Abstract
Background
Childhood obesity has become a public health concern in many countries. In Southern China, the prevalence of childhood obesity increased from 6.2 to 7.5 % between 2007 and 2011. This study aimed to report the current prevalence of overweight and obesity, analyzed the early life and behavioral determinants of obesity, and investigated the weight-loss practices among Chinese children in Guangzhou.
Methods
Three thousand seven hundred sixty-six primary school students aged 7–12 years were recruited in Guangzhou, China in 2013. Questionnaires were used to assess (1) early life factors: birth weight, delivery mode, gestational age and feeding patterns; (2) behavioral factors: dietary intake, eating speed, sedentary time, physical activities and sleep duration; and (3) weight-loss practices: improving diet, increasing exercise, taking weight-loss drugs and undergoing a diet. The criteria of Working Group of Obesity in China were applied to classify overweight and obesity based on measured weight and height. Multivariable logistic regression analyses were performed to examine the determinants of overweight/obesity and adoption of weight-loss practices.
Results
The prevalence of childhood overweight and obesity were 11.2 and 10.0 %, respectively. High birth weight (≥4.0 kg versus 2.5 ~ 4.0 kg, odd ratio [OR]: 2.34; 95 % confidence interval [CI]: 1.53–3.58), sugar-sweetened beverages (SSBs) intake (OR: 1.39; 95 % CI: 1.05–1.85), vegetable intake (OR: 1.12; 95 % CI: 1.01–1.24), and doing homework (OR: 1.24; 95 % CI: 1.08–1.43) were positively associated with obesity. Eating speed faster than peers was positively associated with obesity and yielded the highest OR (versus “as fast as peers”, OR: 3.18; 95 % CI: 2.28–4.44). Approximately 57, 81 and 87 % of normal-weight, overweight and obese children, respectively, reported weight-loss practices. Self-perception of weight status presented as the strongest determinant for weight-loss practices.
Conclusions
The prevalence of overweight and obesity were high in Chinese children in Guangzhou, and both were higher than previous level in 2011. Further research should address the unhealthy dietary (e.g. SSBs intake, fast eating speed) and sedentary behaviors (e.g. doing homework) of these children. Moreover, an accurate perception of body weight can help promote the adoption of weight-loss practices in overweight and obese children.
Similar content being viewed by others
Background
Childhood obesity has become a public health concern in many countries [1]. Worldwide, the prevalence of overweight and obesity combined rose by 47.1 % for children between 1980 and 2013 [1]. In 2013, approximately 23.8 and 22.6 % of boys and girls in developed countries were overweight or obese, while 12.9 and 13.4 % were observed in developing countries [1]. With rapid economic development over the past decades, China has also witnessed an increase in childhood obesity [2, 3]. In 2010, it was estimated that 9.9 and 5.1 % of school-age children and adolescents in China were overweight and obese, respectively, which amounted to approximately 30.4 million individuals [4]. Moreover, the prevalence of obesity in some areas of China has been catching up with that in developed countries. For example, the prevalence of obesity in Shandong Province in 2010 reached 15.8 and 7.1 % in boys and girls, respectively [5].
Childhood obesity is associated with an increased risk of cardiovascular disease and type 2 diabetes mellitus [6] and may persist into adulthood [7]. Given its high prevalence and risk, childhood obesity requires immediate and effective interventions. Health officials must continue to monitor and provide insights into the underlying modifiable determinants of childhood obesity. Previous studies suggested that the determinants of obesity in children varied across different regions, ethnicities and populations [8–16]. In China, several studies reported that behavioral factors such as dietary intake [8, 11, 15], fast eating speed [15], sedentary behaviors [8, 11, 13, 16], physical inactivity [8], and short sleep time [11, 13] were closely associated with obesity risk in children. In recent years, an increasing number of studies have focused on the fetal and early life origins of subsequent obesity (e.g., birth weight, delivery mode and breastfeeding pattern). For instance, a meta-analysis revealed that high birth weight (>4.0 kg) was associated with increased risk of obesity from childhood to early adulthood [17]. A Chinese birth cohort study demonstrated that caesarean delivery modestly increased overweight risk at 4 to 7 years of age compared with vaginal delivery [18]. A longitudinal study suggested that breastfeeding was associated with decreased risk of overweight and obesity among schoolchildren in Japan [19]. In China, the early life factors associated with obesity were mainly studied among younger-aged children [18, 20, 21], but were less understood in primary school children.
Guangzhou is one of the most developed cities in southern China, where the prevalence of obesity in children (aged 7–18 years) increased from 6.0 % in 2007 to 6.6 % in 2011 [22]. Another study also reported that the prevalence of obesity among 7–12-year-old children in Guangzhou increased from 6.2 to 7.5 % between 2007 and 2011 [23]. Further studies are needed to monitor this trend. Previous studies demonstrated that the prevalence of overweight and obesity among children in Guangzhou were lower than other large coastal cities in China [4, 24]. The climate and lifestyle habits in southern China are markedly different from that in other regions. For example, due to the warm and humid climate and cultural difference, most people in this area tend to consume less greasy or strongly flavored food. So the risk factors of childhood obesity may be quite different from those of other areas. However, limited data on the determinants of childhood overweight or obesity has been obtained from this area. Research focusing on the determinants of childhood obesity in this area can provide guidance for effective obesity prevention and intervention programs. Another question is how children would be engaged in weight-loss practices and what factors would be related to their adoption. So far, the picture of weight-loss practices (e.g., exercising to lose weight and going on a diet) among Chinese primary school children is unknown. Our study adds to previous literature by investigating children’s engagement in weight-loss practices, which may contribute to prevention of unhealthy weight-loss practices in primary school children. Therefore, the present study aims to assess the current extent of the obesity epidemic, investigate the early life and behavioral factors influencing such phenomenon, and analyze the weight-loss practices of primary school children in Guangzhou, China.
Methods
Study design and data source
This cross-sectional study is the baseline survey of a school-based obesity intervention project that targeted Chinese children and adolescents (“Development and Application of Student Critical Diseases Prevention and Control Technology and Related Standards”) (Trial registration: January 22, 2015; Registration number: NCT02343588) [25, 26]. The project was approved by the Ethical Committee of Peking University. All participating students and their parents voluntarily signed informed consent forms.
Sampling method and participant recruitment
With multistage random cluster sampling method, the participants were recruited in urban areas of Guangzhou. Firstly, we selected four urban districts from ten districts of Guangzhou using judgment sampling method. Secondly, one or two primary schools were randomly selected from each of the four districts. Probability proportional to size sampling method was used in this stage and a total of seven schools were selected. The principals were sent invitation letters, information sheets and presentations that outlined the research details. After the principals’ permission, all students from the second to the fifth grade were invited to participate, excluding those aged below 7 years old or were diagnosed with visceral diseases, abnormal growth and development, physical abnormality or obesity induced by endocrine diseases or drugs. Consent forms for the physical examination and questionnaire survey were given to each student. The children were advised to discuss the research with their parents and then return the consent forms to the school if they and their parents were willing to participate. A total of 4942 students agreed to participate in the study. The response rates were 100 % (7/7) for schools and 78.4 % (4942/6300) for students. Participants who did not take questionnaires (n = 690) or physical examination (n = 473), or had missing information about their age (n = 1), gender (n = 0), or body mass index (BMI) (n = 12) were excluded from the study, leaving 3766 participants in the sample. The study was conducted between September and November 2013.
Questionnaire survey
To ensure that each question was explained similarly to all the participants, the student and parent questionnaires were administered to the whole class during school hours by the same investigators, who were trained postgraduates. A teacher supervised and assisted the survey procedure in each class. Students in grades 4–5 filled out the student questionnaire by themselves in class, whereas students in grades 2–3 answered the student questionnaire under parents’ guidance at home. The parent questionnaire and explanatory cover letters were delivered by children to their parents and returned to the researchers after 3 days. All questionnaires were checked for integrity upon return. The questionnaires with missing values were resubmitted to children or their parents to be filled out again. Children’s birth date in the questionnaire was checked for logicality, which should be between January 2001 and November 2006.
Socio-demographic characteristics and other measures
Socio-demographic information included children’s birth date, gender and only child or not in the student questionnaire, and parents’ educational level, occupation and monthly household income in the parent questionnaire. Parents reported their own current weight (kg) and height (cm) to evaluate weight status. Weight-loss practices were assessed by asking children the four questions: “Have you tried to lose weight in the following ways over the past 3 months? (1) Improving diet (i.e., eating more fruit or vegetable but less high-energy snacks), (2) Increasing exercise, (3) Taking weight-loss drugs, (4) Undergoing a diet (i.e., not eating staple foods like rice or noodles)”. The responses for each behavior were “yes” or “no”. Children’s self-perception of weight status was assessed by asking: “How do you feel about your current weight status?” with the five response options: “very thin”, “rather thin”, “average”, “rather fat” and “very fat”. The responses were categorized into: perceived underweight (“very thin” and “rather thin”), normal weight (“average”) and overweight (“very fat” and “rather fat”).
Early life factors
Parents were asked about the participating child’s birth weight (kg), mode of delivery (vaginal delivery or cesarean delivery), gestational age (week), feeding patterns (breastfeeding or not), and breastfeeding duration (month) in the parent questionnaire.
Behavioral factors
Behavioral factors included 8 items for dietary intake, 1 item for eating speed, 3 items for sedentary time, 3 items for physical activities, and 1 item for sleep duration. Dietary intake included the consumption of fruits, vegetables, meat products, breakfast, sugar-sweetened beverages (SSBs), high-energy snacks (e.g., chocolates and candies), fried food (e.g., fried chicken and fried potatoes), and western fast food (e.g., KFC and McDonald’s). Children reported the frequency (days) and amount (servings) of fruits, vegetables, meat/meat products and SSBs intake over the past 7 days. The average daily intake of single food was estimated as follows: average daily intake = [days × (amount in each of those days)]/7. Eating speed was evaluated by asking: “What do you think about your eating speed compared with peers?” The three response options were “slower than peers”, “as fast as peers” and “faster than peers”.
Sedentary behavior included doing homework, viewing television and using a computer (including playing video games). Children were asked about the average amount of time (hours and minutes) they spent daily on the three behaviors over the past 7 days. Physical activities included vigorous-intensity physical activities (aerobic activities that significantly increase heart rate and breathing, e.g., running, basketball, football and swimming, etc.), moderate-intensity physical activities (aerobic activities that increase heart rate and breathing to some extent, e.g., cycling, table tennis, badminton and calisthenics, etc.), and walking. Children reported the frequency (days) and duration (hours and minutes in each of those days) of these activities over the past 7 days. The average daily time of physical activities were calculated as follows: average daily time = [days × (amount in each of those days)]/7. Sleep duration was assess by asking: “How long do you sleep every day?” with four response options: “<7.0 h”, “7.0 ~ 8.9 h”, “9.0 ~ 11.0 h”, and “>11.0 h”.
Physical examination
Physical examination was conducted 3 days after questionnaire survey. The children underwent a thorough medical examination to ensure that they were free from visceral diseases and abnormal obesity induced by endocrine diseases or drugs. Height (cm) and weight (kg) were measured by a team of trained technicians following a standardized procedure. Height was measured using the portable stadiometer (model TZG, China) (with 0.1 cm precision), with the subjects standing straight and barefoot. Weight was measured using the lever type weight scale (model RGT-140, China) (weighing 120 kg with 0.1 kg precision). The subjects were asked to use the restroom beforehand and stand on the scale wearing only their underwear. Both height and weight were measured twice and averaged. About 5 % of the children would be rechecked for height and weight. If the error exceeds 10 %, all of the students have to be measured again.
BMI was calculated by dividing weight in kilograms by height in meters squared (kg/m2). Children’s overweight and obesity were defined by using the Working Group of Obesity in China (WGOC) [27] criteria, the cut-off points of which are 85th and 95th percentiles of BMI, respectively (Overweight: 85th percentile ≤ BMI < 95th percentile; Obesity: 95th percentile ≤ BMI). Children’s underweight was defined based on the age-gender-specific BMI cutoffs of malnutrition for Chinese children [28]. Parents’ BMI was calculated using their self-reported height and weight. Parental overweight was defined as BMI ≥ 24 kg/m2 to <28 kg/m2, whereas obesity was defined as BMI ≥ 28 kg/m2 in accordance with the criteria for Chinese adults [29].
Statistical analysis
Calculations were conducted using IBM SPSS software version 19.0. Descriptive statistics were used to characterize the study population. Continuous variables were presented as mean ± standard deviation (SD), whereas categorical variables were presented as percentages. For weight status, the figures for “overweight” excluded those for “obese” and the figures for “normal weight” excluded those for “underweight”. Differences of weight status between two items or more were evaluated by Mann-Whitney U tests or Kruskal-Wallis tests, respectively. Multinomial logistic regression analyses were performed to assess the associations of early life and behavioral factors with overweight/obesity. Such association was initially assessed in the crude model. The second set of model (adjusted model) was adjusted for age, gender and other socio-demographic factors (i.e., only child or not, paternal and maternal educational level, paternal and maternal occupation and monthly household income). Differences in the adoption of weight-loss practices among normal-weight, overweight and obese children were evaluated by Pearson Chi-square tests. Binary logistic regression analyses were performed to assess associated factors of the adoption of weight-loss practices among socio-demographic characteristics and children’s perceptions of weight status. Independent variable screening was performed using the enter method. A two-sided P < 0.05 indicated statistical significance.
Results
Of the 3766 children, the mean age was 8.5 (SD 1.2) years old. Almost half of the children were boys (50.5 %) and most were only child (75.3 %). 1567 (42.6 %) fathers and 1352 (36.9 %) mothers had an education level of college or above. And 1362 (37.7 %) fathers and 1337 (37.0 %) mothers were working in commerce and service industry. Nearly a quarter (23.2 %) of children’s family had a monthly household income of below 8000 RMB, whereas 36.7 % refused to disclose their income (Table 1).
On the basis of the WGOC criteria [27], the prevalence of overweight and obesity among the participating children were 11.2 % (14.3 % in boys and 7.9 % in girls) and 10.0 % (13.8 % in boys and 6.0 % in girls), respectively. A higher prevalence of overweight and obesity was observed among older children or boys (P < 0.01). An increased prevalence of overweight and obesity was also observed among children with high birth weight (≥4.0 kg) or delivered by caesarean section (P < 0.05). Regarding the breastfeeding duration, the lowest prevalence of overweight and obesity was found among children who were breastfed for 4.0 ~ 5.9 months, though there was no significant difference of weight status between different breastfeeding duration (P = 0.20). Furthermore, a higher prevalence of overweight and obesity was observed among children who had an overweight or obese father or mother (P < 0.001) (Table 1). Overweight or obese children consumed more meat products, SSBs and fried food per day over the past week and were more likely to have faster eating speed than peers compared with underweight or normal-weight children (P < 0.05). Overweight or obese children also had longer daily time of doing homework and using a computer than their counterparts (P < 0.01). By contrast, no statistical difference was observed among physical activities and sleep duration between different weight status categories (Table 2).
The associations between early life and behavioral factors and overweight/obesity were examined. Among the early life factors, high birth weight (≥4.0 kg versus 2.5 ~ 4.0 kg) was positively associated with obesity (adjusted odd ratio [OR]: 2.34; 95 % confidence interval [CI]: 1.53–3.58). Gestational age < 37 weeks (versus 37 ~ 42 weeks) was positively associated with overweight (adjusted OR: 1.75; 95 % CI: 1.01–3.05) (Table 3). In terms of behavioral factors, SSBs intake was positively associated with overweight (adjusted OR: 1.37; 95 % CI: 1.03–1.83) whereas sleep duration as 9.0 ~ 11.0 h was negatively related to overweight (versus 7.0 ~ 8.9 h, adjusted OR: 0.60; 95 % CI: 0.43–0.84). Meanwhile, vegetable intake, SSBs intake (adjusted OR: 1.39; 95 % CI: 1.05–1.85) and homework time (adjusted OR: 1.24; 95 % CI: 1.08–1.43) were positively associated with obesity. Eating speed faster than peers (versus “as fast as peers”) was significantly positively associated with both overweight and obesity and yielded the highest ORs (adjusted OR: 1.76; 95 % CI: 1.27–2.43 and adjusted OR: 3.18; 95 % CI: 2.28–4.44, respectively). By contrast, eating speed slower than peers (versus “as fast as peers”) showed negative association with overweight and obesity (adjusted OR: 0.55; 95 % CI: 0.36–0.84 and adjusted OR: 0.55; 95 % CI: 0.34–0.91, respectively). Physical activities showed no relation with overweight or obesity (Table 4).
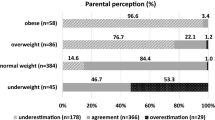
Regarding the adoption of weight-loss practices, there were 40.9, 53.5, 0.7 and 5.9 % children who tried to lose weight through improving diet, increasing exercise, taking weight-loss drugs and undergoing a diet, respectively. Overweight and obese children demonstrated a higher tendency to improve their diet, perform more exercises or undergo a diet than normal-weight children (P < 0.001) (Fig. 1). Among the socio-demographic characteristics and personal weight perception, age was positively associated with adopting any of the four weight-loss practices in all three BMI categories. Normal-weight girls were more likely to adopt weight-loss practice than their counterparts. Personal perceived overweight and obese were strongly positively associated with adopting weight-loss practice in obese children (OR: 4.34; 95 % CI: 1.45–12.98 and OR: 5.55; 95 % CI: 1.35–22.92, respectively) and the total population (Table 5).
Discussion
This study assessed the current prevalence of overweight and obesity among children in Southern China and examined the early life and behavioral factors that influenced such prevalence. The weight-loss practices and the factors associated with their adoption were also investigated.
A relatively high prevalence of overweight (11.2 %) and obesity (10.0 %), which were both higher than that in 2011 (10.5 and 7.5 %, respectively) [23], was observed among the study population. After standardizing based on the age-gender distribution of the population in Ma’s study [23], the standardized prevalence of obesity in our study (8.8 %) was still higher than that in 2011, indicating that the prevalence of childhood obesity has been increasing from 2007 to 2013. A further comparison showed that the prevalence of overweight and obesity in Guangzhou in 2013 were still lower than the average values of other large coastal cities in China (20.7 and 17.8 % in boys and 11.1 and 9.8 % in girls), but exceeded the national level (14.2 and 9.4 % in boys and 7.7 and 5.4 % in girls) in 2010 [4]. The disparity between Guangzhou and other large coastal cities may be attributed to the complex interaction of geographic-climate factors (warm and humid climate in Guangzhou) as well as different appetites (not greasy or strongly flavored) and dietary habits of children (drinking soup before eating) [3]. However, another study indicated that further economic development and lifestyle assimilation may reduce the “south–north gap” [30].
A higher prevalence of overweight or obesity was observed among boys than girls, which was consistent with previous findings in China [3, 13, 14, 31]. Socio-cultural, socio-economic, behavioral, and genetic factors may play important roles in gender disparity of obesity [31]. In Chinese culture, obesity in boys is recognized as strong, whereas Chinese girls prefer a slender shape and are more likely to control their weight compared with boys [31]. Behavioral factors may also contribute to the gender disparity. As presented in our study, boys consumed more fried food, drank more SSBs and were more likely to spent > 2 h per day of screen time (TV and computer) than girls (all P < 0.05), indicating that boys were more likely to engage in unhealthy behaviors. Children with and without siblings showed no difference in their weight status in the present study. A European study [32] revealed that singletons were more likely to be overweight than their peers with siblings when controlling for factors related to childhood overweight. However, the sample in the European study [32] included less than 30 % of singletons, which might contribute to the discrepancy between the current study and this one.
Recently, some studies have supported an influence of intrauterine development on risk of health and disease later in life [33]. Birth weight was generally considered as an indicator of gestational nutritional status [34]. In the present study, high birth weight (≥4.0 kg) was identified as a risk factor for obesity among children (adjusted OR: 2.34; 95 % CI: 1.53–3.58), which was consistent with previous findings [17, 35]. Nevertheless, Chinese pregnant women tend to be urged to consume a large amount of high-nutrition food (e.g., meat, eggs and nuts), which may result in fetal excessive weight gain. It was observed that the proportion of macrosomia increased from 3.2 % in 1985 to 4.3 % in 2005 in healthy term newborns in China [36]. In our study, the percentage of macrosomia was even higher (6.2 %). Considering higher risk of childhood obesity, mothers during pregnancy should keep a healthy diet to avoid infants with high birth weight. On the other hand, the role of low birth weight in the subsequent development of overweight and obesity was still unclear [17]. Compared with normal birth weight (2.5 ~ 4.0 kg), low birth weight (<2.5 kg) presented no significant association with overweight or obesity in our study. Furthermore, gestational age < 37 weeks was positively associated with overweight (versus 37 ~ 42 weeks, adjusted OR: 1.75; 95 % CI: 1.01–3.05) independent of birth weight, which might be explained by infant accelerated weight gain in premature. Previous findings regarding the relationship between gestational age and obesity remained inconsistent [37, 38]. Li et al. suggested that preterm large for gestational age (OR: 2.75) and preterm appropriate for gestational age (OR: 1.56) were both recognized as significant risk factors of childhood overweight and obesity [37]. The above study failed to demonstrate a relationship between preterm small for gestational age and later overweight or obesity [37]. More studies are need to analyze the independent associations between gestational age and obesity. We found no association between cesarean delivery and childhood obesity, on which the findings remained controversial in China [18, 39]. Although a protective effect of breastfeeding for subsequent obesity of children was demonstrated in several studies [19, 40], we found no statistically relationship between feeding patterns and overweight or obesity. However, the lowest prevalence of overweight and obesity was found among children with a breastfeeding duration of 4.0 ~ 5.9 months. A similar pattern was observed in a case-control study in Europe [41] and a cohort study in Brazil [42]. Consistent with other studies [13, 14], we found that children with a parent being overweight or obese were more likely to be overweight or obese compared with those with normal-weight parents. Parental overweight or obesity might have an influence on child’s obesity through genetic or behavioral factors such as dietary habits and family lifestyle.
We also assessed the associations of behavioral factors with overweight/obesity. Among the dietary behaviors, SSBs intake and eating speed faster than peers were positively associated with childhood overweight and obesity. The findings on SSBs intake were supported by previous studies [43, 44]. Given that SSBs intake was a significant contributor to weight gain [45], future obesity intervention strategies should focus on the consumption of SSBs among children. We proposed that schools should restrict the supply of soft drinks. Eating speed was another independent factor that affected overweight/obesity, which was consistent with the findings of other studies [15, 46]. Eating speed faster than peers (versus “as fast as peers”) showed a strong positive association with both overweight (adjusted OR: 1.76; 95 % CI: 1.27 – 2.43) and obesity (adjusted OR: 3.18; 95 % CI: 2.28–4.44), whereas eating speed slower than peers (versus “as fast as peers”) demonstrated an opposite association (adjusted OR: 0.55; 95 % CI: 0.36–0.84 and adjusted OR: 0.55; 95 % CI: 0.34–0.91, respectively). Previous studies found that the energy intake per day can significantly increase along with an increasing eating speed [47]. Among all dietary behaviors, eating speed demonstrated the strongest association with overweight and obesity, which indicated that this factor may play a crucial role in energy intake. Therefore, the eating speed of children should be moderated by launching health education programs. Short sleep duration was also considered a potential risk for overweight/obesity in children [48]. In our study, we found sleep duration as “9.0 ~ 11.0 h” (versus 7.0 ~ 8.9 h) was negatively associated with overweight (adjusted OR: 0.60; 95 % CI: 0.43–0.84), but not with obesity.
With regard to sedentary time, we investigated the relationships of single types of inactivity with obesity and found that daily homework time was independently associated with obesity, which was consistent with previous studies [11]. However, unlike previous findings [49, 50], television viewing was not associated with overweight or obesity. We hypothesized that children of this age can only begin to demonstrate excessive weight gain after a longer duration of television viewing. Sedentary behavior of Chinese children, including screen time and homework time, had increased over the last decade [51]. The unique Chinese culture, in which parents hold high expectations on the academic performance of their children, may influence and differentiate the sedentary behavior of Chinese children from those of children in developed countries [51]. Additional research are warranted to confirm the effect of doing homework on the prevalence of obesity among Chinese children.
It is well known that decreased physical activity was positively associated with increased BMI [52]. However, we did not observe significant associations between physical activities and overweight or obesity, which might be attributed to the lack of physical activities among the study participants. The majority of our participating children, either normal-weight or overweight, failed to meet the recommended 60 min of moderate- to vigorous-intensity physical activity daily [53]. A hypothesis is that these children might be exposed further to physical activity before we can observe any effect. Wang et al. [54] objectively assessed the physical activity levels of 2163 9–17-year-old Chinese children by using accelerometers in 2011 and found that only 9.4 % of boys and 1.9 % of girls reached the recommendation [53]. Intervention strategies must be proposed to promote the participation in physical activities.
Previous studies suggested that perceived overweight and the actual overweight status were strongly associated with weight-loss practices [55]. In our study, overweight/obese children were more likely to adopt weight-loss practice than normal-weight children, and the perception of weight status was strongly associated with the adoption of weight-loss practice among obese children as well as the entire population. Logistic regression analyses showed that the odds of adopting weight-loss practice were 4.9 and 10.7 times as high among children who perceived themselves as overweight and obese, respectively, which indicated that such perception was one of the major driving forces for children to lose weight. Nevertheless, a previous study [56] revealed that Chinese children tended to underestimate overweight and obesity status, particularly among children with high BMI. Therefore, an important first step of obesity intervention might be promoting accurate identification and interpretation of actual weight status in overweight and obese children.
This study presents several limitations. First, the collected data were cross-sectional, which can preclude inferences about causality. Second, a cluster sampling method was used to recruit the participants, which can result in selection bias. Third, BMI was used to measure weight status, which was incapable of distinguishing between total lean mass and fat mass. However, BMI is highly, positively correlated with fat mass in children [57]. So high BMI can be a fairly good indicator of excess body fatness in children. Fourth, the behavioral variables, such as dietary intake of certain foods, duration of physical activities and duration of sedentary behavior, were self-reported, so recall bias may exist. Besides, we did not use previously validated questionnaires to measure behavioral factors, which make the outcomes not straightforward to compare with those measured by the validated questionnaires.
Conclusions
The prevalence of overweight (11.2 %) and obesity (10.0 %) among children in Guangzhou were higher than the previous reported level. High birth weight, SSBs intake, eating speed faster than peers, and homework time were positively associated with obesity among children. Therefore, future studies or programs should focus on the unhealthy dietary and sedentary behavior of children. An accurate perception of weight status plays an important role to improve the weight-loss practices in overweight and obese children.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- OR:
-
Odd ratio
- SD:
-
Standard deviation
- SSBs:
-
Sugar-sweetened beverages
- WGOC:
-
The Working Group of Obesity in China
References
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81. doi:10.1016/S0140-6736(14)60460-8.
Ji CY. Cooperative Study on Childhood Obesity: Working Group on Obesity in China (2008) The prevalence of childhood overweight/obesity and the epidemic changes in 1985–2000 for Chinese school-age children and adolescents. Obes Rev. 2008;9 Suppl 1:78–81. doi:10.1111/j.1467-789X.2007.00443.x.
Ji CY, Cheng TO. Epidemic increase in overweight and obesity in Chinese children from 1985 to 2005. Int J Cardiol. 2009;132:1–10. doi:10.1016/j.ijcard.2008.07.003.
Ji CY, Chen TJ, Working Group on Obesity in China (WGOC). Empirical changes in the prevalence of overweight and obesity among Chinese students from 1985 to 2010 and corresponding preventive strategies. Biomed Environ Sci. 2013;26:1–12. doi:10.3967/0895-3988.2013.01.001.
Zhang YX, Wang SR. Secular trends in body mass index and the prevalence of overweight and obesity among children and adolescents in Shandong, China, from 1985 to 2010. J Public Health (Oxf). 2012;34:131–7. doi:10.1093/pubmed/fdr053.
Kelly AS, Barlow SE, Rao G, Inge TH, Hayman LL, Steinberger J, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128:1689–712. doi:10.1161/CIR.0b013e3182a5cfb3.
McMillan DC, Sattar N, McArdle CS. ABC of obesity. Obesity and cancer. BMJ. 2006;333:1109–11.
Shan XY, Xi B, Cheng H, Hou DQ, Wang Y, Mi J. Prevalence and behavioral risk factors of overweight and obesity among children aged 2–18 in Beijing, China. Int J Pediatr Obes. 2010;5:383–9. doi:10.3109/17477160903572001.
Moraeus L, Lissner L, Yngve A, Poortvliet E, Al-Ansari U, Sjöberg A. Multi-level influences on childhood obesity in Sweden: societal factors, parental determinants and child’s lifestyle. Int J Obes (Lond). 2012;36:969–76. doi:10.1038/ijo.2012.79.
Ness M, Barradas DT, Irving J, Manning SE. Correlates of overweight and obesity among American Indian/Alaska Native and Non-Hispanic White children and adolescents: National Survey of Children’s Health, 2007. Matern Child Health J. 2012;16 Suppl 2:268–77. doi:10.1007/s10995-012-1191-8.
Song Y, Zhang X, Ma J, Zhang B, Hu P-J, Dong B. Behavioral risk factors for overweight and obesity among Chinese primary and middle school students in 2010. Zhonghua Yu Fang Yi Xue Za Zhi. 2012;46:789–95 (Article in Chinese).
Telford RD, Cunningham RB, Telford RM, Riley M, Abhayaratna WP. Determinants of childhood adiposity: evidence from the Australian LOOK study. PLoS One. 2012;7:e50014. doi:10.1371/journal.pone.0050014.
Yi X, Yin C, Chang M, Xiao Y. Prevalence and risk factors of obesity among school-aged children in Xi’an. China Eur J Pediatr. 2012;171:389–94. doi:10.1007/s00431-011-1566-7.
Guo X, Zheng L, Li Y, Zhang X, Yu S, Yang H, et al. Prevalence and risk factors of being overweight or obese among children and adolescents in northeast China. Pediatr Res. 2013;74:443–9. doi:10.1038/pr.2013.116.
Lin M, Pan L, Tang L, Jiang J, Wang Y, Jin R. Association of eating speed and energy intake of main meals with overweight in Chinese pre-school children. Public Health Nutr. 2014;17:2029–36. doi:10.1017/S1368980013002176.
Li L, Shen T, Wen LM, Wu M, He P, Wang Y, et al. Lifestyle factors associated with childhood obesity: a cross-sectional study in Shanghai, China. BMC Res Notes. 2015;8:6. doi:10.1186/s13104-014-0958-y.
Yu ZB, Han SP, Zhu GZ, Zhu C, Wang XJ, Cao XG, et al. Birth weight and subsequent risk of obesity: a systematic review and meta-analysis. Obes Rev. 2011;12:525–42. doi:10.1111/j.1467-789X.2011.00867.x.
Li H, Ye R, Pei L, Ren A, Zheng X, Liu J. Caesarean delivery, caesarean delivery on maternal request and childhood overweight: a Chinese birth cohort study of 181 380 children. Pediatr Obes. 2014;9:10–6. doi:10.1111/j.2047-6310.2013.00151.x.
Yamakawa M, Yorifuji T, Inoue S, Kato T, Doi H. Breastfeeding and obesity among schoolchildren: a nationwide longitudinal survey in Japan. JAMA Pediatr. 2013;167:919–25. doi:10.1001/jamapediatrics.2013.2230.
Zhang J, Jiang J, Himes JH, Zhang J, Liu G, Huang X, et al. Determinants of high weight gain and high BMI status in the first three months in urban Chinese infants. Am J Hum Biol. 2012;24:633–9. doi:10.1002/ajhb.22284.
Zhang J, Himes JH, Guo Y, Jiang J, Yang L, Lu Q, et al. Birth weight, growth and feeding pattern in early infancy predict overweight/obesity status at two years of age: a birth cohort study of Chinese infants. PLoS One. 2013;8(6):e64542. doi:10.1371/journal.pone.0064542.
Liu B, Jing J, Mai J, Chen Y, Xu G, Bao P, et al. Secular trends of overweight and obesity prevalence between 2007 and 2011 in children and adolescents in Guangzhou. Zhonghua Yu Fang Yi Xue Za Zhi. 2014;48:312–7 (Article in Chinese).
Ma L, Zhu Y, Mai J, Jing J, Liu Z, Jin Y, et al. Secular trends in overweight and obesity among urban children in Guangzhou China, 2007–2011. Iran J Public Health. 2015;44:36–42.
Ma L, Mai J, Jing J, Liu Z, Zhu Y, Jin Y, et al. Empirical change in the prevalence of overweight and obesity in adolescents from 2007 to 2011 in Guangzhou. China Eur J Pediatr. 2014;173:787–91. doi:10.1007/s00431-013-2250-x.
Institute of Child and Adolescent Health of Peking University. The health information platform of primary and secondary school students of Plan 1147. 2012. http://health1147.bjmu.edu.cn/. Accessed 28 June 2015.
Chen Y, Ma L, Ma Y, Wang H, Luo J, Zhang X, et al. A national school-based health lifestyles interventions among Chinese children and adolescents against obesity: rationale, design and methodology of a randomized controlled trial in China. BMC Public Health. 2015;15:210. doi:10.1186/s12889-015-1516-9.
Group of China Obesity Task Force. Body mass index reference norm for screening overweight and obesity in Chinese children and adolescents. Zhonghua Liu Xing Bing Xue Za Zhi. 2004;25:97–102 (Article in Chinese).
National Health and Family Planning Commission of the People’s Republic of China. Screening standard for malnutrition of school-age children and adolescents. 2014. http://www.moh.gov.cn/zwgkzt/pqt/201407/38b15c0a1ed444e8908e12752decaffa.shtml. Accessed 10 August 2015.
Chen C, Lu FC, Department of Disease Control Ministry of Health, PR China. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci. 2004;17 Suppl:1–36 (Article in Chinese).
Ji CY, Cheng TO. Prevalence and geographic distribution of childhood obesity in China in 2005. Int J Cardiol. 2008;131:1–8. doi:10.1016/j.ijcard.2008.05.078.
Song Y, Wang HJ, Ma J, Wang Z. Secular trends of obesity prevalence in urban Chinese children from 1985 to 2010: gender disparity. PLoS One. 2013;8:e53069. doi:10.1371/journal.pone.0053069.
Hunsberger M, Formisano A, Reisch LA, Bammann K, Moreno L, De Henauw S, et al. Overweight in singletons compared to children with siblings: the IDEFICS study. Nutr Diabetes. 2012;2:e35. doi:10.1038/nutd.2012.8.
Rinaudo PF, Lamb J. Fetal origins of perinatal morbidity and/or adult disease. Semin Reprod Med. 2008;26:436–45. doi:10.1055/s-0028-1087109.
Fallucca S, Vasta M, Sciullo E, Balducci S, Fallucca F. Birth weight: genetic and intrauterine environment in normal pregnancy. Diabetes Care. 2009;32:e149. doi:10.2337/dc09-1489.
Ren J, Wu J, Ji M, Rong F, Li Y, Gao E, et al. The effect of high birth weight on overweight and obesity in childhood and adolescence. A cohort study in China. Saudi Med J. 2013;34:623–31.
Zhang YQ, Li H. Changes in weight, length, head circumference, and ponderal index at birth of healthy term newborns in nine cities in China during the period of rapid social development 1985–2005. Econ Hum Biol. 2015;19:45–50. doi:10.1016/j.ehb.2015.07.003.
Li P, Yang F, Xiong F, Huo T, Tong Y, Yang S, et al. Nutritional status and risk factors of overweight and obesity for children aged 9–15 years in Chengdu, Southwest China. BMC Public Health. 2012;12:636. doi:10.1186/1471-2458-12-636.
Heppe DH, Kiefte-de Jong JC, Durmuş B, Moll HA, Raat H, Hofman A, et al. Parental, fetal, and infant risk factors for preschool overweight: the Generation R Study. Pediatr Res. 2013;73:120–7. doi:10.1038/pr.2012.145.
Lin SL, Leung GM, Schooling CM. Mode of delivery and adiposity: Hong Kong’s “Children of 1997” birth cohort. Ann Epidemiol. 2013;23:693–9. doi:10.1016/j.annepidem.2013.06.090.
Hunsberger M, Lanfer A, Reeske A, Veidebaum T, Russo P, Hadjigeorgiou C, et al. Infant feeding practices and prevalence of obesity in eight European countries-the IDEFICS study. Public Health Nutr. 2013;16:219–27. doi:10.1017/S1368980012003850.
Bammann K, Peplies J, De Henauw S, Hunsberger M, Molnar D, Moreno LA, et al. Early life course risk factors for childhood obesity: the IDEFICS case-control study. PLoS One. 2014;9:e86914. doi:10.1371/journal.pone.0086914.
Neutzling MB, Hallal PR, Araújo CL, Horta BL, Vieira Mde F, Menezes AM, et al. Infant feeding and obesity at 11 years: prospective birth cohort study. Int J Pediatr Obes. 2009;4:143–9. doi:10.1080/17477160802453530.
Malik VS, Willett WC, Hu FB. Sugar-sweetened beverages and BMI in children and adolescents: reanalyses of a meta-analysis. Am J Clin Nutr. 2009;89:438–9. doi:10.3945/ajcn.2008.26980.
Olsen NJ, Heitmann BL. Intake of calorically sweetened beverages and obesity. Obes Rev. 2009;10:68–75. doi:10.1111/j.1467-789X.2008.00523.x.
Malik VS, Popkin BM, Bray GA, Després JP, Hu FB. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. 2010;121:1356–64. doi:10.1161/CIRCULATIONAHA.109.876185.
Ochiai H, Shirasawa T, Ohtsu T, Nishimura R, Morimoto A, Hoshino H, et al. Eating behaviors and overweight among adolescents: a population-based survey in Japan. J Obes. 2013;2013:717942. doi:10.1155/2013/717942.
Otsuka R, Tamakoshi K, Yatsuya H, Murata C, Sekiya A, Wada K, et al. Eating fast leads to obesity: findings based on self-administered questionnaires among middle-aged Japanese men and women. J Epidemiol. 2006;16:117–24.
Fatima Y, Doi SA, Mamun AA. Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis. Obes Rev. 2015;16:137–49. doi:10.1111/obr.12245.
Rey-López JP, Vicente-Rodríguez G, Biosca M, Moreno LA. Sedentary behaviour and obesity development in children and adolescents. Nutr Metab Cardiovasc Dis. 2008;18:242–51.
Tremblay MS, LeBlanc AG, Kho ME, Saunders TJ, Larouche R, Colley RC, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int J Behav Nutr Phys Act. 2011;8:98. doi:10.1186/1479-5868-8-98.
Cui Z, Hardy LL, Dibley MJ, Bauman A. Temporal trends and recent correlates in sedentary behaviours in Chinese children. Int J Behav Nutr Phys Act. 2011;8:181–90. doi:10.1186/1479-5868-8-93.
Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007;120 Suppl 4:S193–228.
World Health Organization. Global recommendations on physical activity for health. 2010. http://www.who.int/dietphysicalactivity/factsheet_young_people/en/. Accessed 25 June 2015.
Wang C, Chen P, Zhuang J. A national survey of physical activity and sedentary behavior of Chinese city children and youth using accelerometers. Res Q Exerc Sport. 2013;84 Suppl 2:S12–28.
Chung AE, Perrin EM, Skinner AC. Accuracy of child and adolescent weight perceptions and their relationships to dieting and exercise behaviors: a NHANES study. Acad Pediatr. 2013;13:371–8. doi:10.1016/j.acap.2013.04.011.
Yao NL, Hillemeier MM. Weight status in Chinese children: maternal perceptions and child self-assessments. World J Pediatr. 2012;8:129–35. doi:10.1007/s12519-012-0346-4.
Wohlfahrt-Veje C, Tinggaard J, Winther K, Mouritsen A, Hagen CP, Mieritz MG, et al. Body fat throughout childhood in 2647 healthy Danish children: agreement of BMI, waist circumference, skinfolds with dual X-ray absorptiometry. Eur J Clin Nutr. 2014;68:664–70. doi:10.1038/ejcn.2013.282.
Acknowledgements
We acknowledge the Guangzhou Health Care Clinics of Middle and Primary Schools for their contributions in the physical examination and the data collection. We also thank the students for their participation in the survey and the postgraduates for conducting the questionnaire survey and inputting the data.
Funding
This work was funded by Guangdong Natural Science Fund (No. 2015A030313093), Guangdong Science and Technology Program (No. 2014A020220002), and the Special Research Grant for Non-profit Public Service of the Ministry of Health of the People’s Republic of China (Grant No. 201202010).
Availability of data and materials
The dataset supporting the conclusions of this article is available at http://health1147.bjmu.edu.cn/.
Authors’ contributions
YC, JJ and JM designed the experiments. TZ and LM carried out the experiments. TZ performed the statistical analysis and drafted the manuscript. LC guided the statistical analysis and critically revised the manuscript. YC provided suggestions in the statistical analysis and approved the final manuscript. JJ and JM supervised the analysis and revised the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The project was approved by the Ethical Committee of Peking University. Informed consent forms were obtained from all participating students and their parents.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zhang, T., Cai, L., Ma, L. et al. The prevalence of obesity and influence of early life and behavioral factors on obesity in Chinese children in Guangzhou. BMC Public Health 16, 954 (2016). https://doi.org/10.1186/s12889-016-3599-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-016-3599-3