Abstract
Background
Around two and half million neonatal mortality occurred in 2017, especially in developing countries. This study was conducted to determine the determinants of neonatal mortality among newborns admitted in the neonatal intensive care unit at Dilla University Referral Hospital in Gedeo Zone, Southern Ethiopia.
Methods
An unmatched case-control study was conducted from February, 24 to March 6, 2020 at Dilla University Referral Hospital in Gedeo Zone Southern Ethiopia. A total of 304 neonates (76 cases and 228 controls) were involved. Neonates registered as died were considered as cases and neonates registered as improved were considered as controls. Data were extracted by pretested checklists from medical records of neonates admitted during the last one year period. Data was entered into EpiData3.1, and analyzed by statistical package for social science software Version 22.Bivariate and multivariate logistic regressions were used to identify determinants associated with neonatal mortality. Finally, AORs at 95 % CI and P-values < 0.05 were used to declare statistical significance.
Results
In this study, a total of 304 cases were assessed with 100 % reviewed rate. It was found that referrals from other health facilities, [AORs = 2.43, 95 % CI (1.14, 5.22)], gestational age < 37 weeks,[AORs = 2.50, 95 % CI (1.12, 5.58)], the weight of newborn < 2500 g, [AORs = 2.44, 95 % CI (1.13, 5.28)], neonates positive for sepsis, [AORs = 2.45, 95 % CI (1.11, 5.41)]and neonates who not breastfed within first hour after delivery,[AORs = 5.24, 95 % CI (2.42, 11.37)] were statistically significant determinants to neonatal mortality.
Conclusions
This study suggests that referral, gestational age, weight of newborn, sepsis and breastfeeding were significant determinants to neonatal mortality. This study shows that neonatal intensive care unit service should be strengthened in Dilla University Referral Hospital; targeting neonate aged below 28 days. Most of these determinants may be prevented and minimized by strengthening referral linkage, improving intrapartum and postpartum care.
Similar content being viewed by others
Introduction
Neonatal mortality is defined as the death of live-born within the first 28 days of life. Neonatal mortality can be subdivided into very early, early and late neonatal mortality. The very early and early neonatal mortalities are the deaths occurring on the first day and within the first seven days of live-born. Whereas the deaths happening after the seventh days but before the 28 day of life considered as late neonatal mortality [1, 2]. Neonatal mortality rate (NMR) is the number of neonatal deaths per 1000 live births in a given year and is a key indicator of the health of population [1, 3, 4]. The main causes for neonatal mortality are related to congenital anomalies, preterm, small for gestational age, intrapartum injuries, infections, low birth weight, and challenges of adapting extra uterine environment [5].
At the global level, around two and half million neonatal mortality happened within four weeks of life in 2017. About 36 % of them died within the first day they were born, and 75 % of all neonatal mortality occurred in the first week of life. Almost all mortalities of neonates were registered in growing countries and it becomes the riskiest time for an under-five survival [6]. Two-thirds of all live-born death is contributed from 12 countries, six of them are in Sub-Saharan Africa countries and they accounted for about 60 % of all neonatal mortalities [6, 7].In Ethiopia, about 87,000 neonates die each year within 28 days of life after birth and therate of mortality is among the highest in the world [8]. The trend of mortalities also increased from 29 in Ethiopian Demographic Health Survey (EDHS2016) to 30 in Ethiopian Min Demographic Health Survey (EMDHS 2019) per 1000 live births respectively [9, 10].Globally,tremendous strides were done to reduce neonatal mortality over the past few decades by formulating favorable health policies, and appropriate resource allocation to hasten the achievements of the neonatal survival goals [11,12,13].By those trials, many countries had reduced neonatal mortality including Ethiopia [14].
Even though, those countries had reduced neonatal mortality, the progress of decline was not impressive in Ethiopia and the contribution of neonatal mortality to under-five death has also increased from 43.3 % to 2016 to 54.5 % in 2019 [9, 10, 15]. As a result, currently, Ethiopiais far from international standards for the prevention of neonatal mortality and it was expected to reduce neonatal mortality as low as 12 per 1000 live in SDG3.2 [16, 17].
However, there were limited institution-basedstudies in southern Ethiopia [18, 19], despite the severity of the problem. Even if, those studies identified some determinants there was inconsistencies in findings. Therefore, this study aimed to provide the representative information on determinants of neonatal mortality among neonates admitted in the neonatal intensive care unit at Dilla University Referral Hospital in Gedeo Zone, Southern Ethiopia.
Methods
Study area and period
The study was conducted at Dilla University Referral Hospital (DURH) in Southern Ethiopia, from February, 24 to March 6, 2020. The DURH found in Dilla, the town of Gedeo Zone. It is located due south 359 and 90 km far away from Addis Ababa, and Hawassa, respectively [20]. The Hospital was established in 1977 E.C as a District Hospital. The hospital belongs to the government and its administration was taken by Dilla University since 2005 E.C, hence got the name DURH [21]. Nowadays, the hospital is providing preventive, curative, and rehabilitative services around for 2 million catchment population in different wards [22]. Among those, the neonatal intensive care unit is one, and it has two admission wards for preterm and term neonates’ with a total of 38 beds and 1500 annual neonatal admission with 128 deaths in last year. Concerning the health professionals, three pediatricians, 13 general practitioners and 12 nurses having different profession are providing the health services.
Study design and population
An institution-based unmatched case-control study was conducted among neonates admitted in the neonatal intensive care unit. All neonates who were admitted in the neonatal intensive care unit and registered as died and alive within the first 28 days in the last one year (2019) period included. Inclusion Criteria for cases, those neonates who admitted and registered as died within the first 28 days of life and have card numbers stated in the logbook and not lost cards with complete chart information were included. Inclusion Criteria for controls, those neonates who admitted and registered as improved within the first 28 days of life and have card numbers stated in the logbook and not lost cards with complete chart information were included. Sample size determination, the sample size was calculated by the StatCalc in Epi-Info version7 statistical software used for sample size determination designed for unmatched case-control study. The following assumptions were considered during sample size calculation; a 95 % level of confidence, power of 80 % and a case to control ratio of one to three (1:3). Considering no single antenatal care service visit (ANC) as an independent exposure variable since, it gave the largest sample size was taken from the study done in Kenya [23]. This gave a total of sample 304 (76 cases and 228 controls. Among public hospitals found in Gedeo Zone, Dilla University Referral Hospital was illegible and selected for this study. Therefore by using the last one-year period medical records, starting from January 31st, 2020 backward to February 1st, 2019 neonatal logbook was reviewed based on their outcome and inclusion criteria.
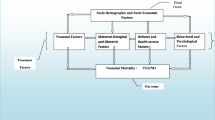
Data collection procedures and study variables
The data extraction checklist was adapted after reviewing related journal articles [19, 23,24,25]by principal investigator. As a data source, a file of admission history, neonatal logbook, history from referral sheet, and delivery summary was used.Based on the medical record numbers, the required numbers of medical record containing cards were drawn out from the card room. Finally, one Bachelor degree of Science (BSc) in midwife and neonatal nurse was collected the data and one health officer supervised data collectors and the collection process was guided by the principal investigator. Dependent variable, neonatal mortality (yes/no).Independent variables Socio-demographic factors: (maternal age, neonatal age, marital status, residence).
Maternal and medical Factors: (parity, ANC follow up, referral status, history of pregnancy-induced hypertension, and Human immune deficiency virus (HIV/AIDS) positive status).
Delivery-related factors: (place of delivery, delivery assistance, mode of delivery.
Newborn factors: (birth weight, preterm, sex of newborn, gestational age, congenital anomalies, sepsis, Activity, Pulse, Grimace, Appearance, and Respiration (APGAR) score, breastfeeding within the first hour, asphyxia, and immediate cry at birth). In an unmatched case-control study of a binary exposure, in which the expected odds ratio deviates from the null (i.e., no effect) and the sum of the number of cases and controls is fixed, 1:1 sampling of cases and controls may yield suboptimal statistical efficiency.
Data quality assurance techniques, data processing and analysis
The data extraction checklists were prepared in the English language. One-day training was given by the principal investigator on the data extraction checklistand procedure. Before actual data collection, the 5 % of checklists were pre-tested in Sidama Regional State, at Yirgalem General Hospital to check the appropriateness of the checklist. After data collection, a 10 % of collected data was cross checked with medical records and assured its consistency by principal investigator. Finally, the coded data was entered into pass word protected computer statistical software by principal investigator. The data was entered and cleaned for missed values and missed variables using EpiData3.1, then exported and analyzed by Statistical Package for Social Science software (SPSS) version 22. The proportion, frequencies, mean, and standard deviations were computed to compare the exposure status between cases and controls. The degree of association between each independent and dependent variable was assessed by a binary logistic regression analysis model. The variables with p-value < 0.25 during bivariate analysis were selected as candidate variables for multivariate logistic regression analysis model. The Hosmer-Lemeshow goodness of fit test was used to determine model adequacy and the model was adequately fitted for the final analysis with p-value > 0. 581, which was insignificant and that indicates the selected variables were important determinants. The Collinearity between independent variables was checked using variance inflation factor (VIF) and confirmed that, there was no existence of multicollinearity effect. Adjusted odds ratios (AORs) at 95 % CI was used to show the strength of association, and statistical significance was declared at a p-value of < 0.05 as determinant for neonatal mortality.
Results
Socio-demographic characteristics
A total of 304 cases were reviewed (76 cases and 228 controls) from the neonatal intensive care unit in the last one year period (February 1st 2019 to January 31st, 2020), with the overall review rate of 100 %. The mean ages of cases were 5.13 (S.D ± 4.71) days and 7.6 (S.D. ±6.38) days for controls. Also, the mean age of mothers in cases and controls was 24.83(S.D ± 5.75) and 25.09(S.D ± 5.93) years respectively. Around three fourth, 55 (72.4 %) of cases and 126 (55.3 %) of controls were admitted within the first seven days of their age. Besides, the average length of stay in the neonatal intensive care unit for cases and controls was 4.49 and 8.18 days respectively (Table 1).
Maternal and medical-related characteristics
In this study, around one third, 23 (30.3 %) of mothers in cases and 34 (14.9 %) of mothers in controls had no single ANC visit during their pregnancy of current neonate. From the mothers having ANC service, thirty seven (69.8 %) of mothers in cases, and 120 (61.8 %) of mothers in controls had ANC visits ranging one up to three. The proportion of mothers who had ANC visit four and above in controls were 74 (38.1 %) which was higher than the proportion of mothers in cases 16 (30.1 %) during the conception of current neonate. The proportions of neonates referred from other health facilities in cases were 53 (69.7 %) which was higher than the proportion of referrals in controls 126 (55.3 %) as illustrated in (Table 2).
The description of delivery-related characteristics
This study found 27 (35.5 %) of mothers in cases and 99 (43.4 %) of mothers in controls gave birth at the hospital. The remaining, 19 (25 %) and 30 (39.5 %) of mothers in cases and 35 (15.4 %) and 94 (41.2 %) of mothers in controls, were from home and health center deliveries respectively. The proportion of assisted vaginal delivery was, 17 (22.4 %) in cases which was higher than the proportion in controls 26 (11.4 %). The proportion of cesarean section was, 7 (9.2 %) in cases and 30 (13.2 %) in controls. Also, the mothers whose labor was not followed by partograph sheet in cases were 34 (59.6 %) which was much higher than the proportion in controls 30 (15.5 %) as indicated in (Table 3).
The description of neonatal related characteristics
More than half of cases, 48 (63.2 %) and 56 (24.6 %) of controls, were below 37 week of gestational age respectively. The proportion of asphyxia in cases were 35 (61.4 %) which was higher than the proportion of asphyxia, 67 (34.7 %) in controls. Regarding sepsis, more than half, 42 (55.3 %) of cases and 57 (25 %) of controls were positive for neonatal sepsis. Also, the proportion of early initiated breastfed within the first hour after delivery in controls was 156 (68.4 %) which was much higher than the proportion in cases 32 (42.1 %). Similarly, the proportion of neonates who cried immediately at birth in controls was 118 (61.1 %) which was higher than the event in cases, 28 (49.1 %) and the remaining variables were indicated (Table 4).
The weight of neonates
The current study found, the proportion of low birth weight (< 2500 g) in cases was 54 (71.1 %), which was much higher than that of proportion in controls 70 (30.7 %) (Fig. 1).
Determinants associated with neonatal mortality
In bivariate analysis, ANC visit, referral status, mode of delivery, gestational age, the weight of newborn, asphyxia, sepsis, statusof breastfed within the first hour, fed colostrum and the ability of neonate to cry at birth were determinants associated with neonatal mortality. In multivariate analysis, referral status, gestational age, the weight of newborns, breastfeedingand sepsis had remained to have an association with neonatal mortality. Those neonates referred from other health institution were 2.43 timesmore likely to die during neonatal period compared to those neonates who were delivered and had follow up in the study hospital[AORs = 2.43, 95 % CI (1.14, 5.22)].Concerninggestational age, those neonates delivered before 37 weeks of gestational agewere 2.50 times more likely to die within the first 28 days of life compared to those neonates delivered at ≥ 37 weeks of gestational age[AORs = 2.50, 95 % CI (1.12, 5.58)].Similarly, those neonates weighing less than 2500 g at birth were 2.44times more likely to die compared with the neonatesweighing greater than or equal to 2500 g at birth [AORs = 2.44, 95 %CI (1.13, 5.28)]. Besides, those neonates who did not breastfeed immediately within the first hour after delivery were5.24 times more likely to die compared to those neonates who fed breast immediately at birth [AORs = 5.24, 95 %CI (2.42, 11.37)].Moreover, those neonates who were positive for sepsis diagnosis were 2.45 times more likely to experience neonatal mortality compared to the neonates who were not positive for sepsis [AORs = 2.45, 95 %CI (1.11, 5.41)] in (Table 5).
Discussion
This study assessed the determinants of neonatal mortality and identified the determinants like; referrals from other health institution, neonates delivered before 37 weeks of gestational age, newborns with birth weight less than 2500 g, neonates who did not feed breast within the first hour after delivery and neonates who were positive for sepsis, as the statistical significant determinants associated with neonatal mortality. Hence, the study findings have implications for the health services targeted to reduce neonatal mortality in the study hospital.
The referrals from other health institution were found to be significantly associated with the occurrence of neonatal mortality. Particularly, the neonates referred from other health institution were 2.43 times more likely to die when compared to the neonates who had no referral. This finding is consistent with the study conducted in Woliata, Ethiopia reported that cases referred from other health institution was 7.32 times more likely to end up in neonatal mortality when compared to the neonates from the study hospital [18]. This finding may be due to birth trauma, infection, delayed action in the health institution and lack of immediate newborn care [12].
The neonates delivered before 37 weeks of gestational age were measured as having a significant association with the event of neonatal mortality. Specifically, those newborns with a gestational age less than 37 weeks were 2.50 times more likely to pass away when compared to neonates who delivered at gestational age of 37 weeks and above.This finding is in line with the result from the study in Rwanda showed newborns with a gestational age less than 37 weeks were 3.1 times more likely to die than their counterparts [26]. Similarly, this result is in agreement with the study in Kenya revealed that cases with gestational age < 37 weeks were 7.0 times more likely to die when compared to controls with gestational age of 37 weeks and above[23]. Likewise the study in Adama, Ethiopia also showed consistent finding with this study in which preterm neonates were 3.3 times more likely to die compared to term neonates [27]. This result might be due to immaturity of respiratory and cardiovascular organs, vulnerability to infection, hypothermia, and lack of skilled medical care during intrapartum, and postpartum period [3, 4].
In this study, the birth weight of newborn less than 2500 g was significantly associated with the event of neonatal mortality. Especially, those neonates weighing less than 2500 g were 2.44 times more likely to die when compared to the neonates weighing 2500 g and above at birth. The current finding is consistent with the report of study from Jimma, Ethiopia which showed cases with low birth weight was 1.54 times more likely to die when compared to their counterparts [25]. Similarly, the study conducted in Adama, Ethiopia illustrated comparable finding with this study in which neonates with birth weight < 2500 g were 1.6 times more likely to die than the neonates with birth weight ≥ 2500 g [27]. Likewise, this result also concur with the study in Wolaita, Ethiopia found low birth weight were 9.0 times more likely to die when compared to newborns with normal birth weight [18]. This finding might be due to birth defect, infections, hypothermia, lack of medical care during intrapartum and postnatal period. Also it might be due to inability to adapt the external environment [3, 7].
This study also found that neonates who didn’t feed breastwithin the first hour after delivery was positively associated with the experience of neonatal mortality. Specifically, neonates who didn’t feed breast milk immediately were 5.24 times more likely to die when compared to those neonates who were breastfed immediately at birth. This finding is in line with the study conducted in Indonesia showed, cases who didn’t feed breast early were 10.46 times more likely to die when compared to their counterparts [28]. Similarly, this finding is in consistent with the study in Amhara, Ethiopia reported neonates who didn’t feed breast within the firsthour of delivery were 23.48 times more likely to die than their counterparts [29]. Likewise, a study in Woliata Ethiopia found comparable finding in which neonates who were not breastfed within first hour were 2.6 times more likely to die than those who breastfed immediately after birth [19]. This finding might be due to lack of protective effect of early initiated breast milk, and increased susceptibility to gastroenteritis, common newborn infections and diseases, as indicated in different reports [7, 12, 13].
Besides, in current study those neonates who were positive for sepsis diagnosis was significantly associated with the event of neonatal mortality. Uniquely, those neonates who were positive for sepsis were 2.45 times more likely to diewhencompared to the neonates who were not positive for sepsis. This finding is concurring with the study report from Adama Ethiopia revealed cases with positive for sepsis were 2.4 times more likely to die when compared to their counterparts [27]. Similarly, this finding in line with the study in MizanTepi, Ethiopia showed cases positive for sepsis were higher risk of death when compared to the neonates not positive for sepsis [24]. This result might be due to the extreme response to an infection, tissue damage, organ failure and lack of immediate medical care [7].
In current study ANC receiving status was not significantly associated with the occurrence of neonatal mortality in multivariate analysis. This finding is contradicting with the studies conducted in Rwanda, Democratic Republic of Congo (DRC), Kenya, Ethiopia (Amhara, and Wolaita) [19, 23, 26, 29, 30], showed those neonates delivered from mothers who had no or incomplete ANC visit were more likely to die than neonates from mothers who have followed ANC visit four and above. This discrepancy might be due to methodological difference and inconsistency of records.
The strength of current study compared one case with three controls to increase the representativeness of the sample, and crosschecked a 10 % of collected data with medical records and assured consistency by principal investigator. The major limitations of this study are its design and selection bias. Only neonates assessed who used healthcare services in the DURH, were included in this study. Another limitation is related to estimation methods. They generally do not allow calculation of incidence (absolute risk). This study used secondary data as a source of information which was not specific and there were difficulties to measure some variables. Further, the collected data was from a single institution, so it may have some drawbacks, regarding population under the study. Also, this study failed to measure the status of neonates who discharged alive before 28 days after admission. Hence, this may decrease the external validity of the study.
Conclusions
Results from this study suggest that the referral status, gestational age below 37 weeks, birth weight less than 2500 g, neonates who did not feed breastwithin the first hour after delivery, and neonates positive for sepsis diagnosis were measured as the significant independent determinants to neonatal. This study shows that neonatal intensive care unit service should be strengthened in Dilla University Referral Hospital; targeting neonate aged below 28 days. Most of the determinants may be prevented and minimized by strengthening referral linkage, improving intrapartum and postpartum care. Further research is needed in order to better understand reasons for neonatal mortality. Further, those who are interested should conduct an institution based incidence study to see the sequence of event.
Availability of data and materials
All data are available within manuscript and it will be upon reasonable request from the corresponding author.
Abbreviations
- AOR:
-
Adjusted Odds Ratio
- APGAR:
-
Activity, Pulse, Grimace, Appearance, and Respiration
- COR:
-
Crude Odds Ratio
- DHS:
-
Demographic Health Survey
- DRC:
-
Democratic Republic of Congo
- DURH:
-
Dilla University Referral Hospital
- EDHS:
-
Ethiopian Demographic Health Survey
- EMDHS:
-
Ethiopian Min Demographic Health Survey
- MOH:
-
Ministry of Health
- LBW:
-
Low Birth Weight
- NICU:
-
Neonatal Intensive Care Unit
- NMR:
-
Neonatal Mortality Rate
- SDG:
-
Sustainable Development Goal
References
WHO, Neonatal and Perinatal Mortality Country, Regional and Global Estimates 20 Avenue Appia, 1211 Geneva 27, Switzerland 2006. P. 1–75.
Barfi eld WD and AAP COMMITTEE ON FETUS AND NEWBORN. Standard Terminology for Fetal, Infant, and Perinatal Deaths. Pediatrics. 2016;137(5):P.1–7.
World Health Organization; Making Every Baby Count Audit and review of stillbirths and neonatal deaths.Department of Maternal, Newborn, Child and Adolescent Health, Geneva 27, Switzerland. (2016):1-144.
United Nations Inter-agency Group for Child Mortality Estimation (UNIGME), ‘Levels & Trends in Child Mortality: Report 2019, Estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation’, United Nations Children’s Fund, New York, 2019. P. 1–52.
World Health Organization: Survive and thrive: transforming care for every small and sick newborn. Geneva (2019). License: CC BY-NC-SA 3.0 IGO. P. 1-162.
United Nations Inter-agency Group for Child Mortality Estimation (UNIGME), ‘Levels & Trends in Child Mortality: Estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation’, United Nations Children’s Fund, New York, Report 2018. P.1–48.
WHO, UNICEF: Every Newborn: An action plan to end preventable deaths.Geneva: World Health Organization. Avenue Appia, 27, Switzerland 2014.P. 1–58.
Zimmerman Linnea, Shiferaw Solomon, Seme Assefa, Yihdego Mahari, Desta Selamawit, Shankar Mirdula, Wood Shannon, and Ahmed Salfuddin Final Report: Maternal and Newborn Health in Southern Nations, Nationalities and Peoples’ Region, Ethiopia. Baltimore, Maryland, USA: Bill & Melinda Gates Institute for Population and Reproductive Health, Johns Hopkins University Bloomberg School of Public Health.(2018) P. 1–166.
Ethiopian Public Health Institute (EPHI) [Ethiopia] and ICF. 2019. Ethiopia Mini Demographic and Health Survey 2019: Key Indicators. Rockville, Maryland, USA: EPHI and ICF. P. 1–35.
Central Statistical Agency (CSA) [Ethiopia] and ICF. 2016. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF. P. 1–551.
World health statistics overview: Monitoring health for the SDGs, Sustainable Development Goals. Geneva: WHO; 2019 (WHO/DAD/2019.1). P. 1–28.
World Health Organization: Reaching every newborn national 2020 milestones: country progress, plans and moving forward. Geneva: 2017. CC BY-NC-SA 3.0 IGO.1–76.
World Bank, IEG, IFC and MIGA; Delivering the Millennium Development Goals To Reduce Maternal and Child Mortality (2015). 1-182.
World Health Organization; World health statistics 2015. P.1-164.
FMOH; National Strategy for Newborn and Child Survival, Addis Ababa, Ethiopia. 2015/16–2029/20 JUNE 2015. P. 1–83.
UN;Transforming our world:The 2030 Agenda for Sustainable Development, 2015.1–73.
The Federal Democratic Republic of Ethiopia Ministry of Health, Health Sector Transformation Plan 2015/16–2019/20 (2008–2012 EFY). P. 1-184.
Mihiretu A, Negash T, Elazar T; Perinatal Death and Associated Factors in Wolaita Sodo Referral Hospital, Southern Ethiopia: A Facility-Based Cross-Sectional Study. Prim Health Care. 2017. 7(2): 1–5.
Tujare Tunta Orsido, Netsanet Abera Asseffa and Tezera Moshago Berheto: Predictors of Neonatal mortality in the Neonatal intensive care unit at referral Hospital in Southern Ethiopia: BMC Pregnancy and Childbirth (2019) 19:83. P.1–9.
Centeral Statistical Agency (CSA):The Management of Cmmercial Road Transport in Ethiopia; Road authority, 2009.p.1-234.
Dilla University Teaching and Referral Hospital Hospital; Hospital based annual plan, 2011EFY. P. 1–44.
Central Statistical Agency(CSA); The Federal Democratic Republic of Ethiopia Population Estimates of 2007. P. 1-243.
Faith Yego, Catherine D’ Este, Julie Byles, Paul Nyongesa and Jennifer Stewart Williams: A case-control study of risk factors for fetal and early neonatal deaths in a tertiary hospital in Kenya; BMC Pregnancy and Childbirth (2014) 14:389. P.1–9.
Tilahun Mekonnen, Tsehay Tenu, Tsegenet Aklilu and Tesfaye Abera: Assessment of Neonatal Death and Causes among Admitted Neonates in Neonatal Intensive Care Unit of Mizan Tepi University Teaching Hospital, Bench Maji Zone, South-West Ethiopia. Clinics Mother Child Health 2018, 15(4) P.1–5.
Sheka Shemsi Seid, Shemsedin Amme Ibro, Abdulwahid Awol Ahmed, Adugna Olani Akuma, Ebrahim Yimam Reta, Tura Koshe Haso, and Gutema Ahmed Fata: Causes and factors associated with neonatal mortality in Neonatal Intensive Care Unit (NICU) of Jimma University Medical Center, Jimma, South West Ethiopia; Dove Press journal: Pediatric Health, Medicine and Therapeutics 2019:10. 39–48.
Théoneste NDAYISENGA. Maternal and Newborn Risk Factors associated With Neonatal Mortality in Gitwe District Hospital in Ruhango District, Rwanda. Int. J. Med. Public Health, 2016; 6(2):98–102.
Kolobo HA, Chaka TE, Kassa RT; Determinants of neonatal mortality among newborns admitted to neonatal intensive care unit Adama, Ethiopia: A case-control study. J Clin Neonatol 2019; 8: p. 232–7.
Asnawi Abdullah, Krishna Hort, Yuli Butu and Louise Simpson: Risk factors associated with neonatal deaths: a matched case-control study in Indonesia. Global Health Action (2016), 9: 30445. 1–12.
Kolola Tufa, Ekubay Meseret, Tesfa Endalamaw, Morka Wogene; Determinants of Neonatal Mortality in North Shoa Zone, Amhara Regional State, Ethiopia. PLoSONE. 2016. 11(10): 1–11.
Mashako RM, BitweM R, Ngbonda D, Mashako KY, Alworong’a OJ, Nsibu NC: Predictive factors of neonatal mortality in the intensive neonatal care unit at Goma Eastern Democratic Republic of Congo. J Pediatrics and Neonatal Care. 2019; 9(2):58–61.
Acknowledgements
We would like to thank the data collectors, and supervisors for their cooperation. We also sincerely appreciate Dilla University Referral Hospital manager, neonatal intensive care unit and card room coordinators, supervisor, and data collectors, for their unreserved effort.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
AA involved in conceptualization, investigation and formally analysis, AD participated in design, data curation and manuscript review, AD participated in preparation and critically revised the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to publication.
Prior to data collection appropriate ethical clearance and supportive letter was obtained from Dilla University College of Medicine and Health Sciences Institutional Review Board (IRB) and the informed consent was obtained from all parents. All methods were carried out in accordance with relevant guidelines and regulations Ethics approval and consent to participate.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Adem, A., Dache, A. & Dona, A. Determinants of neonatal mortality among newborns admitted in neonatal intensive care unit at Dilla University Referral Hospital in Gedeo Zone, Southern, Ethiopia: unmatched case control study. BMC Pediatr 21, 307 (2021). https://doi.org/10.1186/s12887-021-02780-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-021-02780-3