Abstract
Background
Inadequate immunization coverage with increased risk of vaccine preventable diseases outbreaks remains a problem in Africa. Moreover, different factors contribute to incomplete vaccination status. This study was performed in Dschang (West Region, Cameroon), during the polio outbreak occurred in October 2013, in order to estimate the immunization coverage among children aged 12–23 months, to identify determinants for incomplete vaccination status and to assess the risk of poliovirus spread in the study population.
Methods
A cross-sectional household survey was conducted in November-December 2013, using the WHO two-stage sampling design. An interviewer-administered questionnaire was used to obtain information from consenting parents of children aged 12–23 months. Vaccination coverage was assessed by vaccination card and parents’ recall. Chi-square test and multilevel logistic regression model were used to identify the determinants of incomplete immunization status. Statistical significance was set at p < 0.05.
Results
Overall, 3248 households were visited and 502 children were enrolled. Complete immunization coverage was 85.9 % and 84.5 %, according to card plus parents’ recall and card only, respectively. All children had received at least one routine vaccination, the OPV-3 (Oral Polio Vaccine) coverage was >90 %, and 73.4 % children completed the recommended vaccinations before 1-year of age. In the final multilevel logistic regression model, factors significantly associated with incomplete immunization status were: retention of immunization card (AOR: 7.89; 95 % CI: 1.08–57.37), lower mothers’ utilization of antenatal care (ANC) services (AOR:1.25; 95 % CI: 1.07–63.75), being the ≥3rd born child in the family (AOR: 425.4; 95 % CI: 9.6–18,808), younger mothers’ age (AOR: 49.55; 95 % CI: 1.59–1544), parents’ negative attitude towards immunization (AOR: 20.2; 95 % CI: 1.46–278.9), and poorer parents’ exposure to information on vaccination (AOR: 28.07; 95 % CI: 2.26–348.1). Longer distance from the vaccination centers was marginally significant (p = 0.05).
Conclusion
Vaccination coverage was high; however, 1 out of 7 children was partially vaccinated, and 1 out of 4 did not complete timely the recommended vaccinations. In order to improve the immunization coverage, it is necessary to strengthen ANC services, and to improve parents’ information and attitude towards immunization, targeting younger parents and families living far away from vaccination centers, using appropriate communication strategies. Finally, the estimated OPV-3 coverage is reassuring in relation to the ongoing polio outbreak.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Despite the improvement in global immunization coverage, about 16 % of the worlds’ children had not completed the 3-dose diphtheria-tetanus-pertussis vaccine (DTP-3) series by 2013 [1]. The estimated 2013 global DTP-3 coverage among children aged <12 months, which is a key indicator of immunization program performance, was 75 % in the World Health Organization (WHO) African Region, and 84 % worldwide [1]. However, thanks also to the Expanded Program on Immunization (EPI), children immunization coverage in the WHO African Region is improving, even if still sub-optimal in many areas [2].
The EPI was introduced in Cameroon in 1976 [3]. According to the 2011 Cameroonian Demographic Health Survey (DHS) [4], the coverage of the nine EPI vaccines in children aged 12–23 months was 57 % at the national level, and 59.3 % in the West Region. In this region, wild poliovirus (WPV) type 1 was isolated from two acute flaccid paralysis (AFP) cases in October 2013 [5]. In 2013, other four cases due to circulating vaccine-derived poliovirus type 2 (cVPDPV-2) were reported also in the Far North Region of Cameroon. According to the Global Polio Eradication Initiative (GPEI), a total of nine cases of WPV-1 have been reported in Cameroon during the years 2013–2014 [6], representing the first polio-outbreak reported in the country since 2009.
Vaccine preventable diseases outbreaks are linked to inadequate levels of immunization coverage [5]. Several factors are associated with poor vaccination coverage in resources-limited countries. A multilevel analysis involving 24 African countries [7] showed that breaks in childhood vaccination are linked, at the contextual level, to high community illiteracy rates, high country fertility rates, and living in urban areas, while, at the individual level, they are linked to poorest households, uneducated parents, parents with no access to media and/or with low health seeking behaviours; the relative effect of the above factors may significantly vary according to the geographical area [7].
In Africa, a more detailed and comprehensive information at district level is necessary in order to develop and implement appropriate strategies for improving immunization coverage. In Cameroon, there are no studies, conducted at the district level, assessing factors associated with incomplete immunization. To fill this gap, we planned a community-based cross-sectional survey in the district of Dschang (West Region, Cameroon), a rural setting sited only 30 km far from the area affected by the polio outbreak [8]. The objectives of this study were to estimate the districts’ coverage of routine vaccination program, to identify risk factors for incomplete vaccination status among children 12–23 months old, and to assess the risk of WPV spread in the study population.
Methods
Study area
Dschang was selected as the study site because it is close to the outbreak area, and because of an established collaboration between the research team and local health authorities. The district of Dschang is located in the Menoua Department, West Region, Cameroon. According to local health authority, the 2012 districts’ estimated population was of 218,006 inhabitants (17 % under-five years old children), mostly belonging to the Bamiléké ethnic group and Christian religion. The local economy is based on agriculture and livestock. The district has 4 hospitals, 3 public medical centres, and 46 health centres that deliver EPI vaccines to the target population groups. The 2012 Dschang districts’ annual health report indicated a coverage of 90 % for all vaccines. During 2013, considering the increased risk of polio spread, Dschang district was involved in two national immunization days (NIDs) (October and December). Our study focused only on vaccinations received through the routine immunization program because, according to GPEI strategy [9], OPV doses provided during supplementary immunization activities (SIAs) are not registered on the vaccination card, but children are just marked on the finger.
Study design and sampling
We conducted a cross-sectional household survey of children aged 12–23 months, between the 10th of November and the 10th of December 2013. Considering the unavailability of an exhaustive list of households and of children aged 12–23 months, a two-stage sampling design, using firstly the village/neighbourhood (clusters) and then the EPI random walk method, was performed [10]. At the first stage, the clusters were sampled with probability proportional to their size, according to the estimated population data per village provided by the health’ district authority. Assuming an expected vaccination coverage of 50 % (i.e., the percentage with the highest variability), an intracluster correlation coefficient of 0.04 (usually between 0.01 and 0.02 in human study surveys [11–15]), and a precision of ±5 %, a sample of 60 clusters of 9 children each, for a total sample size of 540 children aged 12–23 months, was initially planned. At the second stage, according to the EPI-style random walk [10], the sampling started from the geographic centre of the cluster. The direction of data collection was randomly chosen, using the spinning bottle method, and every house in that direction was selected for the survey, following the principle of the next nearest household. Children were recruited consecutively until the planned cluster sample size was achieved.
Data collection
The Cameroonian immunization schedule at the time of the study is summarized in Table 1. After the identification of a child aged 12-to-23 months from the household selected through house-to-house visits, the presence of child’ immunization card was assessed. In case of two or more 12–23 months old children were found in the same house, the youngest child was selected [10]. A structured interviewer-administered questionnaire was used to obtain information from consenting parents. All interviewers were trained on the questionnaire use and EPI-style random walk. The acceptability and the logical structure of the questionnaire were checked on the field, during pre-testing. The questionnaire was constructed from a review of the available literature on immunization surveys in developing countries [10, 16–24], with the aim to investigate variables related to: parental, household and child characteristics; antenatal/postnatal care; parental perception, knowledge and attitude on immunization; parental exposure to information on immunization; child vaccination history; reasons for non-vaccination. Data on child vaccination (doses, timing and type of vaccines received) were collected from vaccination cards and, if unavailable, by parents’ interview only, as suggested by WHO [10]. Information on other variables was collected by parents’ interview only.
Data analysis
After reviewing for completeness and accuracy, all data from eligible children were included in a database. Double data entry was performed and validated. The parents’ vaccination knowledge, their attitudes towards immunizations and their opinion on Dschang immunization services were assessed through a 5-points scale (1 point per each correct response) closed-ended questions (5 for each area) and classified respectively as good or poor knowledge, negative or positive attitudes, and bad or good opinion. A minimum of 3-points score was established as cut-off. Parents’ exposure to information about immunization was assessed through 4 weighed open questions and classified as present or absent. The socio-economic household status was classified in tertiles, through an algorithm that considered the type of family (two or single-parent), and the parents’ occupation. These scoring systems were constructed from a review of the available literature on immunization surveys in developing countries [16–24]. Children vaccination status definitions are summarized in Table 2. The risk of WPV spread was assessed measuring OPV3 coverage in accordance with GPEI [25]. The dropout rate was defined as the percentage of children who received the 1st but not the 3rd dose of vaccines, or who received the first (BCG, Bacille Calmette Guérin) but not the latest (measles or yellow fever) vaccine included in the vaccine schedule. The dropout rates (by card and by card plus parents’ recall) were evaluated according to WHO calculation method: [(first dose – last dose)/first dose] ×100 [26].
Relative frequencies and other descriptive statistics were calculated to evaluate the immunization coverage and the association of the vaccination uptake (by card plus parents’ recall) with the independent variables. Statistical inference [i.e., 95 % confidence intervals (95 % CI) and p-values] was performed taking into account the two-stage sampling design [13]. Finally, to calculate adjusted odds ratios (AOR) of factors independently associated with incomplete immunization coverage (by card plus parents’ recall), a multiple multilevel logistic regression model was performed. Regarding the selection of this multiple model, initially we planned, following the indication by Hosmer and Lemeshow [27] to select the variables to be included in the final model based on the results of the univariate analysis (i.e., including only those with a log-likelihood ratio test <0.20) and then to further exclude among those initially included in the multiple model that, at each step, had the highest log-likelihood ratio test p-value ≥0.20 until only variables with a p-value <0.20 were remaining. However, this approach actually was not possible because the multiple model based on the characteristics selected at the univariate analysis (i.e., those with p < 0.20) did not converge. We then decided to select the characteristics to be included on the basis of “intermediate” multiple logistic models performed for each section of the survey questionnaire (i.e., children, parents, household characteristics and parents’ perceptions, knowledge and attitudes). The variables were further selected by a subsequent backward selection that at each step excluded that variable with the highest p-value >0.20 (from log-likelihood ratio test) until only variables with a p-value <0.20 remained. All analyses were performed using STATA software (version 12.0).
Ethics approval
Ethical approval was obtained from the “Comité National d’éthique de la Recherche pour la Santé Humain du Cameroun” and Dschang Health Authority. Data collection was conducted confidentially and after obtaining verbal parents’ informed consent. Partially vaccinated children were notified to Dschang Health Authority in order to complete the recommended vaccinations.
Results
A total of 3248 households were visited, and 5 additional clusters were sampled in order to achieve the expected sample size. A total of 502 parents of children aged 12-to-23 months recruited in 65 clusters were interviewed with a response rate of 100 %. The average number of children recruited per cluster was 7.72 (range 2–9), and the average number of households visited per cluster before finding up to 9 eligible children was 49.96 (range 13–99).
Study population characteristics
The children’ mean age was 19.6 months; of them, 50.6 % were male, and the vast majority (97.6 %) were born at health facilities. The most represented parents’ age group was 25–29 years for mothers (40.7 %) and ≥30 years for fathers (70.7 %). With regard to the households, 87.2 % were two parents-family, 51.4 % of Catholic religion; 41.2 % had more than three children <5-years old, and 23.7 % were distant >8 km from the nearest vaccination centre. Only 26.6 % of the parents had secondary education. The principal fathers’ work activity was farmer (27.1 %), while many of the mothers were not working/unemployed (35.8 %); 53.6 % of households belonged to the economic poorest tertile. The majority of the mothers (64.5 %) reported ≥3 ANCs during the last pregnancy, but only 29.1 % reported at least one postnatal visit. Respectively 85.4 % and 50.2 % of the parents showed positive attitude and good knowledge about vaccination, 78.5 % declared to receive regularly information on vaccination, and 80.5 % reported a good opinion on vaccination services of the Dschang health district.
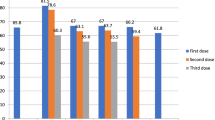
Immunization coverage by card only
Vaccination card was available for 252 (50.2 %) children. As shown in Table 3, 84.5 % (95 % CI 79.5–89.5) of the children were fully immunized, but only 73.4 % (95 % CI 67.6–78.4) within one year of life, while 15.5 % (95 % CI 11.5–20) were partially immunized. The most frequently administered vaccines were BCG (98.8 %) and DTwPHibHepB-1 (Diphtheria and tetanus toxoid with whole cell pertussis, Haemophilus Influenzae type B and Hepatitis B vaccines) (98 %), while measles and yellow fever were the least taken vaccines (90 %). OPV-3 was received by 91.6 % of children. DTwPHibHepB-1/3 and OPV-1/3 dropout rates were respectively 5.3 and 4.2 %, while the dropout rate from BCG to measles and yellow fever vaccination was 8.9 %.
Immunization coverage by card plus parents’ recall
As shown in Table 3, based on data from vaccination card plus parents’ recall, 85.9 % (95 % CI 82.4-89.3) of the children were fully immunized, and 14.1 % (95 % CI 10.7-17.6) were partially immunized; unvaccinated children were not found. Among partially immunized children, the main reported mothers’ reason for not being able to vaccinate their children was “to be very busy” (32.3 %, n = 22). Among the nine vaccines, BCG and DTwPHibHepB-1 were the most frequently administered (99.8 % and 98.8 % respectively), while measles and yellow fever were the least taken vaccines (91.2 %). OPV-3 was received by 95 % of children. DTwPHibHepB-1/3 and OPV-1/3 dropout rates were respectively 4 % and 3.4 %, while the dropout rate from BCG to measles and yellow fever vaccination was 8.6 %.
Factors associated with incomplete immunization coverage: univariate analysis
Table 4 shows the univariate association between the study variables and the children immunization status, assessed by card plus parents’ recall. Children born at health facilities had a higher immunization coverage rate compared with those born at home (p < 0.01), as well as children who were the 1st-2nd born in the family compared with those being the 3rd or later born (p < 0.01). Children from low-educated and younger parents were less immunized (p < 0.01), as well as children from poorest household (p = 0.01) and from single-parent family (p < 0.01). The distance of the household from the vaccination centre was found associated with the immunization status (p < 0.01). Moreover, children of mothers who had ≥3 ANCs and at least one postnatal visit had better immunization coverage (p < 0.01 and p = 0.03 respectively). Finally, children of parents who had good knowledge and positive attitude towards immunization, who received regularly information on vaccinations and who had a good opinion of Dschang immunization services, were more likely to be fully vaccinated (p < 0.01).
Factors associated with incomplete immunization coverage: multilevel logistic regression analysis
Table 5 shows the estimated AORs obtained by the multilevel logistic regression analysis. In the final model, the characteristics significantly associated with incomplete children immunization status were: having the vaccination card (AOR 7.89; 95 % CI 1.08–57.3; p = 0.04), being the 3rd or later born child in the family (AOR 425.4; 95 % CI 9.62–18,808; p < 0.01), having a mother ≤24 years-old (AOR 49.55; 95 % CI 1.59–1544; p = 0.03), having a mother who attended ≤2 ANCs (AOR 8.25; 95 % CI 1.07–63.7; p = 0.04), having parents with negative attitudes towards vaccination (AOR 20.20; 95 % CI 1.46–278.9; p = 0.03) and who do not regularly receive information about immunization (AOR 28.07; 95 % CI 2.26–348; p < 0.01). Finally, the association with longer distance (≥8 Km) from the vaccination centers was marginally significant (AOR 6.44; 95 % CI 1.00–41.4; p = 0.05).
Discussion
We assessed the routine vaccination coverage and risk factors for incomplete vaccination among children aged 12–23 months in the Dschang district, West Region, Cameroon. The survey was performed during a polio outbreak occurred in the same region of the country [5, 8]. Thus, OPV-3 coverage data reported from our study may represent an indicator for the risk assessment of WPV spread in the study area. Vaccination coverage was assessed by card only and by card plus parents’ recall. Immunization cards were available for 50.2 % of the children. As shown in Table 6, the vaccination coverage observed in this survey was higher than that reported for the whole Cameroon by WHO [28], and by the 2011 Cameroonian DHS for the whole country and the West Region [4].
According to card plus parents’ recall, 85.9 % of the children of our survey were fully vaccinated. Vaccination coverage reported by immunization surveys in rural African areas ranged from rates as low as 26 % in Burkina Faso [18] to 88 % in Ghana [29]. Moreover, in our survey, there was no unvaccinated child, confirming the low rate (2.3 %) reported by the 2011 Cameroonian DHS for the West Region [4]. For comparison, unvaccinated children ranged from 6.5 % [24] to 24 % [20] in surveys conducted in Ethiopia. According to immunization card plus parents’ recall, we observed 14.1 % of partially vaccinated children (15.5 % by card only), a lower proportion than that reported by surveys conducted in Mozambique (28.2 %) [22] and Ethiopia (20.3 %) [24]. Although our findings are indicative of a rather high adherence to vaccination schedule in term of completeness, 26.6 % of children did not complete the recommended doses within one year of life; no comparable data were found in the scientific literature. DTwPHibHepB-3 coverage in our survey was 94.8 % by card plus parents’ recall (92.8 % by card only), which is higher than what reported by other surveys performed in rural Ethiopia (47.9 %) [20], Nigeria (80.8 %) [16], and Kenya (90 %) [19]. OPV-3 immunization coverage was >90 %, based on both card plus parents’ recall and card only, indicating that 12–23 months old children living in the Dschang district had a good protection level against the risk of WPV spread related to the ongoing polio outbreak in the West Region of Cameroon [5, 8]. Other surveys performed in Africa reported OPV-3 coverage of 91.8 % in Kenya [19], 80.8 % in Nigeria [16], 86.3 % and 54.3 % in Southern [24] and Central Ethiopia [20], respectively.
Limited differences were found in vaccination coverage when assessed by card plus parents’ recall or by card only. An expected tendency of highest vaccination coverage values when assessed by card plus parents’ recall was observed, in accordance with WHO and the international literature [10, 20]. The biggest difference was related to OPV-0 (+4 %), though it was lower than that reported in a study from Ethiopia [20], where differences ranged from 12 % to 34 %. In our study, as also reported by the 2011 Cameroonian DHS [4] and by another survey from Kenya [30], OPV-0 coverage (by card plus parents’ recall and by card only) was lower than BCG and OPV-1 coverage. The reason of this finding is undefined; OPV-0 could be underreported in the card by health care staff and/or less recalled by parents when compared to BCG vaccine, that is intradermally administered at birth, and to OPV-1 that is administered with DTwPHibHep-1 at 6th weeks of life. No difference was observed between measles and yellow fever vaccination coverage when assessed by card plus parents’ recall or by card only (Table 3), consistently with data reported by the 2011 Cameroonian DHS [4] and by a study from Sierra Leone [31]. This finding suggests that these two vaccines are correctly administered during the same vaccination session. The vaccination dropout rates observed are acceptable, according to the WHO standard (cut-off < 10 %) [26], and lower than those reported by studies from Ethiopia [23, 24].
Several characteristics were associated with immunization status in our study, but only six of them were statistically significant at the final multilevel regression model (Table 5). Birth order was statistically associated with fully immunization, similarly to what reported by studies from Kenya [19] and India [32], but in contrast with a survey from Ethiopia [20]. This finding could be related to a reduced mothers’ attention along with growing number of children, due to an increase of duties, as confirmed by mothers’ interview (the main reported reason for not being able to vaccinate their child was “to be very busy”). Being born at the hospital/health facility was linked to complete vaccination status in studies from different African countries [19, 20, 22], while in our survey it was associated in a restricted multilevel model including only the children characteristics, but the association was no longer statistically significant when adjusting for all other factors. Perhaps, the effect of place of birth was explained in the model by prenatal visits and/or access to health services, of whom it may be considered a proxy. A lower number of mothers’ ANCs and the younger mothers’ age were associated with incomplete vaccination status, as in other studies from African countries [7, 16, 20, 29, 33]. It is possible that reduced contacts with health facilities during pregnancy, especially among younger mothers, could cause poorer information toward immunization. A longer distance (≥8 Km) from vaccination sites was marginally significant (p = 0.05) in the final model. The accessibility to vaccination sites was associated to immunization status in studies from rural Mozambique [21] and Nigeria [16], while no distance related difference was found in a study from Burkina Faso [18]. Mothers’ education was associated in the first multilevel model, including only parents’ characteristics, but no more when all factors were included in the model; this covariate was found associated with complete vaccination in several studies from African countries [7, 16, 18, 29].
A high vaccination knowledge score, positive attitudes toward vaccination, good perception of immunization services, and the exposure to information on vaccinations, were all associated with complete vaccination status. As in other studies from Nigeria [16], Niger [33], and India [32], despite a parents’ poor vaccination knowledge score in 50 % of the cases, the majority of interviewed parents (84.5 %) had a positive attitude toward immunization. Overall, only parents’ positive attitude and regular information received remained significantly associated with complete vaccination in the final multilevel model. These two factors were reported as determinants of complete immunization status in a multilevel analysis involving 24 sub-Saharan African countries [7]. Concerning these aspects, it is noteworthy that the father of the index case of the polio outbreak recorded in the West Region in Cameroon (October 2013) was a political leader and pastor that, despite its good education level and high economic status, was strongly opposed to vaccination [8], and his children had never been vaccinated.
Other demographic factors linked to vaccination status identified in studies conducted in several African countries were found either not statistically associated or associated only at the univariate analysis, or were just not considered in our study. Among these factors, parents’ socio-economic status and number of children in the family were not significant in the final multilevel model, while they were significantly associated in other African studies [18, 28], including one from Cameroon [34]; birth season and residence area, significantly associated in a study from Burkina Faso [18], were not considered in our survey. Surprisingly, in contrast with the results of surveys conducted in African countries [16, 18, 22] and India [32], possessing the vaccination card was associated with incomplete vaccination. This, as suggested by WHO [10], might be due to parents over-reporting of vaccine doses for complacency, without the possibility to check the information. This aspect is controversial and may represent a limit of our study. In fact, a recent systematic review on the validity of vaccination card and parents’ recall to estimate vaccination coverage [35] suggests that parents’ recall information should be cautiously interpreted because it might be not reliable. This issue is not mentioned in WHO EPI-coverage survey guidelines [10] and has not been addressed in the fields’ immunization surveys [16–24]; thus, methodological studies on this aspect are needed.
Another limit is that our survey was conducted in a district of a region affected by a polio-outbreak situation, and two SIAs have been realized before and during our study. This situation could introduce biases in the OPV coverage evaluation for different reasons: firstly, vaccine doses may have been administered from other than Dschang vaccination facilities; secondly, parents could incorrectly report vaccine doses as administered during SIAs or routine immunization and vice-versa. Thus, the contribution of routine immunization activities and SIAs to the OPV coverage rate could not be completely distinguished. However, coverage rates for OPV-3 were similar to DTwPHibHepB-3, as well as all observed coverage for the different vaccines administered during the same routine immunization session. Furthermore, even if the parents’ tendency to over-report doses of vaccines [10, 20] may introduce biases, vaccines coverage rates assessed by card plus parents’ recall and by card only were similar in our study.
A further study limitation concerns the procedure used to determine households’ economic status. In fact, our specific algorithm was based only on the type of family (two or single-parent) and parents’ occupation, while housing conditions and economic activities of other household members were not considered. The sampling procedure was also susceptible of selection bias and the study did not include qualitative methods to address this questions. Moreover, qualitative methods, such as in-depth interviews, were not used to investigate the reasons for partial or delayed vaccination. Planning qualitative studies may be a useful complement to quantitative surveys in better understanding obstacles and possible solutions to increase vaccination coverage.
To our knowledge, despite the above mentioned limitations, this is one of the few studies using a multilevel logistic regression analysis to identify risk factors for incomplete immunization status and the intracluster correlation coefficient for the sampling size calculation. Our study contributes to the identification of factors related to the children immunization status at a district level in Cameroon, where similar studies are lacking. Moreover, we reported the vaccination coverage in children <12 months of age, that is not mentioned in surveys performed in similar African contexts, and we provided an important risk indicator of WPV spread during the ongoing outbreak situation.
Conclusion
In conclusion, our study revealed high vaccination coverage in the Dschang district (West Region, Cameroon), and a good protection level against the risk of WPV spread. However, although none of the children was completely unvaccinated, almost 1 out of 7 children was partially vaccinated, and almost 1 out of 4 children did not complete the recommended vaccinations within 12 months of life. Younger parents and families living far away from vaccination centres should be targeted with appropriate immunization promotion strategies, and the improvement of prenatal care and delivery services should be addressed in order to increase immunization coverage and proper (timely) vaccines administration. Information and attitude towards immunization should be strengthened with adequate vaccination education programmes, in order to favour this evidence-based intervention [36, 37].
References
Harris JB, Gacic-Dobo M, Eggers R, Brown DW, Sodha SV. Global routine vaccination coverage, 2013. MMWR Morb Mortal Wkly Rep. 2014;63(46):1055–8 [http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6346a4.htm]
Arevshatian L, Clements C, Lwanga S, Misore A, Ndumbe P, Seward J, et al. An evaluation of infant immunization in Africa: is a transformation in progress? Bull World Health Organ. 2007;6:449–57.
Ministry of Public Health. Decision n° 0333/MSP/CAB of July 29, 2002 reorganizing the expanded program of immunization in Cameroon. [http://acdevcm.free.fr/sante/pev.html]
Institut National de la Statistique (Yaoundé, Cameroun) et ICF International (Calverton, Maryland, USA). Demographic and Health Survey, Cameroon 2011. [http://www.measuredhs.com/pubs/pdf/FR260/FR260.pdf]
World Health Organization, WHO. Global Alert and Response (GAR), Disease outbreak news: Wild poliovirus in Cameroon. 21 November 2013. [http://apps.who.int/csr/don/2013_11_21/en/index.html.
Global Polio Eradication Initiative. Polio this week. [http://www.polioeradication.org/Portals/0/Document/Data&Monitoring/Wild_poliovirus_list_2010-2015_17FEB.pdf]. [accessed 21 February 2015].
Wiysonge CS, Uthman OA, Ndumbe PM, Hussey GD. Individual and contextual factors associated with low childhood immunization coverage in Sub-Saharan Africa: a multilevel analysis. PLoS One. 2012;7(5):e37905. doi:10.1371/journal.pone.0037905.
International Federation of Red Cross and Red Crescent Societies. Disaster relief emergency fund (DREF). Cameroon: Wild Polio Virus Epidemic. Yaoundé; 2013. [http://www.ifrc.org/docs/Appeals/13/MDRCM017.pdf]
Global Polio Eradication Initiative. Polio Eradication & Endgame Strategic Plan 2013 – 2018. Geneva; 2012. [http://www.polioeradication.org/Portals/0/Document/Resources/StrategyWork/PEESP_ES_EN_A4.pdf]
World Health Organization. Training for mid-level managers. Module 7: The EPI coverage survey. Geneva; 2008. [http://whqlibdoc.who.int/hq/2008/WHO_IVB_08.07_eng.pdf]
Killip S, Mahfoud Z, Pearce K. What is an intracluster correlation coefficient? Crucial concepts for primary care researchers. Ann Fam Med. 2004;3:204–8.
Taljaard M, Donner A, Villar J, Wojdyla D, Velazco A, Bataglia V, et al. Global survey on maternal and perinatal health research group. Intracluster correlation coefficients from the 2005 WHO global survey on maternal and perinatal health: implications for implementation research. Paediatr Perinat Epidemiol. 2008;2:117–25. doi:10.1111/j.1365-3016.2007.00901.x.
Ukoumunne OC, Gulliford MC, Chinn S, Sterne JA, Burney PG. Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review. Health Technol Assess. 1999;5:iii–92.
Gulliford MC, Ukoumunne OC, Chinn S. Components of variance and intraclass correlations for the design of community-based surveys and intervention studies: data from the health survey for England 1994. Am J Epidemiol. 1999;9:876–83.
Doros G, Lew R. Design based on intra-class correlation coefficients. Am J Biostat. 2010;1:1–8. doi:10.3844/amjbsp.2010.1.8.
Odusanya OO, Alufohai EF, Meurice FP, Ahonkhai VI. Determinants of vaccination coverage in rural Nigeria. BMC Public Health. 2008;8:381. doi:10.1186/1471-2458-8-381.
Matsumura T, Nakayama T, Okamoto S, Ito H. Measles vaccine coverage and factors related to uncompleted vaccination among 18-month-old and 36-month-old children in Kyoto, Japan. BMC Public Health. 2005;5:59.
Sanou A, Simboro S, Kouyaté B, Dugas M, Graham J, Bibeau G. Assessment of factors associated with complete immunization coverage in children aged 12–23 months: a cross-sectional study in Nouna district, Burkina Faso. BMC Int Health Hum Rights. 2009;9 Suppl 1:S10. doi:10.1186/1472-698X-9-S1-S10.
Maina LC, Karanja S, Kombich J. Immunization coverage and its determinants among children aged 12–23 months in a peri-urban area of Kenya. Pan Afr Med J. 2013;14:3. doi:10.11604/pamj.2013.14.3.2181.
Etana B, Deressa W. Factors associated with complete immunization coverage in children aged 12–23 months in Ambo Woreda, Central Ethiopia. BMC Public Health. 2012;12:566. doi:10.1186/1471-2458-12-566.
Torun SD, Bakırcı N. Vaccination coverage and reasons for non-vaccination in a district of Istanbul. BMC Public Health. 2006;6:125.
Jani JV, De Schacht C, Jani IV, Bjune G. Risk factors for incomplete vaccination and missed opportunity for immunization in rural Mozambique. BMC Public Health. 2008;8:161. doi:10.1186/1471-2458-8-161.
Tadesse H, Deribew A, Woldie M. Predictors of defaulting from completion of child immunization in south Ethiopia, May 2008 – A case control study. BMC Public Health. 2009;9:150. doi:10.1186/1471-2458-9-150.
Animaw W, Taye W, Merdekios B, Tilahun M, Ayele G. Expanded program of immunization coverage and associated factors among children age 12–23 months in Arba Minch town and Zuria District, Southern Ethiopia, 2013. BMC Public Health. 2014;14:464. doi:10.1186/1471-2458-14-464.
Centers for Disease Control and Prevention (CDC). Assessing the risks for poliovirus outbreaks in polio-free countries--Africa, 2012–2013. MMWR Morb Mortal Wkly Rep. 2013;62(37):768–72.
Burton A, Monasch R, Lautenbach B, Gacic-Dobo M, Neill M, Karimov R, et al. WHO and UNICEF estimates of national infant immunization coverage: methods and processes. Bull World Health Organ. 2009;87:535–41.
Hosmer DW, Lemeshow S. Model-building strategies and methods for logistic regression. In: Applied logistic regression. Hoboken, NJ: John Wiley & Sons, Inc; 2005.
WHO-UNICEF. Estimates time series for Cameroon (CMR). [http://apps.who.int/immunization_monitoring/globalsummary/estimates?c=CMR]
Atuahene M, Adjuik M. Immunization coverage in an under-served Peri-urban community in Ghana. Int J Matern Child Health. 2014;2:32–8. doi:10.12966/ijmch.05.02.2014.
Ndiritu M, Cowgill KD, Ismail A, Chiphatsi S, Kamau T, Fegan G, et al. Immunization coverage and risk factors for failure to immunize within the Expanded Programme on Immunization in Kenya after introduction of new Haemophilus influenzae type b and hepatitis b virus antigens. BMC Public Health. 2006;6:132.
Lorenzo P, Ishata C, Wogba K, Marta GD, Olivier R, William AP, et al. Intervene before leaving: clustered lot quality assurance sampling to monitor vaccination coverage at health district level before the end of a yellow fever and measles vaccination campaign in Sierra Leone in 2009. BMC Public Health. 2012;12:415. doi:10.1186/1471-2458-12-415.
Nath B, Singh JV, Awasthi S, Bhushan V, Kumar V, Singh SK. A study on determinants of immunization coverage among 12–23 months old children in urban slums of Lucknow district, India. Indian J Med Sci. 2007;61:598–606.
Kobayashi M, Hirakawa K, Sawada M, Suzuki C, Saikawa S, Ando H, et al. Vaccination coverage of poliomyelitis among less than 5-year old children in the markets of Niger. Jpn J Infect Dis. 2003;56:175–7.
Waters HR, Dougherty L, Tegang SP, Tran N, Wiysonge CS, Long K. Coverage and costs of childhood immunizations in Cameroon. Bull World Health Organ. 2004;9:668–75.
Miles M, Ryman TK, Dietz V, Zell E, Luman ET. Validity of vaccination cards and parental recall to estimate vaccination coverage: a systematic review of the literature. Vaccine. 2013;12:1560–8.
Feldman-Savelsberg P, Ndonko FT, Schmidt-Ehry B. Sterilizing vaccines or the politics of the womb: retrospective study of a rumor in Cameroon. Med Anthropol Q. 2000;2:159–79.
Jegede AS. What led to the Nigerian boycott of the polio vaccination campaign? PLoS Med. 2007;3:73.
Acknowledgements
The following associations supported this study: Mingha Africa Onlus (Italy), and Projet Intégré pour la Promotion de l’Auto-Developpement – PIPAD - (Cameroon). The conception, methods and results of the study were not influenced by the received support. The authors would like to thank the staff of the Dschang Health District and the students of the Master in Public Health and Epidemiology, Department of Biomedical Sciences, University of Dschang (Cameroon).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
GianlucaR conceived of the study, participated in its design and coordination, data collection and interpretation, and drafted the manuscript. AM conceived of the study, participated in its design, data collection and interpretation, and drafted the manuscript. PP conceived of the study, performed data analysis, and participated to data interpretation. RMB participated in the design of the study and coordinated data collection. MSS conceived of the study and participated in its design and data collection. GBM participated in the design of the study, data collection and interpretation. PS: conceived of the study and participated to data interpretation. VV conceived of the study, participated in its design and data interpretation. GiovanniR conceived of the study and participated in its design, data interpretation and manuscript revision. All authors read and approved the different study steps and the final manuscript.
Gianluca Russo and Alessandro Miglietta are co-authors.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Russo, G., Miglietta, A., Pezzotti, P. et al. Vaccine coverage and determinants of incomplete vaccination in children aged 12–23 months in Dschang, West Region, Cameroon: a cross-sectional survey during a polio outbreak. BMC Public Health 15, 630 (2015). https://doi.org/10.1186/s12889-015-2000-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-015-2000-2