Abstract
Background
Factory workers in low- and middle-income countries (LMICs) are vulnerable to HIV transmission. Interventions are needed to prevent HIV in this population. We systematically reviewed published literature on the efficacy of various HIV interventions in reducing stigma, risk behaviors and HIV transmission among factory workers.
Methods
A systematic review was performed using predefined inclusion and exclusion criteria. Four databases (PubMed, PsycINFO, Scopus and EMBASE) were searched for relevant publications between January 1, 1990 and December 31, 2018. Two independent reviewers assessed the methodological quality of studies.
Results
Thirteen articles were included, with 2 randomized controlled trials and 11 cohort studies. Five interventions and their combinations were summarized. Educational intervention increased condom use and reduced the use of recreational drugs and alcohol before sex. Community intervention that proactively provide HIV counselling and testing (HCT) services could increase the detection rate of HIV and other sexually transmitted diseases (STDs). Lottery intervention increased HCT uptake and decreased HIV public stigma. Education combined with community intervention reduced the proportion of workers with casual sex and enhanced HIV knowledge. Peer education combined with community intervention increased the proportion of workers who were willing to take their partners to HCT. Policy intervention combined with peer education enhanced HIV knowledge, perceived condom accessibility and condom use with regular partners.
Conclusions
Various interventions improved HIV knowledge, decreased HIV stigma and reduced HIV-related risk behaviors among factory workers in LMICs. The combination of multiple interventions tended to achieve better efficacy than a single intervention. Persistent combination interventions are essential to address HIV in this population.
Similar content being viewed by others
Background
Human immunodeficiency virus (HIV) infection is a major public health challenge and a major disease burden in low- and middle-income countries (LMICs) [1]. According to the United Nations Program on HIV/AIDS (UNAIDS) in 2016, about 36.7 million people in the world were living with HIV/AIDS, 95% of whom were from LMICs [2]. Existing studies have shown that demographic characteristics which were associated with increased risk of HIV infection included low level of education [3], unprotected sex [4], and labor-intensive enterprise workers including factory workers [5, 6].
Factory workers are especially vulnerable to HIV. A cohort study in Ethiopia showed that 8.5% of workers in factories were infected with HIV, with an incidence of 0.4 per 100 person-years [7]. According to study published in 2019, Lesotho national textile factory workers had higher HIV prevalence than other adults in the country (42.7% vs 25%, P < 0.05) [6]. A cross-sectional study in 2016 in China also found that factory workers were more likely to be HIV positive than students in the screening of blood donors (0.1% vs 0.03%, P < 0.01) [8]. Various factors influence the susceptibility of factory workers to HIV. The first reason is that this group are sexually active and had insufficient education. According to the literature [7, 9], more than 63% of factory workers were under the age of 35 and more than 44% had less than junior high school education. The second reason is the high prevalence of high-risk sexual behaviors. Available data showed that over 40% of factory workers had two or more sex partners in the past 12 months [7, 9, 10]. Approximately 20% of factory workers had sex with non-regular partners in the last 6 months, with whom 66.3% used alcohol before sex [10]. Studies showed that drinking alcohol before sex increased the risk of HIV infection [11, 12]. Finally, just over 40% of this population would like to accept HIV counselling and testing (HCT) when this service is available [13]. HIV-related stigma may prevent them from accepting HCT.
In LMICs, health education and behavioral interventions have been playing an essential role in the control of HIV. A randomized controlled trial (RCT) in Lithuania showed that health education has a significant impact on improving HIV knowledge and reducing HIV infection risk behaviors, but has little effect on attitude change [14]. However, another intervention-peer education, not only improved HIV knowledge and changed HIV attitude, but improved HCT uptake [15, 16]. Recently, an RCT in Zimbabwe demonstrated that providing financial incentive could also significantly improve HCT uptake [17]. These useful interventions, including educational intervention, peer education, and financial incentives, could produce beneficial outcomes among factory workers [18,19,20]. However, to our knowledge, there was no published review that summarizes and compares the efficacy of these interventions among factory workers. We performed a systematic review to evaluate various interventions reported in published articles involving factory workers in LMICs in reducing HIV infection, changing HIV risk behaviors and attitudes, and decreasing HIV stigma.
Methods
This systematic review followed the guidelines set forth in the 2010 ‘Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)’ [21]. In addition, we developed a protocol, but it was not registered or published (see Additional file 1).
Search strategy
In this paper, studies about factories (also known as manufacturing plants) or people working in factories were included. The Mesh terms “workplace/industry/acquired immunodeficiency syndrome” and the key word “worker” were combined using the Boolean operator and with the following key words: (enterprise, firm, company, workshop, floor shop, machine shop, mill, factory, manufactory) and (worker, workman, workingman, employee). Key words in parentheses were connected to operators. The search strategy was implemented in the databases PubMed, PsycINFO, Scopus and EMBASE using a date range of January 1, 1990 through December 31, 2018. Grey literature online (e.g., AIDS Conference, International AIDS Society Conference), was also searched, but no relevant articles were found. Details of the search strategies are presented in Additional file 2: Table S1.
Two authors of this study (DC and GL) each independently searched for relevant articles. Titles, abstracts, full texts and reference lists of all identified reports were reviewed in duplicate by the two authors, and extracted articles were double-checked. Disagreements were resolved by discussion among the three authors (DC, GL and HZ). Reference lists from related main studies and review articles were also checked for additional relevant reports.
Eligibility criteria
The inclusion criteria were: (1) The scope was formulated using the population, intervention, comparison, outcomes, and study design (PICOS) [22, 23] format, which are listed in Table 1; (2) Studies were conducted in LMICs according to the World Bank (the World Bank classifies countries by income. Countries can be categorized into LMICs and High-Income Countries (HICs). The LMIC status of a country where an included study was conducted was judged according to the World Bank classification of country by income in 2017, the most up-to-date data when we conducted our review) [24]; (3) Studies report on a specific intervention time span; (4) Articles were written in English. In order to ensure that we were not overlooking relevant studies, we had no restrictions on intervention methods.
Studies were excluded based on the following criteria: (1) Participants were not factory workers; (2) No intervention; (3) Article published before 1990; (4) Studies were observational, and did not describe an intervention’s efficacy on reducing HIV infection, changing HIV risk behaviors and attitudes, and decreasing HIV stigma (e.g., a cross-sectional study); (5) Systematic review, literature review, case series; (6) Article published in languages other than English.
Data extraction and statistical analysis
The following data were extracted from publications: year of publication, first author, country in which the study took place, study design, sample size, length of follow-up, intervention method, and intervention outcomes. In addition, for studies that did not provide a χ2 value, we calculated the χ2 value using R version 3.6.0, including P value, if the necessary figures were provided in the paper.
Quality assessment of included studies
In order to assess the quality of the included articles, we used the Quality Assessment Tool for Quantitative studies from the Effective Public Health Practice Project (EPHPP) [25, 26]. This tool has been widely used in literature to evaluate randomized control trials of HIV research [27, 28], and was recommended by the Cochrane Library in the area of Health Promotion and Public Health [29, 30]. Quality assessment included six components: selection bias, study design, confounders, blinding methods, data collection method, and withdrawals and drop-outs. The scores of each component are based on the documents [25, 26]. A study will receive a “strong” overall rating when none of the individual components has been rated as “weak”. If a study cannot get more than one “weak” score on any single component, it will receive a “medium” overall rating. A study of at least two “weak” ratings for individual components will be given a “weak” overall rating. Two authors (DC and GL) independently conducted quality assessment of included articles. If the quality evaluation results were different, the authors (DC and GL) would recheck the original article, and finally disagreements were resolved by discussion with the corresponding author (HZ)”.
Results
Overview of included studies
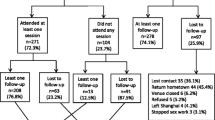
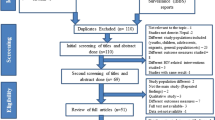
Figure 1 shows the procedure of study inclusion. We identified 4856 articles using the specified search criteria (PubMed: n = 732; EMBASE: n = 1612; Scopus: n = 2277; PsycINFO: n = 235). 940 duplicated papers were removed. Based on the inclusion criteria, 3867 papers were excluded. 49 papers remained for full text review, and 13 papers met inclusion criteria.
Table 2 provides details regarding the 13 studies included in the review. Studies included in our review were published between 1996 and 2018. All countries included in our review either remained as low/mid-income or progressed from low to mid-income, and none of these countries progressed to a higher income status, according to the World Bank [24]. Eight took place in Africa (three in Zimbabwe [19, 31, 32], two in South Africa [20, 33], two in Ethiopia [34, 35] and one in Tanzania [36]), while the remaining five were performed in Asia (three in Thailand [18, 37, 38] and two in China [39, 40]). Two were RCTs [31, 37] and eleven were cohort studies [18,19,20, 32,33,34,35,36, 38,39,40]. All studies reported a statistically significant effect on one or more outcomes, which were reported as follows: eight reported HIV risk behaviors [18, 34,35,36,37,38,39,40], four reported HIV/AIDS knowledge [18, 37, 38, 40], four reported HCT uptake [19, 20, 32, 33], one reported HIV public stigma [20], one reported HIV/AIDS attitude [18] and one reported HIV incidence [31]. Risk behaviors included presence of multiple sex partners, commercial sex, recreational drugs or alcohol use before sex, and condom use, etc. According to the UNAIDS [41], the definition of HIV public stigma was a process of devaluation of people either living with or associated with HIV infection, such as, those who blamed foreigners/migrant workers/prostitutes for spreading HIV/AIDS.
The types and definitions of HIV intervention among factory workers in LMICs are summarized in Table 3. Further details on the risk of bias are reported in Additional file 3: Table S2. In selection bias, seven articles [18, 20, 32, 37,38,39,40] were rated “strong” because those study participants were factory workers, and more than 80% of the selected individuals agreed to participate. Six articles [19, 31, 33,34,35,36] were rated “medium” because only 60–79% of the selected individuals agreed to participate. In study design, two studies [31, 37] were randomized controlled trials (RCTs), so they were rated “strong”, and eleven studies [18,19,20, 32,33,34,35,36, 38,39,40] were cohort studies, so they were rated “medium”. In confounders, two of the thirteen studies [35, 40] were rated as “strong”, five as “medium” [18, 34, 36, 38, 39] and the remaining six [19, 20, 31,32,33, 37] as “weak”. For two RCTs [31, 37], the authors did not report whether confounding factors were balanced at baseline, so they were rated “weak”. In blinding methods, twelve [18, 19, 31,32,33,34,35,36,37,38,39,40] were rated “medium” or “weak” because the evaluator or participant knew the task of the study group. In data collection methods, the research data in most studies [18, 20, 32,33,34,35,36,37,38,39,40] were obtained from the survey and proved to be effective, so they were rated as “strong”, but there were two studies [19, 31] that did not evaluate the quality of the acquisition method (such as validity and reliability), so they were rated as “weak”. Finally, withdrawals and drop-outs were not related to the six studies [20, 33,34,35, 38, 40], as they did not include subsequent evaluations. Overall, five cohort studies were assessed as strong quality [18, 34, 35, 39, 40], four as moderate quality [20, 32, 36, 38], and two as weak quality [19, 33]. Two RCTs only show that RCT method was used, but did not describe how to control mixing and how to achieve blind method, so their final evaluation results were weak [31, 37].
Efficacy of different intervention methods among factory workers
Educational intervention
Three studies focused on educational intervention [18, 37, 39]. Two studies indicated that educational intervention might improve condom use (condomless sex in the last 12 months decreased from 6.9% at baseline to 3.8% at month 12, P < 0.001; use of condom during sexual intercourse in the last 3 months increased from 41% at baseline to 70% at month 3, P < 0.05) [18, 39]. Two studies showed that educational intervention could improve HIV/AIDS knowledge [18, 37]. For example, workers who learned that antibiotics did not prevent HIV transmission increased from 46.9 to 56.3% (P = 0.03) and that mother-to-child could spread HIV increased from 82.6 to 93.4% (P < 0.05). One study showed that educational intervention could reduce the proportion of workers with extra-partners (from 16 to 5%, χ2 = 5.32, P = 0.021) [37]. One study showed that educational intervention could reduce the proportion of workers who used recreational drugs (from 2.6 to 0.7%, P < 0.01) or alcohol (from 17.0 to 6.3%, P < 0.01) before sex [18]. In addition, educational intervention changed HIV attitudes. For example, the proportion of workers who perceived that if they had HIV/AIDS they would not be able to live in society decreased from 46.6 to 30.6% (P < 0.05) [18].
Community intervention
One study conducted community intervention [32]. The study indicated that workers having high risk behaviors were more likely to take HCT, and proactive provision of HCT could increase the detection rate of HIV (relative risk [RR]: 1.87, 95% confidence interval [CI]: 1.01 to 3.61) and sexually transmitted diseases (STDs) (RR: 3.47, 95%CI: 2.51 to 4.89). Moreover, HIV seroconversion was higher among subjects who obtained their test results at the first follow-up visit compared to those who did not (19.5% vs. 16.7%, respectively, P = 0.01).
Combination of lottery intervention and community intervention
Two studies focused on lottery intervention combined with community intervention, both of which analyzed the changes in HCT uptake before and after the intervention [20, 33]. Moreover, these studies had demonstrated that lottery intervention could improve HCT uptake (from 30 to 85% (P < 0.001) [33] and from 27.3 to 53.6% (P < 0.001) [20]). In addition, lottery intervention could also reduce HIV public stigma. For example, the proportion of subjects who thought that foreigners/migrant workers/prostitutes were to blame for spreading HIV/AIDS decreased from 22.2 to 9.6% (P < 0.05) [20].
Combination of educational intervention and community intervention
Four studies conducted educational intervention combined with community intervention [34,35,36, 40]. Three studies demonstrated that educational intervention combined with community intervention reduced the proportion of workers with casual sex (from 12.0 to 6.1%, P = 0.03 [34]; from 17.5 to 3.5%, P < 0.001 [35]; from 8.8 to 4.6%, P < 0.01 [36]). Two studies showed a decrease in the proportion of workers having sex with sex workers [34, 35], but only one report [35] had statistically significant result (from 11.2 to 0.75%, P < 0.001 [35]). One study reported a decrease in the proportion of workers who had more than one sex partner. For example, the proportion of workers with two sexual partners decreased from 17 to 10% (P < 0.05) and with three or more sex partners decreased from 4.7 to 2.0% (P < 0.05) [36]. In addition, the combination of these two interventions increased condom use (from 7.6 to 27.3%, P = 0.002) [36], reduced premarital sex (10.9% in intervention group, 31.3% in control group, P < 0.001) [40], and improved HIV knowledge (P < 0.05) [40] and an increased awareness of the locations providing free health educational counselling (from 3.5 to 6.7%, P < 0.001) [40].
Combination of peer education and community intervention
Two studies focused on peer education combined with community intervention [19, 31]. One study indicated that peer education reduced incident HIV infection rate (1.51 vs. 2.52 per 100 persons-years, P < 0.05) [31]. Another study concluded that peer education rendered more workers to take their partners to HCT (odds ratio [OR] = 1.37, 95% CI: 1.04–1.79), but statistical significance was not found for individuals to take up HCT (OR = 1.05, 95% CI: 0.92–1.20) [19]. In addition, workers with STDs (OR = 2.78, 95%CI: 2.25–3.43), commercial sex (OR = 1.27, 95%CI:1.09–1.49) and multiple sex partners (OR = 1.31, 95%CI: 1.14–1.50) in the last 6 months were more likely to take up HCT [19].
Combination of policy intervention and educational intervention
One study conducted policy intervention combined with educational intervention [38]. This study indicated that combination of these intervention increased HIV/AIDS knowledge (t = 2.84, P = 0.005), perceived condom accessibility (OR = 2.80, 95% CI: 1.13–6.86, P < 0.05), and condom use with regular partners (OR = 1.25, 95% CI: 1.01–1.54, P < 0.05) at the last sex.
Discussion
Our systematic review identified five types of interventions that addressed low HIV/AIDS knowledge, high risk behaviors of HIV infections, high HIV stigma and low HCT uptake among factory workers in LMICs, namely educational intervention, peer education, community intervention, lottery intervention and policy intervention. Educational intervention and policy intervention had a significant effect on improving workers’ knowledge of HIV/AIDS and reducing HIV infection risk behaviors. Community intervention, peer education and lottery intervention were effective in reducing HIV public stigma and increasing HCT uptake.
In this review, most of intervention methods from the included studies were in combination. Among them, community intervention was combined with a variety of interventional methods. This intervention focused primarily on the socio-demographic characteristics and HIV serological status of the workers who underwent HCT [42]. Relevant studies showed that most people who attended HCT were at high risk of HIV infection [43]. Individuals infected with HIV were tested earlier than those who were not, and those who were in the early stages of HIV infection were tested earlier than those who were in the late stages [43]. This review also showed that community intervention demonstrated that the willingness of high-risk workers was likely to attend HCT when offered this opportunity. A recent cohort study in South Africa, demonstrated a similar outcome with a community intervention [44]. These findings suggested that offering HCT services to study subjects could potentially detect HIV infected individuals on a timely basis. In addition, the benefit of HCT could also be improved by active screening for STDs [45].
Although the efficacy of single community intervention was limited, it was significantly better when combined with different interventions. For example, community intervention combined with lottery intervention could improve HCT uptake and reduce HIV public stigma. This effect mainly came from lottery intervention. Lottery intervention encouraged workers to attend HCT by giving away free T-shirts, winning gifts and money and thus provided workers with an opportunity with a forum for open discussion [17, 46]. Social support and encouragement made these workers more willing to improve their HIV knowledge [47]. Social support could promote individual self-esteem and was a key factor in enabling the intervention to proceed smoothly and promote effectiveness [48, 49]. Research has shown that increasing social support and personal self-esteem could effectively reduce HIV stigma [49], which are essential for the UNAIDS to implement the three 90% [50] targets by 2030 (Three 90% prevention and treatment strategies of HIV: 90% of PLWH will know their infection status through testing, 90% of PLWH who have been diagnosed will have received antiviral therapy, and 90% of PLWH who have received antiviral therapy will be able to successfully suppress HIV).
Educational intervention was the most widely applied in HIV/AIDS interventions, and achieved a variety of effective results. Educational intervention had a significant effect on improving HIV/AIDS knowledge, changing HIV attitudes and reducing the proportion of workers with extra-partners, and could also change premarital and paid sexual behavior when combined with community intervention. A recent systematic review showed that educational intervention combined with community intervention could also change the public stigma of HIV [51]. In the future, more attention should be paid to HIV education combined with community intervention [52]. The combination effect of educational intervention and community intervention is better than a single intervention [53, 54]. Highly effective interventions, such as those that have an educational component, are imperative to undertake, but the cost of these designs - especially in LMIC - often limit their implementation even though they demonstrate high uptake of HCT and lower risky behaviors [54, 55]. Cost-effectiveness analysis provides information to help us balance the cost and efficacy when we implement educational intervention [54], so more research is needed to analyze the cost-effectiveness of an educational intervention.
Peer education combined with community intervention was also an effective intervention method, which could result in promoting workers to bring their partners to HCT and encouraging workers with high risk sexual behaviors to carry out HCT. According to recent research, peer education and community intervention not only improved HIV/AIDS knowledge, reduced HIV risk behaviors and incidence, but also increased HCT uptake in high-risk groups [56, 57]. Other relevant research showed that peer education could improve HIV knowledge, change HIV attitudes and reduce risky sexual behavior among adolescents, especially within peer groups [58, 59]. Peers are more likely to influence the behavior of fellow group members because they gain a level of trust that allows them to have more open discussions about sensitive topics [58, 59]. Therefore, in order to analyze whether peer education can achieve this same effect among factory workers, more research is needed.
This review summarized two special intervention methods, lottery intervention and policy intervention. These two interventions were based on incentives, and their purpose was to encourage workers to access HCT services. Policy intervention encourages workers to learn HIV/AIDS knowledge by issuing AIDS-response Standard Organization (ASO) certificates [60], while a lottery intervention encouraged workers to attend HCT by giving away free T-shirts, winning gifts and money and provided workers with an opportunity with a forum for open discussion [33]. Although this review summarized some benefits of these two interventions, only three relevant articles had been included. Further investigation and research are needed to explain their specific efficacy and causes.
In the 13 articles included, we did not find any research on interventions using multimedia or smart devices among factory workers. Reviews have shown that short message service (SMS) and interventions using mobile phone software can significantly improve HIV testing in high-risk groups [61, 62]. In addition, the use of multimedia or intelligent devices can effectively improve the uptake of intervention measures [61]. Therefore, for factory workers in LMICs - a group at high risk of HIV infection - It’s urgent to examine the efficacy of multimedia and smart devices-based interventions.
This study has several limitations. Firstly, it is impossible for us to judge which intervention brought about effect if multiple interventions were involved. With this in mind, more effort should be focused on single intervention or a combination of multiple interventions to compare the efficacy of various interventions in HIV high-risk groups. Secondly, articles included in our study did not analyze the cost-effectiveness and uptake of various methods, which is a key factor to the implementation of an intervention. Thirdly, since we only retrieved articles from four databases (PubMed, PsycINFO, Scopus and EMBASE), we might have missed some relevant articles from other sources (e.g., Google Scholar, EBSCOhost and WEB of Science). Finally, even if the indicators are the same, the methods of index measurement may differ such as the setting of HIV/AIDS knowledge and condom use measurement methods, which could contribute to detection bias.
Conclusions
This review indicated that various HIV interventions were efficacious in improving HIV knowledge and reducing HIV-related high-risk behaviors among factory workers in LMICs. The effectiveness of single intervention is limited and the combination of multiple interventions could achieve better outcomes. The efficacy of multimedia and smart devices-based interventions is warranted to be examined in the future.
Availability of data and materials
All data are provided in the tables, figure, and Additional files presented in the text. The other materials can be made available upon request.
Abbreviations
- HIV:
-
Human immunodeficiency virus
- LMICs:
-
Low- and middle-income countries
- HICs:
-
High-Income Countries
- AIDS:
-
Acquired immune deficiency syndrome
- UNAIDS:
-
United Nations Program on HIV/AIDS
- MSM:
-
Men who have sex with men
- HCT:
-
HIV counselling and testing
- RCT:
-
Randomized controlled trial
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PICOS:
-
Population, intervention, comparison, outcomes, and study design
- RR:
-
Relative risk
- CI:
-
Confidence interval
- STDs:
-
Sexually transmitted diseases
- OR:
-
Odds ratio
- SMS:
-
Short message service
- ASO:
-
AIDS-response Standard Organization
- EPHPP:
-
Effective Public Health Practice Project
References
Naghavi M, Abajobir AA, Abbafati C, Abbas KM, Abd-Allah F, Abera SF, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390:1151–210.
UNAIDS. Global AIDS Update 2016. 2016. https://www.unaids.org/en/resources/documents/2016/Global-AIDS-update-2016. Accessed 9 March 2019.
Zhang X, Yu J, Li M, Sun X, Han Q, Li M, et al. Prevalence and related risk behaviors of HIV, syphilis, and anal HPV infection among men who have sex with men from Beijing, China. AIDS Behav. 2013;17(3):1129–36.
Sentis A, Martin-Sanchez M, Arando M, Vall M, Barbera M, Ocana I, et al. Sexually transmitted infections in young people and factors associated with HIV coinfection: an observational study in a large city. BMJ Open. 2019;9(5):e027245.
Ibrahim SA, Sabitu K, Abubakar A, Poggensee G, Ibrahim S, Riyad M, et al. Demographic factors associated with HIV infection between low and high prevalence areas in Nigeria, 2015. Pan Afr Med J. 2019;32:11.
Mabathoana RS, Wyk CV, Adefuye AO. Factors influencing HIV risk-taking behaviours amongst textile factory workers living with HIV in Lesotho. Pan Afr Med J. 2019;33:166.
McFarland W, Gwanzura L, Bassett MT, Machekano R, Latif AS, Ley C, et al. Prevalence and incidence of herpes simplex virus type 2 infection among male Zimbabwean factory workers. J Infect Dis. 1999;180(5):1459–65.
Shi L, Liu Y, Wang J, Zeng P, Gao Z, Wang S, et al. HIV prevalence and incidence estimates among blood donors in five regions in China. Transfusion. 2020;60(1):117–25.
Li W, Jiang J, Su J, Liang B, Deng W, Huang J, et al. Commercial sexual behaviors among male rural-to-urban migrants in Western China: implications for HIV prevention. Asia Pac J Public Health. 2017;29(5):388–400.
Puri M. J Cleland. Sexual behavior and perceived risk of HIV/AIDS among young migrant factory workers in Nepal. J Adolesc Health. 2006;38(3):237–46.
Schneider M, Chersich M, Temmerman M, Degomme O, Parry C. The impact of alcohol on HIV prevention and treatment for South Africans in primary healthcare. Curationis. 2014;37(1):1137.
Rao N, Jeyaseelan L, Joy A, Kumar V, Thenmozhi M. S Achary. Factors associated with high-risk behaviour among migrants in the state of Maharashtra, India. J Biosoc Sci. 2013;45(5):627–41.
Sasaki Y, Arifin A, Ali M. K Kakimoto. Willingness to undergo HIV testing among factory workers in Surabaya, Indonesia. AIDS Care. 2011;23(10):1305–13.
Mockiene V, Suominen T, Valimaki M, Razbadauskas A. A Martinkenas. The impact of an education intervention to change nurses’HIV-related knowledge and attitudes in Lithuania: a randomized controlled trial. J Assoc Nurs AIDS Care. 2011;22(2):140–9.
Adeomi AA, Adeoye OA, Asekun EO, Abodunrin OL, Olugbenga AI. Evaluation of the Effectiveness of Peer Education in Improving HIV Knowledge, Attitude, and Sexual Behaviours among In-School Adolescents in Osun State, Nigeria. AIDS Res Treat. 2014;2014:131756.
Menna T, Ali A, Worku A. Effects of peer education intervention on HIV/AIDS related sexual behaviors of secondary school students in Addis Ababa, Ethiopia: a quasi-experimental study. Reprod Health. 2015;12:84.
Kranzer K, Simms V, Bandason T, Dauya E, McHugh G, Munyati S, et al. Economic incentives for HIV testing by adolescents in Zimbabwe: a randomised controlled trial. Lancet HIV. 2018;5(2):e79–86.
Sakondhavat C, Sittitrai W, Soontharapa S, Werawatanakul Y. P Pinitsoontorn. AIDS education and intervention trials among youths in factories: a pilot project. J Med Assoc Thail. 1998;81(11):872–8.
Machekano R, McFarland W, Hudes ES, Bassett MT. MT Mbizvo. Correlates of HIV test results seeking and utilization of partner counseling services in a cohort of male factory workers in Zimbabwe. AIDS Behav. 2000;4(1):63–7.
Weihs M, Meyer WA. WF Baasner. The influence of lotteries on employees' workplace HIV testing behaviour. Afr J AIDS Res. 2018;17(1):9–21.
Moher D, Liberati A, Tetzlaff J, Altman DG. P group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41.
O’Connor D, Green S, Higgins JP. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 (updated March 2011). In: London, UK: The Cochrane Collaboration Defining the review question and developing criteria for including studies; 2011. https://handbook-5-1.cochrane.org/chapter_5/5_defining_the_review_question_and_developing_criteria_for.htm. Accessed May 12, 2019.
Dissemination Centre for Reviews and. Systematic Reviews: CRD's Guidance for Undertaking Reviews in Health Care. 2009. https://www.york.ac.uk/media/crd/Systematic_Reviews.pdf. Accessed May 12, 2019.
Group World Bank. low- and middle-income countries in 2017. 2017. https://data.worldbank.org.cn/income-level/low-and-middle-income?view=chart. Accessed May 10, 2019.
EPHPP Project. Quality assessment tool for quantitative studies. 1998. https://merst.ca/ephpp/. Accessed May 10, 2019.
Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid-Based Nurs. 2004;1(3):176–84.
Genberg B, Shangani S, Sabatino K, Rachlis B, Wachira J, Braitstein P, et al. Improving engagement in the HIV care Cascade: a systematic review of interventions involving people living with HIV/AIDS as peers. AIDS Behav. 2016;20(10):2452–63.
Shangani S, Escudero D, Kirwa K, Harrison A, Marshall B. D Operario. Effectiveness of peer-led interventions to increase HIV testing among men who have sex with men: a systematic review and meta-analysis. AIDS Care. 2017;29(8):1003–13.
Jackson N. E Waters. Criteria for the systematic review of health promotion and public health interventions. Health promotion international. Health Promot Int. 2005;20(4):367–74.
Armstrong R, Waters E, N Jackson. Guidelines for systematic reviews of health promotion and public health interventions. Version 2 Australia: Melbourne University. 2007. http://ph.cochrane.org/sites/ph.cochrane.org/files/public/uploads/Guidelines%20HP_PH%20reviews.pdf. Accessed May 10, 2019.
Bassett MT. Impact of peer education on HIV infection in Zimbabwe. Sexual Health Exchange. 1998;4:14–5.
Machekano R, McFarland W, Mbizvo MT, Bassett MT, Katzenstein D, Latif AS. Impact of HIV counselling and testing on HIV seroconversion and reported STD incidence among male factory workers in Harare, Zimbabwe. Cent Afr J Med. 1998;44(4):98–102.
Weihs M, Meyer-Weitz A. A lottery incentive system to facilitate dialogue and social support for workplace HIV counselling and testing: a qualitative inquiry. J Soc Aspects HIV/AIDS Res Alliance. 2014;11:116–25.
Sahlu T, Wit TR, Tsegaye A, Mekonnen Y, Beyene A. B Hailu. Low incidence of syphilis among factory workers in Ethiopia: effect of an intervention based on education and counselling. Sex Transm Infect. 2002;78(2):123–6.
Mekonnen Y, Sanders E, Aklilu M, Tsegaye A, Wit TR, Schaap A, et al. Evidence of changes in sexual behaviours among male factory workers in Ethiopia. AIDS Behav. 2003;17(2):223–31.
Ng'weshemi JZ, Boerma JT, Pool R, Barongo L, Senkoro K, Maswe M. Changes in male sexual behaviour in response to the AIDS epidemic: evidence from a cohort study in urban Tanzania. AIDS. 1996;10(12):1415–20.
Kuchaisit C, Higginbotham N. An education intervention to increase the use of condoms for the prevention of HIV infection among male factory workers in Khon Kaen. J Clin Epidemiol. 1996;49:13.
Chamratrithirong A, Ford K, Punpuing S, Prasartkul P. A workplace intervention program and the increase in HIV knowledge, perceived accessibility and use of condoms among young factory workers in Thailand. J Soc Aspects HIV/AIDS Res Alliance. 2017;14(1):132–9.
Qian X, Smith H, Huang W, Zhang J, Huang Y, Garner P. Promoting contraceptive use among unmarried female migrants in one factory in Shanghai: a pilot workplace intervention. BMC Health Serv Res. 2007;7:77.
Zhu C, Geng Q, Chen L, Yang H, Jiang W. Impact of an educational programme on reproductive health among young migrant female workers in Shenzhen, China: an intervention study. Int J Behav Med. 2014;21(4):710–8.
UNAIDS. The Joint United Nations Programme on HIV and AIDS (UNAIDS): UNAIDS fact sheet on stigma and discrimination. 2003. https://link.springer.com/content/pdf/10.1007/978-3-319-46013-0_3.pdf. Accessed 9 March 2019.
Harichund C, Karim QA, Kunene P, Simelane S, Moshabela M. Exploring factors that influence the integration of HIVST with HCT using a qualitative comparative cross-over design in KwaZulu-Natal, South Africa. Global Public Health. 2019;14(9):1275–87.
VanderBorght SF, SchimvanderLoeff MF, Clevenbergh P, Kabarega JP, Kamo E, VanCranenburgh K, et al. Long-term voluntary counseling and testing (VCT) uptake dynamics in a multicountry HIV workplace program in sub-Saharan Africa. AIDS Care. 2010;22(2):195–205.
Mendelsohn AS, Gill K, Marcus R, Robbertze D, van de Venter C, Mendel E, et al. Sexual reproductive healthcare utilisation and HIV testing in an integrated adolescent youth Centre clinic in Cape Town, South Africa. South Afr J HIV Med. 2018;19:826.
Chen M, Scheer S, Nguyen T, Kohn R, Schwarcz S. HIV Co-infection among Persons Diagnosed with Sexually Transmitted Diseases, San Francisco, 2007 To 2014. Sex Transm Dis. 2018;45(8):563–72.
Choko AT, Corbett EL, Stallard N, Maheswaran H, Lepine A, Johnson CC, et al. HIV self-testing alone or with additional interventions, including financial incentives, and linkage to care or prevention among male partners of antenatal care clinic attendees in Malawi: an adaptive multi-arm, multi-stage cluster randomised trial. PLoS Med. 2019;16(1):e1002719.
Taylor BS, Fornos L, Tarbutton J, Munoz J, Saber JA, Bullock D, et al. Improving HIV care engagement in the south from the patient and provider perspective: the role of stigma, social support, and shared decision-making. AIDS Patient Care STDs. 2018;32(9):368–78.
Kalomo EN. Associations between HIV-related stigma, self-esteem, social support, and depressive symptoms in Namibia. Aging Ment Health. 2018;22(12):1570–6.
Yan H, Li X, Li J, Wang W, Yang Y, Yao X, et al. Association between perceived HIV stigma, social support, resilience, self-esteem, and depressive symptoms among HIV-positive men who have sex with men (MSM) in Nanjing, China. AIDS Care. 2019;31(9):1069–76.
Bain L, Nkoke C, Noubiap J. UNAIDS 90-90-90 targets to end the AIDS epidemic by 2020 are not realistic: comment on "can the UNAIDS 90-90-90 target be achieved? A systematic analysis of national HIV treatment cascades". BMJ Glob Health. 2017;2(2):e000227.
Geter A, Herron AR. MY Sutton. HIV-related stigma by healthcare providers in the United States: a systematic review. AIDS Patient Care STDs. 2018;32(10):418–24.
Aggleton P, Bhana D, Clarke D, Crewe M, Race K. E Yankah. HIV education: reflections on the past, priorities for the future. AIDS Educ Prev. 2018;30(3):254–66.
Kesten JM, Davies CF, Gompels M, Crofts M, Billing A, May MT, et al. Qualitative evaluation of a pilot educational intervention to increase primary care HIV-testing. BMC Fam Pract. 2019;20:74.
Ssewamala F, Bermudez L, Neilands T, Mellins C, McKay M, Garfinkel I, et al. Suubi4Her: a study protocol to examine the impact and cost associated with a combination intervention to prevent HIV risk behavior and improve mental health functioning among adolescent girls in Uganda. BMC Public Health. 2018;18(1):693.
Kapiriri L, Lee NM, Wallace LJ, Kwesiga B. Beyond cost-effectiveness, morbidity and mortality: a comprehensive evaluation of priority setting for HIV programming in Uganda. BMC Public Health. 2019;19:359.
Azuogu BN, Ogbonnaya LU, Umeokonkwo CD, Alo C, Ifebunandu NA, Obionu CN, et al. Effect of multiple intervention models on uptake of HIV testing services and sexual behaviour among residents of military cantonments in south-East Nigeria. Afr J AIDS Res. 2019;18(2):89–94.
Solomon S, Solomon S, McFall AM, Srikrishnan AK, Anand S, Verma V, et al. Integrated HIV testing, prevention, and treatment intervention for key populations in India: a cluster-randomised trial. Lancet HIV. 2019;6(5):e283–96.
Mahat G. MA Scoloveno. Effectiveness of adolescent peer education programs on reducing HIV/STI risk: an integrated review. Res Theory Nurs Pract. 2018;32(2):168–98.
Borgia P, Marinacci C, Schifano P, Perucci CA. Is peer education the best approach for HIV prevention in schools? Findings from a randomized controlled trial. J Adolesc Health. 2005;36(6):508–16.
Sholeye O, Omotosho J, Kuponiyi T, Abosede O. Safeguarding the health of the Nigerian worker: the role of a workplace HIV/AIDS policy. Niger J Med. 2012;21(2):134–7.
Govender K, Beckett S, Masebo W, Braga C, Zambezi P, Manhique M, et al. Effects of a Short Message Service (SMS) Intervention on Reduction of HIV Risk Behaviours and Improving HIV Testing Rates Among Populations located near Roadside Wellness Clinics: A Cluster Randomised Controlled Trial in South Africa, Zimbabwe and Mozambique. AIDS Behav. 2019;23(11):3119–28. https://doi.org/10.1007/s10461-10019-02427-10466 [Epub ahead of print].
El-Bassel N, Gilbert L, Goddard D, Chang M, Wu E, Hunt T, et al. Efficacy of a group-based multimedia HIV prevention intervention for drug-involved women under community supervision: project WORTH. PLoS One. 2014;9(11):e111528.
Acknowledgements
The authors are thankful to Dr. Qihui Lin for assisting with manuscript preparation. The authors are also thankful to all of the participants from a Summit we hosted with our partners ShenZhen LongHua Center for Disease Control and Prevention in September 2018 in which we discussed analytic questions together for this systematic review. The authors are thankful to all authors who were involved in studies included in our reiview.
Funding
This study was supported by the Natural Science Foundation of China International/Regional Research Collaboration Project (72061137001), the Natural Science Foundation of China Young Scientist Fund (81703278), the Australian National Health and Medical Research Commission (NHMRC) Early Career Fellowship (grant ID APP1092621), the National Science and Technology Major Project of China (2018ZX10721102) the Sanming Project of Medicine in Shenzhen (SZSM201811071), the High Level Project of Medicine in Longhua, ShenZhen (HLPM201907020105), and the National Key Research and Development Program of China (2020YFC0840900). All funding parties did not have any role in study design, data collection and analysis, preparation of the manuscript or decision to publish.
Author information
Authors and Affiliations
Contributions
This study was conceived and designed by HZ in consultation with the other authors. DC and HZ extracted data and conducted the data analysis. DC drafted the first version of the manuscript and received extensive feedback from all co-authors. GL, KZ, XM, ZW1, YC2, TH, TY, YX and ZW2 reviewed and edited the manuscript. BC, YC1 and YC2 participated in the discussion of article search strategy in the preparation stage of article draft. WK, CS and KD participated in the information extraction of article in the modification stage, and gave modification opinions on the comments of reviewers. ZW1 and ZW2 represent Zixin Wang and Zhenyu Wang respectively. YC1 and YC2 represent Yaqi Chen and Yong Cai respectively. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests. Dr. Huachun Zou is a member of the editorial board (Associate Editor) of this journal.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:
Efficacy of HIV interventions among factory workers in low- and middle-income countries protocol of a systematic review.
Additional file 2:
PubMed, EMBASE, Scopus and PsycINFO search strategy.
Additional file 3:
Quality assessment of 13 studies of HIV interventions among factory workers in LMICs.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, D., Luo, G., Meng, X. et al. Efficacy of HIV interventions among factory workers in low- and middle-income countries: a systematic review. BMC Public Health 20, 1310 (2020). https://doi.org/10.1186/s12889-020-09333-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-020-09333-w