Abstract
Background
Physical activity (PA) interventions for the promotion of weight-management may benefit from increased choice and flexibility to overcome commonly-perceived barriers to PA. The aim of this study was to investigate the effects of a novel “points-based” approach to PA on body composition in inactive women, who are overweight or obese.
Methods
Seventy-six overweight or obese, inactive women were randomly allocated to one of three conditions: ‘Points-based’ PA (PBPA; 30 “PA points”•week− 1), Structured exercise (StructEx; 150 min moderate-intensity exercise•week− 1) or control (CONT; continue habitual inactive lifestyle) for a 24-week intervention. PA points for activities were adapted from MET values, and 30 points was equivalent to 150 min of brisk walking. Measures of body composition (dual-energy x-ray absorptiometry) and anthropometry were obtained at weeks 0, 4, 12 and 24. Self-report activities were recorded weekly, with objective measures of PA (tri-axial accelerometry) and self-report measures of food intake obtained at weeks 0 and 24.
Results
Fifty-eight women completed the study and provided data for primary outcomes. Of these, n = 41 and n = 19 provided data for food intake and objectively assessed PA. Mixed-design ANOVAs demonstrated that those in PBPA achieved a significant weight-loss at 24 weeks of − 3.3 ± 5.9 kg (− 3.4 ± 7.1%, p = 0.004). Waist circumference was reduced in PBPA at 24 weeks (− 2.8 ± 4.6 cm), compared with CONT (+ 2.1 ± 6.6 cm, p = 0.024). There was a trend for greater reductions in fat mass for those in PBPA vs. CONT (− 2.3 ± 4.6 kg vs. + 0.1 ± 2.0 kg, p = 0.075). Android fat was reduced in PBPA at both 12 weeks (− 6.1 ± 12.6%, p = 0.005) and 24 weeks (− 10.1 ± 18.4%, p = 0.005), while there was a trend for greater reductions in visceral adipose tissue in PBPA (− 5.8 ± 26.0%) vs. CONT at 24 weeks (+ 7.8 ± 18.3%, p = 0.053). Body composition, body weight and waist circumference were unchanged in StructEx. There were trends for increases in light-activity and reductions in sedentary time in PBPA. There was a trend for a reduction in daily energy intake of − 445 ± 564 kcal (p = 0.074), and a significant reduction in daily fat intake (p = 0.042) in PBPA.
Conclusion
A “points-based” approach to physical activity appears to be an effective strategy for inducing modest reductions in body weight and body fat in inactive women with overweight and obesity.
Trial registration
NCT02020239. Registered 12th December 2013.
Similar content being viewed by others
Background
Trends in adult body mass index (BMI) show a consistent increase in the global prevalence of obesity in men (3.2% to 10.8%) and women (6.4% to 14.9%) between 1975 and 2014 [1]. The World Health Organisation cites overweight and obesity as the 5th leading risk factor for mortality worldwide [2]. With such health implications allied with a considerable financial burden on health services [3], effective weight-management strategies are essential.
The importance of physical activity (PA) for weight-management is currently a topic of some contention. Most commonly, PA is accumulated through participation in structured exercise (i.e., purposeful, structured physical activity with the objective of maintaining or improving a component of fitness). Typically, weight-loss interventions consisting of exercise alone, without caloric reduction result in modest reductions in body weight [4, 5]. However, greatest weight-loss is achieved with a combination of exercise and diet [5, 6], and data underlines the efficacy of structured exercise and lifestyle PA for avoidance of weight-gain and for weight-loss maintenance [6,7,8,9,10]. Further, in comparison with dietary interventions, exercise interventions result in more favourable changes in body composition and reductions in fat mass relative to total body weight [11, 12]. Nevertheless, uptake of, and adherence to structured exercise programmes remains low [13,14,15]. For example, Edmunds et al. [13] found that only 51% of individuals who were overweight or obese successfully adhered to a 3-month exercise prescription programme. Similarly, Wiblur and colleagues [15] reported middle-aged, inactive women completed just 64% of the 96 walking exercise sessions in a 24-week programme. Hence, there remains need for effective as well as efficacious exercise and PA interventions [9].
Women represent a particularly inactive population. Recent data indicate that just 4% of women in England, U.K., engage in recommended levels of objectively assessed moderate-to-vigorous physical activity (MVPA) [16]. Still, despite the high prevalence of inactivity, 76% of women indicate they want to be more active [16]. The discrepancy in these statistics suggests there are barriers to PA engagement for this population. Accordingly, PA interventions are required which seek to address such barriers in order to facilitate the uptake and maintenance of PA among women [9].
Recent investigation would suggest two prominent perceived barriers to adoption and maintenance of PA among women: perceived lack of time [17] and lack of motivation [18, 19]. Consequently, it would seem desirable to develop time-efficient PA interventions that are compatible with every-day life [7], and do not require the structuring of exercise into perceived busy daily routines. It may also prove preferable for interventions to afford the exerciser choice and flexibility with regards to the manner in which PA is accumulated. Increased perceptions of autonomy, which can be achieved through offering greater choice and flexibility, is proven to increase intrinsic motivation and promote the uptake of, and adherence to PA behaviour [20, 21]. In addition, greater choice and flexibility, with the focus being on physical activity rather than structured exercise, may help overcome barriers of lack of enjoyment of, and low self-efficacy for exercise [22], the latter being particularly relevant for those who are overweight or obese [23, 24]. Previous research comparing structured exercise with lifestyle PA programmes has reported comparable favourable changes in physical activity and weight loss [25]. Still, research exploring intervention approaches that facilitate perceptions of autonomy and foster intrinsic motivation, may further enhance the effectiveness of PA programmes.
The aim of this study was therefore to investigate the effect of a novel points-based approach to PA on body weight and body composition in inactive middle-aged women, who were overweight. It was hypothesised that a points-based PA intervention (i.e., using PA points to provide choice and flexibility with regards to the accumulation of PA) would result in greater reductions in body weight, waist circumference and fat loss, compared with a traditional “structured” exercise intervention (30 min of moderate intensity exercise, 5 days per week). It was expected that the effectiveness of the intervention would be mediated by greater total PA engagement in the points-based PA condition.
Methods
Study design, Randomisation & Setting
The study utilised a between-subject, randomised control trial design, with participants allocated in a randomized manner to one of three groups for a 24-week study period: a points-based physical activity condition (PBPA); structured exercise condition (StructEx); a waiting-list control condition (CONT). Randomisation of participants (1:1:1 ratio) occurred at the individual level. An equal number of plain, sealed envelopes, each indicating either PBPA, StructEx or CONT, were placed in a box by a member of the research team, and participants drew an envelope to select their randomised condition. All study testing was conducted at the School of Sport, Exercise & Rehabilitation Sciences, University of Birmingham. Ethical approval was gained from the Solihull NRES Committee (Protocol number 13WM0331). This study was registered at clinicaltrials.gov (NCT02020239). The study was conducted and is reported in accordance with the CONSORT 2010 Statement.
Sample size
To identify an approprirate sample size, an a priori sample size calculation was conducted using G* Power software [26]. Based on previous studies demonstrating fat mass or body weight reductions of > 5% [27,28,29,30] calculations revealed a necessary sample of between 33 and 54 participants to detect between-group differences of medium-large effect (f = 0.35–0.45, power = 0.8, α = 0.05). Due to the free-living nature of the present study and the number of primary outcome measures, and allowing for a 20% drop-out rate, a sample of 75 participants was sought. This sample size (total and for each level of the independent variable) is in line with a number of previous studies in the field [31,32,33].
Participants
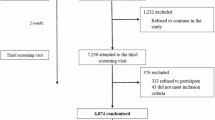
Of the 289 assessed for eligibility, 76 women participants (mean age 41 ± 2 years; mean BMI 29.2 ± 3.4 kg•m− 2) were recruited from the West Midlands, UK and admitted to the study (Fig. 1). Inclusion criteria were: age 21 to 50 years; a BMI of 25-35 kg•m− 2; and being physically inactive (<150mins of self-reported MVPA per week). Exclusion criteria were: dieting or intent to diet; any musculoskeletal, metabolic or cardiovascular disorders; medication that influenced lipid metabolism or appetite; blood pressure > 140/90 mmHg; smoking; and pregnancy or breast-feeding. Participants meeting inclusion/exclusion criteria were given details of study procedures and provided their informed consent.
Intervention
Participants in the StructEx condition were instructed to undertake 5 × 30 min of moderate-intensity exercise per week to achieve the weekly recommendations of 150 min of moderate-intensity exercise [34]. Through discussion with a member of the research team, considering exercise preference, perceived ability and feasibility (based on time, access to facilities and cost), participant identified a structured routine for completing 5 × 30 min of exercise each week to which they felt they would be able to adhere. All identified one or two modes of exercise to form their routine. Participants were advised on how to attain exercise of a moderate-intensity (i.e., “you should be able to talk, but not sing the words of a song” [35]).
Those in the PBPA condition were provided with a table of examples of different activities, each with a points score allocated per ten-minutes of activity (see Additional file 1). Points values were derived from MET scores [36], and adjusted for the MET score of 1.5 for sedentary behaviour. (Points score per 10 min of activity = MET score for that activity - 1.5. For example, the MET score for mowing the lawn is 5.5 METs; so the points score for mowing the lawn = 5.5–1.5 = 4 points). Participants were instructed to accumulate 30 points per week, equating to 5 × 30 min of brisk walking. This enabled the PBPA and StructEx conditions to be matched for MET-assigned PA-related energy expenditure. It was made explicitly clear to participants in both groups that activities should be of ≥10 min duration to contribute to their weekly points total, and these activities had to be additional to regular PA behaviour. In addition to the table of activities provided, participants in PBPA were asked what other forms of activity they may be interested in undertaking and points scores were provided for these activities. It was made clear to participants that they were not restricted to the activities in the table and those discussed at this preliminary visit; if they performed any additional type of activity, they were instructed to contact a member of the research team to receive a points score for that activity. Activities for which points scores were requested included chopping wood (4.5 points), painting and wallpapering (1.5), moving furniture (4.5), shopping (0.8) and bowling (1.5).
To encourage adherence, participants in PBPA and StructEx were contacted by telephone and email twice weekly for the first 4 weeks, and once fortnightly from weeks 4 to 12. Participants were asked of their adherence to the condition in which they were in. If target points/min were being achieved, positive reinforcement was offered. If not, then they were encouraged to persevere, and reminded of the typical benefits of being more active for health and general well-being. No contact was made during weeks 13 to 24, other than to arrange study visits.
Those in the CONT condition were instructed to maintain their current lifestyle for the 24-week study period. They were informed that they would be offered the opportunity to complete the intervention of their choice after the study period. All participants, in all three conditions, were instructed not to consciously change their dietary habits.
Procedures and protocols
Pre-testing
Participants arrived at the School of Sport, Exercise and Rehabilitation Sciences, University of Birmingham for an initial visit. Following informed consent, measurements of height, weight and blood pressure were recorded. Participants were then randomly allocated to one of the three study conditions by draw of opaque, sealed envelopes. Participants were then given verbal instructions on how to accurately complete the three-day food diary and wear the activity monitor. A separate one-day food diary was administered to be completed the day before the baseline test day. Participants would be asked to replicate this intake the day prior to all subsequent test days, with one-day food diaries completed on the day before each trial visit to allow for a check of adherence to the dietary control. One week prior to the test day at week 24, the participant was contacted by email or telephone and food diary and activity monitor were collected by or posted to the participant.
Test-day protocol
Participants returned to the laboratory a minimum of 5 days after visit 1 for baseline measures. Test-day visits were repeated at weeks 4, 12 and 24. At each visit, participants arrived between 07:00 and 09:00 after a minimum 10 h overnight fast and after abstaining from exercise or alcohol consumption during the previous 24 h. Upon the negative result of a urine pregnancy test and after voiding, anthropometric measures of height, weight and waist and hip circumference were obtained. The dual-energy x-ray absorptiometry (DXA) scan for analysis of body composition was then conducted. Participants were then provided with a small glass of water and a cereal bar to break their fast. At baseline and week 24, food diaries and activity monitors were collected from participants.
Outcome measures
Primary outcomes
Body composition
Body composition was assessed using the DXA method (Hologic Discovery QDR). Calibration and quality control checks were conducted prior to data collection for each trial visit. Values of whole-body fat mass (WBFM) and lean mass (WBLM), as well as measures of central adiposity were obtained. Android fat and abdominal visceral adipose tissue area (VAT) were measured across the abdomen in a 5 cm wide region between the iliac crest and the 4th lumbar vertebrae [37]. All values were calculated using the Hologic software programme (version 13.4.2).
Anthropometric measures
Body weight was assessed by semi-nude, post-void weighing using digital scales (Ohaus Champ II). Height was measured using a stadiometer (seca 220) and waist (at the level of the umbilicus) and hip (maximum posterior extension of the buttocks, level in the transverse plane) circumferences were measured using a tape measure (seca 201). Measurements were conducted by the same women researcher to maintain reliability. Circumferences were measured three times and a mean value calculated.
Secondary outcomes
Physical activity
Self-report PA was recorded by participants using a hard-copy activity diary. PA points and minutes of exercise were recorded by those in PBPA and StructEx, respectively, with weekly totals calculated for monitoring. Participants were encouraged to add each entry into the diary as soon after completing the exercise or activity as possible, clearly stating the type of activity or exercise, the duration and the points score for the activity, where relevant. Entries were checked for clarity and calculations checked for accuracy by a member of the research team at each visit to the laboratory. Objectively-measured PA was assessed using the GT3X accelerometer (Actigraph, FL). The GT3X accelerometer records movements measured over pre-specified time periods (epochs). Movements are summed to represent activity counts and interpreted to estimate frequency, intensity and duration of PA. In this study, accelerometers were initialised to measure PA over 15 s epochs. Sedentary time, light intensity PA and MVPA engagement were determined using cut-points as per Troiano and colleagues [38]. Participants were instructed to wear the accelerometer on their right hip during all waking hours for three consecutive days. Data was analysed from participants who provided a full 3 days of valid data (valid day = ≥10 h wear-time).
Food intake
Food intake was recorded using a 3-day weighed food diary (two weekdays and one weekend day). Prior to the collection of data, participants were provided with weighing scales and instructed how to accurately complete the diary. They were also provided with an example of a highly-detailed recording of intake. Participants were asked to avoid recording on days when it was expected that eating behaviour would be atypical. The completed food diaries were inspected upon collection from the participants and any foods or weights that were lacking detail or clarity were queried to help obtain necessary additional information. Food diaries were analysed using Dietplan (version 6.0) to gain mean daily intakes of total energy (kcal), carbohydrate, protein and fat (grams).
Statistical analysis
Analyses were conducted using SPSS (version 22.0). Baseline differences for all variables were assessed using one-way ANOVA. Where significant differences were observed, change-from-baseline values were used. For variables where magnitude of change over time is of likely of specific interest (body weight and fat mass), change-from-baseline data was also presented and analysed. Mixed-design ANOVA with repeated measures were used to assess differences between groups from baseline weeks 4, 12 and 24 (body composition, body weight and waist circumference) and baseline to 24 weeks (objective PA and food intake). For objective PA, percentage times spent in different intensities of PA were used in analyses to adjust for variability in accelerometer wear. Bonferroni post-hoc tests were used to interpret significant main and interaction effects.
For primary outcome measures, missing data analysis using the multiple imputations techniques was conducted for missing data points at weeks 4 and 12. This was the case for 6 measures in total (2 control participants missing data at 4 and 12 weeks and 2 StructEx participants missing data at 12 weeks).
Results
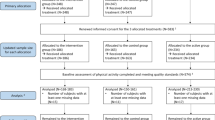
Of the 76 participants admitted to the study, 58 completed the intervention period and attended the 24-week follow up. The data of all 58 were analysed for all primary outcome measures. Data of 19 participants who provided ≥3 days accelerometer data (≥10 h·day− 1) were analysed for objectively measured PA and data of 41 participants were analysed for food intake (Fig. 1).
Body composition
Absolute values for WBLM, WBFM, VAT and android fat are shown in Table 1 and change from baseline data is shown in Fig. 1. For WBFM, the condition x time interaction approached significance (p = 0.060, η2p = 0.89). There was a significant time main effect (p = 0.036, η2p = 0.69), although pairwise comparisons did not identify significant differences between specific time points. When analysing change-from-baseline data (Fig. 2a), there was a significant group x time interaction (p = 0.049, η2p = 0.95), with a trend for a difference in change-from-baseline at 24 weeks for WBFM between CONT and PBPA (p = 0.075, d = 0.683, 95%CI: -5.04 – 0.17 kg). In PBPA, reduction in WBFM was significantly greater at 12 weeks and 24 weeks, compared with at 4 weeks (both p < 0.05). There was a significant group x time interaction for WBLM (p = 0.028, η2p = 0.088). However, no significant post-hoc pairwise comparisons were present.
Values for VAT differed significantly between groups at baseline. Therefore, change-from-baseline values are included and used for analysis (Fig. 2b). There was a significant group x time interaction for VAT change-from-baseline (p = 0.024, η2p = 0.103). The difference in change-from-baseline between CONT and PBPA approached significance at 24 weeks (p = 0.053, d = 0.743, 95%CI: -0.91 – 172.3 g). There was a significant group x time interaction for android fat (p = 0.004, η2p = 0.137. Table 1) with mean values significantly lower at 12 weeks and 24 weeks compared with baseline in PBPA (p = 0.005, d = 0.285, 95%CI: -0.34 – -0.04 kg and p = 0.005, d = 0.373, 95%CI: -0.50 – -0.06 kg, respectively) and values significantly lower in PBPA than StructEx at 24 weeks (p = 0.048 d = 0.771, 95%CI: -1.23 – -0.40 kg).
Anthropometric measures
Data for anthropometric measures are shown Table 1. There was a significant group x time interaction for body weight. Post-hoc analysis for within-group comparison showed that, in PBPA, body weight was significantly lower at 24 weeks compared with baseline (p = 0.004, d = 0.361, 95%CI: -5.73 – -0.78 kg) and 4 weeks (p = 0.008, d = 0.295, 95%CI: -4.59 – -0.50 kg). Comparisons between 24 weeks and 12 weeks approached significance (p = 0.053). There was a significant group x time interaction for change-from-baseline (p = 0.026, η2p = 0.111. Figure 3a). At 24 weeks, change-from-baseline was significantly greater in PBPA compared with CONT (p = 0.020, d = 0.865, 95%CI: -7.38 – -0.49 kg). Within PBPA, body weight-change-from-baseline was significantly greater at 24 weeks compared with 4 weeks (p = 0.004, d = 0.587, 95%CI: -4.39 – -0.70 kg) and 12 weeks (p = 0.006, d = 0.325, 95%CI: -2.84 – -0.39 kg).
Changes in body mass (a) and waist circumference (b) from baseline at 4, 12 and 24 weeks in CONT (○), StructEx (■) and PBPA (●). * denotes significant within-group difference, † denotes significant between-group difference, # denotes significant group main effect: change significantly different between PBPA and CONT
Waist circumference and waist-to-hip ratio differed significantly between CONT and StructEx at baseline. Therefore, change-from-baseline values were assessed. There was no significant group x time interaction effect (p = 0.832) for waist circumference but there was a significant main effect of group (p = 0.029, η2p = 0.123). Change in waist circumference (Fig. 3b) was significantly greater in PBPA compared with CONT (p = 0.024, d = 0.677, 95%CI: 0.3–5.8). There were no significant interaction or main effects for waist-to-hip ratio (all p values> 0.05).
Physical activity
Mean weekly minutes of self-reported exercise across the 24-week intervention period in StructEx was 172 ± 72 min. The mean weekly number of self-reported PA points reported was 39.1 ± 9.3, equating to 197 ± 54 min of brisk walking. When comparing self-reported minutes and self-reported minute equivalents, total activity reported did not differ between groups (p > 0.05).
Objectively measured PA is shown in Table 2. No significant main or interaction effects were observed from baseline to 24 weeks for sedentary time, light PA or MVPA (all p > 0.05). However, the time x group interaction effect for light PA approached significance (p = 0.066) and there was a trend for an interaction effect for sedentary time (p = 0.087). Interpretation of means indicated the PBPA condition increased light PA engagement and reduced sedentary time from baseline to 24 weeks, relative to StructEx and CONT conditions.
Food intake
Mean daily intakes of energy (kcal), carbohydrate, fat and protein at baseline and 24 weeks are shown in Table 3. There was a trend for a group x time interaction (p = 0.054, η2p = 0.122), with reductions in energy intake observed in CONT (− 233 kcal) and PBPA (− 445 kcal), compared with little change in StructEx (− 52 kcal). There was a significant main effect for time (p = 0.001, η2p = 0.219) with intake at 24 weeks lower than intake at baseline (d = 0.488, 95%CI: -384 – -106 kcal). There was a trend for group main effect (p = 0.061, η2p = 0.177).
There was a significant group x time interaction for absolute daily fat intake (p = 0.047, η2p = 0.130), with fat intake significantly lower at 24 weeks compared with baseline in PBPA (p = 0.006, d = 0.720, 95%CI: -5.8 – -32.2 g). Further, fat intake was significantly lower in PBPA compared with StructEx at 24 weeks (p = 0.035, d = 0.903, 95%CI: -1.3 – -47.9 g). There was a trend for a group x time interaction for absolute daily carbohydrate intake that approached significance (p = 0.059). No group x time interaction was observed for absolute daily protein intake. However, both carbohydrate and protein intake were significantly lower at 24 weeks relative to baseline across all groups (main effect for time, carbohydrate: p = 0.005, η2p = 0.163; protein: p = 0.011, η2p = 0.151). When assessing the contribution of energy from each macronutrient to total energy intake, there were no within-group or between group differences (all interactions and main effects, p > 0.1).
Discussion
This study investigated the effect of a novel points-based PA programme on body composition and body weight in inactive middle-aged women, who were overweight or obese, over 24 weeks. No reductions in WBFM, VAT or android fat were achieved in StructEx. However, participants in the PBPA condition successfully reduced WBFM by 2.3 kg (− 6.6%). Perhaps more importantly, significant reductions in android fat of 10.1% and reductions in VAT of 5.8% were achieved. When accounting for the 8% and 4% increases in these two measures, respectively, in the CONT condition, this equates to substantial improvements after 24 weeks of points-based PA.
The reduction in android fat observed in the PBPA condition is considerably greater than previously seen with 12 weeks of moderate intensity exercise training in overweight adults [39], while the reduction in VAT was similar to that observed with 16 weeks of multimodal exercise [33]. Excess visceral adipose tissue and android fat contribute to metabolic disorders [40] and have both been identified as independent risk factors for metabolic syndrome (MS) [41] and cardiovascular disease (CVD) [42, 43]. As such, any reduction in VAT and android fat may contribute towards the prevention of these long-term health conditions.
The PBPA and StructEx conditions were successful at inducing weight-loss and avoiding weight-gain, respectively. Results therefore suggest a PBPA centred intervention may be more effective for encouraging changes in PA behaviour likely to contribute meaningfully towards weight-loss, relative to exercise interventions that promote the following of a structured routine with less choice and flexibility. This study provides some evidence to support public health messages, and advice from practitioners and health care professionals, that advocate accumulating PA through the adoption of a variety and range of activities.
The mean 24-week weight-loss among individuals in the PBPA condition was 3.3 kg, equating to a 4% reduction from baseline. The corresponding rate of weight-loss per week (0.136 kg∙week− 1) is comparable to that observed in more efficacious exercise interventions [6, 12]. Still, this remains a smaller reduction in weight than is typically achieved through dietary restriction, and diet plus exercise interventions of a similar duration [6]. The American College of Sports Medicine [44] indicate that improvements in chronic disease risk factors can be achieved with weight-loss of as little as 2–3% of total body weight. Thus, the 4% reduction in total body weight observed in the PBPA condition further support the utility of employing a PBPA intervention to encourage levels of PA engagement likely to contribute towards clinically meaningful benefit.
This point can be further illustrated when examining results pertaining to waist circumference. Waist circumference is an independent risk factor of CVD [45, 46], with an increase of 1 cm resulting in a 2% increase in relative risk of a CV event [47]. A medium effect for change in waist circumference resulted in a 2.8 cm, (3.4%), reduction in waist circumference in PBPA compared with a 2.1 cm, (3.8%), increase in CONT, while change was minimal in StructEx. A waist circumference of > 88 cm is associated with increased risk of CVD [48]. In PBPA, three of the five participants that were in this at risk category at baseline reduced their waist circumference to less than 88 cm at 24 weeks. In comparison, of the ten participants in StructEx that were at increased risk at baseline all ten remained so at 24 weeks.
Based on self-reported activity, both StructEx and PBPA appeared to be equally well adhered to. Mean values of minutes and points exceeded the target of 150 min and 30 points per week, respectively. However, whilst self-reported adherence was similar between intervention conditions, both self-report and accelerometer assessed PA data indicate the PBPA intervention may have encouraged higher levels of PA engagement, relative to the StructEx and control conditions. Upon examination of individual self-report values, only two participants in PBPA reported failing to average 30 or more points per week over the 24 week whereas 6 participants failed to achieve an average of 150 min per week in StructEx. Further, four participants withdrew from the study in StructEx, citing loss of interest and failure to adhere due to work commitments, whereas only two participants withdrew for these reasons in PBPA. Specifically, while not statistically significant, a mean difference equivalent to 25 min of PA per week was reported between groups, with greater activity in PBPA.
Accelerometer data revealed a trend towards an increase in light PA among participants in the PBPA condition from baseline to 24 weeks, relative to the StructEx and CONT condition for whom declines in light PA were observed. In addition, a trend was also observed for a reduction in sedentary time in PBPA, equating to a group mean of 42 min less of sedentary behaviour a day. With no observed change in MVPA, it is possible that participants in PBPA replaced sedentary time with time engaged in light activity. The health enhancing effects of light PA are becoming increasingly well documented [49,50,51,52], while sedentary behaviour has been identified as an independent risk factor for CVD [53,54,55]. For example, replacing sedentary behavior with light physical activity is reported to result in improvements in cardio-metabolic health (e.g., favourable changes in fasting plasma glucose, triglycerides and cholesterol [56]. This adds further support to the efficacy of utilising a PBPA approach to encourage PA behaviour change in order to improve broader health outcomes among middle-aged women, again supporting public health advice of adopting a variety of activities.
Nonetheless, differences in PA between the three groups do not completely reflect the changes in body composition and anthropometry. The decrease in sedentary time and an apparent increase in light activity alone cannot explain the reduction in body weight and fat mass seen in the PBPA group, and neither do differences in sedentary time, light activity and MVPA explain the differences between PBPA and StructEx in particular at 24 weeks. This study afforded measures of change in self-reported food intake in a free-living setting. While not statistically significant, mean self-reported energy intake reduced by 445 kcal from baseline to 24 weeks in PBPA. This was in comparison to a negligible reduction of 52 kcal in StructEx and a smaller reduction of 233 kcal in CONT. Further, mean self-reported energy intake at 24 weeks was 558 kcal lower in PBPA compared with StructEx: a difference that likely contributed to the observed significant group main effect. This difference appears driven by the significantly lower fat intake (171 kcal) and a trend for a lower carbohydrate intake (268 kcal) in PBPA. It has been claimed that an energy deficit of greater than 500 kcal•day− 1 is required for successful weight-loss [44, 57, 58], so it is likely that the observed reduction in energy intake contributed considerably to the weight loss achieved in PBPA, with changes in PA behaviour having a much smaller role.
It may have been expected that increased activity and subsequent energy deficit and reductions in fat mass would promote mechanisms to increase appetite and food intake [59]. However, conversely, food intake was reduced in PBPA. This may be an example of the “spill-over” effect whereby engagement in one type of health related behaviour has a positive influence on engagement in others [60]. It has been shown from cross-sectional data that active individuals are more likely to display other healthy behaviours [61] including reduced fat intake [62], while women who were overweight reduced total energy intake during 12 weeks of resistance exercise [63]. Interestingly, this was not seen with the StructEx intervention. It may be that encouraging participants to collect PA points throughout the day in numerous activity bouts could have enhanced or prolonged engagement in the health-related behaviour of PA, compared with StructEx. This may have raised consciousness for health-related behaviours, and hence formed a greater stimulus for a “spill-over” effect. Also, the greater early-stage positive changes in body weight and waist circumference observed in PBPA may have resulted in increased self-efficacy for the adoption of other health behaviours [60].
Interestingly, a recent study by Beer et al. [64] observed a greater energy intake, driven by a high prevalence of “unhealthy” food choices, after an acute bout of exercise when participants had no choice over the mode, intensity, duration and time of commencement of the exercise, compared with participants who had choice over these factors. This was despite no difference in subjective appetite ratings. The authors propose that choice resulted in a greater perception of autonomy with regards to their PA engagement, and that this may have also resulted in greater perceived self-regulation in another health-related context (i.e., diet), facilitating the selection of healthier food choices. It is possible that the same mechanism underpinned healthier food choices for participants in PBPA, compared with those in StructEx. As such, a points-based approach to PA, while having small, positive effects on activity and sedentarism, may infer meaningful and beneficial effects on other health behaviors, such as diet.
The approach of favouring measures obtained within a free-living setting was necessary to assess the effectiveness of the exercise and PA interventions of this study, going beyond simply testing efficacy within a controlled laboratory setting. This was deemed preferable for increased ecological validity and generalisabilty. As such, the data would suggest that a points-based approach to physical activity may be an effective strategy for free-living interventions in women who are overweight.
The present study is not without limitations. Secondary measures were obtained only at baseline and week 24. It would have been preferable to obtain and analyse data for secondary measures at weeks 4 and 12. However, whilst attempts were made to do so, protocol adherence for objectively assessed PA and food intake was low. Consequently, the final sample for secondary measures may have been underpowered to detect significant differences between groups in response to the intervention, particularly with regards to PA, so findings in relation to these measures should be interpreted with some caution. Further studies are therefore required to consolidate the findings reported herein for which promising trends were observed (e.g., increases in light PA, reduced sedentary time, reduced energy intake). Further, adherence to the PBPA and StructEx conditions, and dietary intake were measured using self-report methods. It is acknowledged that such approaches can result in misreporting and inaccuracy of data. However, preference was for free-living measures and the assessment of the effectiveness, rather than efficacy, of the interventions. Self-reported PA data was also supported with data on objectively measured PA at baseline and week 24. However, we acknowledge that compliance with accelerometer protocols was low (33%), and as such, firm conclusions regarding the role of interventions tested herein, cannot be drawn on the basis of this data. Still, results provide an initial indication of the relative efficacy of these interventions for promoting engagement in light, moderate and vigorous PA, and reducing sedentary time. Despite the long-held appreciation of the limitations of food diaries [65, 66], this approach is still commonly-used in weight-management research [8, 11, 28, 31, 32]. Recently proposed electronic dietary intake assessment approaches, utilizing technology to allow ecological momentary analysis [67] have shown promise [68], and warrant consideration for use in future research.
The novel points-based approach to PA in the present study demonstrates promise as a strategy for reducing fat mass, body weight, waist circumference, sedentarism and food intake. Nonetheless, it was not successful at maintaining lean mass during weight-loss. This may be because the PBPA condition did not elicit an increase in MVPA, which may be considered a limitation of adopting such an approach to a PA programme. In addition to the current approach, and while ensuring autonomy over exercise components, incorporation of some degree of high-intensity [69] or resistance exercise [70] may help maintain lean mass; it is tempting to speculate that the greater increase in MVPA in StructEx compared with PBPA might have contributed to the better maintenance of lean mass. Further, incorporation of dietary manipulation, specifically increasing protein intake, may also facilitate maintenance of lean mass and further promote fat loss, as was observed by Josse et al. [71]. Further research employing such strategies is warranted to investigate the long-term effectiveness of a points-based approach to for increasing the effectiveness of PA towards levels necessary for improved body composition and weight-loss.
Conclusion
Findings suggest that a point-based approach to PA accumulation is an effective strategy for inducing modest but meaningful reductions in body weight and body fat in inactive women who are overweight and obese. This is likely a result of modest reductions in sedentary time, increases in light activity and of inducing a spill-over effect of altered eating behaviour and reduced energy intake. Consequently, a points-based system may prove a worthwhile consideration for healthcare professionals when administering exercise and PA strategies to tackle inactivity, sedentarism, and overweight and obesity.
Abbreviations
- ANOVA:
-
Analysis of variance
- BMI:
-
Body mass index
- CONT:
-
Control group
- CV:
-
Cardiovascular
- CVD:
-
Cardiovascular disease
- DXA:
-
Dual-energy x-ray absorptiometry
- MET:
-
Metabolic equivalent
- MS:
-
Metabolic syndrome
- MVPA:
-
Moderate-to-vigorous physical activity
- NRES:
-
National research ethics service
- PA:
-
Physical activity
- PBPA:
-
Point-based physical activity condition
- StructEx:
-
Structured exercise condition
- VAT:
-
Visceral adipose tissue
- WBFM:
-
Whole-body fat mass
- WBLM:
-
Whole-body lean mass
- η2 p :
-
Partial eta squared
References
NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet. 2016;387:1377–96.
Prospective Studies Collaboration. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–96.
Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378(9793):815–25.
Thorogood A, Mottillo S, Shimony A, Filion KB, Joseph L, Genest J, et al. Isolated aerobic exercise and weight loss: a systematic review and meta-analysis of randomized controlled trials. Am J Med. 2011;124(8):747–55.
Miller WC, Koceja DM, Hamilton EJ. A meta-analysis of the past 25 years of weight loss research using diet, exercise or diet plus exercise intervention. Int J Obesity. 1997;21:941–7.
Shaw KA, Gennat HC, O'Rourke P, Del Mar C. Exercise for overweight or obesity. Cochrane Database Syst Rev. 2006;2006(4):CD003817.
Saris WHM, Blair SN, Van Baak MA, Eaton SB, Davies PSW, Di Pietro L, et al. How much physical activity is enough to prevent unhealthy weight gain? Outcome of the IASO 1st stock conference and consensus statement. Obes Rev. 2003;4(2):101–14.
Skender ML, Goodrick GK, Del Junco DJ, Reeves RS, Darnell L, Gotto AM Jr, et al. Comparison of 2-year weight loss trends in behavioral treatments of obesity: diet, exercise, and combination interventions. J Am Diet Assoc. 1996;96(4):342–6.
Fogelholm M, Kukkonen-Harjula K. Does physical activity prevent weight gain – a systematic review. Obes Rev. 2000;1(2):95–111.
Wadden TA, Vogt RA, Foster GD, Anderson DA. Exercise and the maintenance of weight loss: 1-year follow-up of a controlled clinical trial. J Consult Clin Psych. 1998;66(2):429–33.
Ross R, Dagnone D, Jones PJ, Smith H, Paddags A, Hudson R, et al. Reduction in obesity and related comorbid condition after diet-induced weight loss or exercise-induced weight loss in men. A randomized, controlled trial. Ann Intern Med. 2000;133(2):92–103.
Janiszewski PM, Ross R. Physical activity in the treatment of obesity: beyond body weight reduction. Appl Physiol Nutr Metab. 2007;32(3):512–22.
Edmunds J, Ntoumanis N, Duda JL. Adherence and well-being in overweight and obese patients referred to an exercise on prescription scheme: a self-determination theory perspective. Psychol Sport Exerc. 2007;8(5):722–40.
Courney KS, Blanchard CM, Laing DM. Exercise adherence in breast cancer survivors training for a dragon boat race competition: a preliminary investigation. Psycho-Oncology. 2001;10:444–52.
Wilbur J, Chandler P, Michaels Miller A, Davis GC, Aaronson LS, Mayo K. Measuring adherence to a women’s walking program. West J Nurs Res. 2001;23(1):8–32.
Townsend N, Bhatnagar P, Wickramasinghe K. Physical activity statistics 2012. London: British Heart Foundation; 2012.
McArthur D, Dumas A, Woodend K, Beach S, Stacey D. Factors influencing adherence to regular exercise in middle-aged women: a qualitative study to inform clinical practice. BMC Womens Health. 2014;14(1):49.
Cerin E, Leslie E, Sugiyama T, Owen N. Perceived barriers to leisure-time physical activity in adults: an ecological perspective. J Phys Act Health. 2010;7(4):451–9.
Borodulin K, Sipila N, Rahkonen O, Leino-Arjas P, Kestila L, Jousilahti P, et al. Socio-demographic and behavioral variation in barriers to leisure-time physical activity. Scand J Public Health. 2016;44(1):62–9.
Teixeira PJ, Carraca EV, Markland D, Silva MN, Ryan RM. Exercise, physical activity and self-determination theory: a systematic review. Int J Behav Nutr Phys Act. 2012;9:78–106.
Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78.
Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc. 2002;34(12):1996–2001.
Deforche BI, De Bourdeaudhuij IM, Tanghe AP. Attitudes towards physical activity in normal-weight and overweight and obese adolescents. J Adolesc Health. 2006;38:560–8.
Ball K, Crawford D, Owen N. Too fat to exercise? Obesity as a barrier to physical activity. Aust N Z J Public Health. 2000;24(3):331–3.
Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW III, Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness. JAMA. 1999;281:327–34.
Faul F, Erdfelder E, Lang AG, Buchner A. G*power 3: a flexible statistical power analysis program for social, behavioral and biomedical sciences. Behav Res Methods. 2007;39(2):175–91.
Jakicic JM, Winters C, Lang W, Wing RR. Effects of intermittent exercise and use of home exercise equipment on adherence, weight-loss, and fitness in overweight women: a randomized trial. JAMA. 1999;282:1554–60.
Ross R, Janssen I, Dawson J, Kungl AM, Kuk JL, Womg SL, Nguyen-Duy TB, et al. Exercise-induced reduction in obesity and insulin resistance in women: a randomized control trial. Obesity. 2004;12(5):789–98.
Trapp EG, Chisholm DJ, Freud J, Boutcher SH. The effects of high-intensity intermittent exercise training on fat loss and fasting insulin levels of young women. Int J Obes. 2008;32:684–91.
Finlayson G, Caudwell P, Gibbons C, Hopkins M, King N, Blundell J. Low fat loss responses after medium-term supervised exercise in obese is associated with exercise-induced increases in food reward. J Obes. 2011;2011.
Volek JS, Gomez AL, Love DM, Weyers AM, Hesslink R Jr, Wise JA, Kraemer WJ. Effects of an 8-week weight-loss program on cardiovascular disease risk factors and regional body composition. Eur J Clin Nutr. 2002;56(7):585–92.
Kerksick C, Thomas A, Campbell B, Taylor L, Wilborn C, Marcello B, et al. Effects of a popular exercise and weight loss program on weight loss, body composition, energy expenditure and health in obese women. Nutr Metab. 2009;6:23.
Arciero PJ, Baur D, Connelly S, Ormsbee MJ. Timed-daily ingestion of whey protein and exercise training reduces visceral adipose tissue mass and improves insulin resistance: the PRISE study. J Appl Physiol. 2014;117(1):1–10.
Chief Medical Officers. Start Active, Stay Active. A report on physical activity by the four home countries‘ Chief Medical Officers. 2011. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/216370/dh_128210.pdf.
Department of Health. NHS Live Well: Physical activity guidelines for adults. https://www.nhs.uk/Livewell/fitness/pages/physical-activity-guidelines-for-adults.aspx.
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR Jr, Tudor-Locke C, et al. 2011 compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575–81.
Micklesfield LK, Goedecke JH, Punyanitya M, Wilson KE, Kelly TL. Dual-energy X-ray performs as well as clinical computed tomography for the measurement of visceral fat. Obesity. 2012;20(5):1109–14.
Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8.
Keating SE, Machan EA, O'Connor HT, Gerofi JA, Sainsbury A, Caterson ID, et al. Continuous exercise but not high intensity interval training improves fat distribution in overweight adults. J Obes. 2014;2014:12.
Wajchenberg BL. Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome. Endocr Rev. 2000;21(6):697–738.
Kang SM, Yoon JW, Ahn HY, Kim SY, Lee KH, Shin H, et al. Android fat depot is more closely associated with metabolic syndrome than abdominal visceral fat in elderly people. PLoS One. 2011;6(11):e27694.
Rexrode KM, Buring JE, Manson JE. Abdominal and total adiposity and risk of coronary heart disease in men. Int J Obes Relat Metab Disord. 2001;25(7):1047–56.
Sasai H, Brychta RJ, Wood RP, Rothney MP, Zhao X, Skarulis MC, et al. Does Visceral Fat Estimated by Dual-Energy X-ray Absorptiometry Independently Predict Cardiometabolic Risks in Adults?. J Diabetes Sci Technol. 2015.
Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK, et al. American College of Sports Medicine position stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41(2):459–71.
Rimm EB, Stampfer MJ, Giovannucci E, Ascherio A, Spiegelman D, Colditz GA, et al. Body size and fat distribution as predictors of coronary heart disease among middle-aged and older US men. Am J Epidemiol. 1995;141(12):1117–27.
Schneider HJ, Friedrich N, Klotsche J, Pieper L, Nauck M, John U, et al. The predictive value of different measures of obesity for incident cardiovascular events and mortality. J Clin Endocrinol Metab. 2010;95(4):1777–85.
de Koning L, Merchant AT, Pogue J, Anand SS. Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: meta-regression analysis of prospective studies. Eur Heart J. 2007;28(7):850–6.
Janssen I, Katzmarzyk PT, Ross R. Body mass index, waist circumference, and health risk. Evidence in support of current National Institutes of Health guidelines. Arch Intern Med. 2002;162(18):2074–9.
Buman MP, Hekler EB, Haskell WL, Pruitt L, Conway TL, Cain KL, et al. Objective light-intensity physical activity associations with rated health in older adults. Am J Epidemiol. 2010;172(10):1155–65.
Gando Y, Murakami H, Kawakami R, Tanaka N, Sanada K, Tabata I, et al. Light-intensity physical activity is associated with insulin resistance in elderly Japanese women independent of moderate-to vigorous-intensity physical activity. J Phys Act Health. 2014;11(2):266–71.
Gando Y, Yamamoto K, Murakami H, Ohmori Y, Kawakami R, Sanada K, et al. Longer time spent in light physical activity is associated with reduced arterial stiffness in older adults. Hypertension. 2010;56(3):540–6.
Howard B, Winkler EA, Sethi P, Carson V, Ridgers ND, Salmon JO, et al. Associations of low- and high-intensity light activity with cardiometabolic biomarkers. Med Sci Sports Exerc. 2015;47(10):2093–101.
Bankoski A, Harris TB, McClain JJ, Brychta RJ, Caserotti P, Chen KY, et al. Sedentary activity associated with metabolic syndrome independent of physical activity. Diabetes Care. 2011;34(2):497–503.
Rosenberg DE, Bellettiere J, Gardiner PA, Villarreal VN, Crist K, Kerr J. Independent association between sedentary behaviors and mental, cognitive, physical and functional health among older adults in retirement communities. J Gerontol A Biol Sci Med Sci. 2016;71(1):78–83.
Carson V, Wong SL, Winkler EA, Healy GN, Colley RC, Tremblay MS. Patterns of sedentary time and cardiometabolic risk amongst Canadian adults. Prev Med. 2014;65:23–7.
Healy GN, Winkler EA, Owen N, Anuradha S, Dunstan DW. Replacing sitting time with standing or stepping: associations with cardio-metabolic risk biomarkers. Eur Heart J. 2015;36(39):2643–9.
Donnelly J, Jakicic J, Blair S, Rankin J, Manore M. ACSM position stand on appropriate intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;42(2):459–71.
Jakicic JM, Clark K, Coleman E, Donnelly JE, Foreyt J, Melanson E, et al. American College of Sports Medicine position stand. Appropriate intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2001;33(12):2145–56.
Martins C, Kulseng B, King NA, Holst JJ, Blundell JE. The effects of exercise-induced weight loss on appetite-related peptides and motivation to eat. J Clin Endocrinol Metab. 2010;95(4):1609–16.
Mata J, Silva MN, Vieira PN, Carraca EV, Andrade AM, Coutinho SR, et al. Motivational "spill-over" during weight control: increased self-determination and exercise intrinsic motivation predict eating self-regulation. Health Psychol. 2009;28(6):709–16.
Pate RR, Heath GW, Dowda M, Trost SG. Associations between physical activity and other health behaviors in a representative sample of US adolescents. Am J Public Health. 1996;86:1577–81.
Simoes EJ. Byers, Coates RJ, Serdula MK, Mokdad AH, heath GW. The association between leisure-time physical activity and dietary fat in American adults. Am J Public Health. 1995;85(2):240–4.
Halliday TM, Davy BM, Clark AG, Baugh ME, Hedrick VE, Marinik EL, et al. Dietary intake modification in response to a participation in a resistance training program for sedentary older adults with prediabetes: findings from the resist diabetes study. Eat Behav. 2014;15(3):379–82.
Beer NJ, Dimmock JA, Jackson B, Guelfi KJ. Proving choice in exercise influences food intake at the subsequent meal. Med Sci Sports Exerc. 2017;49(10):2110–8.
Macdiarmid J, Blundell J. Assessing dietary intake: who, what and why of under-reporting. Nutr Res Rev. 1998;11:231–53.
Bingham SA. Limitations of the various methods for collecting dietary intake data. Ann Nutr Metab. 1991;35:117–27.
Hand RK, Perzynski AT. Ecological momentary assessment: perspectives on applications and opportunities in research and practice regarding nutrition behaviors. J Nutr Educ Behav. 2016;48(8):568–77.
Costello N, Deighton K, Dyson J, McKenna J, Jones B. Snap-N-send: a valid and reliable method for assessing energy intake of elite adolescent athletes. Eur J Sport Sci. 2017;17(8):1044–55.
Airin S, Linoby A, Mohamad Zaki M, Baki H, Sariman H, Esham B, et al. The effects of high-intensity interval training and continuous training on weight loss and body composition in overweight females. In: Adnan R, Ismail SI, Sulaiman N, editors. Proceedings of the international colloquium on sports science, exercise, engineering and technology 2014 (ICoSSEET 2014): Springer Singapore; 2014. p. 401–9.
Ryan AS, Pratley RE, Elahi D, Goldberg AP. Resistive training increases fat-free mass and maintains RMR despite weight loss in postmenopausal women. J Appl Physiol. 1995;79(3):818–23.
Josse AR, Atkinson SA, Tarnopolsky MA, Phillips SM. Increased consumption of dairy foods and protein during diet- and exercise-induced weight loss promotes fat mass loss and lean mass gain in overweight and obese premenapausal women. J Nutr. 2011;141(9):1626–34.
Acknowledgements
The authors would like to acknowledge and thank the funders of this research, Cereal Partners Worldwide, for their support.
Funding
Cereal Partners Worldwide provided an unconditional fund. Funding included the purchase and upkeep of some research equipment and the salary of Adrian Holliday as Research Associate.
Availability of data and materials
The dataset analysed during the current study is available from the corresponding author on resonable request.
Author information
Authors and Affiliations
Contributions
AKB and FT conceived the research question. AH, AKB, SAMF conceived the study design. AH, AKB, AB and EVF made substantial contributions to data collection. AH, AB and SAMF conducted data analysis. AH, AKB, SAMF and AB drafted the manuscript. AH, AKB, SAMF, AB, EVF and FT edited the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was gained from the Solihull NRES Committee (Protocol number 13WM0331). All participants provided informed written consent to partake in the study. Research was performed in accordance with the Declaration of Helsinki.
Consent for publication
Participants provided consent for their research data to be disseminated anonymously in a scientific journal.
Competing interests
The funding body were involved with the conception of the study question, but were not responsible for the study design, the data collection or the data analysis.
None of the authors have any financial interests in the research or in Cereal Partners Worldwide, except Frank Thielecke who was an employee of CPW when this study was initiated and works now as an independent consultant.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Table of activities provided to the participants, with allocated points per 10-min of activity. (PDF 219 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Holliday, A., Burgin, A., Fernandez, E.V. et al. Points-based physical activity: a novel approach to facilitate changes in body composition in inactive women with overweight and obesity. BMC Public Health 18, 261 (2018). https://doi.org/10.1186/s12889-018-5125-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-018-5125-2