Abstract
Background
High-frequency hearing loss is a significant occupational health concern in many countries, and early identification can be effective for preventing hearing loss. The study aims to construct and validate a risk model for HFHL, and develop a nomogram for predicting the individual risk in noise-exposed workers.
Methods
The current research used archival data from the National Key Occupational Diseases Survey-Sichuan conducted in China from 2014 to 2017. A total of 32,121 noise-exposed workers completed the survey, of whom 80% workers (n = 25,732) comprised the training cohort for risk model development and 20% workers (n = 6389) constituted the validation cohort for model validation. The risk model and nomogram were constructed using binary logistic models. The effectiveness and calibration of the model were evaluated with the receiver operating characteristic curve and calibration plots, respectively.
Results
A total of 10.06% of noise-exposed workers had HFHL. Age (OR = 1.09, 95% CI: 1.083–1.104), male sex (OR = 3.25, 95% CI: 2.85–3.702), noise exposure duration (NED) (OR = 1.15, 95% CI: 1.093–1.201), and a history of working in manufacturing (OR = 1.50, 95% CI: 1.314–1.713), construction (OR = 2.29, 95% CI: 1.531–3.421), mining (OR = 2.63, 95% CI: 2.238–3.081), or for a private-owned enterprise (POE) (OR = 1.33, 95% CI: 1.202–1.476) were associated with an increased risk of HFHL (P < 0.05).
Conclusions
The risk model and nomogram for HFHL can be used in application-oriented research on the prevention and management of HFHL in workplaces with high levels of noise exposure.
Similar content being viewed by others
Introduction
Occupational hearing loss is the second most common form of sensory-related hearing loss after age-related hearing loss and is a major occupation-related condition worldwide [1]. The World Health Organization (WHO) reported that 16% of adult hearing loss cases were caused by occupational noise exposure [2]. The WHO also indicated that the number of individuals with hearing loss could increase to 630 million by 2030 and may reach more than 900 million by 2050 [3].
As one of the largest global producers, China has many manufacturing, construction, and mining enterprises [4]. Noise pollution has become one of the key public hazards [5]. Due to the high cost of occupational noise services, mismanagement of occupational health and insufficient personal protective equipment for noise-exposed workers [6], the National Health and Family Planning Commission (NHFPC) of the People’s Republic of China (PRC) reported that the incidence of occupational ear, nose and throat diseases (OENTD) has increased in recent years. New cases of OENTD exceeded those of occupational poisoning to become the second most common occupational disease after occupational pneumoconiosis since 2015, and 95.90% of OENTD cases were noise-induced hearing loss (NIHL). From 2015 to 2019, the NHFPC reported that the numbers of new cases of OENTD were 1097 cases, 1276 cases, 1608 cases, 1528 cases, and 1623 cases, respectively [7,8,9,10,11].
In 2009, the China Centers for Disease Control and Prevention (CDC) launched the National Key Occupational Diseases Survey (NKODS), a nationwide surveillance project of ten key occupational hazards, namely, coal dust (coal silica dust), silica dust, asbestos, benzene, lead, noise, brucella, welding fumes, carbon disulfide, and phosphorus compounds, to cope with the increasingly severe challenges of occupational diseases. Noise is one of the ten key occupational hazards in the NKODS. The NKODS-Sichuan is the provincial level surveillance project of the NKODS.
HFHL is a characteristic of occupational hearing loss that develops slowly, affecting the higher frequencies first and extending gradually to the lower frequencies [12]. Previous studies focused on the prevalence or factors of HFHL in different regions [13,14,15,16,17], HFHL-related diseases [18,19,20], and HFHL-related mental disorders [21,22,23]. Regarding the risk model, the researchers paid more attention to the modelling of noise exposure risk in the workplace. However, few studies have provided risk models of HFHL or hearing loss. Lewkowski et al. [24] identified the risk of miners for developing occupational hearing loss and they found that miners who used planers, sanders, grinders, large machinery, and power hammers in work tended to suffer a high-level noise exposure. Pentti Kuronen et al. [25] constructed a risk model of NIHL in military pilots. It is well known that pilots have better health surveillance and management than other professions. Hong et al. [26] developed a prediction model using 379 South African adults, the predictors included the CD4 count, age, serum albumin level, and body mass index. This model can identify participants with drug resistant tuberculosis who are at high risk of developing minoglycoside-induced hearing loss. This research modelling the risk of disease-related hearing loss is not the same as the hearing loss induced by occupational noise. Therefore, this risk model is not appropriate for predicting HFHL in noise-exposed workers. Kuang et al. [27] predicted the individual risk of HFHL in 822 machinists. The predictors included age, sex male, limited earplug wearing, and high noise intensity. These results provide theoretical support for the prevention of HFHL among machinists. However, this study still has some limitations. On the one hand, the study was limited by its single-centre design, small sample size, and industry type whereby all the objects were mechanists. On the other hand, the study lacked an additional set of objects for external validation as well as a cut-off point to identify the high and low risk groups of workers. Furthermore, most studies have shown that the industry type and enterprise type are related to hearing loss [28]. The early prediction and diagnosis of HFHL in different industrial and enterprise types could provide evidence for the comprehensive prevention of HFHL.
Nomograms are pictorial representations of a complex mathematical formula and are reliable and convenient statistical predictive tools based on the indicators of a clinical event, enabling the calculation of an individual probability with a simple and visual graphical representation [29]. Nomograms are widely used to predict the probability of the higher risk of disease in clinical, which is usually used to predict survival in cancer patients, especially prostate cancer and breast cancer [30, 31]. Few studies on the development of a nomogram for HFHL have been published. As workers in high noise environments are at a high risk of hearing loss, especially HFHL, a risk model and nomogram may be valuable for management and prevention in workplaces with high levels of noise exposure. The approaches for assessing occupational noise exposure have been tested, such as questionnaire-based algorithms [32] and artificial intelligence [33]. However, those studies assessed noise exposure in the workplace or risk assessment of different task. Based on the current situation of HFHL, the development of a predictive tool using the NKODS dataset is a valuable effort for applied research on HFHL prevention. Besides, Chinese researchers have suggested that a predictive tool based on the NKODS dataset would be valuable in China to help regulators and managers effectively use the NKODS dataset and provide early warning for populations at risk for HFHL [34].
Considering the above-mentioned information, the objective of this study was to construct a risk model to identify the predictors of HFHL and develop a HFHL nomogram to calculate the individual risk for noise-exposed workers. The results of this study are expected to provide technical support and enhance application-oriented research on HFHL.
Materials and methods
Research data collection
In the NKODS-Sichuan, every trained health technicians collected the data of basic information and audiometric testing for noise-exposed workers, and entered the data into the NKODS-Sichuan Report System. In this study, we used the basic information and audiometric testing data from the NKODS-Sichuan dataset, collected from 2014 to 2017. The basic information was comprised of two sections: (1) company information including the company name, address, industry type, and enterprise type; and (2) personal information including the worker’s name, phone number, sex, date of birth, NED, exposure to occupational hazards, medical history and family history.
The audiometric testing consisted of a pure tone audiogram (PTA) examination. According to the national standard, Technical Specifications for Occupational Health Surveillance (GBZ 188–2014), audiometric testing were preceded by a period of at least 48 h without exposure to occupational noise. A noisy environment was defined as one with a noise equivalent intensity level greater than 80 dB based on the national Guidelines for Risk Management of Occupational Noise Hazard (AQ/T 4276-2016). The testing was carried out in a sound-isolating room [background noise less than 30 dB] in designated hospitals by trained health technicians. The audiometric testing consisted of: (1) Routine examinations of both ears. The routine examinations including the otoscopic examination was performed for each worker by an otolaryngologist to detect any ear pathology potentially affecting hearing function. The examination checklist also included eustachian tube function test, vestibular function test. (2) Thresholds were obtained three times at six different frequencies (0.5, 1, 2, 3, 4 and 6 kHz), with an interval between tests of at least 3 days. The BHFTA was used to diagnose HFHL, which was calculated using the arithmetic mean of the hearing thresholds at 3, 4, and 6 kHz in both ears. According to the national guidelines of Technical Specifications for Occupational Health Surveillance(GBZ 188–2014), 8 kHz was not included in the audiometric testing. The diagnostic gradation for NIHL was calculated based on the minimum threshold of three consecutive audiometric tests for each frequency (PTA according to the Chinese guidelines GB/T 7583 and GB/T 16403). In our study, PTA mainly consisted of air conduction testing for each worker in the NKODS. If noise-exposed workers had abnormal hearing levels (BHFTA≥40 dB), bone conduction measurements were used to determine whether occupational hearing loss had occurred. To exclude age-related hearing loss, hearing threshold levels were adjusted for age. According to the national standard, GB/T 7582–2004, the values for different age groups and frequencies, as shown in the Supplementary material Table 1, were subtracted from the measured hearing threshold value, yielding the age-adjusted hearing threshold value.
HFHL level categories were determined. Based on the Chinese national standard, Diagnosis of Occupational NIHL (GBZ 49–2014), and national guidelines, Risk Management of Occupational Noise Hazard (AQ/T 4276–2016), HFHL was defined as a BHFTA greater than or equal to 40 dB at 3,4, and 6 kHz. The categories of HFHL are shown in Table 1.
Research subjects
In this study, the inclusion criteria were as follows:
-
the subjects had complete NKODS data and health examination reports from 2014 to 2017;
-
the subjects were continuously exposed to noise in the workplace and were only exposed to noise;
-
the NED was > 1 year;
-
the subjects were older than 18 years old and younger than 50 years old.
The exclusion criteria were as follows:
-
a family history of ear trauma or middle/external ear disease;
-
a history of toxic drug and chemical exposure (such as organic solvents and carbon monoxide).
A total of 47,739 subjects were exposed to occupational noise in Sichuan, China. According to the inclusion and exclusion criteria, 32,121 eligible subjects were enrolled in the study. All subjects were randomly divided into five datasets; 80% of the subjects were included as the training cohort, and 20% were included as the external validation cohort. The study flowchart is shown in Fig. 1.
Data analysis
The characteristics of the training and validation cohorts are described by the frequency and percentage. Categorical variables are expressed as frequencies (%) and were compared by chi-square tests among all subjects.
Binary logistic regression analyses were used to identify the independent predictors of HFHL among the variables of sex, age, NED, industry type and enterprise type. HFHL was processed as a binary outcome in the model, where “0” indicated a BHFTA < 40 dB and “1” indicated a BHFTA ≥40 dB. The risks are expressed as odds ratios (ORs) and 95% confidence intervals (CIs).
A nomogram was established based on the risk model. The receiver operating characteristic (ROC) curve was used to examine the effectiveness of the risk model. The C-index was expressed by the area under the curve (AUC), which reflected the ability of the model to discriminate between those who would suffer HFHL from those who would not. Calibration plots were used to assess the nomogram’s calibration, which refers to how close the risk predicted by the nomogram is to the risk actually observed. To ensure the applicability of the nomogram in clinical practice, the cut-off value corresponding to the maximum Youden’s index was used to stratify HFHL workers into high and low risk groups. A two-tailed P-value< 0.05 was considered statistically significant. All statistical calculations were performed using R statistical software (version 3.5.0).
Results
Subject characteristics and the prevalence of HFHL
Of the 32,121 workers in the study, 73.66% (n = 23,661) were male and 26.34% (n = 8460) were female. The average age of the subjects was 38.41 years (SD = 7.98 years). Workers exposed to noise had a mean exposure duration of 8.63 years (SD = 7.86 years). The demographic and occupational characteristics of the subjects are summarized in Table 2.
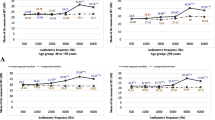
Among the 32,121 noise-exposed workers in this study, the lowest BHFTA was 0 dB, and the highest was 115 dB. Concerning the prevalence of hearing levels, 62.12% (n = 19,952) of the workers had a normal hearing level (BHFTA≤25 dB), 27.82% (n = 8937) of the workers had a BHFTA 26–39 dB, 9.78% (n = 3141) of the workers had a BHFTA 40–79 dB, and 0.28% (n = 91) of the workers had a BHFTA≥80 dB. The distribution of the BHFTA was expressed according to the approximately normal distribution of all parameters (Fig. 2).
Different characteristics of the BHFTA in all subjects
Table 3 shows that the prevalence of HFHL increased stepwise according to age and NED (P < 0.05). Workers employed in manufacturing industries and mining industries were more likely to have HFHL than workers employed in construction and other industries (P < 0.05). In addition, those in POE had a significantly higher BHFTA than those in SOE and FOE (P < 0.05).
The proportion of HFHL in the training and validation cohorts
The characteristics of the training cohort and validation cohort associated with the incidence of HFHL are shown in Table 4. The differences in the characteristics of the two cohorts with respect to the incidence of HFHL were all significant (chi-square test, all P < 0.01).
Risk model and HFHL nomogram
Five variables were included in the final risk model (Table 5). Growth of age, (OR = 1.09, 95% CI: 1.083–1.104), male sex (OR = 3.25, 95% CI: 2.855–3.702), increase in NED (OR = 1.15, 95% CI: 1.093–1.201), and working in manufacturing (OR = 1.50, 95% CI: 1.314–1.713), construction (OR = 2.29, 95% CI: 1.531–3.421), mining (OR = 2.63, 95% CI: 2.238–3.081), or for a POE (OR = 1.33, 95% CI: 1.202–1.476) were associated with an increased risk of HFHL (all P < 0.05). Based on the final risk model, the nomogram was established, which included the five identified variables, to identify the risk probability of HFHL (Fig. 3).
Nomogram for predicting the probability of HFHL in noise-exposed workers. Abbreviations. FOE = foreign-owned enterprise, SOE = state-owned enterprise, POE = private-owned enterprise. Footnote. The sixth row (points) indicates the points that are assigned to each variable’s measurement from rows 1–5, which are the variables that are included in the risk model. The assigned points for all variables are then summed, and the total value is shown as the total score. Once the total score is located, draw a vertical line down to the bottom line to obtain the predicted probability for HFHL
The AUC of the ROC curve in the two cohorts is shown in Fig. 4. In the training cohort, the final risk model had good discrimination, as demonstrated by an AUC of the ROC curve of 0.713 (95% CI: 0.704–0.722). In the validation cohort, the model continued to have the excellent discriminatory ability (AUC = 0.714, 95% CI: 0.695–0.733).
Figure 5 demonstrates the calibration curves of the risk model in the training cohort and validation cohort. The calibration plots of the models are shown for the two cohorts, which each have a certain degree of deviation. For the validation cohort, the model showed good predictions throughout the range of predicted risks and was accurate through a range of predicted probabilities of 15% to approximately 30% risk of HFHL. The average deviation was 2.0%, with a positive probability less than the predicted probabilities of 30%, while the average deviation was 7.0% with a positive probability greater than 30%.
To ensure the practical applicability of the model, the cut-off point of 9.6% was established based on the maximum Youden’s index and was used to stratify patients into high- and low-risk groups. The sensitivity at the cut-off point was 0.73 and the specificity at the cut-off point was 0.60.
Discussion
Most research has supported that long-term noise exposure in workers is likely to cause HFHL [35]. In this study, we identified the risk factors for HFHL and also developed a HFHL nomogram for noise-exposed workers.
In our study, 10.06% (3232/32121) of the workers had HFHL. The prevalence of HFHL in Sichuan is higher than that in China. The prevalence is higher than that in Ordos (5.5%), Wuhan (7.3%), Jining (4.6%), and Tianjin (8.3%) [36,37,38,39], and lower than that in Zhoushan (22.02%) and Sanmenxia (12.0%) [40, 41]. Occupational hearing loss has historically been difficult to compare because the criteria for HFHL among workers vary from country to country [42].
In our risk model, the results indicated that males (OR = 3.25) experience more effects after exposure to occupational noise than females. The reason may be due to males usually having greater exposure to noise at work than females due to differences in occupational categories and lifetime work history. Several animal and human studies have demonstrated that women may be protected against hearing loss because of oestrogen and its signalling pathways [43, 44]. Age (OR = 1.09) and NED (OR = 1.15) have a negative effect on HFHL, and research has showed that age and NED are important factors for changes in the hearing threshold. Our study strongly supports these results [45,46,47].
Interestingly, our risk model showed that age and NED had independent effects on HFHL when the BHFTA was adjusted for age. There could be two explanations for this result: first, the study sample is predominantly comprised of male workers, and studies have shown that male workers are generally more vulnerable to occupational hearing loss than female workers [48]. There was a greater proportion of females was used to control for age, which may have accounted for some of the effects. Second, in the risk model, the variable age may represent occupational hearing loss due to other exposures and not the influence of age on HFHL over time, given that the exposure duration is related to age. Exposures to other factors such as ototoxic chemicals in the workplace may not be detected by occupational environmental monitoring. Chemicals alone or combined with noise have recently become a concern as a cause of occupational hearing loss [49]. In the NKODS-Sichuan, noise-exposed workers were usually asked whether they were exposed to toxic chemicals in the workplace, but in general, workers often do not know or remember which chemicals they have encountered. In addition, toxic chemicals may have greater effects with longer exposure durations or in older workers. This may also explain why age and NED had independent effects on HFHL when age was adjusted for in this study. It is difficult to detect toxic chemical exposure in such nationwide screenings for NIHL among noise-exposed workers. However, toxic chemical effects on occupational hearing loss still should be considered in the future [50].
The risk model showed that the mining industry (OR = 2.63) has a strong negative effect on HFHL, with a higher positive rate of HFHL than the other industry types in both the validation cohort and training cohort. Our results suggest that mining workers should have more hearing protective measures and receive more attention from managers. In Poland, according to a report by the Central Statistical Office, the number of workers who exceeded the noise level (85 dB) was approximately 200 thousand, with the highest numbers in industries related to mining, metal and metal product production, textiles and wood production [51]. The mining of minerals necessitates the use of heavy energy-intensive types of machinery and equipment, leading miners to be exposed to high noise levels [52]. Based on the risk model and nomogram, workers who are employed in POE are more likely to experience HFHL than those in other enterprise types. Private enterprises are mostly small-sized enterprises, which are limited by less investment in occupational disease prevention, a lack of occupational health management, and no personal protective equipment. Moreover, the level of noise exposure for those in POE is more serious than those in SOE and FOE, and POE should be regarded as a key enterprise that is in need of prevention and management strategies for HFHL. In addition, the supervision department should pay more attention to the use of hearing protection by noise-exposed workers in POE [53, 54].
We also developed a HFHL nomogram based on the risk model. In the training cohort, the final risk model had good discrimination, as demonstrated by an AUC of the ROC curve of 0.713 (95% CI: 0.704–0.722), and the model continued to have excellent discriminatory ability in the validation cohort (AUC = 0.714, 95% CI: 0.695–0.733). Our nomogram was successfully subjected to independent external validation, which revealed good calibration and better discrimination in the validation cohort than in the training cohort. The results indicate that the risk model and nomogram for HFHL can be an effective tool to assess noise-exposed workers’ risk for HFHL. Moreover, due to its easy-to-use and the visualization features, noise-exposed workers can use the tool on a daily basis. Furthermore, the maximum Youden’s index revealed that noise-exposed workers have a risk probability of HFHL greater than 9.6%. Administrative staff should pay more attention to providing hearing protection for or transferring the position of noise-exposed workers. Regarding further research on the HFHL nomogram, researchers can focus on: (1) comparing other assessment tools with the HFHL nomogram in different occupation-specific populations and (2) the risk probability of HFHL could be considered a new variable in further studies on occupational hearing loss.
This study still has two limitations. (1) Generally, the direct predictor of HL is noise cumulative exposure (NCE), but the NKODS did not collect the NCE levels of the participants. If data on area noise monitoring instead of the NCE levels were included in the model, differences in the results may have been observed. Therefore, we used the NED to represent the level of noise exposure. (2) Exposure to toxic drugs and chemicals was self-reported by the workers in the NKODS. Workers may be unaware of toxic drugs that they have taken or toxic chemicals that may be present in their work environment, which may have affected our results.
Conclusions
In this study, 10.06% (n = 3232) of the workers had HFHL. In the training cohort, we identified that the risk predictors for HFHL were male sex, growth of age, increase in NED, and employment in the manufacturing industry, construction industry, mining industry, or for a POE. Based on the risk model, a nomogram was developed to predict the individualized risk for HFHL among noise-exposed workers. We believe that risk model and nomogram can be used to enhance application-oriented research on HFHL and will support the development of management strategies to prevent occupational hearing loss.
Availability of data and materials
The all of the research materials are in the manuscript and request of materials should contact with the corresponding author (e-mail: yajialan501@126.com).
Abbreviations
- WHO:
-
World health organization
- NHFPC:
-
National health and family planning commission
- OENTD:
-
Occupational ear, nose and throat diseases
- HFHL:
-
High-frequency hearing loss
- NIHL:
-
Noise-induced hearing loss
- GPD:
-
Gross domestic product
- FYP:
-
Five-year plan
- NKODS:
-
National key occupational disease survey
- CDC:
-
Centers for disease control and prevention
- PTA:
-
Pure tone audiogram
- BHFTA:
-
Binaural high-frequency threshold average
- NED:
-
Noise exposure duration
- FOE:
-
Foreign-owned enterprise
- SOE:
-
State-owned enterprise
- POE:
-
Private-owned enterprise
- OR:
-
Odds ratio
- SE:
-
Standard error
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
References
Seixas NS, Neitzel R, Stover B, Sheppard L, Feeney P, Mills D, et al. 10-year prospective study of noise exposure and hearing damage among construction workers. Occup Environ Med. 2012;69(9):643–50. https://doi.org/10.1136/oemed-2011-100578.
World Health Organization. Prevention of blindness and deafness and grades of hearing impairment. 2019. Available from: URL: http://www.who.int/en/news-room/fact-sheets/detail/deafness-and-hearing-loss
World Health Organization. Prevention of blindness and deafness. 2018. Available from: URL: http://www.who.int/pbd/deafness/estimates/en/
Rowley C. Development in China: position and nationhood in Asia and the world. Asia Pac Bus Rev. 2012;18(1):87–92. https://doi.org/10.1080/13602381.2011.591653.
Fuente A, Hickson L. Noise-induced hearing loss in Asia. Int J Audiol. 2011;50(Suppl 1):S3–S10. https://doi.org/10.3109/14992027.2010.540584.
Lu YQ, Liu JW. Current situation of occupational health in China. Occup and Health. 2019;35(10):1437–40 (in Chinese).
National health commission of the PRC, Statistical Bulletin on the development of health care in China. 2015. Available from: URL: http://www.zywsw.com/news/6331.html (in Chinese).
National health commission of the PRC, Statistical Bulletin on the development of health care in China. 2016. Available from: URL: http://www.nhc.gov.cn/zyjks/zcwj2/201712/90667a5571e44ccca42e317b68f50c40.shtml (in Chinese).
National health commission of the PRC, Statistical Bulletin on the development of health care in China. 2017. Available from: URL: http://www.nhc.gov.cn/guihuaxxs/s10743/201806/44e3cdfe11fa4c7f928c879d435b6a18.shtml (in Chinese).
National health commission of the PRC, Statistical Bulletin on the development of health care in China. 2018. Available from: URL: http://www.nhc.gov.cn/guihuaxxs/s10748/201905/9b8d52727cf346049de8acce25ffcbd0.shtml (in Chinese).
National health commission of the PRC. Statistical Bulletin on the development of health care in China. 2019. Available from: URL: http://www.nhc.gov.cn/guihuaxxs/s10748/202006/ebfe31f24cc145b198dd730603ec4442.shtml (in Chinese).
Vlaming MSMG, Mackinnon RC, Jansen M, Moore DR. Automated screening for high-frequency hearing loss. Ear Hear. 2014;35(6):667–79. https://doi.org/10.1097/AUD.0000000000000073.
Wang XM, Qin WD, In Q, Wang YF. Investigation on occupational high frequency hearing loss in fuling district of Chongqing city in 2019. Occup Health Damage. 2021;36(01):5–11.
Lawson SM, Masterson EA, Azman AS. Prevalence of hearing loss among noise-exposed workers within the mining and oil and gas extraction sectors, 2006-2015. Am J Ind Med. 2019;62(10):826–37. https://doi.org/10.1002/ajim.23031.
Nyarubeli IP, Tungu AM, Moen BE, Bråtveit M. Prevalence of noise-induced hearing loss among tanzanian iron and steel workers: a cross-sectional study. Int J Environ Res Public Health. 2019;16(8):1367. https://doi.org/10.3390/ijerph16081367.
Masterson EA, Themann CL, Calvert GM. Prevalence of hearing loss among noise-exposed workers within the health care and social assistance sector, 2003 to 2012. J Occup Environ Med. 2018;60(4):350–6. https://doi.org/10.1097/JOM.0000000000001214.
Wang Q, Wang X, Yang L, Han K, Huang Z, Wu H. Sex differences in noise-induced hearing loss: a cross-sectional study in China. Biol Sex Differ. 2021;12(1):24. https://doi.org/10.1186/s13293-021-00369-0.
Gan WQ, Moline J, Kim H, Mannino DM. Exposure to loud noise, bilateral high-frequency hearing loss and coronary heart disease. Occup Environ Med. 2016;73(1):34–41. https://doi.org/10.1136/oemed-2014-102778.
Chang TY, Liu CS, Huang KH, Chen RY, Lai JS, Bao BY. High-frequency hearing loss, occupational noise exposure and hypertension: a cross-sectional study in male workers. Environ Health. 2011;10(1):35. https://doi.org/10.1186/1476-069X-10-35.
Chen S, Ni Y, Zhang L, Kong L, Lu L, Yang Z, et al. Noise exposure in occupational setting associated with elevated blood pressure in China. BMC Public Health. 2017;17(1):107. https://doi.org/10.1186/s12889-017-4050-0.
Jayakody DMP, Almeida OP, Speelman CP, Bennett RJ, Moyle TC, Yiannos JM, et al. Association between speech and high-frequency hearing loss and depression, anxiety and stress in older adults. Maturitas. 2018;110:86–91. https://doi.org/10.1016/j.maturitas.2018.02.002.
Xie QY, Chu YM, Hu XC. Anxiety and influencing factors of laborers with high frequency hearing loss. J Environ Occup Med. 2015;32(02):140–2. https://doi.org/10.13213/j.cnki.jeom.2015.14159.
Blazer DG, Tucci DL. Hearing loss and psychiatric disorders: a review. Psychol Med. 2019;49(6):891–7. https://doi.org/10.1017/S0033291718003409.
Lewkowski K, Heyworth J, McCausland K, Fritschi L, Williams W, Li I. Predictors of noise exposure in construction workers. In Proc Acoust AUS. 2017:19–22.
Kuronen P, Toppila E, Starck J, Pa¨a¨kko¨nen R, Sorri MJ. Modelling the risk of noise-induced hearing loss among military pilots. Int J Audiol. 2004;43(2):79–84. https://doi.org/10.1080/14992020400050013.
Hong H, Dowdy DW, Dooley KE, Francis HW, Budhathoki C, Han HR, et al. Aminoglycoside-induced hearing loss among patients being treated for drug-resistant tuberculosis in South Africa: a prediction model. Clin Infect Dis. 2020;70(5):917–24. https://doi.org/10.1093/cid/ciz289.
Kuang D, Tu C, Yu YY, Wang L, Gao Y, Yang Y, et al. Establishment of a nomogram for predicting the high frequency hearing loss of workers exposed to noise. Chin J Industrial Hyg Occup Dis. 2018;36(7):523–6. https://doi.org/10.3760/cma.j.issn.1001-9391.2018.07.012 (in Chinese).
Ai JY, Feng XD, Liu JQ, Wang YJ. Status of high frequency hearing loss of noise-exposed workers in private enterprises of Tangshan City in 2017. Occup and Health. 2019;35(18) :2465-2468. https://doi.org/10.13329/j.cnki.zyyjk.2019.0660 (in Chinese).
Jalali A, Alvarez-Iglesias A, Roshan D, Newell J. Visualising statistical models using dynamic nomograms. PLoS One. 2019;14(11):e0225253. https://doi.org/10.1371/journal.pone.0225253.
Hyun AJ, Zoo LJ, Kee CM, et al. Nomogram for prediction of prostate Cancer with serum prostate specific antigen less than 10 ng/mL. J Korean Med Sci. 2014;29(3):338–42. https://doi.org/10.3346/jkms.2014.29.3.338.
Houvenaeghel G, Bannier M, Nos C, Giard S, Mignotte H, Jacquemier J, et al. Non sentinel node involvement prediction for sentinel node micrometastases in breast cancer: nomogram validation and comparison with other models. Breast. 2012;21(2):204–9. https://doi.org/10.1016/j.breast.2011.09.013.
Lewkowski K, McCausland K, Heyworth JS, Li IW, Williams W, Fritschi L. Questionnaire-based algorithm for assessing occupational noise exposure of construction workers. Occup Environ Med. 2018;75(3):237242. https://doi.org/10.1136/oemed-2017-104381.
Aliabadi M, Farhadian M, Darvishi E. Prediction of hearing loss among the noise-exposed workers in a steel factory using artificial intelligence approach. Int Arch Occup Environ Health. 2015;88(6):779–87. https://doi.org/10.1007/s00420-014-1004-z.
Zhu XJ, Li T, Wang D. Analysis on current situation in key occupational disease monitoring and countermeasures to problems. Chinses J Ind Med. 2016;29(06):403–7. https://doi.org/10.13631/j.cnki.zggyyx.2016.06.001 (in Chinese).
Abujamra AL, Escosteguy JR, Dall'Igna C, Manica D. Lauro José Gregianin. The use of high-frequency audiometry increases the diagnosis of asymptomatic hearing loss in pediatric patients treated with cisplatin-based chemotherapy. Pediatr Blood Cancer. 2013;60(3):474–8. https://doi.org/10.1002/pbc.24236.
Yu XH, Li XY, Zhao XD. Noise inspection results of major occupational disease surveillance in Ordos City in 2018. Occup Health. 2020;36(06):855–7. https://doi.org/10.13329/j.cnki.zyyjk.2020.0228 (in Chinese).
Qiao JJ, Chen ZL, Mao GS. Occupational noise deafness monitoring of Wuhan, 2017. Modern Prev Med. 2018;45(23):4254–8 (in Chinese).
Zhang XM. Monitoring of major occupational diseases and analysis of occupational group's health status of Jining in 2018. Chin J Industrial Hyg Occup Dis. 2020;38(01):41–4 (in Chinese).
Liu J, Li ML, Wang X, Zhang M, Zeng Q. Analysis of occupational noise deafness monitoring in Tianjin in 2016. J Modern Prev Med. 2017;44(23):4252–5.
Gao ML, Zhang YL, Yi JP. Analysis of influencing factors of high frequency hearing loss among noise workers in Zhoushan city. Prev Med. 2020;32(08):834–8. https://doi.org/10.19485/j.cnki.issn2096-5087.2020.08.019.
Fu CC, Liang N. High frequency hearing monitoring results of noise-exposed workers in Sanmenxia City in 2018. Occup Health. 2019;35(21):2888–90. https://doi.org/10.13329/j.cnki.zyyjk.2019.0736.
Rabinowitz PM. The public health significance of noise-induced hearing loss. New York: Noise-Induced Hearing Loss Springer; 2012. https://doi.org/10.1007/978-1-4419-9523-0_2.
Nelson DI, Nelson RY, Concha-Barrientos M, Fingerhut M. The global burden of occupational noise-induced hearing loss. Am J Ind Med. 2005;48(6):446–58. https://doi.org/10.1002/ajim.20223.
Shuste BZ, Depireux DA, Mong JA, Hertzano R. Sex differences in hearing: probing the role of estrogen signaling. J Acoust Soc Am. 2019;145(6):3656–63. https://doi.org/10.1121/1.5111870.
Zhang H, Zhu X, Guo R, Li D, Li L. Study on hearing impairment at high frequency among the flight cadets. J Clin Otorhinolaryngol Head Neck Surg. 2014;28(13):968–71. https://doi.org/10.13201/j.issn.1001-1781.2014.13.014.
Cruickshanks KJ, Nondahl DM, Tweed TS, Wiley TL, Klein BEK, Klein R, et al. Education, occupation, noise exposure history and the 10-yr cumulative incidence of hearing impairment in older adults. Hear Res. 2010;264(1–2):3–9. https://doi.org/10.1016/j.heares.2009.10.008.
Kortlang S, Mauermann M, Ewert SD. Suprathreshold auditory processing deficits in noise: effects of hearing loss and age. Hear Res. 2016;331:27–40. https://doi.org/10.1016/j.heares.2015.10.004.
Ciorba A, Benatti A, Bianchini C, Aimoni C, Martini A. High frequency hearing loss in the elderly: effect of age and noise exposure in an italian group. J Laryngol Otol. 2011;125(8):776–80. https://doi.org/10.1017/S0022215111001101.
Lewkowski K, Heyworth JS, Li IW, Williams W, McCausland K, Gray C, et al. Exposure to noise and ototoxic chemicals in the Australian workforce. Occup Environ Med. 2019;76(5):341–8. https://doi.org/10.1136/oemed-2018-105471.
Yang HY, Shie RH, Chen PC. Hearing loss in workers exposed to epoxy adhesives and noise: a cross-sectional study. BMJ Open. 2016;6(2):e010533. https://doi.org/10.1136/bmjopen-2015-010533.
Wiesław S, Owczarek K, Olszewski J. Contemporary noise-induced hearing loss (NIHL) prevention. Otolaryngol Pol. 2017;71(4):1–7. https://doi.org/10.5604/01.3001.0010.2241.
Tripathy DP, Nanda SK. Noise identification, modeling, and control in mining industry. J Acoust Soc Am. 2015;137(4):2377. https://doi.org/10.1121/1.4920637.
Wang YL, Li MY. Occupational health examination and influencing factor analysis of noise workers in Shengzhou city from 2015 to 2017. Chin J Public Health Management. 2018;34(5):715–20 (in Chinese).
Zhang HS, Liu XY, liao J, et al. Analysis on monitoring results of occupational hazard factors in key enterprises in Guangming New District of Shenzhen, 2011–2013. Chin Occup Med. 2015;42(1):106–108+112 (in Chinese).
Acknowledgements
The authors are grateful to the staff of Sichuan CDC and occupational health examination institutions, and grateful to the data managers of the national key occupational diseases survey.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Study design, data analysis, data interpretation and finished the manuscript: RCS. Data acquisition: WWS. Data analysis: RCS, YQC. Study design and supervision of study: YJL. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Before the audiometric testing and medical examination, all the participants had read the informed consent form. Written consents were received from all participants, and this study was approved by the Ethics Committees of West China School of Public Health and West China Fourth Hospital (No.HXSY-EC-2020090). The study was performed in accordance with the ethical standards of the Declaration of Helsinki.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, R., Shang, W., Cao, Y. et al. A risk model and nomogram for high-frequency hearing loss in noise-exposed workers. BMC Public Health 21, 747 (2021). https://doi.org/10.1186/s12889-021-10730-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-021-10730-y