Abstract
Background
The increase in life expectancy of HIV-infected patients has driven increased costs due to life-long HIV treatment and concurrent age-related comorbidities. This population-based study aimed to investigate the burden of chronic diseases and health costs for HIV+ subjects compared to the general population living in Brescia Local health Agency (LHA) over a 12-year period.
Methods
LHA database recorded diagnoses, deaths, drug prescriptions and health resource utilization for all residents during 2003–2014. We estimated HIV prevalence and incidence, HIV-related mortality as well as prevalence of chronic diseases in HIV+ subjects. Observed/expected ratio of chronic diseases was calculated by indirect standardization with the general population as reference. Direct cost of HIV care and determinants were estimates across the period.
Results
HIV prevalence increased from 220 to 307 per 100 000 person-years while incidence decreased from 16.1 to 10.8 per 100 000 person-years from 2003 to 2014. Prevalence of most comorbidities increased over time but it reduced significantly (annual mean change − 0.7 %) when adjusting for age and gender. Observed to expected ratio for each chronic disease in HIV+ subjects decreased over time. Cost of HIV+ cures increased (+25 %) mainly due to cost for drugs (+50 %) but it stabilized in recent years. CD4+ cell count at the time of diagnosis was an important predictor of cost for HIV management.
Conclusions
Expenditures for HIV-infection are driven mainly by drugs cost and they have increased overtime. However, our findings suggest that spending on public health for HIV care can improve prognosis of HIV-infected patients, reduce transmission of HIV infection and reduce the global burden of chronic diseases, leading to a reduction of HIV global cost in the medium-long time.
Similar content being viewed by others
Background
During the past twenty years, antiretroviral therapy (ART) introduction has dramatically modified the natural evolution of HIV infection, with decreased morbidity and increased survival of infected patients [1–4]. Due to the important decrease in mortality and consequent aging of HIV-infected people, HIV infection is responsible for an increasing burden on healthcare services. Treating with ART has resulted in a continuous increase of the total treatment cost, mainly because of the appearance of new, more effective but more expensive drugs during last years [5, 6]. The increase in life expectancy of HIV-infected patients [7, 8] has also driven increased costs due to life-long HIV treatment and concurrent age-related comorbidities [9].
In our previous population-based study performed in a province of North Italy with high HIV prevalence, HIV infection ranked third among chronic diseases in order of total cost per patient to the National Health Service, with a mean cost of 9 894€ in 2007 (ranging from 8 104€ for HIV–infected patients without comorbidities to 12 013€ for HIV infection plus cancer) [10]. However, an update of the estimates of cost-of-care of HIV+ subjects is needed because of recent changes of HIV epidemiologic pattern and guidelines of treatment, which have moved toward treating HIV+ patients earlier in the course of disease and have added newer, more effective and tolerated but also more expensive drugs [11].
The aim of this population-based study was to investigate the burden of chronic diseases and the direct health costs and resource allocation for HIV+ subjects compared to the general population living in the Brescia Local Health Authority (LHA) over a 12-year period, from 2003 to 2014.
Methods
Setting
This study was conducted in the Brescia Province, located in Lombardy Region (northern Italy) in the period 2003–2014.
The Spedali Civili General Hospital in Brescia is one of the largest public hospitals in Italy, and is also the reference hospital for the local School of Medicine, University of Brescia (University Hospital). It includes the only tertiary, referral center of infectious diseases and HIV of the area. In Italy, the National Health Service (NHS) provides universal coverage and is structured on three organizational levels: the central (the Ministry of Health), regional and local levels (Local Health Agency. LHA). In Italy, hospital service providers are paid on a fee-for-service basis, which is directly related to a system of Diagnosis-Related Groups (DRGs) [12]. Primary care and other out-patient services are based on a co-payment system for drugs, laboratory tests and any services provided to patients affected by chronic diseases. However, these services are fee-exempted for HIV+ subjects.
The study protocol was approved by the provincial Ethical Review Board. Written informed consent was obtained by all the patients enrolled.
Population
We included in the analysis all residents in Brescia LHA registered in the Regional Health Service from 2003 to 2014. Non-documented migrants and non-EU citizens were excluded, as their access to care and utilization of health resources cannot be properly assessed as they can only access to emergency treatment under semi-anonymous condition.
HIV infection was identified using the following two sources, as previously described [10]:
-
Brescia LHA electronic database. HIV diagnosis was based on HIV-related opportunistic illness requiring hospital admission (ICD9 = 042 or V08 diagnoses), receiving HIV drugs prescription or HIV reimbursement code assigned by the general practitioner or a specialist.
-
Clinical charts and electronic databases of the Department of Infectious and Tropical Diseases, University of Brescia and Brescia Spedali Civili General Hospital. HIV diagnosis was based on positive HIV-1 or HIV-2-antibody test or positive HIV RNA.
For each year, we analyzed: a) HIV+ prevalent cases including subjects with HIV diagnosis who were present in the Brescia LHA database, independently of the year of HIV diagnosis; and b) HIV+ incident cases including subjects with HIV diagnosis in that year.
The Brescia local health agency database
The Brescia Local Health Agency database (BLHADB) is a comprehensive and integrated information system including several databases tracking and listing all the health services provided by the NHS for each individual of the resident population [10].
Prescription of specific drugs is monitored for each individual by the BLHADB using the Anatomic and Therapeutic Chemical Classification (ATC) [13]. Each individual’s consumption of drugs is converted into a total number of daily defined doses (DDDs), according to the World Health Organization Collaborating Centre for Drug Statistics and Methodology [13]. Drug consumption data presented in DDDs provide a rough estimate of consumption and not an exact picture of each patient’s actual use. DDDs provide a fixed unit of measurement independent of price and formulation that enable to assess trends in drug consumption and to perform comparisons between population groups.
In this analysis we identified 10 families of chronic diseases using a set of ICD9-CM codes (see Additional file 1: Table S1). Each subject was considered to have a chronic disease if he had had Access to Continuity of Care (ACC) for one or more chronic diseases of interest collected in the BLHADB, according to at least one of the following criteria:
-
receiving in-hospital or out-patient services with an ICD9-CM code for a chronic disease;
-
receiving drugs for chronic diseases above a predefined DDD threshold (e.g. >10 % DDD of insulin or >30 % DDD of oral anti-diabetic drugs to define diabetes);
-
having a chronic disease reimbursement code assigned by the general practitioner or a specialist;
-
being admitted to a residential care or psychiatric facility.
ACC for chronic diseases has therefore been considered a proxy for disease prevalence.
Outcomes and covariates
Information on vital status and date and cause of death were obtained from a record-linkage with the LHA Mortality Registry, based on each individual’s national registration code.
For each year of follow-up, we retrieved the presence of chronic diseases from BLHADB. The chronic diseases of interest evaluated were the following: cardiovascular diseases, liver diseases, dyslipidemia, diabetes, cancer, esophagus gastric duodenum diseases, neuropathies, severe psychiatric disorders, bronco-pneumopathy and kidney failure.
HIV infected persons who were at any time on antiretroviral treatment during the year were classified as ‘on antiretroviral treatment’ according to either hospital or LHA drug databases.
We evaluated the direct costs for each HIV+ subject, calculated as the sum of inpatient hospital costs and out-patients costs. Inpatient hospital costs (for both in-patient and day-care admissions) were based on DRG system as previously described [10]. Costs of out-patient consultations and examinations (laboratory and clinical imaging) were calculated based on the official standard costs assigned by the Italian Ministry of Health. All costs were annualized and expressed in nominal terms for the year in which they were incurred. Indirect Costs were not evaluated.
For patients followed by University Hospital we also retrieved CD4+ cell count at HIV diagnosis.
Statistical analysis
HIV incidence and prevalence rates were calculated using incident and prevalent cases as numerators, respectively, and population living in the Brescia LHA during the period as denominator. Annual mean change was calculated using multivariate Poisson regression adjusted for age and gender.
We calculated the prevalence of chronic diseases in 3 years periods across the follow-up. To evaluate the temporal trend of risk of having a chronic disease, we performed an age-and gender-adjusted Poisson regression model for each chronic disease considered in this study. Results were expressed in terms of percentage of annual mean change of risk ([risk ratio-1]*100).
Prevalence of, and mortality for chronic diseases in HIV+ subjects were compared with those observed in the LHA general population using indirect standardization. Standardized prevalence ratios (SPRs) and standardized mortality ratios (SMRs) were computed adjusting for age and gender. The SPRs and SMRs and their 95 % confidence intervals (95 % CIs) were calculated using the Byar’s approximation of Poisson model. The SPRs were calculated for each chronic disease and for at least one, for each 3 year calendar period. The SMRs were also calculated for specific causes of death (HIV/AIDS, liver disease, suicide and cancer).
Association of chronic diseases, age, gender, period of follow-up and CD4+ cell count at baseline with per capita cost was evaluated by using multivariate regression models with per capita cost as the dependent variable with a bootstrap technique (1000 replications).
All statistical tests were two-sided, assumed a level of significance of 0.05 and were performed using Stata 12 software (Stata Statistics/Data Analysis 12.0-Stata Corporation, College Station, TX, USA).
Results
Characteristics of the HIV-infected population in the BLHA DB
From 2003 to 2014, a total of 4 621 subjects were identified as receiving care for HIV infection and included in this study. The main characteristics of the HIV-infected population are shown in Table 1. The number of HIV+ subjects increased from 2 302 in 2003 to 3 594 in 2014 with an increase in prevalence from 220 per 100 000 person-years in 2003 to 307 per 100 000 in 2014 (annual mean change +2.5 %, p < 0.001). We observed a decrease of HIV incidence rate from 16.1 to 10.8 per 100 000 person-years, (annual mean change − 4.5 %, p < 0.001), and of the overall mortality rate from 25.6 to 13.4 per 1000 HIV+ subjects, (annual mean change − 8.7 %, p < 0.001), with 542 deaths in the period (71 deaths for liver disease, 70 for cancer and 19 for suicide).
Among all HIV+ cases, the mean age increased from 40.1 years in 2003 to 47.8 years in 2014, so as prevalence of non-Italian citizens (from 7.0 % to 13.4 %) and of subjects on ART treatment (from 67.3 % to 82.5 %) (p < 0.001 for each variable). Considering only the new HIV+ cases, the mean age was stable around 40 years, but the proportion of females decreased over time (from 30.4 % to 21.4 %).
The distribution of CD4+ cell count at baseline in new HIV+ cases is shown in Table 2. About half of the patients (54 %) with newly diagnosed HIV infection had a late diagnosis (CD4+ cell count < 350 mm3) in the whole period without substantial change over time (p > 0.1).
Prevalence of chronic diseases
The prevalence of chronic diseases in HIV+ subjects according to observation period is shown in Table 3. The prevalence of at least one chronic disease decreased from 33.9 % in 2003 to 29.8 % in 2014 (annual mean change after adjustment for age and gender − 0.7 %; p < 0.001). Considering chronic diseases separately, we observed statistically significant trends, adjusting for age and gender of increasing of prevalence of dyslipidemia (annual mean change +5.5), diabetes (+1.6 %), and gastrointestinal diseases (+5.7 %) and decreasing prevalence of liver diseases (−4.8 %) and chronic respiratory diseases (−5.6 %). The crude prevalence of cardio-cerebrovascular diseases increased over time from 13.6 % in 2003 to 20.7 % in 2014 but this trend was not significant when adjusting for age and sex.
Comparison with the Brescia LHA general population
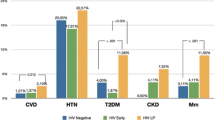
Figure 1 shows SPRs for chronic diseases using Brescia LHA population as the reference. The prevalence of any chronic disease was higher in HIV+ subjects than the general population, with total SPRs ranging from 1.15 to 6.18. However, SPRs decreased for all chronic disease except for dyslipidemia over time.
Standardized prevalence ratios (SPRs) and their 95 % confidence intervals (95 % CIs) of chronic diseases using Local Health Authority general population as reference. The filled segments of the horizontal bars represent the upper limit of the 95 % CI of the SPRs, whereas the open segments represent the lower limit
HIV+ subjects had a higher mortality than the LHA general population in the period, showing SMR of 5.94 (95 % CI 6.47–7.03). The SMR for all causes showed a steady decrease from 9.77 (95 % CI 11.53–13.53) in 2003–2005 to 3.43 (95 % CI 4.15–4.96) in 2012–2014. The mortality rates for liver disease, suicide and cancer were higher in HIV+ subjects than the LHA general population with SMRs of 5.65 (95 % CI 11.08–13.97), 3.55 (95 %, CI 5.90–9.21) and 1.60 (95 %, CI 2.06–2.60), respectively.
Resource utilization and costs
The total health care cost for HIV+ subjects has increased substantially, from a mean of 28.5 million€ per year in 2007 to 36.5 million€ per year in 2014 (+22 %). The overall cost for public health care of subjects with chronic diseases in the Brescia LHA general population in 2014 are shown in Additional file 1: Table S2. HIV infection ranked as the third most costly chronic disease in the Brescia LHA in 2014.
Per capita health care costs by 3 years-time periods are shown in Table 4. Per capita costs increased from 8 271€ in 2003–05 to 10 945€ in 2009–11 (+32 %) with a slight decrease in 2012–14 (+ 25 % from the first to the last interval). The most important item of expenditure was ART, that increased from 5 079€ (61.4 % of the total per capita cost) in 2003–2005 to 7 562€ (72.9 %) in 2012–2014 (+ 49 %). Also in new HIV+ cases, the ART cost increased over time from 2 522€ (31.6 % of the total per capita cost) in 2003–2005 to 3 496€ (35.9 %) in 2012–2014 (+39 %). Of interest, in-patient costs decreased substantially (−28 %) in HIV+ subjects on ART, over the study period. However, in new HIV+ cases the most costly item of expenditure was in-hospital cost that was stable over time.
We also evaluated the association between, age, gender, period of follow-up, CD4+ cell count at baseline and chronic diseases with per capita cost using multivariate regression models (Table 5). The per capita cost was positively associated with age (+36€ every year of age), years of follow-up and CD4+ cell count at baseline (+2 452€ for subjects with CD4+ cell count <200 mm3 at baseline respect to subjects with CD4+ cell count ≥ 500 mm3) and the presence of chronic diseases. In particular, we observed an increase of 3 700€ for subjects with, compared to those without, at least one chronic disease. Kidney failure, psychiatric diseases and cancer were the most expensive comorbidities, with an increase of per capita cost of 13 665€, 8 172€ and 7 557€, respectively.
Discussion
This population-based study carried out in a Health Care District of North Italy is an extension of a previously published assessment of HIV-infection -related health care costs in 2003–2007 up to 2014 [10].
The prevalence of HIV infection increased from 220 to 307 per 100 000 person-years (+2.5 % annual mean change) while incidence decreased from 16 to 11 per 100 000 person-years (-4.5 % annual mean change) and mortality decreased from 25.6 to 13.4 per 1000 person-years (−8.7 % annual mean change). Concomitantly with aging of the cohort of HIV-infected patients, the prevalence of most chronic diseases increased across time and was higher than that of LHA general population. However, the observed to expected ratios (SPRs) in HIV+ subjects decreased over time for each chronic disease except dyslipidemia. Average per capita total cost of HIV infection increased from 2003 to 2014 (+25 %) mainly due to cost for ART (+49 %). Immunodeficiency level at the time of HIV diagnosis had an important weight on healthcare spending: the per capita cost for patients with CD4+cell count <200 mm3 was 2 106€ more than patients with CD4+cell count >500 mm3.
There is mounting evidence that an increase of use on HIV healthcare services leads to a reduction in both mortality and HIV transmission and therefore to reduction of HIV incidence [14–16]. Accordingly, we found an increase of HIV management costs and HIV prevalence and concurrently a decrease of incidence and mortality of HIV-infected patients over the period 2003–14. These findings appear to confirm that spending on public health for HIV management improves patients’ survival and prevents new HIV infections.
However, in spite of the increase of total costs for HIV infection care in the period (+25 % during the period), when ranking total costs for National Health Service of all chronic diseases in the Brescia LHA, HIV infection maintained the third rank in order of cost per patient since 2007 [10] to 2014 (present study).
A recent systematic review about economic impact of HIV infection in five European countries showed a high degree of inter-country variability, the HIV+ patients cost ranging from 6 399€ in Italy and 11 638€ in Spain to 25 339€ in UK and 32 109€ in Germany, ART being the main component of total HIV health cost [17].
In the same line, the increase of total cost for HIV in our study was entirely attributable to increase in ART cost, mainly due to the proportion of patients on ART increased +23 % over the period and because of introduction of new antiretroviral drugs approved from 2005, including new drugs within conventional classes as well as novel drug classes. These newer antiretroviral drugs are more effective in treatment of drug resistant HIV but, on the other hand, are also more expensive than those used previously, causing substantial incremental costs [5, 6].
The cost of ART for HIV+ incident cases was around half of that for all HIV+ patient across the period. The main reasons for this is that cheaper drugs are more commonly used in the first-line regimen than in the following ART lines [18]. Indeed, various authors [6, 19] have shown that the most powerful determinant of ART cost was the line of ART. In our cohort, more than 70 % of patients had used at least four lines of ART and 92 % of patients on ART had plasmatic HIV RNA <37cp/ml. (Data not shown in table). Furthermore, the complexity of HIV+ patients plays an important role in cost of ART including difficulty of achieving virological suppression in ART experienced patients, toxicities, comorbidities and drug-drug interaction thus contributing to the differences in ART cost among centers also inside the same country [6, 20].
In our study however, per capita costs for HIV+ patients increased from 2003 to 2011 and decreased moderately afterwards. This is probably due to the local public health policy. Indeed, in the context of present austerity policies, from 2011 the Lombardy Government has forced health services to increase efficiency of resources allocation and treatment appropriateness [Therapeutic and diagnostic path-PDT- [21]]. As a consequence, HIV- specialists are urged to the “economic efficacy principle” for choosing equally efficient but lower-cost alternative medication and generic drugs whenever available, according to PDT of the Lombardy Health Service [21].
The increase of life expectancy of HIV+ patients in the last decades due to efficacy of ART has determined patients’ aging with consequent increase of comorbidities and related health expenditure [9, 22]. HIV care involves taking ART and having regular check-ups by healthcare providers with opportunity for early diagnosis of comorbidities. Notwithstanding, HIV+ patients with comorbidities have poorer health outcomes than those without comorbidities [23]. The prevalence of chronic diseases was higher in HIV+ patients than in the LHA general population, in agreement with other studies showing that HIV+ patients have an early aging with a prevalence of multi-comorbidities approximately equivalent to that observed in the general population of 10–15 years older [24, 25]. The prevalence of many “non-AIDS” chronic diseases is inversely related to CD4+ cell count. This includes liver diseases [26], non-AIDS malignancies [27, 28] and renal diseases [29]. Whereas, other diseases, particularly cardio-cerebrovascular diseases do not seem to follow this pattern [30].
We observed a significant decreasing trend of the age and gender adjusted prevalence of at least one chronic disease adjusted for age and gender in HIV+ subjects over time (annual mean change − 0.7 %; p = 0.006). One possible explanation for this is that continuous treatment of HIV+ subjects in the period has determined an increase of CD4+ cell levels with consequent decreasing comorbidity, in agreement with the decrease of non-AIDS morbidity concurrently with CD4+ cell level increase in some HIV+ cohorts [2–4].
Although prevalence of all chronic diseases in our HIV+ patients was higher than the general population, the observed to expected ratio (SPR) for HIV+ subjects reduced in the period, especially for liver diseases. At present, HCV infection is the most common cause of chronic liver diseases in both HIV+ patients and the general population in Italy [31–33]. HIV/HCV coinfected subjects are less frequently treated for HCV than HCV-monoinfected ones due to higher difficulties to treat the formers due to immunodeficiency, drug-drug interaction, low tolerability, concomitant intravenous drug use or presence of psychiatric diseases. Furthermore, in Italy HIV+ subjects have a HIV reimbursement code allowing them to have whole health care totally free, including HCV management and cure. Therefore, HIV-HCV coinfected subjects do not ask for HCV reimbursement code, and, as a consequence, they are not detected by the LHA health database.
CD4+ cell count at baseline was inversely related with per capita cost and this cost was particularly high in HIV+ subjects at advanced immunodeficiency stage, in agreement with previous studies [6, 19, 34–36]. The Brescia LHA health status database is a large, population-based comprehensive and integrated information system which has the usual limits of currently available large databases of health data coming from various sources, leading to a certain degree of imprecision in estimating the frequency of chronic diseases and the cost of care of HIV+ subjects. Anyway, a validation study and various analyses have shown a fairly high quality of the database, especially as regards the most common chronic diseases including HIV, cardiovascular diseases, cancer and diabetes [37, 38].
As regards external validity, i.e. generalizability, the HIV patients living in the Brescia LHA are substantially similar to the national ones, in spite of a higher HIV incidence in Brescia than in the whole country (10.8/100000 vs 6.1/100 000 inhabitants). In fact, the HIV cases with first diagnosis in 2014 are similar to those described in the National reports in the same year as regards demographic characteristics (79 % vs 80 % males, mean age 38.8 vs 39 years, 23.8 % vs 27 % non-Italian citizens) [39]. Likewise, as regards clinical aspects, the proportion of HIV incident cases with CD4 level <200 cell / mm3 in our cohort was similar to the national one (33 % vs 35 %) [39].
Another possible limitation is that inflation has not been accounted for. However, the official mean inflation yearly rate in Italy in the period 2003–2104 has been 1.9 % (range: 0.2 % − 3.2 %) [40], hardly impacting on our data and results.
This study has some strengths, too. First, it is population-based allowing to estimate incidence, prevalence and mortality rates for all HIV+ subjects and all residents living in the area and therefore avoiding selection bias. Separate economic analyses could be performed for incident and prevalent HIV+ cases whereas most studies considered all HIV+ cases together. The relatively long observation time (12 years) allowed us to assess the temporal trend of the epidemiological pattern, burden of chronic diseases, and overall and specific costs of HIV+ subjects. Finally, all HIV+ patients have been cured in the unique Infectious Diseases Unit in the area, allowing the collection of clinical data and matching them with the LHA data base.
Conclusions
Our findings suggest that spending on public health for HIV care can improve prognosis of HIV-infected patients, reduce transmission of HIV infection and reduce the global burden of chronic diseases, leading to a reduction of HIV global cost in the medium-long time.
Abbreviations
- ACC:
-
Acces to continuity of care
- ART:
-
Antiretroviral therapy
- BLHDB:
-
Brescia local health agency data base
- DRGs:
-
Diagnosis related groups
- LHA:
-
Local health agency
- NHS:
-
National health service
- SMR:
-
Standardized mortality ratio
- SPR:
-
Standardized prevalence ratio
References
Raffetti E, Albini L, Gotti D, et al. Cancer incidence and mortality for all causes in HIV-infected patients over a quarter century: a multicentre cohort study. BMC Public Health. 2015;15:235. doi:10.1186/s12889-015-1565-0.
Helleberg M, Kronborg G, Larsen CS, et al. Causes of death among Danish HIV patients compared with population controls in the period 1995-2008. Infection. 2012;40(6):627–34.
Grinsztejn B, Luz PM, Pacheco AG, et al. Changing mortality profile among HIV-infected patients in Rio de Janeiro, Brazil: shifting from AIDS to non-AIDS related conditions in the HAART era. PLoS One. 2013;8(4), e59768.
Smith CJ, Ryom L, Weber R, et al. Trends in underlying causes of death in people with HIV from 1999 to 2011 (D:A:D): a multicohort collaboration. Lancet. 2014;384:241–8.
Bayoumi AM, Barnett PG, Joyce VR, et al. Cost-effectiveness of newer antiretroviral drugs in treatment-experienced patients with multidrug-resistant HIV disease. J Acquir Immune Defic Syndr. 2013;64(4):382–91.
Tontodonati M, Cenderello G, Celesia BM, et al. Cost of HAART in Italy: multicentric evaluation and determinants from a large HIV outpatient cohort. Clinicoecon Outcomes Res. 2014;7:27–35. doi:10.2147/CEOR.S69183. eCollection 2015.
Antiretroviral Therapy Cohort Collaboration. Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet. 2008;372:293–9.
Samji H, Cescon A, Hogg RS, et al. Closing the gap: increases in life expectancy among treated HIV-positive individuals in the United States and Canada. PLoS ONE. 2013;8(12), e81355.
Guaraldi G, Zona S, Menozzi M, et al. Cost of noninfectious comorbidities in patients with HIV. Clinicoecon Outcomes Res. 2013;5:481–8. doi:10.2147/CEOR.S40607.
Magoni M, Scarcella C, Vassallo F, et al. The evolving burden of HIV infection compared with other chronic diseases in northern Italy. HIV Med. 2011;12(3):129–37. doi:10.1111/j.1468-1293.2010.00861.x.
HIV/AIDS Italian Expert Panel. (2015). Linee Guida Italiane sull’utilizzo dei farmaci antiretrovirali e sulla gestione diagnostico-clinica delle persone con infezione da HIV-1. Available at: http://www.salute.gov.it/imgs/C_17_pubblicazioni_2442_allegato.pdf. (Accessed 10 Feb 2016).
Lombardy Region. Social and Health Care Plan. No 937/2010. Milan: Lombardy Region; 2010. Italian. Available at: http://www.sanita.regione.lombardia.it/shared/ccurl/956/366/DGRregole_e_allegati.zip. (Accessed 10 Feb 2016).
Guidelines for ATC classification and DDD assignment, 5th edition. WHO Collaborating Centre for Drug Statistic Methodology, Oslo 2002. Available at www.whocc.no/atcddd. (Accessed 28 Feb 2016).
Goldman DP, Juday T, Seekins D, Linthicum MT, Romley JA. Early HIV treatment in the United States prevented nearly 13,500 infections per year during 1996-2009. Health Aff (Millwood). 2014;33(3):362–9. doi:10.1377/hlthaff.2013.0830.
Dieffenbach CW, Fauci AS. Thirty years of HIV and AIDS: future challenges and opportunities. Ann Intern Med. 2011;154:766–71.
Attia S, Egger M, Müller M, Zwahlen M, Low N. Sexual transmission of HIV according to viral load and antiretroviral therapy: systematic review and meta-analysis. AIDS. 2009;23(11):1397–404. doi:10.1097/QAD.0b013e32832b7dca.
Trapero-Bertran M, Oliva-Moreno J. Economic impact of HIV/AIDS: a systematic review in five European countries. Health Econ Rev. 2014;4(1):15. doi:10.1186/s13561-014-0015-5. Epub 2014 Sep 16.
Phillips AN, Cambiano V, Miners A, et al. Effectiveness and cost-effectiveness of potential responses to future high levels of transmitted HIV drug resistance in antiretroviral drug-naive populations beginning treatment: modelling study and economic analysis. Lancet HIV. 2014;1(2):e85–93. doi:10.1016/S2352-3018(14)70021-9. Epub 2014 Oct 14.
Mostardt S, Hanhoff N, Wasem J, et al. Cost of HIV and determinants of health care costs in HIV-positive patients in Germany: results of the DAGNÄ K3A Study. Eur J Health Econ. 2013;14(5):799–808. doi:10.1007/s10198-012-0425-4. Epub 2012 Sep 19.
Barnett PG, Chow A, Joyce VR, et al. Effect of management strategies and clinical status on costs of care for advanced HIV. Am J Manag Care. 2014;20(5):e129–37.
Lombardy Region. Approvazione del documento avente per oggetto Percorso Diagnostico Terapeutico (PDT) per il paziente affetto da malattia HIV/AIDS [Therapeutic and diagnostic path (PDT) for the patient with HIV/AIDS disease]. Decree no 7485, August 5, 2011. Milan: Lombardy Region; 2012. Italian. Available at:http://www.sanita.regione.lombardia.it/cs/Satellite?c=Page&childpagename=DG_Sanita/Page/NormativaDetail&pagename=DG_SANWrapper&cid=1213275902673&keyid=3520. (Accessed 10 Feb 2016).
Krentz HB, Gill MJ. Increased costs of HIV care associated with aging in an HIV-infected population. HIV Med. 2015;16(1):38–47. doi:10.1111/hiv.12176. Epub 2014 Aug 8.
Braithwaite RS, Justice AC, Chang CC, et al. Estimating the proportion of patients infected with HIV who will die of comorbid diseases. Am J Med. 2005;118(8):890–8.
Guaraldi G, Orlando G, Zona S, et al. Premature age-related comorbidities among HIV-infected persons compared with the general population. Clin Infect Dis. 2011;53(11):1120–6. doi:10.1093/cid/cir627. Epub 2011 Oct 13.
Deeks SG. HIV infection, inflammation, immunosenescence, and aging. Annu Rev Med. 2011;62:141–55.
Towner WJ, Xu L, Leyden WA, et al. The effect of HIV infection, immunodeficiency, and antiretroviral therapy on the risk of hepatic dysfunction. J Acquir Immune Defic Syndr. 2012;60(3):321–7.
Reekie J, Kosa C, Engsig F, et al. Relationship between current level of immunodeficiency and non-acquired immunodeficiency syndrome-defining malignancies. Cancer. 2010;116(22):5306–15.
Cutrell J, Bedimo R. Non-AIDS-defining cancers among HIV-infected patients. Curr HIV/AIDS Rep. 2013;10(3):207–16.
Mocroft A, Lundgren JD, Ross M, et al. Cumulative and current exposure to potentially nephrotoxic antiretrovirals and development of chronic kidney disease in HIV-positive individuals with a normal baseline estimated glomerular filtration rate: a prospective international cohort study. Lancet HIV. 2016;3(1):e23–32. doi:10.1016/S2352-3018(15)00211-8. Epub 2015 Nov 17.
Longenecker CT, Triant VA. Initiation of antiretroviral therapy at high CD4 cell counts: does it reduce the risk of cardiovascular disease? Curr Opin HIV AIDS. 2014;9(1):54–62.
Torti C, Raffetti E, Donato F, et al. Cohort Profile: Standardized Management of Antiretroviral Therapy Cohort (MASTER Cohort). Int J Epidemiol 2015 Oct 7. [Epub ahead of print] No abstract available. PMID: 26445966.
Fedeli U, Schievano E, Lisiero M, Avossa F, Mastrangelo G, Saugo M. Descriptive epidemiology of chronic liver disease in northeastern Italy: an analysis of multiple causes of death. Popul Health Metr. 2013;11(1):20. doi:10.1186/1478-7954-11-20.
Sagnelli E, Stroffolini T, Mele A, et al. The importance of HCV on the burden of chronic liver disease in Italy: a multicenter prevalence study of 9,997 cases. J Med Virol. 2005;75(4):522–7.
Fleishman JA, Yehia BR, Moore RD, Gebo KA. HIV Research Network. The economic burden of late entry into medical care for patients with HIV infection. Med Care. 2010;48(12):1071–9. doi:10.1097/MLR.0b013e3181f81c4a.
Krentz HB, Gill MJ. The Direct Medical Costs of Late Presentation (<350/mm) of HIV Infection over a 15-Year Period. AIDS Res Treat. 2012;2012:757135. doi:10.1155/2012/757135. Epub 2011 Aug 29.
Rizzardini G, Restelli U, Bonfanti P, et al. Cost of human immunodeficiency virus infection in Italy, 2007–2009: effective and expensive, are the new drugs worthwhile? Clinicoecon Outcomes Res. 2012;4:245–52.
Calabresi A, Ferraresi A, Festa A, et al. Incidence of AIDS-defining cancers and virus-related and non-virus-related non-AIDS-defining cancers among HIV-infected patients compared with the general population in a large health district of Northern Italy, 1999–2009. HIV Med. 2013;14(8):481–90. doi:10.1111/hiv.12034. Epub 2013 Apr 7.
Lonati F, Scarcella C, Indelicato A, et al. Brescia Local Health Autority Population Database: a method based on current data for monitoring chronic diseases and management. Epidemiol Prev. 2008;32(3):137–44. Italian.
Notiziari ISS che riportano i dati italiani su HIV/AIDS, http://www.iss.it/ccoa/?lang=1&id=2&tipo=5. (Accessed 26 Aug 2016).
Average Annual Inflation Rate, http://www.re.camcom.gov.it/Sezione.jsp?idSezione=753. (Accessed 17 Apr 2016).
Funding
This publication and the study on which it reports have been funded by Gilead Sciences Europe Ltd with no involvement by Gilead Sciences Europe Ltd in the analysis of the data or preparation of the publication.
Availability of data and material
For ethical and legal restriction we can’t upload a minimal data set. The data are available upon request, the interested researchers could contact Prof Francesco Castelli (francesco.castelli@unibs.it).
Authors’ contributions
EQR, FC, MM, ER, CS and FD contributed to the study design. EQR, FC and GP contributed to the acquisition of data. ER and MM performed statistical analysis and compiled the tables and figures. EQR and FD wrote the paper. All authors participated to the interpretation of the data, read, revised critically for important intellectual content and approved the final version of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Written informed consent was obtained by all the patients enrolled. The study was approved by the Comitato etico provinciale della Provincia di Brescia.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
Supplementary Materials. Table S1 and Table S2. (DOC 81 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Quiros-Roldan, E., Magoni, M., Raffetti, E. et al. The burden of chronic diseases and cost-of-care in subjects with HIV infection in a Health District of Northern Italy over a 12-year period compared to that of the general population. BMC Public Health 16, 1146 (2016). https://doi.org/10.1186/s12889-016-3804-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-016-3804-4