Abstract
Background
Currently, family planning metrics derived from nationally-representative household surveys such as the Demographic and Health Surveys (DHS) categorise women into those desiring to space or limit (permanently stop) births, or according to their age in the case of young women. This conceptualisation potentially ignores a large and growing group of young women who desire to delay a first birth. This study uses household survey data to investigate the characteristics and needs for family planning of women who want to delay their first birth.
Methods
The research was conducted in two rural districts in southern Tanzania (Tandahimba and Newala), and nested within the Expanded Quality Management Using Information Power (EQUIP) study. Data were collected as part of a repeated cross sectional household survey conducted between September 2013 and April 2014. The socio-demographic characteristics, including parity, contraceptive practices and fertility intentions of 2128 women aged 13–49 were analysed. The association between women’s life stages of reproduction (delayers of first birth, spacers of subsequent pregnancies and limiters of future birth) and selected contraceptive outcomes (current use, unmet need and demand for modern contraceptives) was assessed using the point estimates and 95% confidence intervals for each indicator, adjusted for the survey design.
Results
Overall, four percent of women surveyed were categorised as ‘delayers of first birth’, i.e. sexually active but not started childbearing. Among this group, the majority were younger than 20 years old (82%) and unmarried (88%). Fifty-nine percent were currently using a modern method of contraception and injectables dominated their contraceptive use. Unmet need for contraception was higher among delayers (41%; 95% CI 32–51) and limiters (41%; 95% CI 35–47) compared to spacers (19%; 95% CI 17–22).
Conclusions
Delayers of first birth have very high unmet needs for modern contraceptives and they should be routinely and separately categorised and measured within nationally-representative surveys such as Demographic and Health Survey and Multiple Indicator Cluster surveys. Acknowledging their unique needs could help catalyse a programmatic response.
Similar content being viewed by others
Background
Evidence that family planning affects the life course of women from the moment of their own birth through to menopause is abundant and compelling [1–6]. Since family planning improves perinatal and child survival outcomes through lengthening the inter-pregnancy interval [3], children born to parents who had the power and means to decide on the number and spacing of pregnancies tend to be healthier, do better in school and get opportunities to earn higher incomes [4]. Furthermore, use of contraceptives can help both adolescent and post-adolescent women to start child-bearing later, thus allowing them to complete their education and offering opportunities to engage in income-producing activities [4, 7].
Currently, family planning metrics derived from nationally-representative household surveys such as the Demographic and Health Surveys categorise women into those desiring to space or limit (permanently stop) birth [8–11], or according to their age (particularly for young women aged 15–24 years). Those wishing to delay their first birth are not readily identifiable as a group with a distinct profile and their specific reproductive needs may be neglected even though this group of women are likely to become increasingly important. For example, an analysis of DHS data revealed unmet need for family planning to be highest amongst young married women with no children than those with a child [12]. In sub-Saharan Africa this finding is consistent with evidence that age at first sex is falling [13], age at first marriage is increasing [14] and women are more empowered to demand education and rights to determine the timing of a pregnancy [15, 16].
In Tanzania, public policies and strategies are in place for the achievement of universal access to family planning, backed-up by strong political commitment [17–20]. Men and women in the country including young people (10–24 years of age) regardless of parity, marital status, creed, race, or sexual preference are legally eligible to access accurate and complete family planning information, education and services without the need for parental or spousal consent [21]. Tanzania is also a Family Planning 2020 focus country, a global initiative that aims to expand contraceptive use to 120 million additional women and girls by 2020 [22, 23]. Girl’s enrolment into secondary school has increased over the last decade as a consequence of government commitment to provide free primary and secondary education [24, 25].
In the context of increased global attention to family planning and reproductive rights, and to the education of girls, it is important to understand the needs of girls and women who are sexually active but who wish to delay their first birth. Using data from the high fertility setting of Tanzania, we estimated how many sexually active married or unmarried women aged 13–49 years expressed a preference to delay their first birth, described their characteristics and examined the family planning outcomes for this group of ‘delayers’, contrasting them to spacers of subsequent pregnancies and limiters of future birth.
Method
Study setting
Detailed information about the study setting is provided elsewhere [26, 27]. Briefly, this research was carried out in two rural districts of Mtwara region in southern Tanzania: Tandahimba and Newala. The research was nested within the Expanded Quality Management Using Information Power (EQUIP) study [26, 27].
Tandahimba and Newala districts in Mtwara region-Southern Tanzania, where this study was carried out, cover an estimated population of over 400,000 people served by 63 health facilities [26–28], and is characterised as predominantly rural, having limited infrastructure [29] and high maternal and newborn mortality rates of 712 per 100,000 live births [30] and 31 deaths per 1000 live births respectively [31]. Makonde is the dominant ethnic group in the study area and over 90% of the population depends on agricultural activities which include cash (cashew nuts, sesame and groundnuts) and food crops (cassava, maize, rice and sorghum) [29]. The most recent Demographic and Health Survey (2010) estimated the Mtwara region to have a total fertility rate of 4.4, median age at first birth of 19 years, and high estimates for use of modern family planning methods (37%) in comparison to the rest of Tanzania mainland (27%) in 2010 [31], measured among married women aged 15–49 years. Among current users of any family planning method, 25% were using for spacing and 13% for limiting; and among those with unmet need (24%), half was for spacing and half for limiting (at 12% respectively) [31].
Study design and participants
Data were collected as part of the repeated cross sectional household surveys conducted by the EQUIP study between September 2013 and April 2014. Full details about the survey methods are reported elsewhere [26]. In short, each month, in each district, a representative sample of 10 household clusters (defined as sub-villages) each of 30 households was drawn. For each district, sub-villages were listed and the number of households in each sub-village cumulated then 10 clusters selected with probability proportional to the total number of households in the district. The survey applied modular survey tools compatible with DHS and Multiple Indicators Cluster surveys to estimate indicators across the reproductive, maternal and newborn health continuum among resident women aged 13–49 years. All household heads and resident women (aged 13 to 49 years) who gave consent were interviewed. Household heads were interviewed about residents and household characteristics; whereas, women aged 13–49 years were interviewed about maternal and newborn health care and family planning knowledge and services.
Data processing and analysis
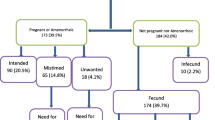
Data were analysed using STATA 13 [32]. For the purpose of this analysis, sexually active women included married (including cohabiting) and unmarried women aged 13–49 years who reported having had sexual intercourse in the past three months. Women’s life stages of reproduction were categorised as follows: (1) delayers of first birth (nulliparous who on survey day reported a preference to delay their first birth for at least two years or more), (2) spacers of subsequent pregnancies (parous who on survey day desired to wait for at least two years or more before having another child), (3) limiters of future birth (parous who had reached their desired family size and on survey day reported that they did not desire any subsequent children), (4) desire child soon (nulliparous and parous who on survey day desired to have a child within two years), and (5) infecund (women who on survey day reported that cannot get pregnant or had never been pregnant in the past five years and had never used contraceptives) as indicated in Table 1.
Modern contraceptives were defined according to Hubacher, [33] and included short acting contraceptives (pills, injectables and condoms), long acting reversible contraceptives (implants and intrauterine devices and systems (IUDs) and permanent contraceptive methods (male and female sterilization). We applied the definition of unmet need for contraceptives as per Bradley S et al. [34], but restricted to modern contraceptive methods as per Westoff [10]. Delayers of first birth who on survey day reported a preference to delay their first birth for at least two years or more but were currently not using modern contraceptives were classified as having unmet need.
Percentages and 95% confidence intervals were used to show distribution of women in various background characteristics including quintiles of socio-economic status that was derived from a wealth index constructed using principal components analysis of asset ownership. The association between women’s life stages of reproduction (delayers of first birth, spacers of subsequent pregnancies and limiters of future birth) and selected contraceptive outcomes (current use, unmet need and demand for modern contraceptives) was assessed using the point estimates and 95% confidence intervals for each indicator, adjusted for the survey design using “svy” commands in STATA.
Results
Study population
Between September 2013 and April 2014 a total of 4723 households were sampled across both districts, 3820 resident women aged 13–49 years identified, of whom 3578 were interviewed. Among the 3578 respondents, 2128 (59%) were sexually active in the last three months and included in this analysis. Of these, 1772 (83%) were currently married or cohabiting, mean parity was 3 births (range 0–11), 13% had no education, 97% were Muslim, and 92% were of the Makonde ethnic group (Table 2).
Women’s life stages of reproduction
The distribution of women across the life stages of reproduction is shown in Table 1. Four percent (95% CI 3–5) had never had a child and reported a preference to delay their first birth for at least two years or more (“delayers”), 37% (95% CI 35–40) had started child bearing and desired to wait for at least two years or more before having another child (“spacers”), 19% (95% CI 17–21) did not desire any subsequent children (“limiters”), 32% (95% CI 30–34) had at least one child and wanted another child in the next two years, 5% (95% CI 4–6) had never had a child and wanted a child in the next two years and 3% (95% CI 2–4) were infecund.
Characteristics of the delayers, spacers and limiters
Table 3 shows selected background characteristics of delayers of first birth and contrasts these to those of spacers and limiters. As expected, women categorised as delayers were younger on average than spacers and limiters, although of interest was that 18% of them were 20 years or older and 12% (95% CI 7–20) of the delayers were currently married or cohabiting. We found no difference in distribution by level of education attained, or other key socio-demographic characteristics (religion, ethnicity or socio-economic status of households) between women’s life stages of reproduction (delayers, spacers and limiters).
Current use, unmet need and demand for modern contraceptives among delayers, spacers and limiters
Table 4 presents current use, unmet need and demand for modern contraceptives by women’s life stages of reproduction (delayers, spacers, limiters). Fifty nine percent (95% CI 49–68) of delayers were currently using a modern method of contraception, similar to the proportion among spacers (65%; 95% CI 62–68) and limiters (53%; 95% CI 47–59). However, the proportion of unmet need for modern contraceptives was higher among delayers (41%; 95% CI 32–51) and limiters (41%; 95% CI 35–47) than spacers (19%; 95% CI 17–22). Total demand for modern contraceptives was high for all groups being universal amongst delayers (as indicated by their definition of not wanting a birth), 94% amongst limiters (95% CI 91–96) and 84% among spacers (95% CI 81–86).
Types of modern contraceptives used
Figure 1 presents the different types of modern contraceptives currently used by women according to their reproductive stage. Injectables (26%; 95% CI 23–29) and pills (25%; 95% CI 22–28) were the most commonly used methods, followed by implants (5%; 95% CI 4–7), female sterilization (3%; 95% CI 2–4) and condoms (2%; 95% CI 1–3). Use of injectables was higher among delayers (43%; 95% CI 34–53) than spacers (28%; 95% CI 24–31) or limiters, (17%; 95% CI 15–24). Condoms were also more commonly used by delayers (7%; 95% CI 3–15) than limiters (1%; 95% CI 1–3) or spacers (2%; 95% CI 1–3).
Discussion
In this study we highlighted a small but important group of sexually active women aged 13–49 years who had not started childbearing and wanted to delay their first birth. The majority of this group are younger than 20 years old and unmarried. More than half were currently using a modern method of contraception, and injectables dominated their contraceptive use. Despite the fact that in our findings, only four percent of women were delayers of first birth, this is equivalent to approximately 281,778 women aged 13–49 years in the whole country of Tanzania in 2010 [35]. Taking our findings on 41% of delayers having unmet need for family planning, this equates to 115,529 women in the whole country of Tanzania who want to delay their first birth but have an unmet need for modern contraceptives.
Delayed first birth, delayed marriage or delayed sexual debut all have the potential to lead to lower fertility [36]. In high and middle income countries, where secondary education is universal, women delay their first birth well beyond the adolescent years [37–39]. For example, in the United Kingdom the average age of women at first birth in 2013 was 30 years [40], and data suggests that first births to women aged 35–39 years and 40–44 years continue to rise [41]. While important cultural differences should persist, similar trends in delayed childbearing are likely to occur in sub-Saharan Africa as school enrolment and income-earning opportunities for women increase, and the continent moves away from widespread high fertility norms that places high expectations on young women to start childbearing, maintain family lineage and provide labour [24, 42].
Injectables are the most commonly used contraceptive method in East Africa (including Tanzania) accounting for over 40% of contraceptive use [43, 44], and were the most commonly used method by delayers of first birth in our study. Of concern is that contraceptive discontinuation rate for users of injectables and pills has been reported to be high, leading to part of the explanation for increases in unmet need in women who have tried either injectables or pills but discontinued their use without switching to another [45]. For young people who may engage in intercourse infrequently, there is clearly a need to provide alternatives, including long-acting reversible contraceptives such as implants or IUDs which can offer long-term contraceptive protection. But currently in Tanzania long-acting reversible contraceptives are not widely available throughout the country [46].
One of the strengths of our study was that it included women aged 13–14 years who are typically not included in the sampling frame of surveys such as DHS. Our analysis indicated that 11% of the sexually active delayers were aged 13–14 years and available data suggests that age at first sex is decreasing [13] and unintended pregnancies continue to exist among young teenage women in Tanzania [47, 48]. This is not a problem for Tanzania alone. The State of World Population report 2013 stated that of 7.3 million (19%) births to women under 18 years in developing countries, two million (3%) were to girls who were 14 years or younger [49] and who are most at risk of grave long-term health and social consequences from pregnancy. They are also likely to be excluded in the family planning policies and other reproductive health services [7].
Our study had three important limitations. First, with regard to definition of family planning indicators used by DHS, in addition to including women aged 13–49 not 15–49 years, we also included a recall period of three months not four weeks for sexual activity because of concerns that young unmarried people may have less frequent sexual relations than other women but still be at risk because of a lack of protection, and ignored because of a lack of attention. However this may have had the effect of over-estimating the number of women classified as recently sexually active, although our findings on family planning use for spacing and limiting were consistent with existing estimates. Further, we did not have data with which to directly categorise women as menopausal or not, although this was unlikely to affect our findings on delaying first birth.
Second, despite intensive training and supervision of enumerators the risk of social desirability bias cannot be eliminated, particularly with regards to reporting sexual activities among unmarried and young women, which may have led to an underestimation of the number of women at risk. A study from Ethiopia suggested that unmarried women aged 13–24 years might only report half of sexual activities but over exaggerated on contraceptive and condom use [50]. Third, recall bias on timing for last sexual activity may also have been present, especially among unmarried women; and errors in age reporting cannot be discounted.
Conclusions
In conclusion, our study demonstrates that even in this rural environment a small but important proportion of sexually active women would like to delay their first birth. Nearly all these women had some formal education, and all had a demand for modern contraceptives, but nearly half had an unmet need for contraception suggesting they are not currently well served by family planning programmes. We propose that delayers of first birth should be consistently categorised, using nationally representative survey data, preferably from a younger age than currently assessed, and their needs addressed in policy and programme formulation.
Abbreviations
- CI:
-
Confidence interval
- DHS:
-
Demographic health surveys
- FP:
-
Family planning
References
Brown W, Ahmed S, Roche N, Sonneveldt E, Darmstadt GL. Impact of family planning programs in reducing high-risk births due to younger and older maternal age, short birth intervals, and high parity. Seminars in perinatology. 2015;39(5):338–344.
Singh S, Darroch J, Ashford L. Adding It Up: The Costs and Benefits of Investing in Sexual and Reproductive Health 2014. New York: The Guttmacher Institute; 2014.
Cleland J, Conde-Agudelo A, Peterson H, Ross J, Tsui A. Contraception and health. Lancet. 2012;380(9837):149–56.
Canning D, Schultz TP. The economic consequences of reproductive health and family planning. Lancet. 2012;380(9837):165–71.
Ahmed S, Li Q, Liu L, Tsui AO. Maternal deaths averted by contraceptive use: an analysis of 172 countries. Lancet. 2012;380(9837):111–25.
Stover J, Ross J. How increased contraceptive use has reduced maternal mortality. Matern Child Health J. 2010;14(5):687–95.
Girls Count: A Global Investment & Action Agenda (Washington, DC: Center for Global Development, A Girls Count Report on Adolescent Girls) [http://www.icrw.org/publications/girls-count-global-investment-and-action-agenda] (Last accesssed 08 Aug 2015)
Cleland J, Harbison S, Shah IH. Unmet need for contraception: issues and challenges. Stud Fam Plann. 2014;45(2):105–22.
Understanding the Adolescent Family Planning Evidence Base. Available at https://pdfs.semanticscholar.org/8d5e/1367eda7ffe117caa0cd89dc22db91286a61.pdf. Accessed Jan 2017.
Westoff CF. Unmet need for modern contraceptive methods: DHS Analytical Studies No.28. Calverton: ICF International; 2012.
Woog V, Singh S, Browne A, Philbin J. Adolescent Women’s Need for and Use of Sexual and Reproductive Health Services in Developing Countries. New York: Guttmacher Institute; 2015.
MacQuarrie KLD. Unmet Need for Family Planning among Young Women: Levels and Trends. DHS Comparative Reports No. 34. Rockville: ICF International; 2014.
Doyle AM, Mavedzenge SN, Plummer ML, Ross DA. The sexual behaviour of adolescents in sub-Saharan Africa: patterns and trends from national surveys. Trop Med Int Health. 2012;17(7):796–807.
Shapiro D, Gebreselassie T. Marriage in sub-Saharan Africa: Trends, determinants, and consequences. Population Res Policy Rev. 2014;33(2):229–55.
You D, Hug L, Anthony D. UNICEF report Generation 2030 Africa calls upon investing in and empowering girls and young women. Reprod Health. 2015;12(1):18.
Cottingham J, Germain A, Hunt P. Use of human rights to meet the unmet need for family planning. Lancet. 2012;380(9837):172–80.
The United Republic of Tanzania, Ministry of Health and Social Wellfare: National Health Policy (in Swahili language) [http://www.tanzania.go.tz/egov_uploads/documents/sera_wizarafnl2_en.pdf] (Last accesssed 08 Aug 2015)
The United Republic of Tanzania, Ministry of Health and Social Welfare: The National Family Planning Costed Implementation Programm 2010–2015, updated July 2013 [http://www.fhi360.org/sites/default/files/media/documents/national-fp-costed-implementation-plan-tanzania-main-text.pdf] (Last accesssed 08 Aug 2015)
The United Republic of Tanzania, Ministry of Health and Social Welfare: Health Sector Strategic Plan III, July 2009 – June 2015: “Partnership for Delivering the MDGs” [http://www.mamaye.org/evidence/tanzania-health-sector-strategic-plan-iii-july-2009-%E2%80%93-june-2015] (Last accesssed 08 Aug 2015)
The United Republic of Tanzania, Ministry of Finance and Economic Affairs: National Strategy for Growth and Reduction of Poverty II [www.unpei.org/sites/default/files/PDF/TZ-MKUKUTA-Nat-Strategy.pdf] (Last accesssed 08 Aug 2015)
The United Republic of Tanzania, Ministry of Health and Socail Welfare: National Family Planning Guidelines and Standards. 2013. https://sites.google.com/a/ihi.or.tz/ihi-main-site/announ/ministryofhealthreleasesnewfamilyplanningguidelines. Accesssed 8 Aug 2015.
FP2020. Progress Report 2012–2013: Partnership in Action. Washington DC: FP2020, 2013. [http://www.mamaye.org/en/evidence/fp2020-partnership-action-2012-13] (Last accesssed 08 Aug 2015)
FP2020: Achieved Commitments for Tanzania: Progress Reports [http://www.familyplanning2020.org/entities/143/commitments] (Last accessed 4th Jan 2016)
Hoogeveen J, Rossi M. Enrolment and grade attainment following the introduction of free primary education in Tanzania. J Afr Econ. 2013;0(0):1–19.
Tanzania Regional Administration and Local Government: Pre- Primary, Primary and Secondary Education Statistics 2013 [http://www.pmoralg.go.tz/noticeboard/tangazo-1023-20141229-Basic-Education-Statistics-BEST/FINAL-NATIONAL-27-MAY-2014.pdf] (Last accessed 11 Mar 2016)
Marchant T, Schellenberg J, Peterson S, Manzi F, Waiswa P, Hanson C, Temu S, Darious K, Sedekia Y, Akuze J. The use of continuous surveys to generate and continuously report high quality timely maternal and newborn health data at the district level in Tanzania and Uganda. Implement Sci. 2014;9(1):112.
Hanson C, Waiswa P, Marchant T, Marx M, Manzi F, Mbaruku G, Rowe A, Tomson G, Schellenberg J, Peterson S. Expanded Quality Management Using Information Power (EQUIP): protocol for a quasi-experimental study to improve maternal and newborn health in Tanzania and Uganda. Implement Sci. 2014;9(1):41. doi:10.1186/1748-5908-1189-1141.
National Bureau of Statistics: 2012 Tanzania Population and Housing Census. Ministry of Finance, Dar es Salaam and President’s Office, Finance, Economy and Development Planning, Zanzibar [http://www.meac.go.tz/sites/default/files/Statistics/Tanzania%20Population%20Census%202012.pdf] (Last accessed 04 Apr 2016)
The Planning Commission Dar es Salaam and Regional Commissioner’s office Mtwara: Mtwara Regional Socio-economic Profile 1997 [www.tzonline.org/pdf/Mtwara.pdf] (Last accesssed 08 Aug 2015)
Hanson C, Cox J, Mbaruku G, Manzi F, Gabrysch S, Schellenberg D, Tanner M, Ronsmans C, Schellenberg J. Maternal mortality and distance to facility-based obstetric care in rural southern Tanzania: a secondary analysis of cross-sectional census data in 226 000 households. Lancet Glob Health. 2015; 3(7):e387-395. doi: 310.1016/S2214-1109X(1015)00048-00040. Epub 02015 May 00021.
National Bureau of Statistics, Tanzania Demographic and Health Survey 2010. Dar es Salaam, Tanzania: NBS and ICF Macro [http://dhsprogram.com/pubs/pdf/FR243/FR243[24June2011].pdf] (Last accessed 04 Apr 2016)
StataCorp. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP; 2013. Available on http://www.stata.com/support/faqs/resources/citing-software-documentation-faqs/. Accessed June 2016.
Hubacher D, Trussell J. A definition of modern contraceptive methods. Contraception. 2015;92(5):420–1.
Bradley S, Croft TN, Fishel JD, Westoff CF. Revising Unmet Need for Family Planning. DHS Analytical Studies No. 25. Calverton: ICF International; 2012.
National Bureau of Statistics: 2012 Tanzania Population and Housing Census. Population Distribution by Age and Sex. Ministry of Finance Dar es Salaam and Office of Chief Government Statistician President’s Office, Finance, Economy and Development Planning Zanzibar [http://ihi.eprints.org/2169/1/Age_Sex_Distribution.pdf] (Last accessed 04 Apr 2016)
Delayed marriage, contraceptive use, and breastfeeding. United Nations University 2016, WIDER Working Paper 2016/43. Available at https://www.wider.unu.edu/sites/default/files/wp2016-043.pdf. Accessed Jan 2017.
Changing families in the European Union: Trends and policy implications. Available on http://www.familiesandsocieties.eu/wp-content/uploads/2015/09/WP44Olah2015.pdf. Accessed Jan 2017.
Zeitlin J, Mohangoo A, Delnorn M, Alexander S, Blondel B, Bouvier-Colle M, Dattani N, Gissler M, Macfarlane A, Pal K. European perinatal health report. The health and care of pregnant women and babies in Europe in 2010. 2013.
Mathews T, Hamilton B. Mean Age of Mothers is on the Rise: United States, 2000–2014. NCHS Data Brief. 2016(232):1–8.
Childbearing across the EU28: 4 Facts [http://www.ons.gov.uk/ons/rel/vsob1/birth-summary-tables--england-and-wales/2013/childbearing-across-the-eu28--4-facts.html] (Last accessed 04 Apr 2016)
First births to older women continue to rise. NCHS Data Brief 152. Hyattsvile MD: National Center for Health Statistics; 2014. Available at https://www.cdc.gov/nchs/data/databriefs/db152.pdf. Accessed Jan 2017.
Dyer SJ. The value of children in African countries–insights from studies on infertility. J Psychosomatic Obstet Gynecol. 2007;28(2):69–77.
United Nations, Department of Economic and Social Affairs, Population Division: The World Contraceptives Patterns 2013 [http://www.un.org/en/development/desa/population/publications/pdf/family/worldContraceptivePatternsWallChart2013.pdf] (Last accessed 11 Mar 2016)
United Nations, Department of Economc and Social Affairs, Infochart: World Contraceptive Patterns 2015 [http://www.un.org/en/development/desa/population/publications/family/contraceptive-infochart-2015.shtml] (Last accessed 04 Apr 2016)
Ali MM, Cleland JG, Shah IH, Organization WH. Causes and consequences of contraceptive discontinuation: evidence from 60 demographic and health surveys. 2012.
Ministry of Health and Social Welfare (MoHSW) [Tanzania Mainland], Ministry of Health (MoH) [Zanzibar], National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), and ICF International 2015. Tanzania Service Provision Assessment Survey (TSPA) 2014–2015. Dar es Salaam, Tanzania, and Rockville, Maryland, USA: MoHSW, MoH, NBS, OCGS, and ICF International [http://dhsprogram.com/pubs/pdf/SPA22/SPA22.pdf] (Last accessed 04 Apr 2016)
Nyalali K, Maternowska C, Brown H, Testa A, Coulson J, Gordon-Maclean C. Unintended pregnancy amongst teenagers in Arusha and Zanzibar, Tanzania: a situation analysis. London: Marie Stopes International; 2013.
Calvert C, Baisley K, Doyle AM, Maganja K, Changalucha J, Watson-Jones D, Hayes RJ, Ross DA. Risk factors for unplanned pregnancy among young women in Tanzania. J Fam Plan Reprod Health Care. 2013;39(4):e2. jfprhc-2012-100389.
State of world population 2013. Motherhood in childhood. Facing the challenge of adolescent pregnancy [http://www.unfpa.org/sites/default/files/pub-pdf/EN-SWOP2013-final.pdf] (Last accessed 08 Aug 2015)
Lindstrom DP, Belachew T, Hadley C, Hattori M, Hogan D, Tessema F. Survey estimates of non-marital sex and condom knowledge among ethiopian youth: improved estimates using a non-verbal response card. Stud Fam Plann. 2010;41(4):251.
Acknowledgements
We are grateful to district medical officers in the study area for their cooperation and research participants for participating in the study. We thank EQUIP continuous survey team for data collection.
Funding
The research leading to these results has received funding from the European Union Seventh Framework Programme FP7/2007–2013 under grant agreement no. 265827 and from Graduate Women International (previously the International Federation of University Women)-Funds for women Graduates Fellowship 2014/2015. The funders of the study had no role in study design, data collection, analysis and interpretation or writing of the report. The corresponding author had full access to all data, drafted the manuscript and had final responsibility for the decision to submit for publication.
Availability of data and materials
Anonymised data table can be available upon request to the corresponding author.
Authors’ contributions
YS and TM were responsible for the study concept and design and statistical analysis. YS wrote the first draft of the manuscript. All authors were involved in the interpretation of findings and revision of the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors have declared that they have no competing interests.
Consent for publication
Not applicable. All individual details were anonymised.
Ethics approval and consent to participate
Ethical approval for the study was granted by review boards at the London School of Hygiene and Tropical Medicine (UK), Ifakara Health Institute (Tanzania) and the National Institute for Medical Research in Tanzania through the Tanzanian Commission of Science and Technology. Written, informed consent from household heads and women aged 13–49 years was obtained, including from caregivers of women younger than seventeen.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Sedekia, Y., Nathan, R., Church, K. et al. Delaying first birth: an analysis of household survey data from rural Southern Tanzania. BMC Public Health 17, 134 (2017). https://doi.org/10.1186/s12889-017-4069-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-017-4069-2