Abstract
Background
The mosquito-borne arboviral disease dengue has become a global public health concern. However, very few studies have reported atypical clinical features of dengue among children. Because an understanding of various spectrums of presentation of dengue is necessary for timely diagnosis and management, we aimed to document the typical and atypical clinical features along with predictors of severity among children with dengue during the largest outbreak in Bangladesh in 2019.
Methods
We conducted a cross-sectional study between August 15 and September 30, 2019. in eight tertiary level hospitals in Dhaka city. Children (aged < 15 years) with serologically confirmed dengue were conveniently selected for data collection through a structured questionnaire. Descriptive, inferential statistics, and multivariable logistic regression were used to analyze data.
Results
Among the 190 children (mean age 8.8 years, and male-female ratio 1.22:1) included in the analysis, respectively 71.1 and 28.9% children had non-severe and severe dengue. All children had fever with an average temperature of 103.3 ± 1.2 F (SD). Gastrointestinal symptoms were the most common associated feature, including mostly vomiting (80.4%), decreased appetite (79.5%), constipation (72.7%), and abdominal pain (64.9%). Mouth sore, a less reported feature besides constipation, was present in 28.3% of children. Atypical clinical features were mostly neurological, with confusion (21.3%) being the predominant symptom. Frequent laboratory abnormalities were thrombocytopenia (87.2%), leucopenia (40.4%), and increased hematocrit (13.4%). Age (AOR 0.86, 95%CI 0.75–0.98, p = 0.023), mouth sore (AOR 2.69, 95%CI 1.06–6.96, p = 0.038) and a decreased platelet count (< 50,000/mm3) with increased hematocrit (> 20%) (AOR 4.94, 95%CI 1.48–17.31, p = 0.01) were significant predictors of severity.
Conclusions
Dengue in children was characterized by a high severity, predominance of gastrointestinal symptoms, and atypical neurological presentations. Younger age, mouth sores, and a decreased platelet with increased hematocrit were significant predictors of severity. Our findings would contribute to the clinical management of dengue in children.
Similar content being viewed by others
Background
Dengue has become a global public health concern, especially in most tropical and subtropical countries. It is a mosquito-borne (Aedes aegypti and Aedes albopictus) arboviral disease caused by the dengue virus (DENV) [1]. Over the last 60 years, the dengue virus has spread to over 130 countries, causing nearly 10,000 deaths and 100 million symptomatic cases every year [2, 3]. Besides, more than 50% of the global population are at risk of dengue transmission, with the vast majority in Asia, followed by Africa and America [4]. It is one of the leading causes of death among children in Southeast Asia [2].
In Bangladesh, the first recognized dengue outbreak was reported in the capital city, Dhaka in 1964 [5]. Subsequently, sporadic dengue cases were reported [6] until 2000, when the first major epidemic occurred throughout the major cities and towns of Bangladesh [7]. In 2019 the most extensive and deadliest outbreak of dengue occurred in the history of Bangladesh. Over 100,000 people were hospitalized, and 129 deaths were recorded [8]. The unofficial number of cases and deaths might be higher as the health reporting system is poor in the country. The high mortality was suspected to be associated with a high incidence of dengue shock syndrome (DSS) and secondary dengue infections [9].
DENV has four different serotypes (DENV-1 to 4). A peculiarity of DENV infection is that infection by one serotype produces serotype-specific lifelong immunity; however, contrary to giving protection or remaining neutral against other serotypes, a secondary infection by a heterogeneous serotype often results in severe disease by a mechanism called antibody dependent enhancement (ADE) [10]. All four serotypes have been isolated in Bangladesh with a predominance of DENV-3 till 2002 [11, 12]. After 2002, DENV-1 and DENV-2 were the prevalent serotypes, which increased the susceptibility of severe secondary infection by other serotypes [13]. In 2017, the DENV-3 serotype reemerged, causing a sharp rise of dengue cases in 2018 [14]. Thereafter, the 2019 outbreak was predominantly caused by type I genotype of the DENV-3 serotype [15].
Among children, nearly 95% of dengue cases are aged less than 15 years [16]. Owing to their immature hemodynamic system, children and particularly infants, tend to develop severe dengue disease [17, 18]. National surveillance data from Asian countries show that infants under 1 year of age and children aged 4–9 have consistently been at the highest risk for severe dengue disease [18].
Being a systemic disease, the clinical features of dengue show wide-ranging variations. Many of the clinical features were explored, but some (like constipation, mouth sores) are seldom reported. Moreover, children with dengue show significant variations in symptoms and signs in comparison to adults. Pain symptoms of dengue infection are less common among children [19,20,21]. Severe infection, when present, maybe preceded by so-called ‘warning’ signs [22]. Many clinical and laboratory factors have been attributed to the severity of the disease [23]. Early detection and appropriate management of severe dengue can reduce dengue-associated mortality [24]. Hence characterization of typical and atypical clinical features and determinants of severity, especially in the context of an outbreak, is essential. Previous studies have described the clinical presentations of dengue in the pediatric population of Bangladesh [25,26,27,28] from single centers and with a small number of samples. Globally, detailed profiling of clinical features, including usual and unusual clinical presentations of dengue in the pediatric population, is lacking. We hypothesized that the ongoing outbreak was characterized by increased severity and atypical clinical features suggestive of multi-system involvement among children with dengue. This study aimed to investigate that hypothesis, describe the typical and atypical clinical features, and model the clinical predictors of the severity of dengue among children in the setting of Bangladesh.
Methodology
Case definition
In Bangladesh, the National Guideline for Clinical Management of Dengue was published in collaboration with the World Health Organization (WHO) in 2018 for efficient management of dengue cases in the context of the country [29]. Based on this guideline, symptomatic dengue cases were initially classified into three major categories based on their severity: dengue fever (group A), and dengue fever with warning signs (group B), and severe dengue (group C). Here the former two (group A and B) are non-severe groups. A detailed description of the defining features is listed in Table S1 (Additional file 1). We also used the classical WHO categories of dengue, namely, dengue fever (DF), dengue hemorrhagic fever (DHF), dengue shock syndrome (DSS), and expanded dengue syndrome (EDS) for comparison purposes. EDS is an entity that was initially absent in the dengue management guideline published by WHO in 2009 [22] but was later incorporated in the revised and expanded edition of the guideline in 2011 [30]. This term was coined by WHO to describe cases that do not squarely fall within the definition of DHF and DSS and is characterized by atypical findings of dengue [31].
Participants, study design, and data collection
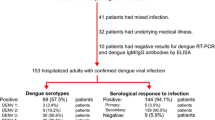
This cross-sectional study was conducted during the peak of the 2019 dengue outbreak from August 15 to September 30, 2019. The study included hospitalized children with laboratory-confirmed dengue and was carried out in accordance with the Declaration of Helsinki. Children were defined as patients with age 14 years or less. Diagnosis was confirmed serologically by positive for the dengue nonstructural glycoprotein 1 (NS1) and/or dengue IgM antibodies. A total of 278 hospitalized children with dengue symptoms were enrolled; of which 237 children were serologically confirmed. After exclusion of incomplete data (19.8%), 190 cases of children with dengue were analyzed. Patients were recruited from five government hospitals and three private hospitals in the capital city of Bangladesh. The data collection centers with the number of pediatric patient data initially collected from each center (given in parenthesis) are as follows. Dhaka Medical College Hospital (n = 95), Kurmitola General Hospital (n = 49), Mugda Medical College Hospital (n = 37), Sir Salimullah Medical College Hospital (n = 1), Suhrawardy Medical College Hospital (n = 11), Popular Medical College Hospital (n = 17), Dr. Sirajul Islam Medical College Hospital (n = 16), and MH Samaarita Medical College Hospital (n = 10) (Figure S1) (Additional file 1). The initiative was taken by the Biomedical Research Foundation, Bangladesh. A team of 85 volunteer researchers composed of undergraduate and graduate medical students, clinicians, public health professionals, and statisticians got involved in this study.
Data was collected using a structured questionnaire via face-to-face interview by the trained volunteer medical students and medical doctors during the convalescent phase of the disease. The questionnaire was developed based on previously published literature and discussion with a multidisciplinary team, including clinicians. The questionnaire was pretested in a sample of 20 patients and any inter-observer variation was resolved through discussion among the team members. Presenting symptoms were grouped according to the system involved. We also incorporated a list of unusual symptoms in the questionnaire, based on the atypical manifestations of dengue [29, 32], to draw a picture of atypical presentations during the outbreak (see Additional file 2).
Enumerators were given one-day training on the use of the questionnaire. Guardians/parents of the respondents were asked about the demographic profile and clinical presentation during their first week of presentation where necessary. The investigation profile was collected from their hospital records. For hematological investigations, only the highest or lowest value of a test was collected when more than one record was found.
Statistical analysis
Descriptive and inferential statistical procedures were used to illustrate the clinical profile of DENV infection and to ascertain the factors associated with severe infection. Descriptive statistics were reported as percentage and means when applicable along with standard deviation. Missing cases were excluded from bivariate analysis and data were expressed among the available responses for different variables. Completed data collection forms were scrutinized by data collection supervisors. Verified data were entered and subsequently managed using REDCap electronic data capture tool hosted at BRF server [33]. Data were analyzed using R statistical software. For testing association between categorical data, Pearson’s chi-square test was used, and Yate’s correction for continuity was applied where appropriate. We performed an independent sample t-test when comparing the means of continuous variables. Logistic regression analysis was used to see associations. A two-tailed p-value smaller than 0.05 was considered statistically significant.
Ethical consideration
The study was approved by the Ethical Review Committee (ERC) of Biomedical Research Foundation (Memo no:BRF/ERB/2019/017). Written approval was taken from the authority of the selected hospitals before data collection. As approved by ERC, verbal and/or written informed consent was obtained from guardians of each participant as per their convenience. Trained enumerators first approached and explained consent forms to the prospective participants, and the study questionnaire was shared or discussed with them. After obtaining consent (oral and/or written) from the guardians or parents of the participants, they were registered for face-to-face interview and hospital document review. Some of them could not sign their names, in which case the questionnaire was marked indicating a case with verbal consent.
Result
Characteristics of the children
Out of 190 pediatric dengue patients, 179 (94.2%) cases were positive for NS1 antigen, and 11 (5.8%) cases for IgM antibody. Overall, children with dengue had an average age of 8.8 ± 3.7 years with a slight male predominance (1.22:1). However, severe cases showed slightly male predominance. The majority (46.1%) of the children belonged to the age group of 10–14 years. According to severity, about 20% fell under group A, 51% group B, and 29% group C. Therefore, more than two-third (71.1%) of the children were non-severe. According to the WHO dengue classification by symptoms, over two-thirds (63.7%) of children presented with DF while 10, 23.2, and 3.2% had DHF, DSS, and EDS, respectively. Past history of dengue and chikungunya were present only in 1.3 and 7.4% of children respectively. The mean age of severe (7.4 years) dengue cases was significantly lower than that of non-severe (9.4 years) dengue cases (p < 0.001). Other socio-demographic parameters were comparable between severe and non-severe groups (Table 1).
Clinical manifestations of the children
Symptoms
Table 2 enlists the frequently occurring general, systematic and unusual clinical presentation of children in relation to severity. Additional less frequent freatures are described in Table S2 (Additional file 1). All of the children presented with fever. The average maximum recorded temperature was 103.3 F (SD ± 1.2). The average duration of fever was 5.4 days (SD ± 2.8). However, it was significantly higher in patients with severe disease than non-severe (6.2 ± 4.1 vs. 5.1 ± 2.0 days, p0.043). Other common presenting symptoms were mostly gastrointestinal, including vomiting (80.4%), lethargy (78.3%) decreased appetite (79.5%), constipation (72.7%), and abdominal pain (64.9%). Itching (33.2%), mouth sore (28.3%), and skin rash (27.7%) were common muco-cutaneous manifestations. Arthralgia was present in 40.8% of patients. About 24% of children experienced hemorrhagic manifestations. Epistaxis (6.3%) and malena (5.8%) were the most frequent bleeding manifestations, followed by subconjunctival hemorrhage (4.2%) and gum bleeding (3.7%). Most of the symptoms were similar between patients with non-severe and severe disease. Mouth sores and malena were significantly associated with severe disease. Interestingly, hair loss was present in 9 (6.9%) patients with the non-severe disease, while no patients with severe disease experienced it.
Atypical symptoms
Several atypical manifestations were noted among patients with most frequent being confusion (21.4%), and blurring of vision (14.9%) (Table 2). Additionally, palpitation (11.9%), chest tightness (9.8%), sensory impairment (9.7%), convulsion (7.0%), disorientation (5.9%), neck stiffness (5.9%), palpable lymph nodes (3.1%), auditory hallucination (2.7%), transient amnesia (1.6%), altered mental state (1.6%) and facial deviation (0.5%) occurred infrequently among participants (Table S2). All the atypical manifestations were comparable between non-severe and severe groups except convulsion and palpitation, which were significantly higher among patients with severe disease.
Signs
Among features of plasma leakage and shock, cold-clammy skin (47.5%) and excessive sweating (40.8%) were most prominent. Moreover, 15.8% of children had obvious manifestations of clinical fluid accumulation (Table 2). Ascites, pleural effusion, and anasarca were present in 6.8, 5.8 and 2.6% patients respectively. While anemia and dehydration were found in 15.1 and 11.9% of children, respectively. Only three children had hepatomegaly (1.8%) (Table S2).
Laboratory investigations
Thrombocytopenia (< 150,000/mm3) was present in most children (87.2%), leucopenia (< 4000/mm3)in 40.4% and increased hematocrit (> 20% from baseline) in 13.4% of children (Table 3).
Variations in clinical presentations by gender and age
Variation in clinical presentation was noted across gender (Table S3) (Additional file 1). Retro-orbital pain, backache, itching, hair loss, arthralgia, and leucopenia were significantly more common among girls than boys. Auditory hallucination was found only among boys (n = 5, p = 0.038). Other features showed statistically similar distribution.
Age-related variations among some clinical features were also documented (Table S4) (Additional file 1). Headache and loose motion were significantly more common among older groups (10–14 years) of children than other groups. Backache was significantly higher in the older (10–14) group compared to younger ones. Rash, decreased appetite, and constipation was significantly higher in the youngest group (< 5 years). Mouth sores were significantly more frequent in children < 10 years. Vomiting, hemorrhage and cold clammy skin was present in significantly higher proportion in the middle group (5–9 years) than other groups. Proportion of cases with severe dengue and dengue with warning signs were higher in respectively < 5 years and 5–9 years in comparison to the rest of the children.
Determinants of severity among children
Factors which differed among children in relation to age, sex and severity were included in a predictive model to determine their predictive values for severe dengue among children (Table 4). These included child’s age, sex, certain clinical features (backache, retroorbital pain, oral ulcer, rash, arthralgia, vomiting, abdominal pain, loose motion, and constipation) and investigation (decreased platelet < 150,000/mm3 with increased hematocrit > 20% and leucopenia). Severity defining features like hemorrhage and signs of plasma leakage and shock were excluded from the model to avoid incorporation bias. Several atypical features were excluded due to their low count. Abdominal pain was kept in the model despite showing non-significant variation across groups as severe abdominal pain is a warning sign. In the final model age, oral ulcer and decreased platelet with increased hematocrit count was found to be a significant predictor of severity among children. One-year increase in age was associated with 14% reduction in risk of severity (OR 0.86, 95%CI 0.75–0.98, p = 0.023). Presence of mouth sores was associated with significantly higher odds of developing severe disease (OR 2.69, 95% CI 1.06–6.96, p = 0.038). A decreased platelet count with increased hematocrit was associated with 4.94 times higher odds (95%CI 1.48–17.31, p = 0.01) of developing severe dengue.
Discussion
This was a large multicenter cross-sectional study of dengue among children, which reports the atypical and less reported clinical presentations, and models severity predictors of dengue in Bangladesh. ‘Mouth sore’ and ‘constipation’, two previously less reported gastrointestinal features, were prevalent among our participants. Atypical features were found mainly in the form of neurological manifestations, with confusion and blurring of vision being predominant. Age, mouth sore (in the form of sore throat and/or mouth ulcers), and decreased platelet with increased hematocrit were clinical predictors of severity.
Nearly one-third of cases had severe dengue in our study, which is higher than that (one-fifth of cases) found in 2018 by both Shultana et al. [27] and Afroze et al. [28] in two separate tertiary care hospitals (sample size, n = 89 and 106 respectively) in Dhaka city. Proportionately dengue shock syndrome cases were higher than any prior outbreaks recorded in the country [25, 27, 28]. This finding supports our hypothesis that the outbreak of 2019 was relatively more intense than the previous ones in terms of clinical severity. Besides, we found six cases of expanded dengue syndrome among whom at least two had features suggestive of encephalitis- a rare manifestation of dengue infection [34]. However, only 1.6% of children had a past history of dengue indicating that the severe cases cannot be explained by the secondary infection by a different serotype alone. The re-emergence of DEN-3 serotype in 2019 [15] combined with the fact that severe primary infection may occur in children [18] might explain the higher severity noted in this study. Moreover, several studies conducted within the last 5 years in India [35], Indonesia [36], and Mexico [37] found respectively 35, 20, and 58% severe dengue cases among their participants, supporting our hypothesis that dengue among children is occurring with increased severity.
Compared to the 2018 outbreak, children infected with dengue were older in the 2019 outbreak in the country [27, 28]. However, our age pattern matches the 2000 outbreak [25, 38], indicating a temporal variation in the age of involvement among children in this region. Additionally, we found that younger age is significantly associated with severe disease in multivariate analysis. This finding is also supported by surveillance studies from Asian countries [18].
A higher proportion of males among dengue-infected children of this study has been persistently noted in Bangladesh [27, 28] and several South-East Asian countries [32,33,34,35]. Anker and Arima [39] explored the sex-related differences in the prevalence of dengue in more detail. They noted that the magnitude of the difference is small and is not consistent in pediatric patients. However, male-female differences in the use of health services, the use of fully covered dresses by female children, and prioritizing provisions of male children in the society might be reasons for the differences noted in our country [40, 41].
Approximately three-fourths of `the families in this study came from the lower economic categories, with 33.7% having income less than 15,000 BDT per month (equivalent to USD 17.7). One explanation for this could be people with a lower monthly income are more likely to live in crowded places having a higher risk of contracting the disease from an infected person. Another possible reason is that public health facilities, from where our data was collected, are mostly visited by poor patients in the country [42].
The most frequent blood group among dengue infected children in our study was ‘O’ positive in contrast to the most common ABO and Rh blood type (‘B’ positive) noted among healthy donors of the country [43, 44]. Reports on the association between blood groups with dengue fever have been mixed. Khode et al. [45] found an association of ‘O’ positive blood groups with higher prevalence of dengue. But, in the study by Ravichandran et al. [46] it was ‘AB’ positive. Contrary to Kalayanarooj et al. [47] we did not find any association of severity of dengue with any particular blood ABO and Rh blood type. Therefore, the high prevalence of ‘O’ positive blood in our study could be a random finding.
Children with dengue show varying clinical presentations throughout the world. But fever is the most common symptom in dengue irrespective of types and severity. Variation exists in other symptoms and signs associated with fever. Likewise, we found a high-rise fever in all cases. Gastrointestinal features were more frequent in our study than that of previous year [48, 49]. Constipation, a seldom sought for feature in studies involving dengue [48, 49], was found to be more frequent than diarrhea in our patients. This might be consequent of decreased appetite and vomiting found in higher proportion in our study. However, the proportion of cases presenting with diarrhea was not less than other recent studies either [50, 51].
One unique finding of this study was independent association of sore mouth (including oral ulcers and/sore throat) with severe disease. Although, it was not found to be a factor for severity by Zhang and colleagues in their systematic review and meta-analysis of predictive symptoms and signs of severe dengue [52]. Sore mouth is a less common feature of dengue compared to other febrile illness which is usually reported as sore throat [51], therefore presence of it especially among younger children with dengue should raise concern regarding severity.
The most common bleeding manifestations was epistaxis and melena similar to several previous studies [53, 54]. A significantly higher proportion of melena was noted in severe dengue than the non-severe one consistent with previous evidence [25, 52].
The unusual features presented by children with dengue were mostly suggestive of nervous system involvement except palpitation and chest tightness which might have occurred due to hypovolemic shock associated cardiac ischemia [55] or due to transient involvement of cardiac muscles [32]. The neurological symptoms were suggestive of encephalopathy due to hypovolemic shock, and/or encephalitis and meningitis due to direct involvement of nervous tissue by the virus [56].
As older children could report their symptoms properly a higher proportion of pain related symptoms was noted among them. Interestingly female children also reported a higher frequency of different aches probably as a result of a lower threshold of pain sensitivity evident in women [57]. The high prevalence of mouth sores, rash, decreased appetite, and constipation among the youngest children might be explained by combinations of a developing immune system, decreased leucocyte counts, and a severe disease in this group.
We used conservative cut-off values for blood counts so that even slight elevation and reduction in specific investigations are not missed. Therefore, elevations in hematocrit value, and reductions in hemoglobin, leucocyte count, platelet count, were statistically similar between non-severe and severe dengue. But an elevation of hematocrit (> 20% from baseline) combined with a reduction in platelet count (< 50,000/mm3) was found to be a significant predictor of severe disease on multivariate analysis. Also, this was the only warning sign among others included in the multivariate logistic regression that came out as a significant predictor of dengue severity. Contrary to the estimates of Zhang et al. [52] our study did not find abdominal pain, vomiting and rash to be significant predictors of severity.
There were several limitations of our study. First, we had a small final sample size due to limited data collection and curation of incomplete data. Our data collection was limited in that we could not include the specialized centers dedicated for mother and child health in the city as because the data on pediatric dengue cases were collected in conjunction with adult cases from the multidisciplinary tertiary care hospitals. Second, we used a non-random convenience sampling, due to the rapidly evolving nature of the outbreak, to collect as many responses as possible near the end of peak time. This should be taken into consideration while interpreting our result. Third, the clinical classification of dengue was used for stratification of severity which might cause misclassification bias due to the subjective nature of the assessment. However, the initial classification of a patient during admission was subsequently verified by experts before discharge reducing the bias. Fourth, our design was cross-sectional in nature making the relations found between predictors and severity general associations.
Conclusion
In 2019 outbreak, dengue among children was characterized by increased severity among preschoolers with a male predominance. Gastrointestinal symptoms were the most common presentation alongside fever. Epistaxis and melena were the main bleeding manifestations. Atypical manifestations were mostly suggestive of neurologic involvement. Decreasing age, presence of mouth sores and a decreased platelet with increased hematocrit were significant predictors of severity. Our findings would contribute to the clinical management and enrich knowledge in dengue research arena. Further randomized case-control and prospective studies with large samples are recommended to characterize particularities of pediatric dengue along with its classification, and complications..
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Simmons CP, Farrar JJ, van VC N, Wills B. Dengue. N Engl J Med. 2012;366(15):1423–32.
Stanaway JD, Shepard DS, Undurraga EA, Halasa YA, Coffeng LE, Brady OJ, et al. The global burden of dengue: an analysis from the global burden of disease study 2013. Lancet Infect Dis. 2016;16(6):712–23.
Bhatt S, Gething PW, Brady OJ, Messina JP, Farlow AW, Moyes CL, et al. The global distribution and burden of dengue. Nature. 2013;496(7446):504–7.
Messina JP, Brady OJ, Golding N, Kraemer MUG, Wint GRW, Ray SE, et al. The current and future global distribution and population at risk of dengue. Nat Microbiol. 2019;4(9):1508–15.
Ordoñez J, Russell PK, McCown JM, Buescher EL. Recovery of dengue viruses from patients during epidemics in Puerto Rico and East Pakistan. Am J Trop Med Hyg. 1966;15(4):573–9.
Karim MN, Munshi SU, Anwar N, Alam MS. Climatic factors influencing dengue cases in Dhaka city: a model for dengue prediction. Indian J Med Res. 2012;136(1):32–9.
Bin YE, Bangali AM, Mahmood MAH, Rahman MM, Chowdhury AR, Talukder KR. Dengue outbreak 2000 in Bangladesh: from speculation to reality and exercises. Dengue Bull. 2001;25:15–20.
Institute of Epidemiology Disease Control and Research. Dengue Situation Update [Internet]. 2011 [cited 2020 Jan 10]. Available from: https://www.iedcr.gov.bd/images/files/dengue/Dengue_status_02.12.2019.pdf.
Akram A. Alarming turn of dengue fever in Dhaka City in 2019. Bangladesh J Infect Dis. 2019;6(1):1–2.
Guzmán MG, Kourí G. Dengue: An update. Lancet Infect Dis. 2002;2(1):33–42.
Pervin M, Tabassum S, Sil BK, Islam MN. Isolation and serotyping of dengue viruses by mosquito inoculation and cell culture technique: an experience in Bangladesh. Dengue Bull. 2003;27:81–90.
Islam MA, Ahmed MU, Begum N, Chowdhury NA, Khan AH, Parquet C, et al. Molecular characterization and Clinical evaluation of dengue outbreak in 2002 in Bangladesh. Japanese J Infect Dis. 2006;59:85–91.
Muraduzzaman AKM, Alam AN, Sultana S, Siddiqua M, Khan MH, Akram A, et al. Circulating dengue virus serotypes in Bangladesh from 2013 to 2016. Virus Dis. 2018;29(3):303–7.
Ahmad FU, Paul SK, Aung MS, Mazid R, Alam M, Ahmed S, et al. Co-circulation of dengue virus type 3-genotype I and type 2-cosmopolitan genotype in 2018 outbreak in Dhaka, Bangladesh. New Microbes New Infect. 2020;33:100629 Available from: https://doi.org/10.1016/j.nmni.2019.100629.
Titir SR, Paul SK, Ahmed S, Haque N, Nasreen SA, Hossain KS, et al. Nationwide distribution of dengue virus type 3 (Denv-3) genotype I and emergence of denv-3 genotype III during the 2019 outbreak in Bangladesh. Trop Med Infect Dis. 2021;6(2):58.
Bhattacharya MK, Maitra S, Ganguly A, Bhattacharya A, Sinha A. Dengue: a growing menace -- a snapshot of recent facts, figures and remedies. Int J Biomed Sci. 2013;9(2):61–7.
Elling R, Henneke P, Hatz C, Hufnagel M. Dengue fever in children: where are we now? Pediatr Infect Dis J. 2013;32(9):1020–2.
Verhagen LM, de Groot R. Dengue in children. J Infect. 2014;69(S1):S77-86.
de Souza LJ, Bastos Pessanha L, Carvalho Mansur L. Assed de Souza L, Barbosa Tâmega Ribeiro M, do Vale da Silveira M, et al. comparison of clinical and laboratory characteristics between children and adults with dengue. Brazilian J Infect Dis. 2013;17(1):27–31.
Kittigul L, Pitakarnjanakul P, Sujirarat D, Siripanichgon K. The differences of clinical manifestations and laboratory findings in children and adults with dengue virus infection. J Clin Virol. 2007;39(2):76–81.
Wang CC, Lee IK, Su MC, Lin HI, Huang YC, Liu SF, et al. Differences in clinical and laboratory characteristics and disease severity between children and adults with dengue virus infection in Taiwan, 2002. Trans R Soc Trop Med Hyg. 2009;103(9):871–7.
World Health Organization. Dengue guidelines for diagnosis, treatment, prevention and control: new edition. Geneva PP - Geneva: World Health Organization; 2009. Available from: https://apps.who.int/iris/handle/10665/44188.
Wakimoto MD, Camacho LAB, Guaraldo L, Damasceno LS, Brasil P. Dengue in children: a systematic review of clinical and laboratory factors associated with severity. Expert Rev Anti-Infect Ther. 2015;13(12):1441–56.
World Health Organization. Global strategy for dengue prevention and control 2012-2020. Geneva PP - Geneva: World Health Organization; 2012. Available from: https://apps.who.int/iris/handle/10665/75303.
Ahmed FU, Mahmood CB, Das SJ, Hoque SM, Zaman R, Hasan MS. Dengue and dengue haemorrhagic fever in children during the 2000 outbreak in Chittagong, Bangladesh. Dengue Bull. 2001;25(2):33–9.
Hoque S, Sarkar PK, Nawshad ASM, Ahmed U. Clinical profile and outcome of dengue in children admitted in pediatric intensive care unit in Dhaka shishu (children) hospital, Dhaka, Bangladesh. Int J Med Heal Res. 2019;5(12):97–101.
Shultana K, Motiur Rahman AZM, Al Baki A, Shohidul Islam Khan M, Deb B, Chowdhury D, et al. Dengue Infection in Children: Clinical Profile and Outcome in Dhaka City. Am J Pediatr. 2019;5(3):111.
Afroze S, Shakur S, Wahab A, Shakur S. Clinical profile of dengue and predictors of its severity among children. Am J Pediatr. 2019;5(4):219–23.
DGHS. National Guideline for Clinical Management of Dengue [Internet]. Dhaka; 2018. Available from: https://dghs.gov.bd/images/docs/Guideline/NationalGuidelineforDengue2018.pdf
World Health Organization, Regional Office for South-East Asia. Comprehensive Guideline for Prevention and Control of Dengue and Dengue Haemorrhagic Fever. Revised and expanded edition. New Delhi PP - New Delhi: WHO Regional Office for South-East Asia; 2011. Available from: https://apps.who.int/iris/handle/10665/204894.
Kadam DB, Salvi S, Chandanwale A. Expanded dengue. J Assoc Physicians India. 2016;64(July):59–63.
Gulati S, Maheshwari A. Atypical manifestations of dengue. Trop Med Int Heal. 2007;12(9):1087–95.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Varatharaj A. Encephalitis in the clinical spectrum of dengue infection. Neurol India. 2010;58(4):585–91.
Ramabhatta S, Palaniappan S, Hanumantharayappa N, Begum SV. The Clinical and serological profile of pediatric dengue. Indian J Pediatr. 2017;84(12):897–901.
Adam AS, Pasaribu S, Wijaya H, Pasaribu AP. Warning sign as a predictor of dengue infection severity in children. Med J Indones. 2018;27(2):101–7.
Alvarado-Castro VM, Ramírez-Hernández E, Paredes-Solís S, Legorreta-Soberanis J, Saldaña-Herrera VG, Salas-Franco LS, et al. Clinical profile of dengue and predictive severity variables among children at a secondary care hospital of Chilpancingo, Guerrero, Mexico: case series. Boletín Médico Del Hosp Infant México (English Ed). 2016;73(4):237–42.
Shah GS, Islam S, Das BK. Clinical and laboratory profile of dengue infection in children. Kathmandu Univ Med J (KUMJ). 2016;4(1):40–3.
Anker M, Arima Y. Male-female differences in the number of reported incident dengue fever cases in six Asian countries. West Pacific Surveill response J. 2011;2(2):17–23.
Masud S, Adams AM, Chowdhury M. Gender , socioeconomic development and health-seeking behaviour in Bangladesh. Soc Sci Med. 2000;51:361–71.
Mishra S, Ramanathan R, Agarwalla SK. Clinical Profile of Dengue Fever in Children: A Study from Southern Odisha, India. Scientifica (Cairo). 2016;2016:1–6.
Manna M. Access to Public Health Facilities in Bangladesh: A Study on Facility Utilisation and Burden of Treatment. Bangladesh Dev Stud. 2013;XXXVI(4):25–80.
Karim S, Hoque M, Hoque E, Begum H, Rahman S, Shah T, et al. The distribution of ABO and Rhesus blood groups among blood donor attending transfusion medicine department of Dhaka Medical College Hospital in 2014. J Dhaka Med Coll. 2015;24(1):53–6.
Dipta TF, Iqbal MR, Hossain AZ, Rahman MT, Chowdhury S. Distribution of phenotypic and genotypic ABO and Rhesus blood groups among Bangladeshi population. Ibrahim Med Coll J. 2011;5(2):59–62.
Khode V, Ruikar K, Kabbin G. Association of ABO Rh blood group with dengue fever and dengue hemorrhagic fever: a case-control study. J Appl Hematol. 2013;4(4):145.
Ravichandran S, Ramya SR, Kanungo R. Association of ABO blood groups with dengue fever and its complications in a tertiary care hospital. J Lab Physicians. 2019;11(03):265–9.
Kalayanarooj S, Gibbons RV, Vaughn D, Green S, Nisalak A, Jarman RG, et al. Blood group AB is associated with increased risk for severe dengue disease in secondary infections. J Infect Dis. 2007;195(7):1014–7.
Karunakaran A, Ilyas WM, Sheen SF, Jose NK, Nujum ZT. Risk factors of mortality among dengue patients admitted to a tertiary care setting in Kerala. India J Infect Public Health. 2014;7(2):114–20.
Al Awaidy ST, Al Obeidani I, Bawikar S, Al Mahrouqi S, Al Busaidy SS, Al Baqlani S, et al. Dengue epidemiological trend in Oman: a 13-year national surveillance and strategic proposition of imported cases. Trop Dr. 2014;44(4):190–5.
Yolanda N, Alfan H. Initial clinical and laboratory profiles to predict pediatric dengue infection severity. Paediatr Indones. 2017;57(6):303–9.
Chen C-H, Huang Y-C, Kuo K-C, Li C-C. Clinical features and dynamic ordinary laboratory tests differentiating dengue fever from other febrile illnesses in children. J Microbiol Immunol Infect. 2018;51(5):614–20.
Zhang H, Zhou YP, Peng HJ, Zhang XH, Zhou FY, Liu ZH, et al. Predictive symptoms and signs of severe dengue disease for patients with dengue fever: a meta-analysis. Biomed Res Int. 2014;2014:104.
Ahmed S, Arif F, Yahya Y, Rehman A, Abbas K, Ashraf S, et al. Dengue fever outbreak in Karachi 2006 - a study of profile and outcome of children under 15 years of age. J Pak Med Assoc. 2008;58(1):4–8.
Sahana KS, Sujatha R. Clinical profile of dengue among children according to revised WHO classification: analysis of a 2012 outbreak from southern India. Indian J Pediatr. 2015;82(2):109–13.
Taghavi S, Askari R. Hypovolemic Shock. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2020. [cited 2020 Oct 18]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513297/.
Li GH, Ning ZJ, Liu YM, Li XH. Neurological manifestations of dengue infection. Front Cell Infect Microbiol. 2017;7:449.
Hashmi JA, Davis KD. Deconstructing sex differences in pain sensitivity. Pain. 2014;155(1):10–3.
Acknowledgements
We would like to acknowledge to Mahbubul H Siddiqee and Mahbub Hasan of Biomedical Research Foundation, Dhaka Bangladesh; Professor Shakil Ahmend of Shaheed Suhrawardy Medical College & Hospital; Professor HAM Nazmul Ahsan of Popular Medical College and Hospital; Mohammad Jahid Hasan of Pi Research consultancy centre for their valuabe support. We also acknowledge to all data collectors, particularly Alina Firoze, Fayal Prince and Mohammad Shojon.
Funding
This project was partially funded by Techno Drug Ltd., Bangladesh.
Author information
Authors and Affiliations
Contributions
MSH conceived the study. MSH, AAM, ER, MASK for project contributed design and data analysis and manuscript writing. AA, RR, MH, FBA, NH, SY, RA, NA, SA, SA contributed in data collection and critical feedback during manuscript preparation. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and conset to participate
The study was approved by the Ethical Review Committee (ERC) of Biomedical Research Foundation (Memo no:BRF/ERB/2019/017). Written approval was taken from the authority of the selected hospitals before data collection. Verbal and/or written informed consent was obtained from guardians of each participant as per their convenience.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary figures and tables.
Additional file 2.
Questionnaire.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Khan, M.A.S., Al Mosabbir, A., Raheem, E. et al. Clinical spectrum and predictors of severity of dengue among children in 2019 outbreak: a multicenter hospital-based study in Bangladesh. BMC Pediatr 21, 478 (2021). https://doi.org/10.1186/s12887-021-02947-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-021-02947-y