Abstract
Background
Overweight or obesity is detrimental during pregnancy. We studied time trends in the educational gradient of overweight and obesity among pregnant women. Differences in overweight and obesity by area of residence and country of birth were also examined.
Methods
The study was based on the Swedish Medical Birth Register between 1992 and 2010 and included 1,569,173 singleton pregnancies. Weight and height were registered during the first visit at the antenatal-care clinic. Data on education, country of birth, and area of residence were derived from registers with national coverage.
Results
In 2008–2010, 32% of Swedish nulliparous pregnant women were overweight or obese. The relative risk of obesity among lower educated women compared to women with higher education increased from 1.91 (95% confidence interval: 1.85-1.97) in 1992–1995 to 2.09 (95% confidence interval: 2.05-2.14) in 2008–2010. There was an inverse linear relationship between risks of overweight or obesity, and population density and type of residence municipality. An excessive gestational weight gain according to the American Institute of Medicine was observed among 57-63% of the overweight or obese women, but there were small differences by education. Pregnant women born in Africa, Middle East or Latin America had higher risks of being overweight or obese compared to women born in Sweden.
Conclusions
The prevalence of obesity as well as the social inequalities in obesity during pregnancy increased in Sweden between 1992 and 2010. Further understanding of social inequalities and geographical differentials in health behaviours of pregnant women is needed when planning public health interventions.
Similar content being viewed by others
Background
As obesity has taken epidemic proportions, higher prevalence of obesity is observed also in pregnant women [1-3]. Maternal overweight or obesity during pregnancy can lead to several adverse outcomes for both mother and foetus. Obese women are more likely to have gestational diabetes mellitus, hypertension, pre-eclampsia, other obstetric complications and caesarean section [1,4,5]. Pre-pregnancy obesity is further associated with increased risk of adverse pregnancy outcomes such as stillbirth [6], preterm delivery [3], birth injuries [7], and that the new-borns become large for gestational age [1,4,5] with subsequent increased risk for childhood obesity [1]. Maternal gestational weight gain (GWG) is also related to these adverse pregnancy and birth outcomes [8,9], including an increased risk of macrosomia at birth [9], and increased risk of childhood obesity [10,11]. Thus, obesity in early pregnancy and also excessive GWG are known to have consequences for pregnancy and birth outcomes and the risk of childhood obesity in the next generation.
It is well known that individuals with lower education and socioeconomic position are more often overweight or obese in comparison to people with higher education or socioeconomic position. This social inequality is also observed in pregnant women [5,12,13]. A steepened social gradient has been implied in the Nordic countries but the evidence for increased social inequality of overweight and obesity is inconsistent [14]. Thus, further knowledge about time trends of socioeconomic inequalities in overweight or obesity is needed.
An urban–rural gradient of obesity has also been observed [12,15,16], with lower risk of obesity in urbanized areas. Among Swedish pregnant women, living in rural areas has been shown to almost double the odds of obesity after taking occupation and education into account [12]. Also in young Swedish males an urban–rural gradient is observed taking socioeconomic position, intelligence quotient and parental education into account [16]. The risk of obesity is further related to country of birth and data from the Swedish Medical Birth Register indicate that women with non-Nordic origin have higher prevalence of overweight [3], but more specific results on country of birth are lacking. Other European studies indicate higher pre-pregnancy BMI among women from African and Middle Eastern countries compared to the majority population in each country [17].
The main aim was to explore time trends of weight status among pregnant women in Sweden and to investigate if the educational gap in overweight or obesity has increased, decreased or remained stable during the last two decades. Additional aims were to explore differences in overweight and obesity according to area of residence and country of birth.
Methods
Study population
The study was based on the Swedish Medical Birth Register between 1992 and 2010. This is a national register including almost all pregnancies resulting in labour [18]. In 2010, 99.4% of all newborn were reported to the register [2]. Data are derived from medical records written at the antenatal health care centres, obstetric departments, and sometimes neonatal units. The present study includes singleton pregnancies with data on weight and height from the first visit to the antenatal-care (n = 1,569,173). Data on GWG were available for 38% (n = 596,699) of the pregnancies.
Weight and height were registered during the first visit at the antenatal-care clinic. This visit most often takes place between gestational week 8 to 12 [18]. According to the guidelines for antenatal care, weights registered in the medical records should be measured by the midwife. Thus, most weights are measured, even though some weights may be self-reported. GWG was calculated by subtracting weight at the first antenatal care visit from the weight at delivery. Body mass index (BMI) was calculated as weight (kg) divided by height (m) squared and categorised according to the World Health Organization (WHO) categories [19]: underweight (<18.5 kg/m2), normal weight (18.5-24.9 kg/m2), overweight (25.0-29.9 kg/m2) and obese (≥30.0 kg/m2). Maternal age was categorized into five groups: ≤24 years, 25–29 years, 30–34 years, 35–39 years, and 40 years or higher.
Data on education, country of birth, and area of residence were derived from the Longitudinal Integration Database for Health Insurance and Labour Market Studies (LISA) held by Statistics Sweden. Low education was defined as elementary school or high school, and high education as university level or doctoral degree. When used as a covariate, education was categorized into five levels: ≤ 9 years of elementary school, higher than 9 years of elementary school but less than 3 years of high school, 3 years of high school, higher than high school but less than 3 years of higher education, ≥ 3 years of higher education or doctoral degree. Area of residence was applied by an abbreviated version of a classification with seven categories mostly based on population-density but also on size and location of the municipalities (Table 1). The following categories were used in the abbreviated version: Stockholm area, Gothenburg area, Malmö area, larger municipalities, central district municipalities, densely populated municipalities, and sparsely populated municipalities. To investigate the magnitude of GWG, the recommendations of Institute of Medicine (IOM) [8,20] were used. The recommendations are as follows: 12.7-18.1 kg (for women who are underweight), 11.3-15.9 kg (for women who are normal weight), 6.8-11.3 kg (for overweight women), and 5.0-9.1 kg (for obese women). The study was approved by the Regional Ethical Review Board in Stockholm (“Regionala etikprövningsnämnden i Stockholm”), Sweden (Dnr 2011/591-31/5).
Statistical analyses
Linear regression models where used to calculate age-adjusted prevalence. Relative risks (RR) of overweight versus normal weight and obesity versus normal weight were estimated using Poisson regression with robust variance with the Genmod procedure in SAS 9.3. Childbearing is associated with weight gain, also in the long term [21,22], and pregnancy related weight retention is highly variable among women [23]. We stratified for parity and used only nulliparous women in the time trend analyses of overweight and obesity prevalence. These analyses were further adjusted for maternal age. To increase the power, all other relative risk estimates were based on all singleton pregnancies between 1992 and 2010. These relative risks were adjusted for maternal age, parity, education, year of birth, and country of birth when not used as the outcome. Relative risks of GWG above the IOM recommendations depending on education were calculated within strata of normal weight, overweight and obesity. Women gaining less than the recommendations were excluded.
Results
Time trends and the educational gradient
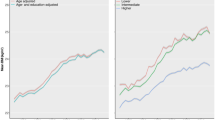
The overweight and obesity prevalence among all singleton pregnancies in 2008–2010 were 25% and 12%, respectively. Prevalence of overweight and obesity among nulliparous women at their first visit to the antenatal-care clinic between 1992 and 2010 are presented in Table 2. The prevalence of overweight and obesity has increased since 1992. During the 21th century, the increase seems to have levelled off but an increase in obesity prevalence was still observed among lower educated women (Table 2). The relative risk of obesity among women with low education compared to higher educated women increased slightly from 1992–1995 to 2008–2010 (Figure 1). In absolute terms, the differences in prevalence between high and low educated women increased more than two-fold from 3.1% in 1992–1995 to 6.7% in 2008–2010 (Table 2).
Time trends in relative risks of overweight and obesity between Swedish nulliparous women with low vs high education. BMI was assessed at the first visit to the antenatal-care clinic. aRelative risk (95% confidence interval) for overweight/obesity among women with low education compared to higher educated women, adjusted for maternal age.
Area of residence and country of birth
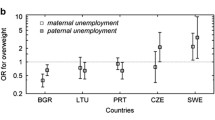
There were large differences in overweight and obesity by type of residence municipality. The relative risks of overweight and obesity were inversely related to population density and women living in sparsely populated municipalities had the highest risk (Figure 2). Pregnant women born in Africa, Middle East or Latin America had higher risks of being overweight or obese compared to women born in Sweden with adjustment for level of education. In contrast, women born in Europe (excluding the Nordic countries), North America, Australia, New Zealand or former USSR (Union of Soviet Socialist Republics) had lower risk of overweight or obesity, also adjusted for education. Asian born mothers had the lowest risk of both overweight and obesity (Table 3). Similar results were obtained after adjusting for gestational week at the first antenatal care visit.
Risk of overweight or obesity among pregnant women in relation to population density of residence municipality. BMI was assessed at the first visit to the antenatal-care clinic. RR Relative Risk n: Stockholm area: overweight = 69 273, obese = 24 068, Gothenburg area: overweight = 32 892, obese = 11 814, Malmö area: overweight = 22 272, obese = 8 307, larger municipalities: overweight = 136 935, obese = 59 021, central district municipalities: overweight = 64 299, obese = 29 517, densely populated municipalities: overweight = 19 490, obese = 9 085, sparsely populated municipalities: overweight = 20 642, obese = 10 146. aCalculated among all pregnancies between 1992 and 2010, and adjusted for maternal age, education, parity, country of birth, and year of birth.
BMI in early pregnancy and total gestational weight gain
BMI in early pregnancy and total GWG by level of education among nulliparous women are shown in Table 4. Among all parities, 63% of the overweight and 57% of the obese women gained weight above the IOM recommendations. There were only minor educational differences in total GWG. However, among those with normal weight, women with a low education had a higher risk of excessive GWG compared to women with a high education, after adjusting for BMI at the first antenatal care visit, maternal age, parity, year of birth, and country of birth (adjusted RR: 1.08 [95% confidence interval (CI): 1.07-1.09]). In contrast, lower educated overweight or obese women had slightly lower risk of excessive weight gain than women with higher education (adjusted RR: 0.98 [95% CI: 0.97-0.99], and adjusted RR: 0.98 [95% CI: 0.96-0.99], respectively).
Discussion
The prevalence of overweight and obesity among Swedish pregnant women has increased since 1992, especially among those with low education. Women with low education or living in sparsely populated areas are at higher risk of obesity in early pregnancy.
In 2008–2010, 25% of Swedish pregnant women were overweight and 12% were obese at their first visit to the antenatal care clinic. This is slightly higher than pre-pregnancy weights observed in other countries [24-27]. Discrepancies are that most previous studies investigated somewhat older data, and that weight was assessed early in the first trimester instead of pre-pregnancy weight in the present study. A GWG rate of 0.22 kg per week has previously been estimated during the first trimester [28] and the most frequent time point for the initial visit to the antenatal clinic is at ten weeks of gestation. If a 2.2 kg weight gain before the first antenatal care visit was anticipated for all participants, estimated pre-pregnancy obesity prevalence among nulliparous women was 1.0-1.6 percent units lower than the prevalence observed in Table 2. According to the Danish Medical Birth Register, 21% of the pregnant women had overweight and 12% had obesity during 2004–2010 [24]. In the Norwegian Mother and Child Cohort Study conducted between 1999 and 2008, 22% of the women becoming pregnant were overweight and 9% were obese [25].
Our results showed a slower increase in prevalence of obesity during the 21th century, which is in accordance with previous findings in Swedish populations [29-31]. However, Swedish data on whether the socioeconomic gradient of obesity is changing are inconsistent [14]. A previous Swedish study has indicated a narrowing of the socioeconomic gap for adults aged 25–44 years between 1988–1989 and 1996–1997, whereas it seemed stable for adults 45–64 years [32]. In contrast, a higher increase in prevalence of obesity in lower social classes has been suggested in Stockholm County during the 21th century [30]. Increased socioeconomic gap in overweight and obesity has also been shown among young Swedish men between 1970 to 2000 [33]. An increased socioeconomic difference in obesity prevalence from 1990–1995 to 2002–2007 was further observed in the North of Sweden [29]. Using education as a measure of socioeconomic position, the present study indicates that the socioeconomic gap in obesity is increasing, both in relative and absolute terms. In contrast, the socioeconomic difference in overweight seems to be stable over time. We can only speculate in why the socioeconomic gap of obesity appears to increase but the increasing physical activity in Sweden seems to be mainly among individuals with higher education [29]. Further, individuals with higher education may be moving to urbanized areas, with its beneficial contextual factors, to a higher degree [29]. It may also be speculated that individuals without university education are more excluded from the labour market today or that health literacy has become more central in the health care system.
In line with other Swedish studies [12,15,16,29], an urban–rural gradient of overweight and obesity was observed among pregnant women independently of educational level. The sample size in the present study allowed for a more detailed categorisation of residential area than the often used urban/rural classification. Interestingly, the risk for overweight or obesity seems to increase linearly with decreasing population density of municipality of residence based on comparisons of risk ratios. Possible explanations may be that habitants in rural areas are more dependent on motorized transportation and higher accessibility to training facilities in urbanized areas. Also other contextual factors could contribute, such as that a larger part of the population is highly educated in urbanized areas, irrespective of the own educational level.
Our results show both increased and decreased risks of overweight or obesity in different groups of non-Swedish born pregnant women compared to Swedish born pregnant women. Women born in Africa, the Middle East, and Latin America had higher risk compared to native Swedes, whereas women born in other countries had lower risk. These risks remained after adjustment for education. Other studies [27,34,35] confirm ethnical differences in obesity prevalence, especially among immigrants from Middle East or Latin America. Compared to native Swedes, more than twice as high obesity prevalence has been observed among women from Middle East [35], Turkey [34] and Chile [34]. Likewise, in a Dutch study [27], ethnical differences in GWG and postpartum weight retention were observed, with Turkish women being at higher risk for retaining weight. Women born in other Nordic countries than Sweden had a slight over risk of obesity. Previous studies have shown higher BMI and body fat percentage among Finnish-born women compared to native Swedes [36,37]. Possible factors explaining the differences in obesity between countries of birth could be socioeconomic inequalities, difficulties to be included on the labour market, diverse lifestyle, genetic susceptibility, language barriers and cultural attitudes to sickness and health care [35].
Large proportions (57-63%) of the overweight and obese women gained more in weight during pregnancy than recommended by the IOM [8,20] and were at increased risk of short-term and long-term complications to the mother and the offspring during pregnancy, delivery and the post-term period. Our results indicate that further research is needed on evaluations of primary prevention interventions which might be implemented in routine antenatal care to limit excessive GWG among Swedish pregnant women. While the educational differentials in body weight in early pregnancy were strongly inversely related to maternal level of education, GWG showed less strong associations. In line with ours, a recent study showed that excessive GWG was more prevalent among low educated normal weighted women whereas education did not seem to protect against excessive GWG among overweight and obese women [13]. In fact, we observed a slightly higher risk of excessive gestational weight gain among higher educated overweight or obese women, also after adjusting for pre-pregnancy BMI.
The present study has strengths and limitations. It is a strength that it is nationwide by including almost all pregnancies progressing to labour in Sweden during the investigated time period. Due to the large number of women, we had sufficient power to investigate residential area and country of birth at more detailed levels. Since nearly 75% of the Swedish women have at least one child [22], the results are believed to be generalizable to the fertile Swedish female population. The study is limited by that the Swedish Medical Birth Register does not contain data on weight before conception. Weight was assessed at the first visit to the antenatal care clinic. Most of these visits are scheduled between gestational week 8 to 12 [18].
Conclusions
The prevalence of obesity as well as the social inequalities in obesity during pregnancy increased in Sweden between 1992 and 2010. Pregnancy is thought to be a susceptible period where motivation for risk-reducing behaviour changes is higher [38]. Antenatal care could therefore be a suitable arena for preventive interventions. Such interventions could benefit both mothers and their children in the short as well as long term. To reduce social inequalities in maternal gestational overweight and obesity, emphasis should be on understanding health behaviour change and health literacy in different socioeconomic and ethnic groups and how effective primary and clinical interventions might be implemented in primary and antenatal care settings.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- GWG:
-
Gestational weight gain
- IOM:
-
Institute of Medicine
- RR:
-
Relative risk
- WHO:
-
World Health Organization
References
Guelinckx I, Devlieger R, Beckers K, Vansant G. Maternal obesity: pregnancy complications, gestational weight gain and nutrition. Obes Rev. 2008;9(2):140–50.
The National Board of Health and Welfare. Sveriges officiella statistik. Statistik – Hälso- och Sjukvård. Graviditeter, förlossningar och nyfödda barn. Medicinska födelseregistret 1973–2012. Assisterad befruktning, 1991–2011 (Official statistics of Sweden. Statistics – Health and Medical Care. Pregnancies, Deliveries and Newborn Infants. The Swedish Medical Birth Register 1973–2012. Stockholm: Assisted Reproduction, treatment 1991–2011; 2013.
Cnattingius S, Villamor E, Johansson S, Edstedt Bonamy AK, Persson M, Wikstrom AK, et al. Maternal obesity and risk of preterm delivery. JAMA. 2013;309(22):2362–70.
Sebire NJ, Jolly M, Harris JP, Wadsworth J, Joffe M, Beard RW, et al. Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. Int J Obes Relat Metab Disord. 2001;25(8):1175–82.
Athukorala C, Rumbold AR, Willson KJ, Crowther CA. The risk of adverse pregnancy outcomes in women who are overweight or obese. BMC Pregnancy Childbirth. 2010;10:56.
Aune D, Saugstad OD, Henriksen T, Tonstad S. Maternal body mass index and the risk of fetal death, stillbirth, and infant death: a systematic review and meta-analysis. JAMA. 2014;311(15):1536–46.
Blomberg M. Maternal obesity, mode of delivery, and neonatal outcome. Obstet Gynecol. 2013;122(1):50–5.
IOM (Institute of Medicine) and NRC (National Research Council). Weight Gain During Pregnancy: Reexamining the Guidelines. Washington (DC): The National Academies Press; 2009.
Viswanathan M, Siega-Riz AM, Moos MK, Deierlein A, Mumford S, Knaack J, et al. Outcomes of maternal weight gain. Evid Rep Technol Assess (Full Rep). 2008;168:1–223.
Ludwig DS, Rouse HL, Currie J. Pregnancy weight gain and childhood body weight: a within-family comparison. PLoS Med. 2013;10(10):e1001521.
Dello Russo M, Ahrens W, De Vriendt T, Marild S, Molnar D, Moreno LA, et al. Gestational weight gain and adiposity, fat distribution, metabolic profile, and blood pressure in offspring: the IDEFICS project. Int J Obes (Lond). 2013;37(7):914–9.
Edvardsson K, Lindkvist M, Eurenius E, Mogren I, Small R, Ivarsson A. A population-based study of overweight and obesity in expectant parents: socio-demographic patterns and within-couple associations. BMC Public Health. 2013;13:923.
Holowko N, Mishra G, Koupil I. Social inequality in excessive gestational weight gain. Int J Obes (Lond). 2014;38(1):91–6.
Magnusson M, Sorensen TI, Olafsdottir S, Lehtinen-Jacks S, Holmen TL, Heitmann BL, et al. Social Inequalities in Obesity Persist in the Nordic Region Despite Its Relative Affluence and Equity. Curr Obes Rep. 2014;3:1–15.
Moraeus L, Lissner L, Yngve A, Poortvliet E, Al-Ansari U, Sjoberg A. Multi-level influences on childhood obesity in Sweden: societal factors, parental determinants and child’s lifestyle. Int J Obes (Lond). 2012;36(7):969–76.
Neovius M, Rasmussen F. Place of residence and obesity in 1,578,694 young Swedish men between 1969 and 2005. Obesity (Silver Spring). 2008;16(3):671–6.
Jenum AK, Sommer C, Sletner L, Morkrid K, Baerug A, Mosdol A. Adiposity and hyperglycaemia in pregnancy and related health outcomes in European ethnic minorities of Asian and African origin: a review. Food Nutr Res 2013, 57. doi:10.3402/fnr.v57i0.18889
Centre for Epidemiology, the National Board of Health and Welfare. The Swedish Medical Birth Register - A summary of content and quality. Stockholm: Centre for Epidemiology, the National Board of Health and Welfare; 2003.
Report of a WHO consultation, Report of a WHO consultation. Obesity: preventing and managing the global epidemic. World Health Organ Tech Rep Ser. 2000;894:1–253.
Rasmussen KM, Catalano PM, Yaktine AL. New guidelines for weight gain during pregnancy: what obstetrician/gynecologists should know. Curr Opin Obstet Gynecol. 2009;21(6):521–6.
Gunderson EP, Murtaugh MA, Lewis CE, Quesenberry CP, West DS, Sidney S. Excess gains in weight and waist circumference associated with childbearing: The Coronary Artery Risk Development in Young Adults Study (CARDIA). Int J Obes Relat Metab Disord. 2004;28(4):525–35.
Linne Y, Dye L, Barkeling B, Rossner S. Weight development over time in parous women–the SPAWN study–15 years follow-up. Int J Obes Relat Metab Disord. 2003;27(12):1516–22.
Gore SA, Brown DM, West DS. The role of postpartum weight retention in obesity among women: a review of the evidence. Ann Behav Med. 2003;26(2):149–59.
Ovesen P, Rasmussen S, Kesmodel U. Effect of prepregnancy maternal overweight and obesity on pregnancy outcome. Obstet Gynecol. 2011;118(2 Pt 1):305–12.
Cupul-Uicab LA, Skjaerven R, Haug K, Melve KK, Engel SM, Longnecker MP. In utero exposure to maternal tobacco smoke and subsequent obesity, hypertension, and gestational diabetes among women in the MoBa cohort. Environ Health Perspect. 2012;120(3):355–60.
Casas M, Chatzi L, Carsin AE, Amiano P, Guxens M, Kogevinas M, et al. Maternal pre-pregnancy overweight and obesity, and child neuropsychological development: two Southern European birth cohort studies. Int J Epidemiol. 2013;42(2):506–17.
Van Poppel MN, Hartman MA, Hosper K, Van Eijsden M. Ethnic differences in weight retention after pregnancy: the ABCD study. Eur J Public Health. 2012;22(6):874–9.
Walter JR, Perng W, Kleinman KP, Rifas-Shiman SL, Rich-Edwards JW, Oken E. Associations of trimester-specific gestational weight gain with maternal adiposity and systolic blood pressure at 3 and 7 years postpartum. Am J Obstet Gynecol 2014. doi: 10.1016/j.ajog.2014.11.012
Norberg M, Lindvall K, Stenlund H, Lindahl B. The obesity epidemic slows among the middle-aged population in Sweden while the socioeconomic gap widens. Glob Health Action 2010, 3. doi: 10.3402/gha.v3i0.5149
Neovius K, Johansson K, Kark M, Tynelius P, Rasmussen F. Trends in self-reported BMI and prevalence of obesity 2002–10 in Stockholm County, Sweden. Eur J Public Health. 2013;23(2):312–5.
Sundquist J, Johansson SE, Sundquist K. Levelling off of prevalence of obesity in the adult population of Sweden between 2000/01 and 2004/05. BMC Public Health. 2010;10:119.
Lissner L, Johansson SE, Qvist J, Rossner S, Wolk A. Social mapping of the obesity epidemic in Sweden. Int J Obes Relat Metab Disord. 2000;24(6):801–5.
Kark M, Rasmussen F. Growing social inequalities in the occurrence of overweight and obesity among young men in Sweden. Scand J Public Health. 2005;33(6):472–7.
Gadd M, Sundquist J, Johansson SE, Wandell P. Do immigrants have an increased prevalence of unhealthy behaviours and risk factors for coronary heart disease? Eur J Cardiovasc Prev Rehabil. 2005;12(6):535–41.
Faskunger J, Eriksson U, Johansson SE, Sundquist K, Sundquist J. Risk of obesity in immigrants compared with Swedes in two deprived neighbourhoods. BMC Public Health. 2009;9:304.
Carlsson AC, Wandell P, Riserus U, Arnlov J, Borne Y, Engstrom G, et al. Differences in anthropometric measures in immigrants and Swedish-born individuals: Results from two community-based cohort studies. Prev Med. 2014;69C:151–6.
Lahmann PH, Lissner L, Gullberg B, Berglund G. Differences in body fat and central adiposity between Swedes and European immigrants: the Malmo Diet and Cancer Study. Obes Res. 2000;8(9):620–31.
Phelan S. Pregnancy: a “teachable moment” for weight control and obesity prevention. Am J Obstet Gynecol. 2010;202(2):135. e131–138.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
All authors have made substantial contributions to conception, design and interpretation of data. SL performed the statistical analyses. HB wrote the manuscript. FR provided critical feedback on the manuscript. All authors read and approved the final manuscript.
An erratum to this article is available at http://dx.doi.org/10.1186/s12889-016-3156-0.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Bjermo, H., Lind, S. & Rasmussen, F. The educational gradient of obesity increases among Swedish pregnant women: a register-based study. BMC Public Health 15, 315 (2015). https://doi.org/10.1186/s12889-015-1624-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-015-1624-6