the study and the study participants for their participation and giving their valuable time. The authors also thank all members of the research team who helped during data collection.
Funding
Research for this article was funded by the Children’s Investment Fund Foundation (CIFF), UK. The views, opinions, assumptions, or any other information set out in this article are solely those of the authors and should not be attributed to CIFF or any person connected with CIFF.
Author information
Authors and Affiliations
Contributions
M.A.I. and H.S. conceptualized the paper. M.A.I., M.T., M.R., H.S., and G.K. engaged in formal analysis. M.A.I., M.R., M.F.U., and H.S. prepared the first draft. M.A.R., M.K., D.G., and T.A. critically reviewed and provided technical feedback on the draft version of the paper. H.S. rewrite and finalized the paper considering review comments from all authors. All authors reviewed and approved the final version of the paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the National/International guidelines. This study was approved by the IRB of icddr,b which comprises a Research Review Committee and an Ethical Review Committee (Protocol number PR-14048). Written consents were taken from all caregivers before taking any interview. The participants were informed by the interviewer that their participation is voluntary and they have the right not to answer any question or to withdraw themselves any time during the interview.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Household Hunger Scale questionnaire.
Additional file 2:
Supplementary Table 1. Questions, responses and variables description used in this paper.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Islam, M.A., Rahman, M., Uddin, M.F. et al. Household food insecurity and unimproved toilet facilities associate with child morbidity: evidence from a cross-sectional study in Bangladesh. BMC Public Health 22, 1075 (2022). https://doi.org/10.1186/s12889-022-13469-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-13469-2