Abstract
Background
Postpartum family planning services is one of the recommended public health intervention aimed at reducing maternal and child morbidity and mortalities. However, there is a paucity studies in rural Tigray region. Therefore, determining the level and associated factors of contraceptive use among postpartum women has the potential to contribute in achieving the Ethiopian Health Sector Transformation Plan and to the Sustainable Development Goals on maternal and infant survival.
Methods
A community-based cross-sectional study was done among 1109 postpartum women from March 29, 2017 to April 29, 2017. Face –to–face interview was used for data collection. The collected data were entered and cleaned using EPI - INFO version 7statistical software and later exported to and analyzed using STATA version 12. Mixed-effects multilevel logistic regression analysis was used to identify the individual and community-level factors associated with contraception adoption. A two side p-value< 0.05 was considered to be statistically significant.
Results
The level of contraceptive use was 38.3%. Individual-level variables such as women belong to fourth (AOR = 1.2; 95% CI: 1.1–3.2) and fifth (AOR = 1.5; 95% CI: 1.3–2.5) wealth quintiles were identified as key predictors of contraception use. In addition, partner secondary (AOR = 2.3; 95% CI: 1.8–3.5) and diploma (AOR = 1.2; 95% CI, 1.1–2.6) educational-level and postnatal care (AOR = 2.0; 95% CI: 1.9, 4.3) were also significantly affected contraception use. Community-level variables such as high community-level antenatal care services use (AOR = 2.1; 95% CI: 1.9–4.2) and proximity of women to health facility (AOR = 3.0; 95% CI: 2.7–4.6) were also determinants of contraception uptake.
Conclusions
The status of contraceptive use in rural Tigray region was found to be low. It was found that both individual and community-level variables showed a marked determinant on postpartum contraception use. This study suggested that in order to increase contraceptive use the government should focus on increasing postnatal care, antenatal care services use and reduction of poverty level are important avenues for intervention.
Similar content being viewed by others
Background
Maternal health issue is remains a global challenge [1, 2]; complication related with pregnancy and childbirth is the leading cause of mortality and morbidity among women in their reproductive age period [3]. Every day, around 830 women die from preventable cause’s related pregnancy and childbirth. Of maternal mortality, almost all (99%) happened in developing countries [3]. In Ethiopia, maternal mortality is an important public health issue; 412 per 100,000 live births are dying [4], among the highest in the Sub-Saharan Africa (SSA) countries.
Postpartum family planning (PPFP) mainly focuses on the prevention of unintended and closed spaced pregnancies through the first one year following childbirth [5, 6]. An increase in contraception adoption during the postpartum period substantially reduces the rate of maternal and infant mortality [7]. A study done among women within one year of their last birth found that 95% of the women in middle and low income countries want to delay pregnancy within the next two years, but 70% are not yet using contraception [8].
In developing countries, if all unmet need for contraception are satisfied three-quarters would be declined in unintended pregnancies [9]. Existing studies show that if couples space their pregnancies more than 2 years apart, contraception can avert more than 30% of maternal mortalities and 10% of child deaths [10, 11]. However, the largest proportion of women with an unmet need for contraception is found among those in their first year after childbirth [8].
Accordingly, the World Health Organization (WHO) recommended that the interval between and attempt to the next pregnancy should be 24 months [12] since short birth intervals are associated with adverse pregnancy outcomes: induced abortions, miscarriage, preterm births, neonatal and child mortalities, still births and maternal depletion syndrome [13].
In Ethiopia, the higher proportions of unplanned pregnancies are due to short birth intervals [14] and low contraceptive utilization [4]. Based on the research findings approximately 21% of births happened due to short intervals of less than 24 months, and other 35% occur between 24 and 35 months [14]. In this context, postpartum period is important particularly for initiating contraception to space births in a healthy manner [5, 6, 15]. The Federal Democratic Republic of Ethiopia (FDRE) expanded and promoting through community-based distribution of family planning services at the women’s door level through health extension program since 2002 [16]. The government has removed all duty and taxes on the imported contraceptive and are available free of charge at public health care facilities since family planning is considered as key for enhancing attainment of the nation’s development goals [17]. Despite these interventions, the unmet need for contraceptive among postpartum women remains high (86%) [18]. There are a number of safe and effective family planning methods that can begin at various points after giving birth, including those used immediately postpartum to optimize birth spacing [19]. Addressing contraception issue in the postpartum period has a positive effect on maternal, neonatal, infant and child health survival because it enables women to achieve the ideal birth spacing [13, 20].
In Ethiopia, research finding are concentrated only on the micro-level characteristics [21,22,23] and have been positively associated with postpartum contraceptive use (e.g., secondary and above level of the mother’s educational, delivered with the assistance of a skilled attendant, attended postnatal care services). But associations with macro-level characteristics (e.g., district-level of antenatal care use, distance, sources of income and district residence) have largely been under looked. Furthermore, most of the studies on postpartum contraception use have applied single-level analytic techniques. Analyzing variables at the macro-level as if they were micro-level variables using the standard binary logistic regression model leads to loss of power. The traditional approach also suffers from a problem of analysis at the inappropriate level (atomistic or ecological fallacy) [24, 25].
The utilization of contraception is a complex scenario and influenced by different predictors [26, 27]. Individual characteristics interact with community variables to which individuals belong, meaning that women are influenced by their social contexts and that the characteristics of those communities are in turn affected by the individual variables that make up that community. However, most research evidence [21,22,23] did not addressed how predictors influence across the levels by applying a multilevel logistic regression analysis.
Therefore, the purpose of this study was to fill these gaps by assessing the use level and to estimate the effects (fixed and random) of individual and community-level factors with postpartum contraception use in the Tigray region. The finding from this research could help planners, programmers and decision makers to have a good insight of determinants of contraceptive use and to take appropriate intervention and this may increasing in the use of contraception methods, and a reduction of unintended pregnancies, maternal and child mortality rates.
Methods
Study design and setup
A community-based cross-sectional study was conducted from March 29, 2017 to April 29, 2017 in Central Zone of Tigray region. Four districts were selected from the 12 districts by lottery method. According to the 2017 Tigray Regional Health Bureau (TRHB) annual report, there were 1 comprehensive and specialized referral hospital, 1 infant comprehensive and specialized referral hospital, 17 general hospitals, 224 health centers and 668 health posts. Each cluster (Kebele) has a health post to provide maternal, child and reproductive health services. The Tigray regional state has made a tremendous achievements in improving maternal and child health services such as: currently unmet need for family planning in general population dropped to 18%, percentage with 4+ antenatal care visits (56.5%), institutional delivery (56.9%), postnatal care services utilization (45.4%), under-5 child mortality 59 per 1000 live births and magnitude of women age 15–49 have ever had an obstetric fistula 1.1% [4]. The Maternal Mortality Ratio (MMR) is 266 deaths per 100,000 live births [28].
Sample size determination
A single population proportion formula was applied to calculate the sample size required in the study. The following assumptions were considered to determine sample size required for the study. As there is no study done in rural Tigary region in particular and Ethiopia in general, the prevalence of women using contraceptives in the extended postpartum period was assumed to be 50%, a 95% Confidence Interval (CI), a 5% margin of error (d) [29] and a design effect (DE) of 3. The sample size was also increased by 5% for none-response rate. Accordingly, the estimated sample size was 1109.
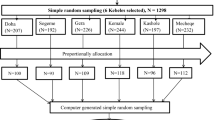
Study population and sampling techniques
All postpartum women who gave birth in the last 12 months prior to the study period in randomly selected clusters were taken as study population. A multi-stage cluster sampling technique was applied to select the study participants. Initially, four districts of the Central Zone of Tigray, namely Rural Adwa, Tanquae-Abrgelle, Tahtay-Maychew and Laelay-Maychew districts/woredas were selected randomly. A total of twelve clusters (three clusters per district) were selected randomly. All eligible women who gave birth within the past one year preceding the survey who were found in the selected clusters were studied using house-to-house survey.
Instruments
The main outcome variable for this study was postpartum contraceptive use and the independent variables were categorized in to two levels: Level one (lower- level variables) included the individual characteristics such as: socio-demographic, wealth index, maternal health use, infant sex and birth order. Level two (higher- level variables) included community variables such as distance to health facility, district residence, source of income and district- level of antenatal care use. The detail measurement variables are indicated in Table 1.
Data collection process
A structured and pre-tested questionnaire was used to collect the quantitative data. It was prepared first in English and then translated into ‘Tigrigna’, the local language. The tools were adapted from related kinds of studies [23, 26, 30]. Trained twelve BSc Nurse holders conducted the face- to- face interview and four MSc holders with a health background were supervised the data collection process. A field supervisor reviewed the questionnaires for completeness, quality and consistency at the end of each day while the investigators made periodic checks to ensure the quality of data collection process.
Data analysis and modeling
The collected data were entered and cleaned using EPI - INFO version 7 statistical software [31] and later exported to and analyzed using STATA version 12 [32]. Descriptive statistics was performed to determine the frequency of the outcome variable and the explanatory variables. The frequency and percentage of each category within the predictor variables was obtained. This study employed mixed-effects multilevel logistic regression analysis to identify the individual and community-level factors associated with contraception use. Multilevel model analysis considered into account the hierarchical structure of the data and clustering of responses at the different levels [25]. During the statistical analysis, the characteristics of postpartum women was considered as individual-level (lower-level variables) and characteristics of the clusters were taken as level two (higher- level variables).
In this study, the following equation elaborates the multilevel analysis for postpartum contraceptive use:

The two-level model was performed to assess the predictors of individual and community-level variables for contraception use. Where i and j are the level 1 (individual) and level 2 (community) units respectively; Pij is the probability of the outcome of interest for woman i in the cluster j; the b’s are the fixed coefficients (AOR); I and C refer to individual and community-level independent variables, respectively; and u indicate the random effects for the jth cluster. The error term, ε, shows unmeasured factors that may influence the primary outcome interest. In the model 1, no exposure variables were included in order to indicate the total variance in the uptake of postpartum contraception between community clusters. In the model 4, fixed effects at individual-level were included together with the community-level random effects. Finally, the results of fixed effects were presented as adjusted odds ratio (AOR) along with 95% confidence intervals (CI) and random effects as variance coefficients (VPC). The independent variables were retained in each of the models if the p- value< 0.2. A two side p-value < 0.05 was considered to be statistically significant. The variance coefficients were assessed as shown:
Where, π2/3 denotes the variance between mother from the same district (individual-level) and σ2u0 is the variance between districts (community-level variance). It gives how much of the variance is explained at the community-level [33].
Results
Socio-demographic characteristics
Table 2 summarizes the socio-demographic characteristics of the study participants. A total of 1109 postpartum women were interviewed. All of the study participants were between 16 and 49 years old. The women’s mean (±SD) age was 28.7(±6.4) years. All of the samples were Tigriyan by ethnicity. Forty-two percent of the mothers did not have any formal education while 42.7% of them attended primary-level education and 15.7% of them completed secondary or higher-level education. The majority of the interviewed mothers (80%) and their partners (86.1%) were farmers by occupation.
Characteristics of maternal health services use
One thousand eighteen (91.79%) attended at least one antenatal visit and 547(49.3%; 95% CI: 46.3–52.3%) attended the World Health Organization (WHO) recommended four visits. Nine hundred forty five (85.2%) of the mothers were reported that they delivered at health institutions. Seven hundred and two hundred forty five of the study participants gave birth at health centers and hospitals respectively. Out of the total interviewed women: one hundred fifty seven (14.0%; 95% CI: 12.3–16.3%), one hundred ninety three (17.4%; 95% CI: 15.1–19.6%) and one hundred fifty (13.5%; 95% CI: 11.5–15.6%) were reported having complication during prenatal period, delivery and puerperium period respectively. Moreover, 6.7% of the study participants delivered by caesarean section and instrumental. The postnatal care services were most frequently received from the health center. About 96.9% of the mothers and 68.1% of partner had tested for human immuno deficiency virus (HIV). Of them, seven mothers and five partners were infected for HIV. Nearly three-forth of the study participants received counseling services regarding postnatal care at their home by health extension workers (Table 3).
Postpartum contraceptive use
Table 4 highlights the key descriptive statistics of current contraceptive practice, revealing that four hundred twenty five (38.3%; 95%CI: 33.8–43.5%) were currently found using modern contraception among the postpartum women. Depot medroxy progesterone acetate contraceptive and implants were the most prevalent methods of contraception use. All of the study participants received their contraception from government health facility.
Predictors of contraceptive use
As clearly depicted on the multilevel logistic regression analysis Table 5, husband/partner education level, wealth index, postnatal care follow up, high community-level antenatal care utilization and distance from household to the health facility was independently and statistically associated with postpartum contraception use.
Individual-level effects
Women who had postnatal care visit were two times (AOR = 2.0; 95% CI: 1.9–4.3) more likely to adopt contraception in the extended postpartum period (EPP) than those who had no follow up services. The odds of contraceptive utilization were higher for postpartum women with higher socio economic status. Wealthier women who belonged to the fourth (AOR = 1.2; 95% CI: 1.1–3.2) and fifth quintile (AOR = 1.5; 95%CI: 1.3–2.5) were more likely to use postpartum modern contraception compared to women in the first, second and third quintile. Partners who attended secondary school were 2.3 times more likely to use contraception than those with no formal and primary educational-level (AOR = 2.3; 95% CI: 1.8–3.5) and those with diploma and above educational-level were 1.2 times more likely to use contraception during postpartum period (AOR = 1.2; 95% CI:1.1–2.6) (Table 5).
Community-level effects
High community-level antenatal care utilization was 2.1 times more likely to use contraception (AOR = 2.1; 95% CI: 1.9–4.2). Women who were found proximal to the health facility (< 1 km) had higher odds to utilize contraception compared to health facility with distance more than 1 km far found from the community household (AOR = 3.0; 95% CI:2.7–4.6) (Table 5).
Random effects
Results in Table 5, model 1 revealed that there are a variations in the probability of using postpartum contraception across communities and the variation were found significant (τ = 8.07, p = 0.001). The variance partition coefficient (VPC) showed that the intra-community correlation coefficient was estimated at 70%, which is variance that was explained by community-level variable. Model 2 showed the results of the effects of the individual-level variables. The intra-community correlation was 55.8% indicating that the clustering of the outcome variable (modern contraceptive use) across communities was as a result of the composition of the communities by individual-level characteristics. Model 3 the variation in use of postpartum contraception across communities remained significant. The model three shows that 50.9% of variation in the uptake of contraceptive use among the community is due to higher-level variables. The variance at the community-level in the model 4 remained significant. The intra-community correlation decreased to 49.6% indicating that the inclusion of community-level variables was important for obtaining a better explanatory model. In the model 4, the proportional change in community variance (PCV) (71.4%) of the variance in the contraceptive use across communities was due to the combination effects of lower and higher-level variables.
Model fitness statistics
Akakie Information Criterion (AIC) was used to estimate the goodness of the fit of the adjusted final model in comparison to the preceding models (individual and community-level model adjustments). Therefore, as indicated in Table 5, the values of AIC showed subsequent decreasing from model 1 to model 4. This implies that each model represents a significant improvement over the previous model and it points out the goodness of the fit of the final model built in the multilevel analysis [34, 35].
Multi-collnearity and interaction
Multi-collinearity was performed using the means variance inflation factor (VIF = 1.94). This means absence of any multi-collinearity between the predictor variables in the models. The presence of interaction among predictor variables was checked and there was no significant interaction between the individual and community-level variables.
Discussion
Postpartum family planning services is one of the recommended public health intervention aimed at reducing maternal and child morbidity and mortalities [15, 36]. Therefore, determining the level and associated factors of contraceptive use among postpartum women has the potential to contribute in achieving the Ethiopian Health Sector Transformation Plan (EHSTP) [17] and to the Sustainable Development Goals (SDGs) [1] on maternal and infant survival.
The overall prevalence of the current contraception method use in the extended postpartum period was 38.3% [95% CI: 33.8–43.5%]; injectable (47.1%) and Implants (29.4%) were the most frequently use methods. In addition, pills (14.1%) and Intra-uterine contraceptive device (IUD) (9.4%) were the other least frequently used methods by the users.
This finding was higher than that of studies done among postpartum women in North West Ethiopia (10.3%) [23], Uganda (28%) [30] and India (14%) [37]. This finding might be justified by the fact that due to the efforts done by the Ethiopian government health policy to strengthen for maternal and child health morbidity and mortality reduction strategies like: the different community and institutional-based reproductive health services and health education being given by health workers, introducing women development army and community health insurance [17] might have a positive effect for the increasing use of contraceptive.
Partner/husband-level of education was positively associated with postpartum modern contraceptive. Educational status of husbands promotes the use of contraceptives. This finding parallels to studies done in North West Ethiopia [23], Jimma town [38] and India [39]. This might be explained by the fact that higher educational-level of husbands/partner plays a key role in promoting discussion, communication and support for their partner/wife for contraceptives use.
Postnatal care service use was found as a significant determinant of contraceptive uptake. A similar finding is observed in studies conducted in North Ethiopia [22], North West Ethiopia [23], Kenya and Zambia [26], India [39] and Mexico [40]. The possible explanation is that those women who attended postnatal care visit higher odds to get information toward postpartum contraception. Moreover, postnatal visit may give the opportunity for contraceptive counseling and adoption in the postpartum period.
This study indicated a direct relationship between women’s wealth status and the adoption of postpartum contraceptive. This is because rich women can provide opportunity for better information and knowledge on postpartum contraceptive methods and better access to services. Moreover, rich women are more likely to be engaged in business association and other employment activities, and thus may be more likely to want to limit their fertility. This finding is goes in line with the reports from Zambia [26], Mozambique [41] and Nigeria [42]. This study highlights the need to empower women through economic opportunities enable them to make voluntarily informed choices.
High community-level antenatal care services use were found to be significantly associated with the use of modern contraception in the extended postpartum period. The possible explanation is the study participants who have high antenatal care use in the community are more likely to get information towards family planning utilization. This relationship is consistent with the findings reported by other studies [21, 26, 40, 43, 44].
Proximity of women to health facility was the other important community-level variable which is affecting contraceptive use. This study showed strong evidence that mother who lived near the health facility are more likely to use modern contraceptive method compared to those who lived far from the health institution [45]. Higher physical accessibility may increase postpartum contraceptive uptake. This may have an implication to policy change, design important justification and implementation of appropriate interventions.
The result showed that educational status was not statistically associated with postpartum contraceptive use to what would be expected. This finding might be influenced by certain contexts. Traditional factors may affect for postpartum women and the contribution of education to contraceptive use could be low [46].
The model 4 which combined both individual and community-level variables had a best fit than model 2 and model 3. This indicated that lower and higher-level variables should be considered when studying predictors of contraption utilization among postpartum women.
Limitations of the study
The main objective of the study was to assess the effect of individual and community-level variables on postpartum contraceptive use using a multilevel analysis. This study has some limitations that should be noted. It did not assess the whole array of determinants of contraceptive utilization; specifically, those variables related to reproductive health quality services and cultural related factors. However, we held a strong view that the inclusion of these variables wouldn’t change the main findings and subsequent conclusion as our analysis captured the most important services use measuring tools for the rural population in the study area.
Policy implications
At the district-level, it would be helpful to look at the variations in the use of modern contraceptive during extended postpartum period and critically analyze the predictors for the differences. The differences in postpartum contraceptive uptake associated with wealth quintile, antenatal care services use, postnatal care follow up and distance from household to health facility.
Conclusions
The status of contraceptive use is found to be low (i.e.38.3%) in rural areas of Tigray region. It was found that lower and higher-level variables showed a marked determinant on postpartum contraception use (Table 5). This study suggested that in order to increase contraceptive use the government should focus on increasing postnatal care, antenatal care services use and reduction of poverty level are important avenues for intervention.
Abbreviations
- AIC:
-
Akaike Information Criterion
- ANC:
-
Antenatal Care
- AOR:
-
Adjusted Odds Ratio
- CI:
-
Confidence Interval
- CS:
-
Cesarean Section
- DE:
-
Design Effect
- EHSTP:
-
Ethiopian Health Sector Transformation Plan
- EPP:
-
Extended Postpartum Period
- FDRE:
-
Federal Democratic Republic of Ethiopia
- HEW:
-
Health Extension Worker
- IRB:
-
Institutional Review Board
- MMR:
-
Maternal Mortality Ratio
- PCV:
-
Proportional Change in Community Variance
- PNC:
-
Postnatal Care
- PPFP:
-
Postpartum Family Planning
- SD:
-
Standard Deviation
- SDGs:
-
Sustainable Development Goals
- TRHB:
-
Tigray Regional Health Bureau
- VIF:
-
Variance Inflation Factor
- VPC:
-
Variance Partition Coefficient
- WHO:
-
World Health Organization
References
United Nations. The sustainable development goals report, New York. 2016.
McDougall L, Campbell O, Graham W. Maternal health. An executive summary for the Lancet’s series. Lancet. 2016;388
WHO, UNICEF, UNFPA, Group WB, Division at UNP. Trends in maternal mortality: 1990 to 2015.2015.
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF 2016..
World Health Organization. Programming strategies for postpartum family planning. 2013.
WHO,MCHIP,World bank,FIGO,Jhpiego, UNFPA, et al. Statement for Collective Action for Postpartum Family Planning. 2012.
Vernon R. Meeting the family planning needs of postpartum women. Stud Fam Plan. 2009;40(3):235–45.
Ross JA, Winfrey WL. Contraceptive use, intention to use and unmet need during the extended postpartum period. Int Fam Plan Perspect. 2001:20–7.
ADDING IT UP: Investing in Contraception and Maternal and Newborn Health, 2017. Guttmacher Institute 2017.
Singh S, Darroch JE. Adding it up: costs and benefits of contraceptive services. Guttmacher Institute and UNFPA. 2012;
Cleland J, Bernstein S, Ezeh A, Faundes A, Glasier A, Innis J. Family planning: the unfinished agenda. Lancet. 2006;368(9549):1810–27.
Marston C. Report of a WHO Technical Consultation on Birth Spacing Geneva Switzerland 13–15 June 2005.2007.
DaVanzo J, Hale L, Razzaque A, Rahman M. Effects of interpregnancy interval and outcome of the preceding pregnancy on pregnancy outcomes in Matlab, Bangladesh. BJOG Int J Obstet Gynaecol. 2007;114(9):1079–87.
USAID/MCHIP-Family Planning Access. Family planning needs during the First Two year postpartum period in Ethiopia. 2012.
McKaig C, Chase R. Postpartum family planning technical consultation—meeting report. Washington, DC: JHPIEGO, Baltim ore, Maryland; 2007.
Federal Democratic Republic of Ethiopia [FDRE], Ministry of Health [MOH]. National Guideline for Family Planning Services in Ethiopia. 2011.
Federal Democratic Republic of Ethiopia [FDRE], Ministry of Health [MoH]. Health Sector Transformation Plan [HSTP]. 2015/16–2019/20. Addis Ababa: Ministry of Health; 2015.
USAID-Family Planning Acess. Family Planning Needs during the Extended postpartum period in Ethiopia. 2009.
World Health Organization [WHO]. Medical eligibility criteria for contraceptive use. Geneva: World Health Organization; 2015.
Rutstein SO. Effects of preceding birth intervals on neonatal, infant and under-five years mortality and nutritional status in developing countries: evidence from the demographic and health surveys. Int J Gynecol Obstet. 2005;89:S7–S24.
Abera Y, Mengesha ZB, Tessema GA. Postpartum contraceptive use in Gondar town, Northwest Ethiopia: a community based cross-sectional study. BMC Women's Health. 2015;15(19)
Abraha TH, Teferra AS, Gelagay AA. Postpartum modern contraceptive use in northern Ethiopia: prevalence and associated factors. Epidemiol Health. 2017;39:e2017012.
Mengesha ZB, Worku AG, Feleke SA. Contraceptive adoption in the extended postpartum period is low in Northwest Ethiopia. BMC pregnancy and childbirth. 2015;15(1):160.
Dickinson LM, Basu A. Multilevel modeling and practice-based research. Ann Fam Med. 2005;3(suppl 1):S52–60.
Diez-Roux AV. Multilevel analysis in public health research. Annu Rev Public Health. 2000;21(1):171–92.
Do M, Hotchkiss D. Relationships between antenatal and postnatal care and post-partum modern contraceptive use: evidence from population surveys in Kenya and Zambia. BMC Health Serv Res. 2013;13(1):6.
Ngome E, Odimegwu C. The social context of adolescent women’s use of modern contraceptives in Zimbabwe: a multilevel analysis. Reproductive health. 2014;11(1):64.
Godefay H, Byass P, Kinsman J, Mulugeta A. Understanding maternal mortality from top–down and bottom–up perspectives: Case of Tigray Region, Ethiopia. Journal of global health. 2015;5(1):010404.
Lemeshow S, Hosmer D Jr, Klar J, Lwanga S. Adequacy of sample size in health sciences. New York: John Wiley and Sons; 1990.
Rutaremwa G, Kabagenyi A, Wandera SO, Jhamba T, Akiror E, Nviiri HL. Predictors of modern contraceptive use during the postpartum period among women in Uganda: a population-based cross sectional study. BMC Public Health. 2015;15(1):262.
Center for Disease Control and Prevention (CDC). https://www.cdc.gov/epiinfo/support/userguide.html.
Stata P. Stata survey data reference manual, release 12. StataCorp LP: College Station, TX; 2011.
Goldstein H, Browne W, Rasbash J. Partitioning variation in multilevel models. Underst Stat: Stat Issues in Psychol, Educ, Soc Sci . 2002;1(4):223–31.
Akaike H. A new look at the statistical model identification. IEEE Trans Autom Control. 1974;19(6):716–23.
Schwarz G. Estimating the dimension of a model. Ann Stat. 1978;6(2):461–4.
Gaffield ME, Egan S, Temmerman M. It's about time: WHO and partners release programming strategies for postpartum family planning. Global Health: Sci Prac. 2014;2(1):4–9.
Mahmood SE, Srivastava A, Shrotriya VP, Shaifali I, Mishra P. Postpartum contraceptive use in rural Bareilly. Indian J Comm Health. 2011;23(2):56–7.
Haile A, Enqueselassie F. Influence of women's autonomy on couple's contraception use in Jimma town, Ethiopia. Ethiopian journal of health development. 2006;20(3).
Shah NJ, Pradhan P. Reddy as, Joseph B. Contraceptive practices in newly married women in sub-urban Bangalore. Health and Popul-Perspect Issues. 2006;29(1):21–8.
Barber SL. Family planning advice and postpartum contraceptive use among low-income women in Mexico. Int Fam Plan Perspect. 2007:6–12.
Dias JG, de Oliveira IT. Multilevel effects of wealth on women's contraceptive use in Mozambique. PLoS One. 2015;10(3):e0121758.
Igbodekwe FC, Oladimeji O, Oladimeji KE, Adeoye IA, Akpa OM, Lawson L. Utilisation of modern contraceptive among women of childbearing age in resource constraint setting: evidence from 2008 National Demographic and health survey in Nigeria. J Health Sci. 2014;4(3):72–8.
Sebastian MP, Khan ME, Kumari K, Idnani R. Increasing postpartum contraception in rural India: evaluation of a community-based behavior change communication intervention. Int Perspect Sex Reprod Health. 2012:68–77.
Wilson EK, Fowler CI, Koo HP. Postpartum contraceptive use among adolescent mothers in seven states. J Adolesc Health. 2013;52(3):278–83.
Shiferaw S, Spigt M, Seme A, Amogne A, Skrovseth S, Desta S, Radloff S, Tsui A, Geer D. Does proximity of women to facilities with better choice of contraceptives affect their contraceptive utilization in rural Ethiopia? PLoS One. 2017;12(11):e0187311.
Riyamia AA, Afifib M, Mabryc RM. Women’s autonomy, education and employment in Oman and their influence on contraceptive use. Reprod Health Matters. 2004;12(23):144–54.
Acknowledgements
The authors would like to thank the Aksum University for funding this research project. Authors would also like to thank the study participants, data collectors, resident supervisors for their commitment and collaboration throughout the study period.
Funding
This research project was funded by Aksum University (AKU) with cooperative agreement code of AKU 0010/2009 is received by Teklehaymanot Huluf Abraha (MPH in Reproductive and Child Health). The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the article.
Availability of data and materials
All the required data are available in the main article document. In addition, the data set used and analyzed during the current study is available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
THA was principally involved in the proposal writing, designing, analysis, interpretation of the data and article preparation. BBG, BGA, DSB, LTT and GMW contributed to interpretation of the results, discussion and conclusion. All authors THA, BBG, BGA, DSB, LTT and GMW scientifically reviewed and approved the final version of the article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethical approval was approved by the Institutional Review Board (IRB) of College of Health Sciences, Aksum University, with the reference number of IRB 005/2017. Communications with the districts administration health office was made through a formal letter obtained from Aksum University. After explaining the objective of this study, written and voluntary informed consent was secured from each study participants before the actual data collection. The study participants were informed that they could withdraw from the study at any stage, and they were assured of confidentiality and privacy of the information they give.
Consent for publication
This article does not contain any individual person’s data in the form of image or video. Hence consent for publication is not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Abraha, T.H., Gebrezgiabher, B.B., Aregawi, B.G. et al. Predictors of postpartum contraceptive use in rural Tigray region, northern Ethiopia: a multilevel analysis. BMC Public Health 18, 1017 (2018). https://doi.org/10.1186/s12889-018-5941-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-018-5941-4