Abstract
Background
The demographic characteristics of pandemic influenza decedents among middle and low-income tropical countries are poorly understood. We explored the demographics of persons who died with influenza A (H1N1)pdm09 infection during 2009–2010, in seven countries in the American tropics.
Methods
We used hospital-based surveillance to identify laboratory-confirmed influenza deaths in Costa Rica, El Salvador, Guatemala, Honduras, Nicaragua, Panama and Dominican Republic. An influenza death was defined as a person who died within two weeks of a severe acute respiratory infection (SARI) defined as sudden onset of fever >38 °C, cough or sore-throat, and shortness of breath, or difficulty breathing requiring hospitalization, and who tested positive for influenza A (H1N1)pdm09 virus by real time polymerase chain reaction. We abstracted the demographic and clinical characteristics of the deceased from their medical records.
Results
During May 2009-June 2010, we identified 183 influenza deaths. Their median age was 32 years (IQR 18–46 years). One-hundred and one (55 %) were female of which 20 (20 %) were pregnant and 7 (7 %) were in postpartum. One-hundred and twelve decedents (61 %) had pre-existing medical conditions, (15 % had obesity, 13 % diabetes, 11 % asthma, 8 % metabolic disorders, 5 % chronic obstructive pulmonary disease, and 10 % neurological disorders). 65 % received oseltamivir but only 5 % received it within 48 h of symptoms onset.
Conclusions
The pandemic killed young adults, pregnant women and those with pre-existing medical conditions. Most sought care too late to fully benefit from oseltamivir. We recommend countries review antiviral treatment policies for people at high risk of developing complications.
Similar content being viewed by others
Background
Early in the pandemic, the epidemiologic and clinical characteristics of influenza A (H1N1)pdm09 were poorly understood. Pending information about this emerging pathogen, influenza prevention and control policies in the American tropics still targeted persons at risk of developing complications as a result of seasonal influenza disease (e.g. children aged < 5 years, persons with certain chronic medical conditions, and persons aged ≥ 65 years) [1]. For example, health officials worried that physiologic changes during pregnancy and the postpartum period would place women at risk for developing complications as a result of pandemic influenza illness [2–4].
At the start of the pandemic, Central American countries used CDC’s Guidelines for Treatment of Suspected Cases of Influenza A(H1N1)pdm09 [5]. At the end of 2009, Central America countries sought to implement the PAHO treatment recommendations developed in July 2009 [6]. These recommendations prioritized the early use of oseltamivir among children, older adults, pregnant women and people with chronic diseases [7–11]. Health officials used television, print and radio to urge persons presumed to be at high-risk who developed sudden onset fever, cough or sore throat, and all persons who developed danger signs (e.g. respiratory difficulty), to seek timely care [7, 12, 13]. Risk communication messages urged the people to seek medical care, but only Nicaragua, Panamá and Guatemala, explicitly recommended that to people at high risk of developing complications from influenza illness [14–17]. National guidelines recommended to treat patients with oseltamivir when it was most effective (i.e. within 48 h from symptom onset) [1, 7, 9, 11, 18, 19].
WHO also recommended to the countries vaccinate pregnant women and other high risk persons against pandemic influenza [20]. To accomplish this, WHO provided three shipments of donated monovalent influenza A(H1N1)pdm09 vaccine to 4 of the 7 countries in Central America during March 2010. This donation was the only source of influenza vaccine for public health sector and allowed for a vaccination coverage of 14–34 % among the general population in Central America (El Salvador: 2,2 million doses, coverage: 34 %; Guatemala: 1,3 million doses, coverage: 10 %; Honduras: 1,7 million doses, coverage: 24 %; Nicaragua: 750,000 doses, coverage: 14 %) [21].
Pharmaceutical interventions in middle and low income countries of the American tropics were in limited supplies or only available late during the pandemic. In Central America, while in some countries social security coverage is almost universal, in others is as low as 12 %. Investment in health varies between 5-11 % of gross domestic product, the density of beds varies 0.7-2.4 per 1000 inhabitants; physician density 0.4-1.9 per 1000 inhabitants; and rural population of 25–50 % [22]. In this manuscript we explore the impact of the pandemic in Central America and the Dominican Republic through a description of the demographics, clinical characteristics, and oseltamivir treatment of persons who died with laboratory-confirmed influenza A(H1N1)pdm09.
Methods
Case identification
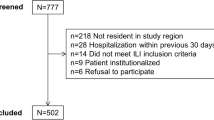
In 2007, the Ministries of Health of Central America and the Dominican Republic implemented the PAHO-CDC Generic Protocol for Influenza Surveillance to identify influenza among severe acute respiratory infection (SARI) cases (defined as sudden onset fever >38 °C, cough or sore-throat, and shortness of breath or difficulty breathing requiring hospitalization) [23]. Cases were tested for influenza through immunofluorescence and real-time reverse transcription-polymerase chain reaction. Starting April 2009, countries also documented laboratory-confirmed influenza A(H1N1)pdm09 SARI cases that died in hospital within two weeks from illness onset. We used hospital-based surveillance to identify laboratory-confirmed influenza deaths in Costa Rica, El Salvador, Guatemala, Honduras, Nicaragua, Panama and Dominican Republic. SARI decedents were identified through event-based surveillance and outbreak response activities. Upon identifying potential cases, health authorities reviewed clinical records and autopsy reports to determine if decedents had indeed met the SARI case-definition.
We defined women of reproductive age as those aged between 15–49 years. We categorized pregnant women who developed respiratory illness before delivery as “pregnant” and those who developed respiratory illness within 42 days of delivery as “postpartum” cases. We categorized a case as obese if such a diagnosis was recorded in their medical record or if height and weight information were available and the body mass index exceeded 30 kg/m2.
Data collection
We collected data using standardized questionnaires, from May 2009 to June 2010. Health authorities systematically obtained demographic (e.g. age and sex) and clinical information (e.g. date of illness onset, health seeking behavior, treatment with oseltamivir, history of pre-existing medical conditions, symptoms, signs, laboratory, radiology, and pathology findings) from SARI decedents associated with influenza A(H1N1)pdm09 from clinical records (by reviewing the medical records of hospitals, outpatient clinic records and referral sheets which were available) and obtaining information from relatives, and surveillance data.
Ethics
The review of the clinical records was performed in the context of the pandemic outbreak for the characterization of the first 100 cases, following recommendations of WHO. For the emergency, at that moment, was no required approval for IRB. Approvals by Ministries of Health consisted of administrative permission to access medical records. The review of medical records was performed and with the accompaniment of officials of the Ministries of Health. No patient identifiers were received or used for analysis.
Analyses
We summarized demographic and clinical characteristics of decedents associated with influenza A(H1N1)pdm09 using proportions to compare both, as the participation of each country and as the age groups, with variables of interest (ie. Percentage of pregnant and postpartum women, underlying medical conditions and treatment). We stratified the analyses into three age groups (i.e. 0–18, 19–64 and ≥65 years). We conducted Chi-square, t-tests and analysis of variance tests for comparisons when appropriate. We eliminated missing data from the calculations, buy declared in the results section.
We verify the check list for observational studies from the STROBE Statement.
Results
Epidemiologic and demographic case characteristics
During epidemiological week (EW) 19 in 2009 through EW 25 in 2010, we identified 183 SARI decedents who tested positive for influenza A(H1N1)pdm09 in seven countries (Belize did not identify any influenza A(H1N1)pdm09 deaths). The first case was identified in Costa Rica during EW 19. Influenza A(H1N1)pdm09 deaths peaked during EW 30 (Fig. 1). Forty percent (74 cases) of the 183 decedents were identified in Costa Rica, 17 % (32 cases) in El Salvador, 11 % (21 cases) in Dominican Republic, 10 % (18 cases) in Honduras, 9 % (17 cases) in Guatemala, 7 % (12 cases) in Panama, and 5 % (9 cases) in Nicaragua (Table 1).
The median age among cases was 32 years (interquartile range: 18–46 years). Children aged <5 years represented 16 % (29 cases) and persons aged 15–44 years represented 48 % (88 cases) and persons aged >65 years represented 9 % (17 cases) of the 183 deaths. El Salvador had the lowest median age (15 years) and Costa Rica the highest (41 years) among decedents (Table 1). In El Salvador, cases aged <5 years were most prevalent (45 %) while in Guatemala cases aged 35–44 years (35 %).
Seventeen (9 %) of 183 cases had a history of smoking. Among 112 cases (61 %) with a pre-existing medical condition, 27 (15 %) were obese, 23 (13 %) had diabetes, 20 (11 %) had asthma, 15 (8 %) had other chronic metabolic diseases, 10 (5 %) had chronic obstructive pulmonary disease, 11 (6 %) had seizure disorder, and 7 (4 %) had cerebral palsy. Underlying medical conditions were identified in 38 % of cases <5 years old, in 61 % of cases aged 5–59 years old, and in all cases with 60 or more years old (Table 2). Among cases aged <18 years, seizure disorders (reported among 7 of 46 cases [15 %]) and asthma (6 cases [13 %]) were the most common pre-existing medical conditions. Among cases aged 18–64 years, obesity (24 of 120 cases [20 %]) and diabetes mellitus (19 cases [16 %]) were the most common. Among cases aged ≥65 years, diabetes mellitus (4 cases of 17 [24 %]) was the most common pre-existing medical condition. Cases with underlying medical conditions were older (mean age 37 years) than those without underlying medical conditions (mean age 26 years) (p < 0.01).
One hundred and one (55 %) of 183 the decedents were female. Of the 101 female decedents, 61 (60 %) were women of reproductive age. Thirty-three percent (20 cases) of women of reproductive age who died were pregnant, and 7 (12 %) were in their puerperium. El Salvador reported that all women of reproductive age who died were maternal deaths, Guatemala reported 5 (71 %) of 7, and Honduras reported 5 (63 %) of 8 were maternal deaths.
Nearly half (48 %) of the pregnant women were in their third trimester, 24 % in the second trimester, and 24 % did not have a gestational age recorded. Fourteen (52 %) of 27 maternal deaths had other underlying medical condition (i.e. 5 (18 %) had asthma, 3 (11 %) had cardiac disease, 2 [7 %] had obesity, 2 [7 %] had chronic lung disease, 2 [7 %] had diabetes and 1 [4 %] AIDS) (Table 2). The proportion of pre-existing medical conditions between maternal deaths and cases without pregnancy were similar, except for the proportion with chronic cardiac disease which was higher among maternal deaths (11 % [3/27] cases) when compared to non-pregnant women (3 % [4/156], p = 0.03). The average age of maternal deaths was 29 years.
Clinical, laboratory, radiology, and pathology characteristics
One hundred and fifty-one (82 %) of 183 decedents had a history of fever before their first contact with a clinic, but only 85 (46 %) had documented fever during admission. Dyspnea was reported in only 124 (68 %) of cases during admission.
Seventy five (41 %) of 183 cases had a chest x-rays (CXR) during their illness, of which 71 % had consolidation 53 % had interstitial findings. Five (28 %) of the 18 cases with interstitial infiltrates subsequently developed consolidation during hospitalization. Sixteen (9 %) of the 183 cases had autopsy reports, of which 11 (69 %) had cardiomegaly, 5 (31 %) intra-alveolar hemorrhage, 4 (25 %) neutrophilic bronchopneumonia, and 4 (25 %) cerebral edema.
Timing of health seeking and oseltamivir use
Decedents sought care a median of 4 days (IQR 1–5 days) after symptom onset. The median duration between health seeking and death was 14 days (IQR 6–17 days). There was no statistically significant difference in the average amount of time elapsed between symptom onset and health seeking by age groups (p = 0.4), or country (p = 0.2). Overall, one hundred nineteen (65 %) out of the 183 cases received treatment with oseltamivir, (Table 3) but there was variability in the proportion treated depending on the country where they lived (range 25–89 %). Of the 119 that received oseltamivir, only 10 (5 %) received it within the first 48 h of onset of symptoms, and 21 (11 %) within the first 72 h (Table 3). Twenty (74 %) of 27 pregnant / postpartum women received oseltamivir (4 cases did not receive oseltamivir, and 4 had no treatment data). Oseltamivir use among pregnant /postpartum women was significantly higher compared to women who were not pregnant (OR = 10 [95 % CI 3–32]) but there was no difference between days from hospitalization and oseltamivir treatment (p = 0.9).
Fifty five percent (100/183 cases) were also tested through immunofluorescence for other respiratory virus. Two cases also were positive for respiratory syncytial virus, 1 for influenza B, 1 for adenovirus, 1 for parainfluenza virus. Twenty-three percent (43 cases) were tested for bacteremia through blood cultures; 1 was positive for Streptococcus pneumoniae.
Discussion
Decedents infected with influenza A(H1N1)pdm09 were frequently young, pregnant, or had other pre-existing medical conditions. Unlike seasonal influenza deaths, which predominately occur among older adults [24, 25], the median age of those who died with influenza A(H1N1)pdm09 infections was 32 years. More than half had a pre-existing medical condition. In addition, 15 % of all decedents with influenza A(H1N1)pdm09 in Central America were reported as maternal deaths, more than twice the 2009 prevalence of pregnancy among study countries (6.5 %) [26]. The proportion of influenza A(H1N1)pdm09 maternal deaths was more than twice the global estimates (5–7 %) [27–30]. It could be effect of relevance of maternal mortality for these countries.
Such findings suggest that the influenza pandemic disproportionately affected pregnant women and mothers during their puerperium and consider targeting this group during future epidemic/pandemic periods with risk communications, early antiviral treatment, and vaccination [31].
Costa Rica had the higher proportion of deaths (40 %); this could be explained by diagnosis skills and access to health services in this country.
Although most influenza A(H1N1)pdm09 case-patients were treated with oseltamivir (65 %), less than 6 % received oseltamivir within 48 h of symptom onset when the antiviral are thought to be most effective [32–34]. We found no evidence that non-pregnant persons at high risk for complications [5–7, 9, 14, 19, 35] were more likely to receive timely oseltamivir than other cases. Indeed, there was a wide variability among the proportion of case-patients who were treated with oseltamivir depending on their country of residence. Such findings raise questions about the accessibility to timely oseltamivir stockpiles, physicians experience using oseltamivir during routine clinical care, and direct medical costs associated with oseltamivir in the American tropics. Our findings underscore importance of exploring the timely use of oseltamivir in middle and low income countries.
This study has important limitations. We assumed that all SARI decedents identified by health authorities comprised the majority of laboratory-confirmed influenza A(H1N1)pdm09 deaths. It is likely that a proportion of persons with severe influenza A(H1N1)pdm09 illness may have remained unidentified or untested and that these persons could have had different demographic and clinical characteristics than those identified through surveillance. For example, it is possible that cases with pre-existing medical conditions may have been preferentially tested for influenza A(H1N1)pdm09 thus increasing the proportion of high risk laboratory-confirmed case-patients identified in our case-series. Also we have no access to socioeconomic status of cases.
Conclusions
Our study demonstrates the utility of influenza surveillance which provided valuable data to the epidemiology of influenza A(H1N1)pdm09 during 2009–2010. Our findings suggest that decedents associated with influenza A(H1N1)pdm09 were frequently young persons with prevalent pre-existing medical conditions. Our data suggest that few cases received oseltamivir within 48 h of treatment, highlighting challenges with the use of antivirals during periods of epidemic activity in the region. Based on these data, current national treatment protocols urge clinicians prioritize individuals with preexisting medical conditions such as pregnancy, asthma, and diabetes for timely oseltamivir treatment. Future studies should explore the availability and accessibility of oseltamivir as well as the potential value for presumptive treatment of high-risk individuals during periods of epidemic influenza activity in tropical middle and low income countries.
Abbreviations
- AIDS:
-
Acquired immune deficiency syndrome
- CDC:
-
Centers for Disease Control and Prevention
- CXR:
-
Chest X Rays
- EW:
-
Epidemiological week
- H1N1pdm09:
-
Corresponding to pandemic strain of influenza for 2009
- IQR:
-
Interquartile range
- OR:
-
Odds ratio
- PAHO:
-
Pan American Health Organization
- SARI:
-
Severe acute respiratory infection
- WHO:
-
World Health Organization
References
Center for Disease Control and Prevention. People at High Risk of Developing Flu–Related Complications [Internet]. Seasonal Influenza (Flu). 2012. Available from: http://www.cdc.gov/flu/about/disease/high_risk.htm.
Jamieson DJ, Theiler RN, Rasmussen S. a. Emerging infections and pregnancy. Emerg Infect Dis [Internet]. 2006;12(11):1638–43. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3372330&tool=pmcentrez&rendertype=abstract.
Goodnight WH, Soper DE. Pneumonia in pregnancy. Crit Care Med [Internet]. 2005 [cited 2012 Nov 13]:33(Supplement):S390–7. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00003246-200510001-00021.
Laibl VR, Sheffield JS. Influenza and pneumonia in pregnancy. Clin Perinatol [Internet]. 2005 [cited 2013 Jan 31];32(3):727–38. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16085029.
Center for Disease Control and Prevention. Updated Interim Recommendations for the Use of Antiviral Medications in the Treatment and Prevention of Influenza for the 2009–2010 Season. H1N1 Flu CDC [Internet]. 2010; Available from: http://www.cdc.gov/H1N1flu/recommendations.htm.
Pan-American Healt Organization. Considerations and interim recommendations for the clinical management of pandemic (H1N1) 2009. Expert Consultation PAHO /WHO.2009. http://www2.paho.org/hq/dmdocuments/2009/informe_consulta%20expertos_clinica_ENG.pdf.
Ministry of Health Costa Rica. Guidelines for the prevention, care and control of people with influenza. Natl Guidel. 2010.
Ministerio de Salud Pública y Asistencia Social El Salvador. Lineamientos actualizados para el manejo del virus pandémico (H1N1) 2009 en humanos. [Internet]. Available from: http://www.salud.gob.sv/index.php/servicios/descargas/documentos/Documentaci?n-Institucional/Lineamientos-y-Filtros/Lineamientos-actualizados-para-el-manejo-del-virus-pand?mico-(H1N1)-2009-en-humanos/.
Ministry of Healt Guatemala. Update Protocol for outpatient care, prevention guidelines and epidemiological influenza A H1N1. 2009.
Minister of Helath of Nicaragua. National Plan for prevention and response of human influenza outbrake [Internet]. 2010. Available from: http://www.minsa.gob.ni/index.php?option=com_remository&Itemid=52&func=fileinfo&id=6668.
Ministry of Health of Panama. Guidelines for care of patiens with influenza A (H1N1) [Internet]. 2009. Available from: http://www.minsa.gob.pa/minsa/tl_files/documents/influenza/personal_salud/protocolos/MANEJO DE PACIENTES.pdf.
San Pedro Daily. No need for cuntrywide panic over the H1N1 cases. San Pedro Dly Newsp. 2009;20:1–7.
Morrobel J. Agentes policiacos pegan afiches que contienen medidas de prevención de gripe A/H1N1. Nuevo D [Internet]. 2009;Santo Domi(June 2009). Available from: http://elnuevodiario.com.do/app/article.aspx?id=156564.
Ministry of Healt of Costa Rica. National Guidelines for surveillance, prevention, patient care and control of pandemic influenza H1N1 [Internet]. 2010. Available from: http://www.google.com.gt/url?sa=t&rct=j&q=lineamientos normas influenza pandemica costa rica&source = web&cd = 2&cad = rja&ved = 0CDEQFjAB&url=http://www.ministeriodesalud.go.cr/index.php/inicio-alerta-alerta-sanitaria-ms/doc_download/369-lineamientos-nacionales-para-la-pandemia-de-influenza-ah1n1&ei=E4E-UdqfOs-p0AGAvoAI&usg=AFQjCNFG_D67btXhWEPZTdS_Ik-_1YTGlQ&bvm=bv.43287494,d.cWE.
Health Secretary Honduras. Influenza H1N1 Recomendations [Internet]. Influenza H1N1. 2010. Available from: http://www.salud.gob.hn/recomendacionesh1n1.html.
Minister of Health of Nicaragua. Poster Influenza Humana [Internet]. 2009. Available from: http://www.minsa.gob.ni/index.php?option=com_remository&Itemid=52&func=fileinfo&id=6650.
Ministry of Health of Panama. National Risk Comunication Guidelines. 2009.
McGeer A, Green K, Plevneshi A. Antiviral therapy and outcomes of influenza requiring hospitalization in Ontario, Canada. Clin Infect Dis. 2007;45:1568–75.
Ministry of Healt El Salvador. Updated guidelines for the management of pandemic (H1N1) 2009 in humans [Internet]. Institutional Documentation. 2010. Available from: http://www.salud.gob.sv/servicios/descargas/documentos/func-download/440/chk,f719c3f3370f3916d5436512a3bc9fb4/no_html,1/.
Centers for Disease Control and Prevention. Pregnant Women and Influenza [Internet]. Seasonal Influenza (Flu). 2014. Available from: http://www.cdc.gov/flu/protect/vaccine/pregnant.htm.
World Health Organization. Report of the WHO Pandemic Influenza A(H1N1) Vaccine Deployment Initiative. WHO Libr Cat Data. 2012; http://www.who.int/influenza_vaccines_plan/resources/h1n1_deployment_report.pdf.
Central Intelligence Agency. The World Factbook [Internet]. 2011. Available from: https://www.cia.gov/library/publications/the-world-factbook/fields/2212.html#cs.
Pan-American Health Organization-CDC. Generic Protocol for Influenza Surveillance. PAHO Heal Surveill Dis Atention Area. 2006; http://new.paho.org/hq/images/stories/AD/HSD/CD/INFLUENZA/flu-snl-gpis.pdf.
Pebody RG, McLean E, Zhao H, Cleary P, Bracebridge S, Foster K, et al. Pandemic Influenza A (H1N1) 2009 and mortality in the United Kingdom: risk factors for death, April 2009 to March 2010. Euro Surveill [Internet]. 2010;15(20):1–11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20504388.
Shiley K, Nadolski G. Differences in the Epidemiological Characteristics and Clinical Outcomes of Pandemic (H1N1) 2009 Influenza, Compared with Seasonal Influenza. Infect Control Hosp Epidemiol. 2010;31(7):676–82.
Ministry of Healt El Salvador. El Salvador Variables and Indicators 2007. Planif Heal Serv Dir. 2007;3–6.
Mosby LG, Rasmussen S a, Jamieson DJ. 2009 pandemic influenza A (H1N1) in pregnancy: a systematic review of the literature. Am J Obstet Gynecol [Internet]. Elsevier Inc.; 2011 [cited 2012 Oct 31];205(1):10–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21345415.
Siston AM, Rasmussen S a, Honein M a, Fry AM, Seib K, Callaghan WM, et al. Pandemic 2009 influenza A(H1N1) virus illness among pregnant women in the United States. JAMA [Internet]. 2010;303(15):1517–25. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20407061.
Balanzat AM, Hertlein C, Apezteguia C, Bonvehi P, Cámera L, Gentile A, et al. An analysis of 332 fatalities infected with pandemic 2009 influenza A (H1N1) in Argentina. PLoS One [Internet]. 2012 [cited 2013 May 16];7(4):e33670. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3323608&tool=pmcentrez&rendertype=abstract.
Velásquez J, Vélez G, Zuleta J, Franco F, Gómez J. H1N1 influenza pandemic and maternal mortality in Antioquia, Colombia. Int J Gynaecol Obstet [Internet]. 2011 [cited 2013 May 16];115(2):144–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21872236.
World Health Organization. WHO recommends seasonal influenza vaccination to pregnant women as the highest priority [Internet]. Immunization, Vaccines and Biologicals. 2012. Available from: http://www.who.int/immunization/newsroom/newsstory_seasonal_influenza_vaccination_pregnancy/en/.
McGeer A, Green K a, Plevneshi A, Shigayeva A, Siddiqi N, Raboud J, et al. Antiviral therapy and outcomes of influenza requiring hospitalization in Ontario, Canada. Clin Infect Dis [Internet]. 2007 [cited 2012 Nov 2];45(12):1568–75. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18190317.
Farias J a, Fernández A, Monteverde E, Vidal N, Arias P, Montes MJ, et al. Critically ill infants and children with influenza A (H1N1) in pediatric intensive care units in Argentina. Intensive Care Med [Internet]. 2010 [cited 2013 Jan 25];36(6):1015–22. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20237757.
Lee N, Chan PKS, Hui DSC, Rainer TH, Wong E, Choi K-W, et al. Viral loads and duration of viral shedding in adult patients hospitalized with influenza. J Infect Dis [Internet]. 2009 [cited 2012 Nov 2];200(4):492–500. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19591575.
Rasmussen S a, Jamieson DJ, Macfarlane K, Cragan JD, Williams J, Henderson Z. Pandemic influenza and pregnant women: summary of a meeting of experts. Am J Public Health [Internet]. 2009 [cited 2012 Dec 4];99 Suppl 2:S248–54. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19461110.
Acknowledgement
Dr. Nivaldo Linares Former Coordinator of CDC-CAR Influenza Program. Staff of the laboratory influenza of Ministry of Health of Central America and Dominican Republic: Celina Calderon (El Salvador), Leticia Castillo (Guatemala), Jenny Lara (Costa Rica), Alex Martinez (Panama) and Mildred Disla (Dominican Republic); the Informatics team of the Influenza Program including Marcelo Adaglio and Daniel Otzoy; and the CDC Influenza Division including Nancy Cox, Joseph Bresee, Ann Moen and Marc-Alain Widdowson.
Disclaimer
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the Centers for Disease Control and Prevention or the institutions with which the authors are affiliated.
Financial disclosure
This study was supported by the Cooperative Agreement No. 1U01GH000028-03 from the U.S. Centers for Disease Control and Prevention. None of the coauthors have any conflicts of interest to declare. The findings and conclusions in this report are those of the authors and do not necessarily reflect the official position of the Centers for Disease Control and Prevention or the institutions with which the authors are affiliated.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
RC has designed the research, has participate in acquisition of data; He has been performed the analysis and interpretation of data; and have been involved in drafting the manuscript. SM participated in the analysis of data, and helped to draft the manuscript. DR participated in the data acquisition from El Salvador, and helped to draft the manuscript. AP participated in the data acquisition from Guatemala, and helped to draft the manuscript. GG participated in the data acquisition from Costa Rica, participated in recovery of background and design and to draft the manuscript. LM participated in the data acquisition from Panama. CT participated in the data acquisition from Dominican Republic. JJ helped to draft the manuscript. NB helped to draft the manuscript. LB participated in the design and helped to draft the manuscript. WC has advised all steps of the study, included design, interpretation of data and drafting the manuscript. PM participated in the design of the study. RP helped to draft the manuscript. EA has advised on data interpretation, design of the manuscript and helped to draft the manuscript. All authors have read and approved the final manuscript.
Additional file
Additional file 1:
STROBE Statement—Checklist of items that should be included in reports ofcross-sectional studies. (DOC 87 kb)
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Chacon, R., Mirza, S., Rodriguez, D. et al. Demographic and clinical characteristics of deaths associated with influenza A(H1N1) pdm09 in Central America and Dominican Republic 2009–2010. BMC Public Health 15, 734 (2015). https://doi.org/10.1186/s12889-015-2064-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-015-2064-z