Abstract
Background
This study compares the effectiveness of psychotherapeutic consultation in the workplace (PSIW) with psychotherapeutic outpatient care (PSOC) in Germany.
Methods
Work ability (WAI), quality of life (SF-12), clinical symptoms (PHQ) and work-related stress (MBI, IS) were assessed in 367 patients seeking mental health care via two routes (PSIW n = 174; PSOC n = 193) before consultation and 12 weeks later. Changes in outcome variables were assessed using covariance analysis with repeated measures (ANCOVA) with sociodemographic variables (propensity score method), therapy dose, setting and symptom severity as covariates.
Results
The PSIW and PSOC groups included 122 and 66 men respectively. There were 102 first-time users of mental healthcare in the PSIW group and 83 in the PSOC group. There were group differences in outcome variables at baseline (p < 0.05); PSIW patients were less impaired overall.
There were no group difference in sociodemographic variables, number of sessions within the offer or symptom severity. There was no main effect of group on outcome variables and no group*time interaction. Work-related stress indicators did not change during the intervention, but work ability improved in both groups (F = 10.149, p = 0.002; baseline M = 27.2, SD = 8.85); follow-up M = 28.6, SD = 9.02), as did perceived mental health (SF-12 MCS), depression (PHQ-9) and anxiety (PHQ-7). Effect sizes were between η2 = 0.028 and η2 = 0.040.
Conclusions
Psychotherapeutic consultation is similarly effective in improving patients’ functional and clinical status whether delivered in the workplace or in an outpatient clinic. Offering mental health services in the workplace makes it easier to reach patients at an earlier stage in their illness and thus enables provision of early and effective mental health care.
Trial registration
DRKS00003184, retrospectively registered 13 January 2012.
Similar content being viewed by others
Background
Common mental disorders (CMD) will be one of the main contributors to the global economic burden of non-communicable diseases by 2030 [1]. Recently it has been anticipated that the direct and indirect costs of CMD amount to 3.5 % of the gross domestic product of industrial countries on average [2]. CMD and even sub-threshold mental health conditions have adverse effects on everyday life, work capacity and even mortality [3–6]. Because of their prevalence and costs CMD have an enormous impact on public health [7]. The increase in the prescription of psychotropic drugs, such as antidepressants, demonstrates that in practice this is the preferred approach to treatment, although it has been shown that a combination of psychotherapy and medication is the most effective treatment for most CMD [8, 9]. German guidelines recommend pharmacotherapy or psychotherapy as treatments for mild to moderate depressive disorders and explicitly recommend a combination of both for severe depression [10].
The treatment gap for CMD is estimated at 55 % globally while the improvement of treating CMD effectively has been considered to be very encouraging [11, 12]. Long waiting periods for initial consultations and psychotherapy are obstacles to appropriate treatment in healthcare systems across Europe, including in Belgium, Denmark, the Netherlands and Germany [13–17]. The interface between primary and secondary care may represent another barrier to effective treatment. In most countries general practitioners (GPs) mediate access to secondary services, i.e. specialist care. Unfortunately GPs often struggle to identify mental health problems [15, 18]. Fear of stigmatisation is another obstacle to timely treatment [19]. Thus there is a need to strengthen psychotherapeutic approaches by making them more accessible.
20 % of the working age population experience CMD at any one time [20]. The workplace has been identified as a key social context for early identification and treatment of mental health problems [2, 21, 22]. Focusing on what improves return to work after being sick listed due to depression [23] or on the effectiveness of work-directed interventions within the return to work process [24] restricted to randomised controlled trials showed positive but weak effects on work-related outcomes such as returning to work faster. Putting these findings together and including controlled trials Pomaki et al. [25] emerged important factors of how workplace-based interventions improve work disability outcomes: facilitation of access to clinical treatment, and availability of workplace-based psychotherapeutic interventions [25]. Chronic mental health problems, including subclinical symptoms, and impaired work ability are strong predictors of long sickness absence [26, 27]; this underlines the importance of early intervention.
Collaborative care offers (CCO) such as “psychotherapeutic consultation in the workplace” have been established as part of programmes to promote mental health in the workplace and are well-accepted by patients [28, 29].
Although the workplace environment is considered by many experts as an appropriate setting for a psychosocial intervention, there are currently no studies on the effectiveness of such interventions. A standard form of mental health treatment, short-term psychotherapeutic outpatient care (PSOC), has been adapted for delivery in the workplace under the label “psychotherapeutic consultation in the workplace” (PSIW) [30–32]. In this article we present the results of an observational controlled trial on the effectiveness of the PSIW program in comparison to the PSOC as a measure of routine care.
Methods
Study design
Due to reasons of the involved companies, staff policy and legal restrictions it was not possible to conduct a randomised controlled trial. Therefore, a prospective, controlled, observational trial comparing 174 employees from three companies who received PSIW with 193 outpatients from two clinics who received PSOC was conducted. Outcome indicators were assessed prior to the initial consultation (t1) and 12 weeks later (t2) [33].
Study context
In the German healthcare system patients with CMD are treated by physicians specialising in psychiatry or psychosomatic medicine or by psychological psychotherapists. Treatment is usually delivered through private practices, the outpatient clinics of psychosomatic hospitals and psychosomatic departments or psychosomatic outpatient clinics at general hospitals [34]. In the German healthcare system PSOC is covered by statutory health insurance as well as by the private health insurance, and nearly 100 % of the population is covered by health insurance. Thus comprehensive care should be available to all those who need it [35]. In spite of this the treatment gap for CMD in Germany is comparable to that in other European countries [36–38].
Intervention
Psychotherapeutic consultation in the workplace (PSIW)
PSIW is provided by a mental health expert (medical or psychological psychotherapist) who, although not employed by the host company, may be paid by the company (as an external contractor) or by the company’s health insurance funds. The service is available to all staff free of charge.
Staff members are usually informed about the service by the company physician. In one company employees must be referred to PSIW by the company physician but in others self-referral is possible. If self-referral is available information about PSIW (nature of the service; location; how to make an appointment) is communicated via paper and online.
In the first session the user’s clinical status and needs are being assed. This assessment is used to determine severity of the mental health problem and whether workplace consultation is a suitable treatment option or whether additional or more intensive mental health care (e.g. outpatient psychotherapy; short-term (8–10 sessions) psychotherapy; psychopharmacological treatment; inpatient treatment) is needed. Each session lasts 50–60 minutes and a maximum of four sessions can be offered under the PSIW programme.
After assessment the PSIW user will be informed about any further therapeutic steps that are indicated, motivating the service user to obtain additional help and providing specific advice to help individuals overcome barriers to service use. This involves providing the PSIW user with information about CMD and psychotherapeutic approaches to treatment. The strengths and resources of the patient are stressed and further treatments are recommended. If appropriate information about self-help books, counselling centres, e.g. family or drug and addiction counselling, and other services such as workshops on relaxation techniques is provided. Recommendations are made according to the clinical guidelines of the Association of the Scientific Medical Societies in Germany (AWMF) as they exist e.g. for depression [10].
PSIW takes place only in companies that agree to offer the service and provide structural support. Company support includes appointment making and providing a suitable location for consultations. Subject to patient consent the next steps in treatment are determined in a case conference involving the occupational health physicians and the psychotherapeutic consultant.
Psychotherapeutic outpatient care (PSOC)
Initial PSOC treatment is limited to two sessions and the core elements are assessment of clinical symptoms and service needs, provision of information about CMD and treatment methods and recommendations for further treatment. Referral to PSOC is predominantly via GPs. Self-referral is encouraged and information for patients drafted via the clinic websites.
Eligibility criteria and recruitment process
To be eligible for the study participants had to be at least 18 years old, capable of understanding and writing German and currently employed. Participants in the PSIW group had to be employed by one of the participating companies.
Participants in the PSOC group were recruited consecutively from two outpatient clinics, the University Clinic of Psychosomatic Medicine and Psychotherapy, Ulm, and Sonnenbergklinik, Division of Psychosomatic Medicine of the ZfP Suedwuerttemberg, Stuttgart, from June 2012 to January 2013.
Participants in the PSIW group were recruited consecutively from November 2011 to June 2013.
Assessment
Assessment of clinical status was made by means of self-administrated questionnaires (Table 1). Questionnaires for baseline assessment were handed over at the first meeting. Follow-up questionnaires were sent out by mail. Data were double entered manually and checked twice.
Work ability
Ability to work was the primary outcome indicator and was assessed using the work ability index (WAI), a self-report instrument used to assess current and future work ability and work demand management based on behavioural measures [39].
Use of mental health services and symptom duration
Lifetime history of psychotherapeutic treatment and number of contacts with mental health services over the previous 12 months were recorded. Duration (in months) of the symptoms which had prompted the consultation was recorded by the therapist.
Mental health and somatic symptoms
Depression was assessed with the 9-item Patient Health Questionnaire - depression scale (PHQ-9) [40], anxiety with the 7-item Patient Health Questionnaire - generalised anxiety disorder scale (PHQ-7) [41] and somatic symptom severity with the 15-item Patient Health Questionnaire - somatisation (PHQ-15) [42]. Interpretation of PHQ scores was based on the diagnostic criteria of the DSM-IV and ICD-10, using the recommended cut-off of 10 or above to distinguish between clinical and non-clinical levels of symptoms [43].
Health-related quality of life
Health-related quality of life was assessed using the SF-12, a validated, short version of the SF-36, to measure the functional health status of patients [44]. Weighted summation provided summary scores for perceived mental health (MCS; mental health component score) and perceived physical health (PCS; physical health component score).
Work-related stress
We assessed work-related stress using the German version (MBI-GS-D) of the Maslach Burnout Inventory (MBI), which is used to assess burnout syndrome as a manifestation of mental exhaustion [45]. The three components of burnout are: emotional exhaustion (EE), depersonalisation (DP) and reduced personal accomplishment (PA). Respondents indicate the frequency with which they experience each item. Sum scores were used instead of means for each subscale.
Irritation
Irritation is defined as subjectively perceived emotional and cognitive strain in occupational contexts [46, 47]. We assessed irritation with the irritation scale (IS).
Statistical analyses
Sample size determination
We calculated that a sample of 220 participants would be needed to detect a medium (effect size f = 0.25) difference in WAI with a power of 0.95 at a significance level of p < 0.05 using repeated measures ANOVA.
Bias control
The propensity adjustment method was used for bias control [48]. Propensity scores were estimated as the conditional probability of belonging to the PSIW group using a logistic regression model including age, gender, family status (marital status, living with children or not, living with other adults or not), job status (school-leaving qualification, full or part-time employment, occupation: uneducated, skilled or white collar worker, managerial staff), duration of psychopathological symptoms, history of psychiatric or psychotherapeutic treatment (outpatient treatment: lifetime, previous 12-month, inpatient treatment: lifetime, previous 12-month, other physician’s care: previous 12-month, psychosocial treatment within company: previous 12-month, other like pastoral advice service etc.), and baseline clinical differences as independent variables. Number of sessions and presence of treatment between the first consultation and follow-up assessment were included in the model as covariates.
Latent profile analysis (LPA) [49] including the WAI, PHQ-9 and the SF-12 was used to provide an overall indication of clinical differences at baseline. Details of the LPA procedure and results are published elsewhere (Rothermund et al. submitted). On the basis of the LPA participants were classified into four classes (1 = severely mentally ill, 2 = moderately affected with low quality of life, 3 = moderately affected with low work ability, 4 = less affected but at risk) which captured global differences in baseline clinical measures. Class membership was included in the logistic regression model as a categorical independent variable with class four as the reference category.
Effectiveness analysis
The effectiveness of the intervention was estimated with respect to primary and secondary outcomes on an intention to treat (ITT) basis. Missing endpoint data were imputed as last observation carried forward (LOCF).
Change in outcome indicators was analysed by covariance analysis with repeated measures (ANCOVA) with propensity scores as covariates. Statistical analyses were performed using SPSS version 21.
Results
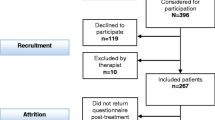
A total of 367 participants were included in the analyses (PSIW n = 174; PSOC n = 193) (see flow diagram, Fig. 1 and Table 2 for sociodemographic data). Due to missing propensity scores a total of 17 cases (4.6 %) was excluded from the analyses. Follow-up data were obtained of 60 % of participants. Reasons for dropout were not given. Non-respondents were younger (38, SD 11.3) than respondents (45, SD 10.7). No significant differences were found for gender, educational level, symptom severity or any of the psychometric measures. The PSIW group was slightly older (45 years, SD = 10.1) than the comparison group (40 years, SD = 12.1) and PSIW participants tended to have been experiencing symptoms for a shorter period of time (38 months, SD = 65.4) than PSOC participants (51 months, SD = 72.9). The majority of the PSIW group were men (n = 122, 70 %) and just over a third of the PSOC group was men (n = 66, 34 %). The PSIW group contained 102 first-time users of mental health services (65 %); the corresponding figure for the PSOC group was 83 (45 %). 12-month usage of mental health services (number of participants who had at least one contact with mental health services) was lower in the PSIW group (n = 65) than the PSOC group (n = 119).
At two companies most referrals to PSIW were made by occupational physicians or social workers; at the third company employees were usually self-referred. For a more detailed description of procedures of PSIW see Rothermund et al. 2014 [31].
Baseline data (Table 3)
At baseline the PSIW group had higher work ability (M = 29.5, SD = 8.02) than the PSOC group (M = 25.3, SD = 9.07; p < 0.001). The PSIW group also had better perceived mental health (SF-12 MCS: M = 33.3, SD = 11.13) than the PSOC group (M = 29.8, SD = 10.24, p = 0.002) at baseline. Depression scores at baseline were also lower in the PSIW group (M = 11.3, SD = 5.72) than the PSOC group (M = 14.5, SD = 6.28, p < 0.001). Anxiety scores showed a similar pattern (PSIW group: M = 9.6, SD = 5.36; PSOC group: M = 11.2, SD = 5.71; p < 0.001). There were no group differences in physical health (SF-12 PCS) and somatic symptom severity (PHQ-15) at baseline.
Work-related stress was also lower in the PSIW group at baseline. IS scores were lower in the PSIW group (M = 30.7, SD = 11.74) than the PSOC group (M = 35.2, SD = 12.12, p = 0.001). The PSIW group also had lower scores on two aspects of burnout. EE was lower in the PSIW group (M = 3.9, SD = 1.27) than in the PSOC group (M = 4.5, SD = 1.24; p < 0.001) and the PSIW group showed less DP (M = 3.2, SD = 1.11) than the PSOC group (M = 3.5, SD = 1.22; p = 0.015). There was no baseline group difference in PA.
Overall, patients that were recruited in the workplace context (PSIW group) appeared to be healthier than patients that were using established services.
Effects of PSIW and PSOC on work ability and clinical and work-related parameters (Table 3)
Both groups showed a similar improvement in work ability over time (baseline M = 27.2, SD = 8.85; follow-up M = 28.6, SD = 9.02; F = 10.149, p = 0.002). At follow-up the mean work ability of the PSIW group (M = 30.8, SD = 8.32) was higher than that of the PSOC group (M = 26.8, SD = 9.21). However there was no group effect and no group*time interaction for WAI score. None of the 3 covariates (propensity score; number of sessions; presence of further treatment) had an effect on WAI.
Both groups showed similar improvements in perceived mental health (SF-12 MCS; baseline M = 31.4, SD = 10.78; follow-up M = 34.9, SD = 11.62; F = 9.093, p = 0.003), depression (PHQ-9; baseline M = 12.9, SD = 6.20; follow-up M = 11.1, SD = 6.40; F = 13.946, p < 0.001) and anxiety (PHQ-7; baseline M = 10.4, SD = 5.50; follow-up M = 8.9, SD = 5.41; F = 12.259, p = 0.001). The effect sizes for the changes were small (η2 between 0.028 and 0.040). There was no effect of group and no group*time interaction on these outcome parameters.
There were no changes in measures of physical health (perceived physical health measured as SF-12 PCS score; somatoform symptoms, measured as PHQ-15 score) or work-related stress (all aspects of burnout: EE, DP and PA; IS score).
Discussion
In this trial we assessed work ability, quality of life, clinical symptoms and work-related stress in 367 patients who received mental health services via two programmes, PSIW and PSOC. Patients were assessed before their first consultation and 12 weeks later and in the analyses we controlled for variance in sociodemographic factors, therapy dose, setting and symptom severity.
Our results indicate that psychotherapeutic consultation is similarly effective in improving patients’ functional and clinical status whether delivered in the workplace or in a psychotherapeutic outpatient clinic. Our data clearly suggest that workplace-based services reach people with mental health problems at an earlier state of illness than the traditional health care system. Thus, psychotherapeutic care in an occupational healthcare setting can be considered an early and effective form of mental health care.
The work ability of individuals improved after the initial intervention independent of the setting in which patients sought help; this was a small effect (baseline WAI: M = 27.2 points, SD = 8.02; follow-up WAI: M = 28.6, SD = 9.02; η2 = 0.031; p = 0.002). The same pattern of improvement was observed for depression (baseline PHQ-9: M = 12.9, SD = 6.20; follow-up PHQ-9: M = 11.1, SD = 6.40; F = 13.946, p < 0.001) and anxiety (baseline PHQ-7: M = 10.4, SD = 5.50; follow-up PHQ-7: M = 8.9, SD = 5.41; F = 12.259, p = 0.001). Perceived mental health (SF-12 MCS), also known as health related quality of life, also improved (baseline M = 31.4, SD = 10.78; follow-up M = 34.9, SD = 11.62; F = 9.093, p = 0.003). Effect sizes for all improvements were small, between η2 = 0.028 and η2 = 0.040.
The small effects are plausible as the interventions were very short: one or two sessions, primarily focusing on diagnostic assessment and facilitation of access to other clinical services. A recent study showed that better work ability at baseline was associated with better outcomes, e.g. early return to work [27]. This study focused on short time effects, as the follow-up assessment occurred 12 weeks after the initial consultation. This limitation may have obscured better outcomes in the group treated in the workplace due to the earlier detection of illness. Nevertheless the parallel improvement of clinical parameters and work ability is meaningful, as we know that recovery from depression does not automatically mean that a person is once more capable of dealing with the demands of everyday life [50–52].
One might have expected the PSIW group to show less spontaneous improvement than the PSOC group on the grounds that they were healthier and would therefore show a smaller response to the initial very short, primarily diagnostic intervention offered. Alternatively one might expect the PSIW group to show greater improvement as prognosis for mental health conditions is usually better in cases where intervention is provided early in the course of disease [53–55].
The findings of this study are in line with findings on return to work process following CMD-related absence. Vlasveld et al. 2012 [56] investigated employees absent from work with major depressive disorder and found that collaborative care produced similar effects to care as usual when outcome was measured as a continuous variable with PHQ-9; however the response rate was higher in the collaborative care group. This probably reflects an aspect of the collaborative care which was not captured in the analyses. Van der Feltz-Cornelis et al. 2010 [57] showed that return to work was faster in an intervention group than a group who received care as usual. The intervention consisted of treatment by occupational physicians who were advised by psychiatric consultants. Both groups showed comparable improvements in symptom severity and quality of life.
During the 12-week period between first consultation and follow-up assessment there was no change in work-related stress (irritation, burnout) in either group, although there were improvements in overall mental well-being, depression and anxiety. There were also no changes on the scales measuring aspects of physical health, namely somatoform symptoms (PHQ-15) and perceived physical health (SF-12 PCS). The lack of effects on work-related stress and physical health may have been because the PSIW programme did not target work-related health or physical health but focused on diagnostic assessment and motivation for further psychotherapeutic treatment.
Limitations and strengths
Our observation that the group accessing psychotherapeutic services in the workplace did not improve more than those accessing services via conventional outpatient clinics may have been influenced by the short length of the observation period of only 12 weeks. We know from research on maintaining gains from psychotherapy that psychotherapeutic interventions may have long term effects and hence follow-up for at least at 12 month after intervention is recommended [58–60]. Our study also suffers from the familiar limitations associated with lack of a randomised group assignment. Thus, bias control was addressed using the propensity score method [61] with only rare (max. 6 %) reduction of sample size. The controlled observational design allowed us to manage the problem of artificial deterioration of the sample. Randomised controlled trials may suffer deterioration of the sample, due to the better control of intervening variables, which often leads to homogenous samples that differ from samples under routine conditions [60, 62, 63]. In our study the intervention was studied under routine conditions and thus the study has good external validity and the findings should be generalizable.
A loss to follow-up of 40 % is quite high. The only detectable difference between non-respondents and respondents was age (38, SD 11.3 vs 45, SD 10.7 years). Thus we conclude the results might not be generalizable to younger workers.
Another limitation is that we did not collect data on therapeutic recommendations and whether they were followed. Such data would have helped us to interpret the pattern of changes between the baseline and follow-up assessment and will therefore be collected and analysed in our next investigation. Finally, the sample was drawn from a single region of Germany rather than from across Europe and so the findings should only be generalised to other countries with different healthcare systems with caution.
Conclusions
We conclude that the PSIW intervention is effective over a 3 month-follow-up period, covering diagnostic assessment and the very early psychotherapeutic sessions. The effects of the intervention were most marked with respect to social functioning (work ability) and mental health in patients with sub-syndromal illness and CMD. To make the intervention more effective in this setting than it is in its current form it would need to be tailored even more to the specific needs of the target group. Exhaustion is one of the major topics mentioned as reason for utilising PSIW (qualitative data in preparation for publication). Ongoing interpersonal conflicts, problems regulating demands and efforts, or problems in prioritising are likely drivers for exhaustion on the individual side. On the organisational side working conditions may contribute to this problem. A short time psychotherapeutic intervention (up to 10 sessions) should be offered to detect relevant areas of conflict and to consequently analyse and address specific individual and/or organisational reasons in more detail. Together with consecutive motivation for further clinical treatment if necessary this approach should make a short-time intervention even more powerful.
Showing that the intervention is effective in the new setting workplace while reaching different users especially due to gender and course of disease drafts the need for in depth information about: which ingredients, barriers, drivers and synergies can be identified in that kind of health care offer in the workplace? We are currently analysing qualitative data which address these questions.
Abbreviations
- ANCOVA:
-
Covariance analysis with repeated measures
- AWMF:
-
Association of the scientific medical societies in Germany
- CCO:
-
Collaborative care offers
- CMD:
-
Common mental disorder
- DP:
-
Depersonalisation
- EE:
-
Emotional exhaustion
- GP:
-
General practitioner
- IS:
-
Irritation scale
- ITT:
-
Intention to treat
- LOCF:
-
Last observation carried forward
- LPA:
-
Latent profile analysis
- M:
-
Mean
- MBI:
-
Maslach burnout inventory
- N:
-
Number
- n.s.:
-
Not significant
- PA:
-
Depersonalisation
- PHQ-7/-9/-15:
-
Patient health questionnaire 7 items generalised anxiety/9 items depression/15 items somatisation
- PSIW:
-
Psychotherapeutic consultation in the workplace
- PSOC:
-
Psychotherapeutic outpatient care
- SD:
-
Standard deviation
- SF-12 mcs/pcs:
-
Short form-12 Items mental health component score/physical health component score
- WA:
-
Work ability
- WAI:
-
Work ability index
References
Bloom DE, Cafiero E, Jané-Llopis E, Abrahams-Gessel S, Bloom L, Fathima S, Feigl AB, Gaziano T, Mowafi M, Pandya A, Prettner K, Rosenberg L, Seligman B, Stein AZ, Weinstein C: The Global Economic Burden of Noncommunicable Diseases. Geneva: World Economic Forum; 2012.
OECD. Fit mind, fit job: from evidence to practice in mental health and work, mental health and work. Paris: OECD Publishing; 2015.
Bertilsson M, Vaez M, Waern M, Ahlborg G, Hensing G. A prospective study on self-assessed mental well-being and work capacity as determinants of all-cause sickness absence. J Occup Rehabil. 2015;25:52–64.
Cuijpers P, Vogelzangs N, Twisk J, Kleiboer A, Li J, Penninx BW. Differential mortality rates in major and subthreshold depression: Meta-analysis of studies that measured both. Br J Psychiatry. 2013;202:22–7.
Russ TC, Stamatakis E, Hamer M, Starr JM, Kivimaki M, Batty GD. Association between psychological distress and mortality: individual participant pooled analysis of 10 prospective cohort studies. Br Med J. 2012;345:e4933.
Jain G, Roy A, Harikrishnan V, Yu S, Dabbous O, Lawrence C. Patient-reported depression severity measured by the PHQ-9 and impact on work productivity: results from a survey of full-time employees in the United States. J Occup Environ Med. 2013;55:252–8.
Vos T, Barber RM, Bell B, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800.
Cuijpers P, Sijbrandij M, Koole SL, Andersson G, Beekman AT, Reynolds CF. Adding psychotherapy to antidepressant medication in depression and anxiety disorders: a meta-analysis. World Psychiatry. 2014;13:56–67.
Huhn M, Tardy M, Spineli LM, Kissling W, Förstl H, Pitschel-Walz G, Leucht C, Samara M, Dold M, Davis JM, Leucht S. Efficacy of pharmacotherapy and psychotherapy for adult psychiatric disorders a systematic overview of meta-analyses. JAMA Psychiatry. 2014;71:706–15.
DGPPN, BÄK, KBV, AWMF, AkdÄ, BPtK, BApK, DAGSHG, DEGAM, DGPM, DGPs, DGRW. Unipolare Depression. S3-Leitlinie/Nationale Versorgungsleitlinie Unipolare Depression - Langfassung. last updat. DGPPN BÄK KBV AWMF AkdÄ BPtK BApK DAGSHG DEGAM DGPM DGPs DGRW; 2009. Available from: www.depression.versorgungsleitlinien.de; [cited: 23.08.2016]; doi:10.6101/AZQ/000239.
OECD. Making mental health count: the social and economic costs of neglecting mental health care OECD health policy studies. Paris: OECD Publishing; 2014.
Chisholm D, Sweeny K, Sheehan P, Rasmussen B, Smit F, Cuijpers P, Saxena S. Scaling-up treatment of depression and anxiety: a global return on investment analysis. Lancet Psychiatry. 2016;0366:1–10.
OECD. Mental Health and Work: Denmark. Paris: OECD Publishing; 2013.
OECD. Mental Health and Work: Belgium. Paris: OECD Publishing; 2013.
OECD. Mental Health and Work: Netherlands. Paris: OECD Publishing; 2014.
Schulz H, Barghaan D, Harfst T, Koch U. Psychotherapeutische Versorgung [Psychotherapeutic healthcare]. Gesundheitsberichterstattung des Bundes. 2008;41:1–47.
Kruse J, Herzog W. Zur ambulanten psychosomatischen/psychotherapeutischen Versorgung in der kassenärztlichen Versorgung in Deutschland - Formen der Versorgung und ihre Effizienz - Zwischenbericht 2012 [About psychosomatic and psychotherapeutic outpatient care in Germany - e. Berlin: Kassenärztliche Bundesvereinigung (KBV); 2012.
Munk-Jørgensen P, Allgulander C, Dahl AA, Foldager L, Holm M, Rasmussen I, Virta A, Huuhtanen M-T, Wittchen H-U. Prevalence of generalized anxiety disorder in general practice in Denmark, Finland, Norway, and Sweden. Psychiatr Serv. 2006;57:1738–44.
Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, Morgan C, Rüsch N, Brown JSL, Thornicroft G. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2015;45:11–27.
OECD. Sick on the job?: myths and realities about mental health and work. Paris: OECD Publishing; 2012.
Gilbody S, Bower P, Rick J. Better care for depression in the workplace: Integrating occupational and mental health services. Br J Psychiatry. 2012;200:442–3.
Leka S, Cox T. The European Framework for Psychosocial Risk Management : PRIMA-EF. Nottingham: Institute of Work, Health and Organisation; 2008.
Nieuwenhuijsen K, Faber B, Verbeek JH, Neumeyer-Gromen A, Hees HL, Verhoeven AC, van der Feltz-Cornelis CM, Bültmann U. Interventions to improve return to work in depressed people. Cochrane Database Syst Rev. 2014;12:CD006237.
van Vilsteren M, van Oostrom SH, de Vet HC, Franche R-L, Boot CR, Anema JR. Workplace interventions to prevent work disability in workers on sick leave. Cochrane Database Syst Rev. 2015;10:CD006955.
Pomaki G, Franche R-L, Murray E, Khushrushahi N, Lampinen TM. Workplace-based work disability prevention interventions for workers with common mental health conditions: a review of the literature. J Occup Rehabil. 2012;22:182–95.
Brouwers EPM, Terluin B, Tiemens BG, Verhaak PFM. Predicting return to work in employees sick-listed due to minor mental disorders. J Occup Rehabil. 2009;19:323–32.
Ekberg K, Wåhlin C, Persson J, Bernfort L, Öberg B. Early and late return to work after sick leave: predictors in a cohort of sick-listed individuals with common mental disorders. J Occup Rehabil. 2015;25:1–11.
Brohan E, Evans-Lacko S, Henderson C, Murray J, Slade M, Thornicroft G. Disclosure of a mental health problem in the employment context: qualitative study of beliefs and experiences. Epidemiol Psychiatr Sci. 2014;23:289–300.
Burman-Roy S, Butterworth M, Madan I, Henderson M, Harvey SB. Which patients are seen by an occupational psychiatry service? Occup Med (Lond). 2013;63:507–9.
Mayer D, Schmidt H, Hoelzer M. “Psychosomatische Sprechstunde “und “Psychosomatische Grundversorgung in der Arbeitsmedizin”. [“Psychosomatic consultation” and “Basic Psychosomatic care in occupational medicine”.]. Arbeitsmed Sozialmed Umweltmed. 2010;45:593–7.
Rothermund E, Gündel H, Kilian R, Hölzer M, Reiter B, Mauss D, Rieger MA, Müller-Nübling J, Wörner A, von Wietersheim J, Beschoner P. Behandlung psychosomatischer Beschwerden im Arbeitskontext - Konzept und erste Daten. [Treatment of psychosomatic disorders occurring in the vocational context – concept and first findings]. Z Psychosom Med Psychother. 2014;60:177–89.
Preiser C, Rothermund E, Wittich A, Gündel H, Rieger MA. Psychosomatic consultation in the workplace - opportunities and limitations of the services offered. Results of a qualitative study. Int. Arch. Occup. Environ. Health. 2016;89:599-608.
Rothermund E, Kilian R, Hoelzer M, Mayer D, Mauss D, Krueger M, Rieger MA, Guendel H. “Psychosomatic consultation in the workplace” -- a new model of care at the interface of company-supported mental health care and consultation-liaison psychosomatics: design of a mixed methods implementation study. BMC Public Health. 2012;12:780.
Diefenbacher A. Psychiatry, psychosomatic medicine and the general hospital in Germany. World Psychiatry. 2003;2:95–7.
Kruse J, Larisch A, Hofmann M, Herzog W. Ambulante psychosomatische und psychotherapeutische Versorgung in Deutschland - Versorgungsprofile abgebildet durch Daten der Kassenärztlichen Bundesvereinigung (KBV) [Psychosomatic and psychotherapeutic outpatient care in Germany – Capacity profile based. Z Psychosom Med Psychother. 2013;59:254–72.
Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, de Girolamo G, Graaf R, Demyttenaere K, Gasquet I, Haro JM, Katz SJ, Kessler RC, Kovess V, Lepine JP, Ormel J, Polidori G, Russo LJ, Vilagut G, Almansa J, Arbabzadeh-Bouchez S, Autonell J, Bernal M, Buist-Bouwman MA, Codony M, Domingo-Salvany A, Ferrer M, Joo SS, Martinez-Alonso M, Matschinger H, Mazzi F, Morgan Z, Morosini P, Palacin C, Romera B, Taub N, Vollebergh WAM. Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr. Scand. Suppl. 2004;109:21–27.
Kessler RC, Üstün B. The WHO world mental health surveys. Global perspectives of mental health surveys. first. New York: Cambridge University Press; 2008.
Mack S, Jacobi F, Gerschler A, Strehle J, Höfler M, Busch MA, Maske UE, Hapke U, Seiffert I, Gaebel W, Zielasek J, Maier W, Wittchen H-U. Self-reported utilization of mental health services in the adult German population – evidence for unmet needs ? Results of the DEGS1-Mental Health Module (DEGS1-MH). Int J Methods Psychiatr Res. 2014;23:289–303.
Tuomi K, Ilmarinen J, Jahkola A, Katajarinne L, Tulkki A. Work ability index. 2nd ed. Helsinki: Finnish Institute of Occupational Health; 1998.
Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13.
Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: The gad-7. Arch Intern Med. 2006;166:1092–7.
Kroenke K, Spitzer RL, Williams JBW. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64:258–66.
Kroenke K, Spitzer RL, Williams JBW, Löwe B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. 2010;32:345–59.
Morfeld M, Bullinger M, Kirchberger I. SF-36 Fragebogen zum Gesundheitszustand [Short form-36 health survey questionnaire]. 2nd ed. Goettingen: Hogrefe; 2011.
Maslach L, Jackson S, Leiter M. Maslach Burnout inventory general version. 3rd ed. Palo Alto: Consulting Psychologists Press; 1996.
Mohr G, Rigotti T, Müller A. Irritation - ein Instrument zur Erfassung psychischer Beanspruchung im Arbeitskontext. Skalen- und Itemparameter aus 15 Studien [Irritation - an instrument assessing mental strain in working contexts. Scale and item parameters from 15 studies]. Zeitschrift für Arbeits- und Organ. 2005;49:44–8.
Mohr G, Müller A, Rigotti T. Normwerte der Skala Irritation: Zwei Dimensionen psychischer Beanspruchung [Standardisation data of the Irritation Scale. Two dimensions of mental strain]. Diagnostica. 2005;51:12–20.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46:399–424.
Lanza ST, Rhoades BL. Latent class analysis: an alternative perspective on subgroup analysis in prevention and treatment. Prev Sci. 2013;14:157–68.
Buist-Bouwman MA, Ormel J, De Graaf R, Vollebergh W. Functioning after a major depressive episode: complete or incomplete recovery? J Affect Disord. 2004;82:363–71.
Pachoud B, Plagnol A, Leplege A. Outcome, recovery and return to work in severe mental illnesses. Disabil Rehabil. 2010;32:1043–50.
Lagerveld SE, Blonk RWB, Brenninkmeijer V, Wijngaards-de Meij L, Schaufeli WB. Work-focused treatment of common mental disorders and return to work: a comparative outcome study. J Occup Health Psychol. 2012;17:220–34.
Dell’Osso B, Glick ID, Baldwin DS, Altamura AC. Can long-term outcomes be improved by shortening the duration of untreated illness in psychiatric disorders? A conceptual framework. Psychopathology. 2013;46:14–21.
Cosci F, Fava GA. Staging of mental disorders: systematic review. Psychother Psychosom. 2013;82:20–34.
Beck A, Crain L, Solberg L, Unützer J, Glasgow R, Maciosek M, Whitebird RR. Does severity of depression predict magnitude of productivity loss? Am J Manag Care. 2014;20:e294–301.
Vlasveld MC, van der Feltz-Cornelis CM, Adèr HJ, Anema JR, Hoedeman R, van Mechelen W, Beekman ATF. Collaborative care for major depressive disorder in an occupational healthcare setting. Br J Psychiatry. 2012;200:510–1.
van der Feltz-Cornelis CM, Hoedeman R, de Jong FJ, Meeuwissen JA, Drewes HW, van der Laan NC, Adèr HJ. Faster return to work after psychiatric consultation for sicklisted employees with common mental disorders compared to care as usual. A randomized clinical trial. Neuropsychiatr Dis Treat. 2010;6:375–85.
Blonk RW, Brenninkmeijer V, Lagerveld SE, Houtman IL. Return to work: a comparison of two cognitive behavioural interventions in cases of work-related psychological complaints among the self-employed. Work Stress. 2006;20:129–44.
Imamura K, Kawakami N, Furukawa TA, Matsuyama Y, Shimazu A, Umanodan R, Kawakami S, Kasai K. Does Internet-based cognitive behavioral therapy (iCBT) prevent major depressive episode for workers? A 12-month follow-up of a randomized controlled trial. Psychol Med. 2015;45:1–11.
Lambert M. The efficacy and effectiveness of psychotherapy. In: Lambert M, editor. Bergin Garfield’s Handb. Psychother. Behav. Chang. 6th ed. New York: Wiley; 2013. p. 169–218.
Freemantle N, Marston L, Walters K, Wood J, Reynolds MR, Petersen I. Making inferences on treatment effects from real world data: propensity scores, confounding by indication, and other perils for the unwary in observational research. BMJ. 2013;347:f6409.
Tschuschke V, Freyberger HJ. Zur aktuellen Situation der Psychotherapiewissenschaft und ihrer Auswirkungen – eine kritische Analyse der Lage.[On the present situation in psychotherapy and its implications – A critical analysis of the facts]. Z Psychosom Med Psychother. 2015;61:122–38.
Cuijpers P, Cristea IA. How to prove that your therapy is effective, even when it is not: a guideline. Epidemiol Psychiatr Sci. 2015;28:1–8.
Hasselhorn HM, Freude G. Der Work Ability Index – ein Leitfaden [The Work Ability Index – a practical guide]. Dortmund/Berlin/Dresden: Bundesanstalt für Arbeitsschutz und Arbeitsmedizin; 2007.
Cieza A, Ewert T, Üstün B, Chatterji S, Kostanjsek N, Stucki G. Development of ICF Core Sets for patients with chronic conditions. J Rehabil Med. 2004;36:9–11.
Acknowledgements
We thank all participating patients, Anita Gutbrod, Petra Beschoner and cooperating occupational consultants, Daniel Mauss, Marc Krueger, Bernhard Reiter, Jutta-Mueller Nuebling and Andreas Woerner for patient recruitment, Gabi Kreutzer-Stierle and Firuzan Sari-Kundt for data management.
Funding
The study was supported by the young scientists programme run by the German network “Health Services Research Baden-Wuerttemberg” of the Ministry for Science, Research and Arts in collaboration with the Ministry for Work and Social Affairs, Family, Women, and Senior Citizens, Baden-Wuerttemberg and by the company Airbus. The work of the Institute of Occupational and Social Medicine and Health Services Research Tuebingen is supported by an unrestricted grant from the employers’ association for the metal and electric industry in Baden-Wuerttemberg (Suedwestmetall).
Availability of data and materials
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request after consultation with the cooperating partners of the study.
Authors’ contributions
EVR, RK, MH, DM, MAR, and HG conceived and designed the study. EVR, EDR, HG, and RK were responsible for the analysis and interpretation of the data. EVR, EDR, MH and DM worked on the acquisition of the data. EVR and HG obtained funding and are the study guarantors. EVR, HG, and RK drafted the manuscript. MAR, EDR, DM, and MH critically revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Competing interests
EVR is senior physician and HG and MH director of a clinic that offers the service of PSIW to interested organisations and companies.
Consent for publication
not applicable.
Ethics approval and consent to participate
The Medical Ethical Board of the University Medical Centre of the University of Ulm gave approval for the study (No224/11). All participants gave written consent to participate.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Rothermund, E., Gündel, H., Rottler, E. et al. Effectiveness of psychotherapeutic consultation in the workplace: a controlled observational trial. BMC Public Health 16, 891 (2016). https://doi.org/10.1186/s12889-016-3567-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-016-3567-y