Abstract
Background
A peripherally inserted central catheter (PICC) with its tip preferably in the vena cava is essential in caring for patients with chronic conditions in general pediatrics. However, PICC-related complications are concerning and warrant further investigations.
Objectives
To share the experience of a nurse-inserted peripherally inserted central catheters (PICC) program initiated in a general pediatric department.
Methods
A retrospective descriptive cohort study based on a prospectively collected database was conducted. All PICCs inserted in the departments of gastroenterology and pulmonology in a tertiary pediatric center from Dec. 2015 to Dec. 2019 were included in the study. Complications and risk factors were analyzed by comparing cases with and without complications. We also reported arm movements in correcting mal-positioned newly-inserted PICCs.
Results
There were 169 cases with a median (IQR) age of 42(6, 108) months who received PICC insertion during a 4-year period. Inflammatory bowel disease was the leading diagnosis accounting for 25.4% (43/169) of all cases. The overall complication rate was 16.4 per 1000 catheter days with malposition and occlusion as the two most common complications. Multivariate models performed by logistic regression demonstrated that young age [p = 0.004, OR (95%CI) = 0.987(0.978, 0.996)] and small PICC diameter (1.9Fr, p = 0.003, OR (95%CI) = 3.936(1.578, 9.818)] were risk factors for PICC complications. Correction of malpositioned catheters was attempted and all succeeded in 9 eligible cases by using arm movements.
Conclusion
The nurse-inserted PICC program in general pediatrics is feasible with a low rate of complications. PICC tip malposition and occlusion were two major PICC-related complications when low age and small catheter lumina were major risk factors. Furtherly, arm manipulation potentially is an easy and effective approach for correcting malpositioned newly-inserted PICC catheters.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Key messages
The nurse-inserted PICC program in general pediatrics out of intensive care units is feasible, with a low rate of complications.
PICC tip malposition and occlusion were two major PICC-related complications in the nurse-inserted PICCs, and younger age and smaller catheter lumina were risk factors.
Arm manipulation, as an easily performed practice, is effective in correcting mal-positioned newly-inserted PICC catheters.
Background
Obtaining peripheral venous access in pediatric patients with chronic disease for the purpose of infusing parenteral nutrition or stimulant drugs is often challenging for nursing professionals. A peripherally inserted central catheter (PICC) with its tip preferably in the vena cava allows for middle to long-term intravenous therapy, blood sampling, and reductions in repeated intravenous catheterizations [1, 2]. Though PICC insertion is a relatively convenient and effective technique, it can cause life-threatening complications such as catheter-related bloodstream infection [3, 4] and pericardial tamponade [5,6,7,8].
PICCs, inserted by nurses at the bedside, have been routinely used in the neonatal and pediatric intensive care units for decades in our hospital, a leading pediatric academic center in China. With increasing numbers of pediatric patients with chronic conditions referred from other hospitals, PICC insertion in pediatric sub-specialties other than intensive care units, such as the department of gastroenterology and pulmonology, was promoted. However, interventional pediatric radiologists inserting PICC under fluoroscopic guidance, which is common in developed countries, is not available yet in China. Therefore, a nurse-led PICC insertion program outside of the intensive care unit was established in the department of gastroenterology and pulmonology in Dec. 2015. Since then, there have been 169 patients who received PICC insertion in the department. The objective of this study was to share the experience of a nurse-inserted pediatric PICC program outside intensive care units, mainly focusing on PICC-related complications and risk factors.
Patients and methods
Study design, setting, and participants
This is a retrospective cohort study. All inpatients with PICC insertion in the department of gastroenterology and pulmonology at the Children’s Hospital of Fudan University from Dec. 2015 through Dec. 2019 were included in the study. The department is a leading pediatric referral center in China for the treatment of chronic pediatric gastrointestinal and lung diseases, such as infant onset inflammatory bowel disease, intractable diarrhea, infant chronic lung disease, and pneumonia with complications. Most of the admitted cases were referred from other hospitals across China. The study was approved by the Institutional Review Board of the Children’s Hospital of Fudan University.
The indications for PICC insertion in the department included: patients requiring intermediate- to long-term intravenous access for medications, fluid therapy, or parenteral nutrition; expected difficult peripheral IV catheter insertion during hospitalization. Contraindications included infection at the insertion site; damaged or thrombosed vessels caused by previous catheter insertions or repeated attempts; severe coagulopathy or thrombocytopenia. All PICCs performed in the department during the 4-year period were included in the current study.
PICC practice
Informed consent was obtained from the parent or guardian. PICC insertion occurred in a therapeutic suite using a sterile technique and a topical anesthetic was applied by PICC nurses. All involved nurses need to get a 6-month training in PICC insertion, dressing, and troubleshooting prior to an independent performance, and they need to perform at least 10 PICCs per year to maintain qualifications. The insertion procedure and post-insertion maintenance were guided by institutional protocol. Bedside ultrasound was used in assessing the diameters of targeted veins and guiding needle insertion mainly in elder children with Fr 3.0 or 4.0 catheters, but not in infants with relatively smaller veins. The placement of the PICC tips was confirmed by x-ray after insertion with tips in the vena cava as the preferred position [1]. Of note, if PICC tip malposition occurred in upper limb insertion, a serial arm movements procedure as reported by Nadroo et al. was attempted to correct the malposition in eligible patients [9]. For PICCs inserted via basilic veins, the arm was abducted at the shoulder and the elbow extended as far as possible, then adducted at the shoulder and flexed at the elbow; for PICCs inserted via cephalic veins, the arm was adducted at the shoulder and extended at the elbow as far as possible, then the shoulder was abducted and the elbow flexed. After the movements, a repeat x-ray was performed within 24 hours to confirm the placement of the PICC.
Data collection and definition
All data including patient gender, age, clinical diagnosis, indications for PICC, insertion procedure, post-insertion x-ray, PICC dwell time, and complications were extracted from a prospectively registered database. All clinical data related to the PICC were timely input into the database when the patient was in the hospital. PICC procedure time was recorded from entry into the procedure room to exit from the room after completion of the procedure. PICC tip placement was determined by radiography as either central or non-central. Reasons for PICC removal were categorized as planned if the therapy ended, otherwise categorized as unplanned removal. Complications of PICC were defined as following [10]: malposition, the inappropriate position of PICC tip after insertion; catheter occlusion, blockage of the catheter; dislodgment, accidental removal of PICC; fracture and fragmentation, catheter breakage; mechanical phlebitis, clinical signs of tenderness, erythema, and edema at insertion site; infection, systemic or insertion site bacteremia or fungi infection.
Statistical analysis
Analyses were performed using SPSS 25 (SPSS, Inc., Chicago, IL). Patient characteristics were demonstrated as counts with proportions for categorical variables and median with interquartile range (IQR) for continuous variables. The comparison between patients with and without complications was conducted using Pearson chi-square or Fisher’s exact test for categorical variables and the Mann-Whitney U test for continuous variables. The variables with a p-value less than 0.1 were collected and used to study the risk factors for PICC-related complications by logistic regression analyses using multivariate models. PICC diameter choice was significantly dependent on age, therefore, PICC diameter and age were collinear variables and put in the model separately. A p-value< 0.05 was considered statistically significant.
Results
PICC and patient characteristics
There were 169 cases of patients with a median (IQR) age of 42(6, 108) months who received PICC insertion during the 4-year period. Inflammatory bowel disease (43/169, 25.4%) was the leading diagnosis in all cases followed by chronic diarrhea(18/169, 10.7%), upper gastrointestinal bleeding(18/169, 10.7%), pneumonia(15/169, 8.9%) etc. Requiring parenteral nutrition was the major indication for PICC insertion in 65.1% (110/169) cases followed by expected intravenous infusion requirement> 6 days (49/169, 29.0%) and difficult peripheral intravenous catheter insertion (10/169, 5.9%). For all PICC insertions, one puncture success rate was 52.7% (89/169); the total device days was 2859, with a median catheter retention duration of 12 (8, 20) days; 32.5% (55/169) received 1.9 Fr catheter; 43.2%(73/169) was inserted through a basilic vein.
Complications of PICC and risk factors
Forty-seven onsets of complications occurred in 43 cases including 16 catheter malposition, 14 catheter occlusion, 9 mechanical phlebitis, 6 external breakages, 1 catheter-related bloodstream infection, 1 bleeding, and 1 limb edema. The total complication rate was 16.4 per 1000 catheter days. 56.3% (9/16) of malposition and 100% (14/14) of occlusion occurred in 1.9Fr cases. The complications of PICC were demonstrated in table 1.
The comparison between patients with and without PICC complications demonstrated that age, procedure time, catheter diameter, and puncture attempts were potential risk factors for complications with a p-value less than 0.1(Table 2). As age and catheter diameter were collinear variables, two multivariate models were performed by logistic regression, with the results demonstrating that young age and small PICC diameter were risk factors for PICC complications (Table 3).
PICC malposition correction
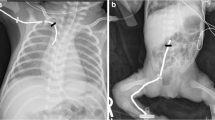
Of 16 incidents of PICC malposition, 9 cases eligible for arm movement were successfully corrected by arm movements. The typical x-ray images before and after the maneuver were demonstrated in fig. 1 (6 cases were demonstrated, while the other 3 cases were reported previously [11]).
X-ray images of PICC before(a) and after arm movements(b). 1a/1b, 13-year boy, right basilic vein insertion, 4.0 Fr catheter, the tip was in the right jugular vein before arm movements. 2a/2b, 6-year girl, right basilic vein insertion, 4.0 Fr catheter, the tip was in the left subclavian vein before arm movements. 3a/3b, 5-year boy, right cephalic vein insertion, 4.0 Fr catheter, the tip was in the left subclavian vein before arm movements. 4a/4b, 5-month boy, left axillary vein insertion, 1.9Fr catheter, the tip was in the left jugular vein before arm movements. 5a/5b, 7-year boy, right cephalic vein insertion, 3.0 Fr catheter, the tip was in the right jugular vein before arm movements. 6a/6b, 20-month boy, right basilic vein insertion, 3.0 Fr catheter, the tip was in the left brachiocephalic vein before arm movements. Tips of all PICCs were in the superior vena cava after arm movements
Discussion
This study reported the experience of a nurse-inserted PICC program in a pediatric sub-specialty outside intensive care units in a tertiary children’s hospital from China. Of all cases, 83.4%(141/169) were from the department of gastroenterology with inflammatory bowel disease as the most common diagnosis while 16.6%(28/169) were from pulmonology with pneumonia as the most common diagnosis. The age range of cases was from 1 month to 16 years old. PICCs inserted during the study had catheter diameters ranging from 1.9Fr to 4.0Fr. Regarding the age range of patients, PICC insertion in such a pediatric sub-specialty seems more challenging than that in neonatal intensive care units, where age and body weight were more uniform.
Our study demonstrated the feasibility of PICC insertion in pediatric sub-specialties apart from intensive care units which are consistent with previously published articles. For example, Piper et al. reported that, for infants with intestinal failure, PICCs offer an advantage over central venous catheters with a low rate of catheter-related bloodstream infection and venous thrombosis. The study recommended PICCs for infants with intestinal failure requiring parenteral nutrition [12]. And PICC usage was increasing annually in other pediatric centers [13]. In China, PICC use in pediatric sub-specialties other than oncology and intensive care units is underdeveloped. Since interventional pediatric radiologists inserting PICCs under fluoroscopic guidance, which is common in developed countries, is not widely available yet in China. The nurse-inserted PICC program reported in this study is a feasible alternative model meriting introduction to other pediatric subspecialties.
In our study, we reported a low PICC-related complication rate of 16.4 per 1000 catheter days. The result is similar to other reports. In a review, Westergaard et al. reported the overall rates of complications in pediatric populations ranging from 1.11 to 19.3 per 1000 catheter days [14]. Of all complications in our cases, only 19.1%(9/47) required removal or replacement of the PICC, the rate was much lower than one-third as reported in the previous publications [15]. Therefore, only a small proportion of complications in cases included in this study could be classified as severe.
We found that malposition was the leading complication in our cases, however, 93.8%(15/16) of malposition occurred just after insertion; only one occurred as a result of patient behavior (severe cough). And most of the primary malposition occurred in 1.9Fr cases, ultrasound not being used for guiding PICC procedure in such a low age group potentially delayed the detection of malposition. PICC occlusion was the second most common complication, all occurring in cases with 1.9Fr lumen PICCs. Daily flushing of the catheter with saline or a heparin solution(50-100 U/ml) is a potentially effective approach to preventing PICC occlusion [14]. Besides malposition and occlusion, we reported a much lower rate of catheter-related bloodstream infection(0.3 per 1000 catheter days) than those reported in previous studies (from 1.4 to 2.0 per 1000 catheter days) [16, 17]. Standard PICC insertion and dressing practice guided by institutional protocols and early removal of unnecessary catheters are essential in preventing PICC-related bloodstream infection. Furtherly, we ascertained that the risk factors for PICC complications were low age and small PICC lumina which is similar to other study [18]. As mentioned above, promoting bedside ultrasound usage and practicing daily flushing using normal saline or low concentration heparin warrant further investigation in preventing small lumen catheter-related complications in young children.
Of 16 malposition, 9 were corrected by arm movement. Correct PICC tip position by arm manipulation has been reported previously. Nadroo et al. reported that arm movements significantly affect the position of the tip of the PICCs in neonatal cases. For catheters that were placed in the basilic vein, simultaneous shoulder adduction and elbow flexion caused the greatest movement toward the heart(15.11 ± 1.22 mm)9. Another adult study reported that there was a large amplitude of PICC tip position change with the depth of inspiration and arm position [19]. Since arm movement significantly alters PICC tip position, there were studies using arm movement for correcting malposition. Nadroo et al. described the maneuver for correcting PICC malposition and approved the effectiveness [9]. The maneuver was used in this study. Besides arm movement, a high-flow flush technique was another approach to malposition correction studied in previously published studies with a success rate of approximately 70% [20]. Of note, arm movement and high-flow flush are only alternative approaches for PICC malposition correction while radiologic intervention is the first or only choice in certain complicated cases [21].
Our study comprehensively reported the experience of PICC practice in infants and children outside intensive care units from a single tertiary pediatric center. All clinical data were collected prospectively, therefore, the data accuracy was high. Risk factor analyses for complications and malposition correction techniques provided a valuable reference for counterparts. Our study has limitations as well. Firstly, in analyzing risk factors for complications, some risk factors reported in previous studies [22, 23], such as dual lumen catheters, non-central position of the catheter tip, were not identified due to small sample size (only 2 non-central cases) and only single lumina catheters used in our practice. Secondly, Rastogi et al. reported that a mal-positioned PICC potentially could be corrected spontaneously [24]. Arm movement was approved effective in malposition correction in our descriptive study, however, without non-intervention control, the necessity of proactive correction by arm movement warrants further comparison studies.
Even though the complication rate in overall cases was not remarkably high, there is still large room for improvement. The following approaches could be carefully reviewed in future cases: ultrasound for guiding PICC insertion [25, 26], routine daily heparin flushing in 1.9Fr cases [27], novel approaches for guiding PICC insertion, such as intracavitary electrocardiogram etc. [28].
Conclusions
The nurse-inserted PICC program in general pediatrics is feasible with low complication rate. PICC tip malposition and occlusion were two major PICC-related complications with low age and small catheter lumina as risk factors. Arm movement potentially is an easy approach for correcting malpositioned PICC catheters.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, Jianguo Zhou.
Abbreviations
- PICC:
-
Peripherally inserted central catheter
References
Practical guide for safe central venous catheterization and management 2017. J Anesth. 2019;34(2):167–86. https://doi.org/10.1007/s00540-019-02702-9.
Pitiriga V, Bakalis J, Theodoridou K, et al. Lower risk of bloodstream infections for peripherally inserted central catheters compared to central venous catheters in critically ill patients. Antimicrob Resist Infect Control. 2022;11(1):137.
Vachharajani AJ, Vachharajani NA, Morris H, et al. Reducing peripherally inserted central catheters in the neonatal intensive care unit. J Perinatol. 2017;37(4):409–13.
Mori N, Nishihara Y, Tayama H, Higuchi A, Aoki Y. Peripherally inserted central catheter-related bloodstream infection caused by Kocuria marina in an elderly man. Infection. 2017;45(5):683–6.
Hou A, Fu J. Pericardial effusion/cardiac tamponade induced by peripherally inserted central catheters in very low birth weight infants: a case report and literature review. Front Pediatr. 2020;8:235.
Russell B, Klein Y, Rimon U, Kirshenboim Z, Horesh N, Zager Y. Acute cardiac tamponade due to peripherally inserted central catheter vascular perforation. Isr Med Assoc J. 2021;23(12):821–3.
Valente-Aguiar MS, de Carvalho ER, Magalhães T, Dinis-Oliveira RJ. Fatal iatrogenic cardiac tamponade due to central venous catheterization. Forensic Sci Med Pathol. 2022;18(3):275–9.
Barreiros LL, Andrade FM, Torres RA, Magalhaes LVB, Farnetano BDS, Fiorelli RKA. Cardiac tamponade by peripherally inserted central catheter in preterm infants: role of bedside ultrasonography and therapeutic approach. Rev Col Bras Cir. 2018;45(3):e1818.
Nadroo AM, Glass RB, Lin J, Green RS, Holzman IR. Changes in upper extremity position cause migration of peripherally inserted central catheters in neonates. Pediatrics. 2002;110(1 Pt 1):131–6.
Pettit J. Assessment of infants with peripherally inserted central catheters: part 1. Detecting the most frequently occurring complications. Adv Neonatal Care. 2002;2(6):304–15.
Yu Z, Gu Y, Zhang Y, Huang Y, Shen G, Hu X. The feasibility of peripherally inserted central catheters use for intermediate⁃ to long⁃term infusion at a tertiary pediatric hospital: sixty cases report. Chin J Evid Based Padiatr. 2017;12(2):100–5.
Piper HG, de Silva NT, Amaral JG, Avitzur Y, Wales PW. Peripherally inserted central catheters for long-term parenteral nutrition in infants with intestinal failure. J Pediatr Gastroenterol Nutr. 2013;56(5):578–81.
Gibson C, Connolly BL, Moineddin R, Mahant S, Filipescu D, Amaral JG. Peripherally inserted central catheters: use at a tertiary care pediatric center. J Vasc Interv Radiol. 2013;24(9):1323–31.
Westergaard B, Classen V, Walther-Larsen S. Peripherally inserted central catheters in infants and children - indications, techniques, complications and clinical recommendations. Acta Anaesthesiol Scand. 2013;57(3):278–87.
Barrier A, Williams DJ, Connelly M, Creech CB. Frequency of peripherally inserted central catheter complications in children. Pediatr Infect Dis J. 2012;31(5):519–21.
Thiagarajan RR, Ramamoorthy C, Gettmann T, Bratton SL. Survey of the use of peripherally inserted central venous catheters in children. Pediatrics. 1997;99(2):E4.
Levy I, Bendet M, Samra Z, Shalit I, Katz J. Infectious complications of peripherally inserted central venous catheters in children. Pediatr Infect Dis J. 2010;29(5):426–9.
Flores Moreno M, Pueblas Bedoy KS, Ojeda Sanchez A, Zurita-Cruz J. Risk factors associated with complications that required the removal of peripherally inserted central venous catheters in a tertiary pediatric hospital. Bol Med Hosp Infant Mex. 2017;74(4):289–94.
De Carvalho BR, Eagar GM. Immediate post-insertion tip migration of peripherally inserted central catheters dependent on arm position and depth of inspiration. J Med Imaging Radiat Oncol. 2018;62(3):324–9.
Spencer TR. Repositioning of central venous access devices using a high-flow flush technique - a clinical practice and cost review. J Vasc Access. 2017;18(5):419–25.
Gebauer B, Teichgraber UK, Podrabsky P, Werk M, Hanninen EL, Felix R. Radiological interventions for correction of central venous port catheter migrations. Cardiovasc Intervent Radiol. 2007;30(4):668–74.
Isemann B, Sorrels R, Akinbi H. Effect of heparin and other factors associated with complications of peripherally inserted central venous catheters in neonates. J Perinatol. 2012;32(11):856–60.
Costa P, Kimura AF, Brandon DH, Paiva ED, de Camargo PP. The development of a risk score for unplanned removal of peripherally inserted central catheter in newborns. Rev Lat Am Enfermagem 2015;23(3):475–482.
Rastogi S, Bhutada A, Sahni R, Berdon WE, Wung JT. Spontaneous correction of the malpositioned percutaneous central venous line in infants. Pediatr Radiol. 1998;28(9):694–6.
Li S, Lu H. Functions of heparin sodium injection in the prevention of peripherally inserted central catheter-related venous thrombosis in NSCLC patients during postoperative chemotherapy. Comput Math Methods Med. 2022;2022:1239058.
Cho Y, Lee S, Park SJ, Lee HN, Chung HH. Validation of the PICC length prediction formula based on anteroposterior chest radiographs for bedside ultrasound-guided placement. PLoS One. 2022;17(11):e0277526.
Bradford NK, Edwards RM, Chan RJ. Normal saline (0.9% sodium chloride) versus heparin intermittent flushing for the prevention of occlusion in long-term central venous catheters in infants and children. Cochrane Database Syst Rev. 2020;4(4):Cd010996. https://doi.org/10.1002/14651858.CD010996.
Ling Q, Chen H, Tang M, Qu Y, Tang B. Accuracy and safety study of Intracavitary electrocardiographic guidance for peripherally inserted central catheter placement in neonates. J Perinat Neonatal Nurs. 2019;33(1):89–95.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
ZY and JZ conceived the original idea and designed the study. XX and LL collected the data. ZY and XH interpreted the results. ZY and JZ drafted the paper. YG revised it critically. All authors approved the final.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The research proposal was approved by Ethics Committee of Clinical Research, Children’s Hospital of Fudan University, Shanghai. Informed consent was assured from guardians of children for participation in this research. All study methods were implemented in line with the involved guidelines of the Helsinki Declaration.
Consent for publication
Not Applicable.
Competing interests
The authors declare that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yu, Z., Hu, X., Xu, X. et al. A nurse-inserted peripherally inserted central catheter program in general pediatrics: a single-center experience. BMC Pediatr 23, 21 (2023). https://doi.org/10.1186/s12887-022-03809-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03809-x