Abstract
Background
Sarcopenia and obesity have been independently associated with physical function decline, however little information is currently available on the relationship between sarcopenic obesity and physical performance, mainly in middle aged women. The present study aims to estimate the prevalence of sarcopenic obesity and to explore the relationship between sarcopenic obesity and physical performance in middle-aged women from Northeast Brazil.
Methods
A cross-sectional study of women (40–65 years) living in Parnamirim, a city in Northeast Brazil (n = 491). Physical performance was assessed by grip strength, knee extensor and flexor strength (isometric dynamometry), gait speed, and chair stands. Using bioelectrical impedance analysis (BIA), appendicular skeletal muscle mass divided by height squared (kg / m2) was used to define sarcopenia. Waist circumference ≥ 88 cm was defined as abdominal obesity. Sarcopenic obesity was defined as the coexistence of obesity and sarcopenia. The physical performance outcomes were regressed in four groups defined by combinations of sarcopenia and obesity, adjusting for potential confounders (age, education and menopausal status).
Results
Prevalence rates of the four obesity-sarcopenia groups were: Sarcopenic obesity (7.1 %), obesity (67.4 %), sarcopenia (12.4 %) and normal (13 %). Women with sarcopenic obesity had significantly lower grip strength, weaker knee extension and flexion and longer time to raise from a chair compared with non-obese and non-sarcopenic women (p.values < 0.001). Except for the chair stands, these statistically significant differences were also found between sarcopenic obese and obese women. There was no significant difference for gait speed across the four groups (p = 0.50).
Conclusion
Sarcopenic obesity was present in 7 % of this population of middle-aged women from Northeast Brazil and it was associated with poor physical performance. Sarcopenic obesity may occur in middle-aged women with performance limitations beyond pure sarcopenia-related muscle mass or obesity alone.
Similar content being viewed by others
Background
Aging is a continuous process that involves physiological changes in multiple body systems resulting in reduced functional capacity [1]. The musculoskeletal system, involving bodily functions such as muscle contraction, movement and locomotion, is affected by loss of lean mass, particularly muscle mass (sarcopenia) [1].
Progressive muscle mass loss begins around 40 years and it is estimated that it decreases by 8 % every decade [2, 3]. After age 70, this loss rate increases to 15 % per decade [2, 3]. Although these changes have been found in the aging process of both men and women, a decrease in muscle mass does not occur at the same rate and age for both sexes. Study has reported a rapid strength loss in women around the age of 50, which is not observed in men until at least the age of 60 [4]. Menopause occurs during the same middle-aged period and it is associated with the natural decline of estrogen directly reflected in increasing visceral fat mass and decreasing bone density, muscle mass and strength [4]. A higher prevalence of obesity and a decrease in muscle mass are observed during menopause, and these health issues are separately related to a decline in function [5–7].
Furthermore, a higher rate of functional decline has been reported in subjects with sarcopenic obesity (SO), the co-existence of obesity and sarcopenia [8–10]. Lipid infiltration in muscle tissues seems to exacerbate sarcopenia, since accumulation of lipids both prevents incorporation of amino acids and reduces protein synthesis in the muscle [11]. For both men and women, having obesity and sarcopenia together due to a possible synergic effect can further decrease physical functioning [10, 12]. However, changes in body composition, such as obesity and sarcopenia, have been underdiagnosed; and when diagnosed they tend to be more frequent in older women than men [13].
Although sarcopenia and obesity have been independently associated with physical function decline [7, 14], little information is currently available on the relationship between SO and physical performance [10, 12]. Questions remain whether the effects of obesity on physical performance can be detected beyond those of sarcopenia among women that are both obese and sarcopenic. Furthermore, to our best knowledge, no study has examined this relation using objective and valid measures of physical performance and body composition in middle-aged women.
The number of obese people is increasing in Brazil and the current prevalence of excess weight is at least 3-times higher than that of undernutrition [15]. To illustrate, in two recent studies conducted in the south of Brazil [16, 17], two thirds of middle-aged women had abdominal obesity; however, these studies did not look at sarcopenia.
The present study aims to estimate the prevalence of sarcopenic obesity and to explore the relationship between sarcopenic obesity and physical performance in middle-aged women from Northeast Brazil.
Methods
Study population/data collection
This cross-sectional study took place in Parnamirim, a city in the Northeast of Brazil located in Natal’s metropolitan region, the capital of Rio Grande do Norte (RN) state. This city has around 200,000 inhabitants, distributed across 123.5 km2, and is 100 % urbanized.
In this paper, we used baseline data from an ongoing longitudinal research [18]. The longitudinal study aims to analyze the influence of hormone levels on sarcopenia (muscle loss) and physical functioning. The present data were collected between April and November of 2013.
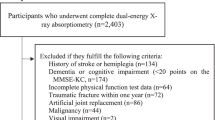
The study population was composed of women living in Parnamirim (40–65 years). Women were recruited by advertisements in all primary care centers across the city. Brazil has universal health care coverage, and all citizens are entitled to register at local neighborhood health centers. The coverage of the primary health care is system is estimated to be 74.5 % in Parnamirim [19]. A convenience sample of five hundred women comprised the baseline study sample. To be eligible to participate in the study, women had to have at least one ovary, with no pituitary or thyroid alterations, without serious neurological diseases that could prevent them from responding to questions, and be free of painful conditions that could compromise the measurement of physical performance outcomes. Women who refused to complete all data collection stages were excluded. Our final sample consisted of 491 women.
All women were evaluated in a single community health center of Parnamirim, RN. The assessments were conducted by trained interviewers using standard protocols.
Ethics
All participants were informed of the objectives and procedures of the research at first contact and signed an informed consent form. The study protocol received approval from the Ethics and Research Committee of the Federal University of Rio Grande do Norte (number: 387.737).
Procedures
Physical performance
Physical performance was assessed by five tests: grip strength, knee extension and flexion strength, gait speed and chair stands. These constituted the dependent variables for this study. Grip strength: the dominant hand was evaluated with a Jamar® dynamometer in the second handle position [20]. The participant was positioned, as recommended by the American Society of Hand Therapists [21], seated with shoulder fully adducted and neutrally rotated, elbow flexed at 90° and forearm in a neutral position. The participants were requested to squeeze the dynamometer with maximal isometric effort without any other body movement, for five seconds. The test was performed three times, with a one-minute interval between measurements. The mean of these three trials was used for analysis.
Knee flexion and extension strength (dominant limb) were measured with the Hoggan® portable dynamometer, MicroFET2® model (isometric dynamometer). The evaluation of extensors was performed with the subject positioned in the prone position on a stretcher, with the knee flexed at 90° and the thigh fixed to the stretcher by an inelastic band. The dynamometer was fixed on the anterior surface of the lower limb, on the line immediately proximal to the malleolus. The evaluation of flexors was carried out in the same position, however with the extended knee and the dynamometer positioned on the posterior surface of the lower limb, immediately above the line of the malleolus. Three maximal isometric contractions of five seconds were requested with one-minute intervals between measurements. The arithmetic mean of the three measurements in kilograms/force (kgf) was considered for analysis [22].
For gait speed, a 4-m walk at the subject’s usual pace was timed. The faster of two walks was used. Gait speed was calculated in meters per second [23, 24].
For the chair stand test, participants were asked to stand up and sit down five times as quickly as possible with arms folded across their chests and were timed in seconds from the initial sitting position to the fifth standing position [23, 24].
Classification of obesity, sarcopenia and sarcopenic obesity
Women with a waist circumference ≥ 88 cm were considered obese, as proposed by Brazilian obesity guidelines [25]. Janssen et al. [26] have described their results suggesting that waist circumference is a better marker of health risk than BMI, and consequently a greater emphasis should be placed on waist circumference in the obesity classification system. Waist circumference may provide an estimate of increased abdominal fat even in the absence of a change in BMI, avoiding some misclassification [26]. Waist circumference (cm) was measured using a “fiber glass” metric tape (divisions of 1 mm) and the measurement point was the mid-way point between the lowest rib and the iliac crests while the subject was standing at the end of normal expiration [27]. Participants were positioned with their feet together, arms crossed over their chest and instructed to relax.
All participants underwent body composition analysis using the same InBody R20 bioelectrical impedance analysis (BIA) machine in compliance with the manufacturer’s instructions. This BIA model is composed of eight electrodes, two for each hand and two for each foot, and performs analysis in 20 and 100 KHz with a current of 250 μA. The body composition was automatically calculated according to predictive equations provided by the manufacturer. The skeletal muscle mass index (SMI) was assessed considering SMI = ASM (sum of appendicular skeletal muscle mass) (kg) / height2 (m). BIA presents good correlation with predictions made by magnetic resonance imaging [28] and Dual-energy X-ray absorptiometry-DEXA [29]. Although it is not the gold standard, it is used in research [30–32], it is a reliable alternative for evaluation of body composition, and it has advantages of being portable, lower cost and not exposing subjects to radiation.
Using the skeletal muscle mass index (SMI) measured by bioelectrical impedance, women were classified as sarcopenic if they had SMI values below the 20th percentile of the sample studied (<6.08 kg / m2) [33, 34]. SO was defined as the coexistence of obesity and sarcopenia [8, 9]. Next, the women were classified into four groups: Obese, sarcopenic, sarcopenic obese, and lastly, non-sarcopenic non-obese women, herein called normal women.
Covariates
Age, sex, marital status, education, income, physical activity and menopausal status were identified as potential confounders of the association between obesity, sarcopenia and physical function, according to the literature on risk factors for physical performance [18, 35, 36].
Demographic and socioeconomic variables
Age was evaluated in years. Education was assessed as years of schooling and then categorized into three groups: less than basic education (up to seven years), between basic and secondary (more than seven and less than eleven years), and secondary or more (eleven years and over). Marital status was classified according to the self-reported presence or absence of a common law union. The race/ethnic group was also declared by the participant as white, black or mixed race (pardo).
Family income was categorized according to the Brazilian minimum monthly wage (MW), which is the lowest remuneration that employers may legally pay workers. Theoretically, this MW should be enough to supply the normal needs of food, housing, clothing, hygiene and transport for a family. At the time of the interview, the MW was R$678.00 (Brazilian Real) per month (approximately $250US dollars/month). However, according to the Statistics and Socioeconomic Studies Department of Brazil (DIEESE) [37], this minimum salary is insufficient. In our study, family income was dichotomized as less than 3 MW and 3 MW or more (3 MW is R$2.034 Brazilian Real, which is equivalent to US$750 dollars). The choice of 3 MW was based on what is considered to be the poverty threshold in the Northeastern region of Brazil [18].
Physical activity
Women were asked if they regularly practiced physical activity. In the event of an affirmative answer, they were asked further about frequency, duration and type of physical activity. To register sedentary activity, women were asked to report how many hours they remained seated in a regular day. This variable was dichotomized into 4 h/day or less and more than 4 h/day [38]. For walking behavior, women were instructed to report how many days per week, and for how long per day they had walked for more than 10 min without stopping during the last week. A walking indicator was constructed to distinguish women walking 90 min/week or more [18].
Menopausal status
Menopausal status was defined using the classification STRAW (Stages of Reproductive Aging Workshop classification) [39] or a self-report of hysterectomy. Women were classified into five groups: premenopausal (regular menses), perimenopausal (irregular menses, with differences in cycle length over seven days or amenorrhea up to one year), postmenopausal (absence of menses for over one year), hysterectomy carried out before 40 years old or after age 40.
Body mass index, hip-waist ratio and skeletal muscle mass index
Weight (kg) was measured by the Wiso® W903 digital scale and height (m) by a stadiometer. To measure hip circumference (cm), a fiber glass® metric tape was used and the hip measurement was the largest horizontal circumference around the hips. Waist-hip ratio was calculated by dividing these variables (waist/hip) [27]. Body mass index (BMI) was calculated by dividing body weight by height squared (kg/m2). The skeletal muscle mass index (SMI) was assessed considering SMI = ASM (sum of appendicular skeletal muscle mass) (kg) / height2 (m) [33], by an InBody R20 BIA machine.
Data analysis
We started the data analysis with a descriptive analysis of the sample. Means and standard deviations of quantitative variable frequencies of categorical variables were estimated. We utilized Analysis of Variance (ANOVA) methods to compare the mean of physical performance measures across the four normal, obese, sarcopenic and sarcopenic obese groups. We used the Kolmogorov-Smirnov test to evaluate the normality of the data. The post-hoc multiple comparisons Bonferroni test was used to verify which of these four groups were significantly different from each other. Finally, we constructed multivariate linear regression models to estimate the mean of physical performance measures in each of the four groups, adjusting for potential confounders. The potential confounders were identified according to the literature and bivariate analyses (p < 0.20) of their relationships with physical performance measures. All analyses were conducted using SPSS version 20.0 (SPSS, Chicago, IL, USA).
Results
The total sample characteristics are shown in Table 1. The sample consisted of 491 women with a mean age of 49.95 ± 5.56 years. Approximately 70 % were married or living in common law unions and 55 % were of mixed ethnic groups. Nearly 41 % had less than primary education, and 70 % were living below the poverty threshold of 3 MW. Almost 75 % reported no regular physical activity.
Table 2 shows the sample distributions for categorical variables by groups of obese women (67.4 %), normal (13 %), sarcopenic (12.4 %) and sarcopenic obese (7.1 %). No significant differences between the four groups were found according to socioeconomic status or health behaviors. SO was more prevalent among the women who had had a hysterectomy and among the premenopausal women than among peri and post-menopausal women (p < 0.05).
In multiple comparisons using Bonferroni correction, all differences in body distribution variables across the four groups were significant, except differences in BMI between normal women (25.18 ± 2.06) and sarcopenic obese (26.23 ± 2.68) (p = 0.98); in waist/hip between obesity and SO (p = 1.00); and in skeletal muscle mass between sarcopenia and SO (p = 1.00) (Table 3).
Table 4 summarizes the results of adjusted and unadjusted analyses of the physical performance variables across the groups. Age, education and menopausal status were considered potential confounders according to the literature and the bivariate analyses, since they were associated with obesity/sarcopenia groups (p < 0.20). There were significant differences between groups in strength (grip strength, knee flexor and extensor strength) and timed chair stands: women classified as sarcopenic obese had the worst physical performance, with lowest mean values for strength variables and the longest time for the timed chair stands. Average gait speed was not different across groups (p = 0.50).
Multiple comparisons showed that in general, women with sarcopenia had significantly worse performance than obese women (grip strength p < 0.001; knee flexor strength p < 0.003; knee extensor strength p < 0.001). SO women showed lower mean values than obese women in all strength variables (p < 0.001) (Table 4). It also appears that obesity and sarcopenia impose a synergic ill effect on physical performance. It is best demonstrated when we look at differences in times for chair stands. For sarcopenic obese women, it took an average of 1.18 (that is, 10.89–9.71) seconds longer than normal women to stand, which is more than what would be expected by adding the 0.40 (that is, 10.11–9.71) excess time of obese women compared to normal women, and 0.05 (that is, 9.76–9.71), the corresponding excess time for sarcopenic women.
Discussion
Summary of results
Sarcopenic obesity (SO) was relatively frequent and associated with poor physical performance in middle-aged women from Northeast Brazil. Women with SO had significantly lower grip strength and knee extension and flexion strength when compared with normal and obese women. Although not statistically significant, women with SO tended to have lower values in the three muscle strength indicators (grip strength, knee extension and flexion strength), compared with sarcopenic non-obese women. Concerning chair stands, sarcopenic obese women did not differ from obese women, but it took them longer to raise from a chair than non-obese women with or without sarcopenia.
Prevalence findings
The prevalence of SO in our study was 7.1 %. Due to the lack of a standard definition for SO, it is difficult to compare its prevalence across populations. In addition, in the eyes of clinicians and researchers, SO is more a problem for older women and has seldom been studied in middle-aged women. The few existing studies report wide-ranging results. A Korean study found that the prevalence of SO varies from 0.8 to 11.8 % in women between 40 and 59 years, according to different indices of definition [40]. Among older women, the prevalence of SO has been as high as 19.2 % in Taiwanese women (mean age: 63.3 years) [41] and 21.5 % in Brazilian women (mean age: 67.2 years) [42]. Furthermore, the prevalence rate of SO in Canadian women aged 68–82 years old was 10.8 % [43], close to the prevalence of 9.2 % in post-menopausal European women (mean age 57.4 years) [44]. The muscle mass can be influenced by age, height, body weight and ethnicity, but also by nutrition and life course exposure to social and economic adversity [45, 46]. Ethnicity and social and economic life course adversity are often difficult to separate. As an illustration, elderly Mexicans have less muscle and greater total fat than New York dwelling Caucasians, but researchers were unable to separate the ethnic and socioeconomic influences [47].
Obesity is increasing in Brazilian female adolescents and women without a marked socioeconomic gradient [15]. The high prevalence of obesity in our study population is in the range of what has been reported in the literature for adult women in Northeast Brazil [48–50]. Andrade et al. [51] found a similar prevalence of 55.5 % (≥88 cm), based on waist circumference in women with a mean age of 39.9 years [51].
Concerning sarcopenia, in a study conducted in France, the prevalence was 9 % for individuals between 45 and 54 years, 13.5 % in the group aged between 55 and 64 years, and reaching 64.3 % in those aged 85 years or older, with no difference between men and women, indicating that sarcopenia is already present in middle-aged populations. Sarcopenia was negatively associated with BMI, although the authors did not report on SO [52].
Findings on grip strength
Low muscle mass predisposes physical function decline and increases the risk of falls, disability, poor quality of life and mortality [53, 54]. It has been suggested that SO could exert a synergistic impact on physical performance of the elderly [12].
In concordance with a recent Brazilian study of older women, we found that SO is associated with reduced grip strength [1]. Two additional studies support our results. First, Lim et al. [55] found significant difference between these four sarcopenic-obesity groups in older Asian women from Singapore and concluded that obesity coupled with sarcopenia results in worsening of performance and strength parameters, including grip strength [55]. Second, Baumgartner et al. [56] observed the lowest grip strength among sarcopenic obese men and women of 60 years and greater in a United States population, corroborating our results [56].
Previous research indicates that obese people have higher absolute muscle strength and a similar or higher ‘strength to muscle size ratio’ compared to their lean counterparts [57]. However, the disabling effect of excess fat mass may reduce motor performance of complex motor tasks that require body mass support or mobilization [57, 58]. Non-sarcopenic and sarcopenic obese women may be considered an apparently homogenous group of obese women; however, they have very different physical performance because of their muscle mass. We are in agreement with Newman et al. [54], who highlighted the importance of detecting obese individuals who do not appear to be sarcopenic, but in fact their muscle mass is reduced for their body size and this reduction is masked by obesity [54].
Lower limb strength findings
We found lower limb strength differs between the groups, with obese women showing similar results as normal women, while sarcopenic obese women presented the worst performance. Miyatake et al. [59] showed the absolute isometric strength of knee extensors was higher in obese adults (20–60 years) compared to non-obese controls [59]. Moreover, Rolland et al. [60] showed that active obese elderly produced higher relative strength per unit muscle size than non-obese, while sedentary obese older adults had similar muscle strength compared to non-obese [60]. Consequently, favourable adaptations to excess body mass on muscle function might depend on the maintenance of sufficient physical activity during aging. However in our study, the four groups reported similar practice of regular physical activity, sedentary and walking behaviours. The reason that in our sample obese participants showed the same strength as normal women might be due to the fact that all have the same level of physical activity (Table 2).
Findings on chair stands
Unlike strength variables, obese and sarcopenic obese women took longer time for chair stands compared with normal and sarcopenic women. Chair stands is an activity in which the body sequentially displaces itself in the shortest time possible and requires more than strength; it also involves muscle power and coordination [57, 58]. For chair stands, the SO women performed even worse than the sarcopenic, which corroborates reviewed studies stating that central fat and relative loss of fat-free mass can determine the health risk associated with obesity at older ages [61]. Sarcopenia and obesity may act synergistically, leading to functional and metabolic changes [62], and our results provide evidence for this synergism by showing the decline in the chair standing performance in SO participants. Waters et al. [63] found several functional deficits in the SO group relative to normal, sarcopenic and obese women, with the worst performance on the chair stands test by SO. However, Lim et al. [55] found no significant difference across groups in this test, despite a longer observed time in the SO group [55].
Gait speed findings
We did not find any significant differences in gait speed across groups despite the fact that high intermuscular fat in the thigh is a known predictor of gait-speed decline [64]. Fat infiltration into muscle contributes to the loss of mobility associated with aging, and decreasing thigh muscle area is also predictive of decline in gait speed [64].
The observed lowest mean values of gait speed in women with SO, albeit non-significant, may reflect on their functional capacity and quality of life in the near future. While Meng et al. [10] found an absence of association between gait speed and the groups (obesity, sarcopenia and SO) in older women [10], Lim et al. [55] reported lower gait speed in sarcopenic obese older Asian men and women (≥65 years) from Singapore [55].
Limitations and strengths
Our research has some limitations. The participants were middle-aged women from Northeast Brazil, therefore caution should be used in inferring the results to other populations. Firstly, cross cultural comparisons of prevalence and distribution of SO are difficult due to variability in body sizes and body composition, as well as the lack of standard protocols in diagnosis of SO. This diagnosis is usually based on combinations of body composition indices and muscle mass with varying population specific cut-off points, as is usually recommended to study of diverse populations [47]. Second, we used a convenience sample and our participants might have been healthier than the average target population. The possibility of healthy volunteer bias cannot be ruled out. However, education and income of the study sample is similar to the census data for the women of similar ages residing in the city of Parnamirim. Lastly, there is a possibility of information bias due to self-reported measures of health behaviors; however, since there is no reason to think that this bias is related to physical performance, the misclassifications are probably non-differentiatial.
The main strength of this study is its focus on a very rarely studied condition-sarcopenic obesity-in lower income middle-aged women. Objective measurement of physical performance and body composition by valid, non-invasive, and inexpensive tools is another strength of this study.
Relevant clinical implications
Obesity associated with sarcopenia seems to worsen physical performance, beyond what has been reported by obesity or sarcopenia alone. Although the differences between the groups were relatively small, it has been shown in the literature that changes in chair stand performance, for example, provide a marker of current health and were predictive of mortality among middle-aged women in a ten years period [65], and also predictive of disability in older adults [23].
Investigation of sarcopenia and sarcopenic obesity should be considered in the clinical assessment of menopausal women. Furthermore, preventive measures and/or rehabilitation in relation to SO need to be implemented to decrease the ill effects of SO.
Conclusion
Sarcopenic obesity was relatively frequent in middle-aged women from Northeast Brazil, and it was associated with poor physical performance. Sarcopenic obesity may occur in middle-aged women with subsequent performance limitations beyond sarcopenia—related muscle mass or obesity alone.
The number of obese women is rapidly increasing in many Latin America countries and a substantial proportion of middle-aged women may be affected both by obesity and low muscle mass. It is anticipated that SO will be a future public health burden.
Most studies on SO have been conducted in older adults. Further research in the etiology and onset of SO in middle-aged women is needed. These studies may include longitudinal data to confirm our cross-sectional findings. Furthermore, an assessment of the efficacy of interventions to maintain muscle mass and strength in this age group should be carried out.
Abbreviations
- BIA:
-
bioelectrical impedance analysis
- BMI:
-
body mass index
- MW:
-
monthly wage
- SMI:
-
skeletal muscle mass index
- SO:
-
sarcopenic obesity
- WHO:
-
world health organization
- STRAW:
-
stages of reproductive aging workshop classification
References
Silva Neto LS, Karnikowiski MGO, Tavares AB, Lima RM. Associação entre sarcopenia, obesidade sarcopênica e força muscular com variáveis relacionadas de qualidade de vida em idosas. Brazilian J Phys Ther. 2012;16:360–7.
Kim TN, Choi KM. Sarcopenia: definition, epidemiology, and pathophysiology. J bone Metab. 2013;20:1–10.
Grimby G, Saltin B. The ageing muscle. Clin Physiol. 1983;3:209–18.
Maltais ML, Desroches J, Dionne IJ. Changes in muscle mass and strength after menopause. J Musculoskelet Neuronal Interact. 2009;9:186–97.
Barbosa AR, Souza JMP, Lebrão ML, de Marucci MFN. Estado nutricional e desempenho motor de idosos de São Paulo. Rev Assoc Med Bras. 2007;53:75–9.
Vilaça KHC, Carneiro JAO, Ferriolli E, da Lima NKC, de Paula FJA, Moriguti JC. Body composition, physical performance and muscle quality of active elderly women. Arch Gerontol Geriatr. 2014;59:44–8.
Jensen GL. Obesity and functional decline: epidemiology and geriatric consequences. Clin Geriatr Med. 2005;21:677–87.
Zamboni M, Mazzali G, Fantin F, Rossi A, Di Francesco V. Sarcopenic obesity: a new category of obesity in the elderly. Nutr Metab Cardiovasc Dis. 2008;18:388–95.
Prado CMM, Wells JCK, Smith SR, Stephan BCM, Siervo M. Sarcopenic obesity: a critical appraisal of the current evidence. Clin Nutr. 2012;31:583–601.
Meng P, Hu YX, Fan L, Zhang Y, Zhang MX, Sun J, et al. Sarcopenia and sarcopenic obesity among men aged 80 years and older in Beijing: prevalence and its association with functional performance. Geriatr Gerontol Int. 2014;14(1):29–35.
Parr EB, Coffey VG, Hawley JA. “Sarcobesity”: a metabolic conundrum. Maturitas. 2013;74:109–13.
Chang CI, Huang KC, Chan DC, Wu CH, Lin CC, Hsiung CA, et al. The impacts of sarcopenia and obesity on physical performance in the elderly. Obes Res Clin Pract. 2014;9:256–65.
Chung JY, Kang HT, Lee DC, Lee HR, Lee YJ. Body composition and its association with cardiometabolic risk factors in the elderly: a focus on sarcopenic obesity. Arch Gerontol Geriatr. 2013;56:270–8.
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147:755–63.
Conde WL, Monteiro CA. Nutrition transition and double burden of undernutrition and excess of weight in Brazil. Am J Clin Nutr. 2014;100:1617S–22.
Theodoro H, Rodrigues AD, Mendes KG, Liane RH, Paniz VMV, Olinto MTA. Reproductive characteristics and obesity in middle-aged women seen at an outpatient clinic in southern Brazil. Menopause. 2012;19:1022–8.
Gravena AAF, Brischiliari SCR, Lopes TCR, Agnolo CMD, Carvalho MDB, Pelloso SM. Excess weight and abdominal obesity in postmenopausal Brazilian women: a population-based study. BMC Womens Health. 2013;13:46.
Da Câmara SMA, Zunzunegui MV, Pirkle C, Moreira MA, Maciel ÁCC. Menopausal status and physical performance in middle aged women: a cross-sectional community-based study in northeast Brazil. PLoS One. 2015;10, e0119480.
Brazil. IDSUS-Índice de Desempenho do Sistema Único de Saúde [Internet]. 2011. Available from http://idsus.saude.gov.br/mapas.html. Accessed 20 May 2015.
Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C, et al. A review of the measurement of grip strength in clinical and epidemiological studies: Towards a standardised approach. Age Ageing. 2011;40:423–9.
Fess E. Grip Strength. 2nd ed. Chicago: American Society of Hand Therapists; 1992.
Martin HJ, Yule V, Syddall HE, Dennison EM, Cooper C, Aihie SA. Is hand-held dynamometry useful for the measurement of quadriceps strength in older people? a comparison with the gold standard Bodex dynamometry. Gerontology. 2006;52:154–9.
Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–61.
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94.
Godoy-Matos AF, Oliveira J, Guedes EP, Carraro L, Lopes AC, Mancini MC, et al. Diretrizes brasileiras de obesidade, ABESO-Assoc. Bras. para o Estud. da Obesidade e da Síndrome Metabólica. Itapevi: AC Farmacêutica; 2009. p. 11–4.
Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr. 2004;79:379–84.
Lean ME, Han TS, Morrison CE. Waist circumference as a measure for indicating need for weight management. BMJ. 1995;311:158–61.
Janssen I, Heymsfield SB, Baumgartner RN, Ross R. Estimation of skeletal muscle mass by bioelectrical impedance analysis. J Appl Physiol. 2000;89:465–71.
Malavolti M, Mussi C, Poli M, Fantuzzi AL, Salvioli G, Battistini N, et al. Cross-calibration of eight-polar bioelectrical impedance analysis versus dual-energy X-ray absorptiometry for the assessment of total and appendicular body composition in healthy subjects aged 21–82 years. Ann Hum Biol. 2003;30:380–91.
Ruiz JR, Segura-Jiménez V, Ortega FB, Alvarez-Gallardo IC, Camiletti-Moirón D, Aparicio VA, et al. Objectively measured sedentary time and physical activity in women with fibromyalgia: a cross-sectional study. BMJ Open. 2013;3, e002722.
Carbonell-Baeza A, Ruiz JR, Aparicio VA, Ortega FB, Munguía-Izquierdo D, Alvarez-Gallardo IC, et al. Land- and water-based exercise intervention in women with fibromyalgia: the al-Andalus physical activity randomised controlled trial. BMC Musculoskelet Disord. 2012;13:18.
do Sales ATN, de Fregonezi GAF, Silva AGCB, Ribeiro CTD, Dourado-Junior MET, Sousa AGP, et al. Identification of peripheral arterial disease in diabetic patients and its association with quality of life, physical activity and body composition. J Vasc Bras. 2015;14:46–54.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing. 2010;39:412–23.
Pagotto V, Silveira EA. Methods, diagnostic criteria, cutoff points, and prevalence of sarcopenia among older people. ScientificWorldJournal. 2014;2014:231312.
de Sousa ACPA, Guerra RO, Thanh Tu M, Phillips SP, Guralnik JM, Zunzunegui MV. Lifecourse adversity and physical performance across countries among men and women aged 65–74. PLoS One. 2014;9, e102299.
Koh ES, Jang SN, Paik NJ, Kim KW, Lim JY. Age and gender patterns in associations between lifestyle factors and physical performance in older Korean adults. Arch Gerontol Geriatr. 2014;59:338–45.
Brazil. Salário mínimo nominal e necessário (julho) [Internet]. DIEESE. 2014. Available from: http://www.dieese.org.br/analisecestabasica/salarioMinimo.html. Accessed 3 Sep 2014.
Gómez-Cabello A, Vicente-Rodríguez G, Pindado M, Vila S, Casajús JA, de la Fuente PF, et al. Increased risk of obesity and central obesity in sedentary postmenopausal women. Nutr Hosp. 2012;27:865–70.
Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, et al. Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging. J Clin Endocrinol Metab. 2012;97:1159–68.
Kim TN, Yang SJ, Yoo HJ, Lim KI, Kang HJ, Song W, et al. Prevalence of sarcopenia and sarcopenic obesity in Korean adults: the Korean sarcopenic obesity study. Int J Obes (Lond). 2009;33:885–92.
Lu CW, Yang KC, Chang HH, Lee LT, Chen CY, Huang KC. Sarcopenic obesity is closely associated with metabolic syndrome. Obes Res Clin Pract. 2013;7:e301–7.
Dos Santos EP, Gadelha AB, Safons MP, Nóbrega OT, Oliveira RJ, Lima RM. Sarcopenia and sarcopenic obesity classifications and cardiometabolic risks in older women. Arch Gerontol Geriatr. 2014;59:56–61.
Bouchard DR, Dionne IJ, Brochu M. Sarcopenic/obesity and physical capacity in older men and women: data from the nutrition as a determinant of successful aging (NuAge)-the Quebec longitudinal study. Obesity (Silver Spring). 2009;17:2082–8.
Monteiro MA, Gabriel RC, Sousa MF, Castro MNE, Moreira MH. Temporal parameters of the foot roll-over during walking: influence of obesity and sarcopenic obesity on postmenopausal women. Maturitas. 2010;67:178–85.
Vadiveloo M, Dixon LB, Mijanovich T, Elbel B, Parekh N. Dietary variety is inversely associated with body adiposity among US adults using a novel food diversity index. J Nutr. 2015;145:555–63.
Bann D, Cooper R, Wills AK, Adams J, Kuh D. Socioeconomic position across life and body composition in early old age: findings from a British birth cohort study. J Epidemiol Community Health. 2014;68:516–23.
Aleman Mateo H, Lee SY, Javed F, Thornton J, Heymsfield SB, Pierson RN, et al. Elderly Mexicans have less muscle and greater total and truncal fat compared to African-Americans and Caucasians with the same BMI. J Nutr Health Aging. 2009;13:919–23.
Abrantes MM, Lamounier JA, Colosimo EA. Prevalência de sobrepeso e obesidade nas regiões Nordeste e Sudeste do Brasil. Rev Assoc Med Bras. 2003;49:162–6.
Montenegro NAN, da Silva SOM, de Medeiros DAC, da Silva PA, da Silva MDP, Knackfuss IM. Estado nutricional alterado e sua associação com perfil lipídico e hábitos de vida em idosos hipertensos. Arch Latinoam Nutr. 2008;58:350–6.
Tribess S, Virtuoso Junior JS, Petroski ÉL. Estado nutricional e percepção da imagem corporal de mulheres idosas residentes no nordeste do Brasil. Cien Saude Colet. 2010;15:31–8.
Rivera-Andrade A, Luna MA. Trends and heterogeneity of cardiovascular disease and risk factors across Latin American and Caribbean countries. Prog Cardiovasc Dis. 2014;57:276–85.
Cherin P, Voronska E, Fraoucene N, de Jaeger C. Prevalence of sarcopenia among healthy ambulatory subjects: the sarcopenia begins from 45 years. Aging Clin Exp Res. 2014;26:137–46.
Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. 2002;50:889–96.
Newman AB, Haggerty CL, Goodpaster B, Harris T, Kritchevsky S, Nevitt M, et al. Strength and muscle quality in a well-functioning cohort of older adults: the health, aging and body composition study. J Am Geriatr Soc. 2003;51:323–30.
Lim JP, Leung BP, Ding YY, Tay L, Ismail NH, Yeo A, et al. Monocyte chemoattractant protein-1: a proinflammatory cytokine elevated in sarcopenic obesity. Clin Interv Aging. 2015;10:605–9.
Baumgartner RN. Body composition in healthy aging. Ann N Y Acad Sci. 2000;904:437–48.
Maffiuletti NA, Ratel S, Sartorio A, Martin V. The impact of obesity on in vivo human skeletal muscle function. Curr Obes Rep. 2013;2:251–60.
Hergenroeder AL, Brach JS, Otto AD, Sparto PJ, Jakicic JM. The influence of body mass index on self-report and performance-based measures of physical function in adult women. Cardiopulm Phys Ther J. 2011;22:11–20.
Miyatake N, Fujii M, Nishikawa H, Wada J, Shikata K, Makino H, et al. Clinical evaluation of muscle strength in 20–79-years-old obese Japanese. Diabetes Res Clin Pract. 2000;48:15–21.
Rolland Y, Lauwers-Cances V, Pahor M, Fillaux J, Grandjean H, Vellas B. Muscle strength in obese elderly women: effect of recreational physical activity in a cross-sectional study. Am J Clin Nutr. 2004;79:552–7.
Zamboni M, Mazzali G, Zoico E, Harris TB, Meigs JB, Di Francesco V, et al. Health consequences of obesity in the elderly: a review of four unresolved questions. Int J Obes. 2005;29:1011–29.
Lim S, Kim JH, Yoon JW, Kang SM, Choi SH, Park YJ, et al. Sarcopenic obesity: prevalence and association with metabolic syndrome in the Korean Longitudinal Study on Health and Aging (KLoSHA). Diabetes Care. 2010;33:1652–4.
Waters DL, Hale L, Grant AM, Herbison P, Goulding A. Osteoporosis and gait and balance disturbances in older sarcopenic obese New Zealanders. Osteoporos Int. 2010;21:351–7.
Beavers KM, Beavers DP, Houston DK, Harris TB, Hue TF, Koster A, et al. Associations between body composition and gait-speed decline: results from the health, aging, and body composition study. Am J Clin Nutr. 2013;97:552–60.
Kuh D, Karunananthan S, Bergman H, Cooper R. A life-course approach to healthy ageing: maintaining physical capability. Proc Nutr Soc. 2014;73:237–48.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
MAM, MVZ and ACCM contributed to the conception and design of the present study and analysis plan. MAM, MVZ and AV analyzed the data with feedback from all authors. MAM, MVZ and AV also wrote the manuscript. MAM, SMAC and TSO contributed to the acquisition of data. All authors contributed to the interpretation of the data and to critical review of the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Moreira, M.A., Zunzunegui, M.V., Vafaei, A. et al. Sarcopenic obesity and physical performance in middle aged women: a cross-sectional study in Northeast Brazil. BMC Public Health 16, 43 (2015). https://doi.org/10.1186/s12889-015-2667-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-015-2667-4