Abstract
Background
Acute respiratory infection is manifested by cough accompanied by short rapid breathing which may be associated with death especially when there are other co-morbidities. From an estimated 5.4 million children under –five years that died in 2017—roughly half of those deaths occurred in sub-Saharan Africa and acute respiratory infection contributed to the highest number of deaths. The current study aimed at evaluating the prevalence of, and risk factors associated with, acute respiratory infection hospitalization in under-five years children hospitalized at the University of Gondar Comprehensive Specialized Hospital.
Method
An institution-based cross-sectional study was carried out from May 01/2019 to July 10/2019. After the selection of participants using simple random sampling, face to face interview was performed using a semi-structured pre-tested questionnaire. Data were also extracted from medical registration charts. We used EPI Info 7 for data entry and exported into SPSS 21 for analysis. Results were presented by simple frequency, percentage and mean for descriptive variables. Binary logistic regression analysis was used to test the association of covariates and outcome variable. Variables with a p < 0.2 during the bivariable binary logistic regression analysis were included in the multivariable logistic regression analysis. Variables with p < 0.05 were considered as significantly associated with acute respiratory infection. This study is reported following the Strengthening the Reporting of Observational Studies in Epidemiology guideline.
Results
Four hundred and twenty-two under-five years’ children attending the Pediatrics ward were included in this study. The prevalence of acute respiratory infection among under-five years’ children in this study was 27.3%. Children aged below 12 months (AOR:3.39, 95% CI: 1.19, 9.65), maternal age of 16 to 27 years (AOR: 1.95, 95% CI: 1.03, 3.70), maternal age of 28 to 33 years (AOR: 2.73, 95% CI: 1.40, 5.34), lack of maternal awareness of handwashing (AOR: 2.79, 95% CI: 1.15, 6.76), rural residence (AOR:2.27, 95% CI: 1.18, 4.39), and lack of meningitis (AOR: 0.22, 95% CI: 0.08, 0.55), were significantly associated with acute respiratory infection.
Conclusion
Acute respiratory infection was common among children under-five years. Child and maternal age, residence and maternal hand hygiene information were significant factors identified to be associated with an acute respiratory infection.
Similar content being viewed by others
Background
Acute respiratory infection (ARI) is manifested by cough accompanied by short rapid breathing which may be associated with death especially when there are other co-morbidities [1], even though a significant decline has been achieved over the past two decades [2]. From an estimated 5.4 million under-five children that died in 2017—roughly half of those deaths occurred in sub-Saharan Africa and ARIs contributed to the highest number of deaths [3]. ARIs are among the leading causes of morbidity and mortality among children under-five years worldwide [3]. Mortality due to ARI is significantly varied across regions [4]. In 2010, global burden disease reported that more than 12 million children with severe ARI were admitted to hospitals every year worldwide [5]. ARI accounts for up to 50% of visits of children to health facilities globally [6].
Pneumonia accounts for the death of approximately 2400 under-five years children a day [7]. ARIs are responsible for approximately 70% of under-five years of childhood morbidities in developing countries [8]. A study conducted to assess the prevalence of acute lower respiratory infections (ALRIs) among children under-five years from 28 sub-Saharan African countries revealed the overall prevalence of ARI for all the countries was 25.3% [9]. In Ethiopia, 7 % of under-five years had symptoms of ARI in the 2 weeks before the Ethiopian Demographic and Health survey and three out of 10 of these children sought treatment [10]. The under-five years’ mortality rate in Ethiopia is 67 deaths per 1000 live births [10] .
Several factors predispose children under five years of age for ARIs. These factors may be attributed to child factors such as age [11,12,13,14,15] and female sex [16], maternal factors such as lower age [11, 13], unemployment [11, 13] and lower educational status [16, 17] environmental-related factors such as urban residence [17], rural residence [18], wet season [19,20,21] and co-morbid diseases [14, 22, 23]. There is a paucity of studies regarding the prevalence and associated factors of ARI among hospitalized under-five years children in Ethiopia even though few community-based cross-sectional studies [24,25,26] have been undertaken in to assess the prevalence and associated factors of ARIs among under-five years children. The current study, therefore, is aimed at assessing the prevalence and associated factors of ARI among under-five years’ children hospitalized in the Pediatric ward at University of Gondar Comprehensive Specialized Hospital, northwest Ethiopia.
Methods
Study design and settings
The current study was conducted at the University of Gondar Comprehensive Specialized Hospital among randomly selected under-five years children who were admitted at the Pediatrics ward of the Hospital from May 01/2019 to July 10/2019. The mothers of the children were respondents in this study. The Hospital is located in Gondar city, northwest Ethiopia. It is located 738 km from Addis Ababa and is serving more than 5 million people annually. In 2018, the Hospital had 1040 health care professionals, 580 beds in five different inpatient departments and 14 wards, and 14 different units giving outpatient services to customers [27, 28].
Sample size determination and sampling technique
The sample size was calculated using a single population proportion formula [29] assuming; prevalence of ARI (p) = 50% to allow maximum variation (as there was no previous institutional-based study in the country about the proportion of under-five years hospitalized children with ARIs), 95% confidence level, z = the standard normal tabulated value, and α = level of significance and margin of error (d) =0.05
After adding expected oversampling of 10% for unexpected events, the final total sample size was 422. Study participants were selected using a computer-generated simple random sampling technique using their medical registration number. Sampling was taken on daily basis and children were selected from a random number list for each day. Whenever parents did not consent the next number was taken.
Eligibility criteria
Under-five years who visited the Paediatrics ward at University of Gondar Comprehensive Specialized Hospital at time of data collection period in which their mothers consented to participate were included whereas children whose mothers or caretakers refused to take part in the study due to different reasons were excluded.
Data collection instrument and quality control
A pre-tested, semi-structured questionnaire containing socio-demographic variables on maternal and child factors and extraction tool to review chart was used. Interviews and chart reviews were undertaken by three BSc Nurse Professionals. Training about the data collection tool, techniques, the purpose of the study, data extraction tool and ethical issues was given for data collectors. The questionnaire was validated for content and reliability analysis was performed based on the pretest result on 20 individuals. We have also made corrections for ambiguities before actual data collection. Comments were obtained from each participant and based on their recommendations, the questionnaire was updated. The internal consistency was analyzed using Cronbach’s α coefficient [30]. The Cronbach’s α results were 0.7 for knowledge, 0.73 for attitude, 0.87 for practice and 0.78 overall results. According to George, this is acceptable internal consistency [31].
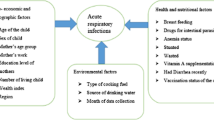
Study variables
The dependent variable in the current study was children’s acute respiratory infection. The independent variables were child-related (age, sex, residence, comorbidities (diarrhoea, meningitis and malnutrition), maternal factors (age, education, information, knowledge, attitude and practice of handwashing)).
Measurement of variables
The variable of interest in this study was ARI occurring in under-five years children. Presence or absence of ARI was determined by the health professionals with any one or combination of symptoms and signs like cough, sore throat, rapid breathing, noisy breathing, chest indrawing, at any time in the last 2 weeks and the status is taken directly from the chart review. Meningitis assessment was based on physicians assessment. Diarrhoea was defined as having three or more loose or watery stools within 24 h [32]. Malnutrition was determined by anthropometric measurement of mid-upper arm circumference, weight for age and height for age [33]. The maternal knowledge, attitude and practice regarding handwashing were determined by asking the mothers knowledge, attitude and practice questions. Since the data for all of the three variables were normally distributed, we used mean to dichotomize maternal handwashing knowledge, attitude and practice as good or poor. Study subjects that scored at the mean or above the mean on maternal knowledge, attitude and practice questions were considered having good knowledge, attitude and practice. The maternal age was categorized based on the quartile range.
Data processing and analysis
The data were entered using Epi-Info version 7 and analyzed using SPSS statistical package version 21.0. All assumptions for binary logistic regression were checked.
To determine predictor variables for ARI, a binary logistic regression model was fitted and variables at a p-value < 0.2 during the bi-variable analysis were included in the multivariable analysis.
Finally, variables found to be significant at a p-value < 0.05 in the final model were declared as predictors. Crude odds ratios (COR) and adjusted odds ratios (AOR) with 95% confidence interval were reported. Hosmer and Lemeshow goodness- of -fit test (p > 0.05) was used to check model fitness. The report was prepared based on the Strengthening the Reporting of Observational Studies guideline.
Results
Sociodemographic characteristics of study participants
Four hundred and twenty-two under-five years’ children were included in the current study.
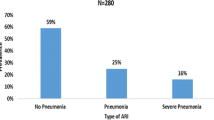
Most (238/422, 56.4%) of the children resided in an urban setup and 221 (50.0%) were male. The prevalence of ARI, diarrhea and malnutrition were 27.3, 30.1 and 24.4%, respectively (Table 1).
Factors associated with ARI
The bivariable analysis revealed that child and maternal age, residence, maternal educational status and information about handwashing, knowledge and practice about handwashing were variables with a p-value < 0.2, and these variables were included in the multivariable logistic regression model. Child and maternal age, residence, and maternal information about handwashing were significantly associated with ARI among under-five years in the final model.
Children below 12 months had a 3.39-fold (AOR: 3.39, 95% CI: 1.19, 9.65) increased adjusted odds of ARI hospitalization. Under-five years children of mothers aged 16 to 27 and 28 to 33 years had a 1.95 (AOR: 1.95, 95% CI: 1.03, 3.70) and a 2.73(AOR: 2.73, 95% CI: 1.40, 5.34) adjusted odds of ARI hospitalization compared to those whose mothers older than 42 years. The adjusted odds of ARI was 2.27-fold (AOR: 2.27, 95% CI: 1.18, 4.39) higher in children residing in a rural setting compared to those from urban setup. Similarly, children with meningitis had 78% reduced adjusted odds of ARI hospitalization (AOR: 0.22, 95% CI: 0.08, 0.55) compared to those without meningitis. Children whose mothers reported lack of knowledge about handwashing had a 2.79-fold (AOR: 2.79, 95% CI: 1.15, 6.76) increased odds of ARI hospitalization compared to those whose mothers knew about handwashing (Table 2).
Discussion
The current study aimed at evaluating the prevalence of, and risk factors associated with, ARI hospitalization in under-five years children hospitalized at the University of Gondar Comprehensive Specialized Hospital. The proportion of under-five years children with ARI in this study was 27.3 95% CI (23.2–31.5%). This is in line with the overall prevalence of ARIs among children under-five years from 28 Sub-Saharan African countries (25.3%) [9], previous studies in Gondar (26.3%) [24] and Addis Ababa (23.9%) [26]. However, it is lower than prevalence of ARI reported from India (41.6%) [34], Cameroon (54.7%) [35], Nigeria (64.9%) [36], Kenya (69.7%) [37], and Bangladesh (70%) [38]. The current prevalence is slightly higher than a study conducted in southern Ethiopia (21%) [25]. This variations in the proportions of ARI could be as a result of differences in study populations, study settings (community-based versus institutional-based), age categories studied, the method used to assess the outcome variable, comorbidities and variations in the study period and season of the study.
From the factors tested in the current study; child age, maternal age, residence, and maternal handwashing information were significantly associated with ARIs among under-five years children attending the Pediatric ward of the University of Gondar Comprehensive Specialized Hospital.
Child age was associated with ARI hospitalization. The odds of developing ARI was higher among children below 12 months of age as compared to those aged above 48 months. This was in line with a previous study [39]. Higher risk of ARI among lower age children might be due to less developed immunity [40]. However, it was inconsistent with another study [35].
Maternal age was associated with children’s ARI status. The adjusted odds of developing ARI was 1.95 and 2.73-folds higher among children having mothers aged 16 to 27 and 28–33 years, respectively. This was in line with previous studies [11, 41,42,43]. Maternal age was not associated in several earlier studies [9, 14, 24, 35]. The association of maternal age with ARI can be explained by mothers’ experience to give necessary and sufficient care for their children as younger mothers may be less experienced in child care services.
Children from rural setup were more prone to develop ARI in the current study which is in line with several earlier studies [12, 39, 44,45,46]. The probable justification for the greater ARI symptoms proportion for rural children may be due to lack of access to medical care, low socio-economic standards in rural regions [47] and most risk factors for ARI prevail in rural setup [48]. However, in other studies [23, 49], the residence was not significantly associated and Kumar et’ al reported urban residence to be a risk factor for ARI [17].
Children with meningitis infection were less likely to develop ARI. Pneumococcal meningitis incidence was found to be highly associated with the incidence of acute viral respiratory infection in previous studies [50,51,52,53,54,55]. The lesser odds of ARI among children with meningitis may be attributed to the fact that children with meningitis will receive antibiotics.
Unlike several previous studies [56,57,58] in the current study maternal self-defined handwashing practice and attitude were not significantly associated with ARI in the final model. This might be due to the fact that self-reported handwashing practice is from a simple cleansing to the appropriate level of recommended duration and method of handwashing. However, the lack of association in the current study is in line with a population-based study in Sweden [59]. In the current study children of mothers who have reported a lack of information about handwashing were more likely to be at higher risk of ARI.
Limitations of the study
This study was not without limitation. Treatment and outcomes were not collected; recruitment only took place over a 3 month period, so prevalence may be different during different months of the year. The seasonality of ARI was not studied in Ethiopia previously and we had collected information within 3 months’ time and unable to see the temporal variability in the prevalence in the current study. The housing-related confounders and comorbidities such as HIV were not assessed. Hand washing practice was assessed by self-report and may be prone to social desirability bias. Besides, the cause-effect relationship cannot be established as this is a cross-sectional study. Because of the lack of sufficient institutional-based prevalence studies regarding ARI among under-five years children comparing with previous similar studies was difficult.
Conclusion
A significant proportion of under-five years children admitted at pediatrics ward at the University of Gondar Comprehensive Specialized Hospital had ARI. Maternal and child age, residence, and maternal hand hygiene information were significant factors identified to be associated with ARI.
Availability of data and materials
The dataset is accessible at the corresponding author upon a reasonable request.
Abbreviations
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- COR:
-
Crude odds ratio
- EPI Info:
-
Epidemiological information
- SPSS:
-
Statistical package for social sciences
References
Johnson W, Abdulkarim A. Childhood pneumonia in developing countries. Afr J Respir Med. 2013;8:574–84.
Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1736–88.
Accinelli RA, Leon-Abarca JA, Gozal D. Ecological study on solid fuel use and pneumonia in young children: a worldwide association. Respirology. 2017;22(1):149–56.
Collaborators GCM. Erratum: Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015 (The Lancet (2016) 388 (10053)(1725–1774)(S0140673616315756)(10.1016/S0140-6736 (16) 31575-6)). Lancet. 2017;389(10064):e1.
Nair H, Simões EA, Rudan I, Gessner BD, Azziz-Baumgartner E, Zhang JSF, et al. Global and regional burden of hospital admissions for severe acute lower respiratory infections in young children in 2010: a systematic analysis. Lancet. 2013;381(9875):1380–90.
West T, Goetghebuer T, Milligan P, Mulholland EK, Weber M. Long-term morbidity and mortality following hypoxaemic lower respiratory tract infection in Gambian children. Bull World Health Organ. 1999;77(2):144.
United nations children’s fund (UNICEF). Pneumonia 2018. Available from: https://data.unicef.org/topic/child-health/pneumonia/. [cited 2020 February, 19].
Selvaraj K, Chinnakali P, Majumdar A, Krishnan IS. Acute respiratory infections among under-5 children in India: A situational analysis. J Nat Sci Biol Med. 2014;5(1):15.
Seidu A-A, Dickson KS, Ahinkorah BO, Amu H, Darteh EKM, Kumi-Kyereme A. Prevalence and determinants of acute lower respiratory infections among children under-five years in sub–Saharan Africa: evidence from demographic and health surveys. SSM-Popul Health. 2019;8:100443.
Ethiopia Demographic. Health Survey 2016. Rockville: Ethiopian Central Statistical Agency and The DHS Program ICF; 2017.
Cardoso AM, Coimbra CE Jr, Werneck GL. Risk factors for hospital admission due to acute lower respiratory tract infection in Guarani indigenous children in southern Brazil: a population-based case-control study. Tropical Med Int Health. 2013;18(5):596–607.
Seidu A-A, Ameyaw EK, Ahinkorah BO, Baatiema L, Appiah F. Ecological zone and symptoms of acute respiratory infection among children under five in Ghana: 1993–2014. SSM-Popul Health. 2019;100414.
Gebretsadik A, Worku A, Berhane Y. Less than one-third of caretakers sought formal health care facilities for common childhood illnesses in Ethiopia: evidence from the 2011 Ethiopian demographic health survey. Int J Fam Med. 2015;2015.
Matu MN. Risk factors and cost of illness for acute respiratory infections in children under five years of age attending selected health facilities in Nakuru County. Kenya: Jomo Kenyatta University of Agriculture and Technology; 2015.
Chalabi D. Acute respiratory infection and malnutrition among children below 5 years of age in Erbil governorate, Iraq. EMHJ-Eastern Mediterr Health J. 2013;19(1):66–70.
Al-Sharbatti SS, LI AJ. Infant feeding patterns and risk of acute respiratory infections in Baghdad/Iraq. Ital J Public Health. 2012;9(3).
Kumar SG, Majumdar A, Kumar V, Naik BN, Selvaraj K, Balajee K. Prevalence of acute respiratory infection among under-five children in urban and rural areas of puducherry, India. J Nat Sci Biol Med. 2015;6(1):3.
Prajapati B, Talsania N, Lala M, Sonalia K. A study of risk factors of acute respiratory tract infection (ARI) of under five age group in urban and rural communities of Ahmedabad District. Gujarat Healthline. 2012;3(1):16–20.
Fienemika A, Ojule I, Best O. Prevalence of acute respiratory infections among children under-five years old in a hospital in Port Harcourt, Nigeria: A two year follow-up study. J of Respir Med. 2018;2(1):1–6.
Gessner BD, Shindo N, Briand S. Seasonal influenza epidemiology in sub-Saharan Africa: a systematic review. Lancet Infect Dis. 2011;11(3):223–35.
Hart CA, Cuevas LE. Acute respiratory infections in children. Rev Brasileira de Saúde Materno Infantil. 2007;7(1):23–9.
Dadi AF, Kebede Y, Birhanu Z. Determinants of pneumonia in children aged two months to five years in urban areas of Oromia zone, Amhara region. Ethiopia Open Access Lib J. 2014;1(08):1.
Amsalu ET, Akalu TY, Gelaye KA. Spatial distribution and determinants of acute respiratory infection among under-five children in Ethiopia: Ethiopian demographic health survey 2016. PLoS One. 2019;14(4):e0215572.
Alemayehu M, Alemu K, Sharma HR, Gizaw Z, Shibru A. Household fuel use and acute respiratory infections in children under five years of age in Gondar city of Ethiopia. J Environ Earth Sci. 2014;4(7):77–85.
Desalegn B, Suleiman H, Asfaw A. Household fuel use and acute respiratory infections among younger children: an exposure assessment in Shebedino Wereda, southern Ethiopia. Afr J Health Sci. 2011;18(1–2):31–6.
Sanbata H, Asfaw A, Kumie A. Association of biomass fuel use with acute respiratory infections among under-five children in a slum urban of Addis Ababa, Ethiopia. BMC Public Health. 2014;14(1):1122.
University of Gondar Comprehensive Specialized Hospital. Planning, monitoring and evaluation department report 2017.
Gedif G, Sisay Y, Alebel A, Belay YA. Level of job satisfaction and associated factors among health care professionals working at University of Gondar Referral Hospital, Northwest Ethiopia: a cross-sectional study. BMC Res Notes. 2018;11(1):824.
Arifin WN. Introduction to sample size calculation. Educ Med J. 2013;5(2).
Barua A. Methods for decision-making in survey questionnaires based on Likert scale. J Asian Sci Res. 2013;3(1):35–8.
George D. SPSS for windows step by step: A simple study guide and reference, 17.0 update, 10/e. Boston: Pearson Allyn & Bacon; 2011.
Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet. 2003;361(9376):2226–34.
Grellety E, Golden MH. Weight-for-height and mid-upper-arm circumference should be used independently to diagnose acute malnutrition: policy implications. BMC Nutr. 2016;2(1):10.
Savitha A, Gopalakrishnan S. Determinants of acute respiratory infections among under five children in a rural area of Tamil Nadu, India. J Fam Med Prim Care. 2018;7(6):1268.
Tazinya AA, Halle-Ekane GE, Mbuagbaw LT, Abanda M, Atashili J, Obama MT. Risk factors for acute respiratory infections in children under five years attending the Bamenda regional Hospital in Cameroon. BMC Pulmon Med. 2018;18(1):7.
Solomon O, Odu O, Amu E, Solomon O, Bamidele J, Emmanuel E, et al. Prevalence and risk factors of acute respiratory infection among under fives in rural communities of Ekiti state Nigeria. Global J Med Public Health. 2018;7(1):12.
角井, 信弘. The prevalence of acute respiratory infections and the associated risk factors: a study of children under five years of age in Kibera Lindi village, Nairobi, Kenya. J Natl Inst Public Health. 2002;51:1.
Rahman M, Shahidullah M. Risk factors for acute respiratory infections among the slum infants of Dhaka city. Bangladesh Med Res Counc Bull. 2001;27(2):55–62.
Harerimana J-M, Nyirazinyoye L, Thomson DR, Ntaganira J. Social, economic and environmental risk factors for acute lower respiratory infections among children under five years of age in Rwanda. Arch Public Health. 2016;74(1):19.
Amugsi DA, Aborigo RA, Oduro AR, Asoala V, Awine T, Amenga-Etego L. Socio-demographic and environmental determinants of infectious disease morbidity in children under 5 years in Ghana. Glob Health Action. 2015;8(1):29349.
César JA, Victora CG, Santos IS, Barros FC, Albernaz EP, Oliveira LM, et al. Hospitalização por pneumonia: influência de fatores socioeconômicos e gestacionais em uma coorte de crianças no Sul do Brasil. Rev Saude Publica. 1997;31(1):53–61.
Victora CG, Fuchs SC, Flores JAC, Fonseca W, Kirkwood B. Risk factors for pneumonia among children in a Brazilian metropolitan area. Pediatrics. 1994;93(6):977–85.
Prietsch SO, Fischer GB, César JA, Lempek BS, Barbosa LV Jr, Zogbi L, et al. Acute lower respiratory illness in under-five children in Rio Grande, Rio Grande do Sul state, Brazil: prevalence and risk factors. Cadernos de saude publica. 2008;24:1429–38.
Sultana M, Sarker AR, Sheikh N, Akram R, Ali N, Mahumud RA, et al. Prevalence, determinants and health care-seeking behavior of childhood acute respiratory tract infections in Bangladesh. PLoS One. 2019;14(1):e0210433.
Rehman M, Ishaq M. Prevalence of acute respiratory infections (ARI) and its risk factors in under five children in urban and rural areas of Matta, district swat. Int J Infect Dis. 2018;73:230.
Sk R, Rasooly MH, Barua S. Do fuel type and place of cooking matter for acute respiratory infection among afghan children? Evidence from the Afghanistan DHS. J Biosoc Sci. 2015;2019:1–14.
Kilabuko J, Nakai S. Effects of cooking fuels on acute respiratory infections in children in Tanzania. Int J Environ Res Public Health. 2007;4(4):283–8.
Sharma D, Kuppusamy K, Bhoorasamy A. Prevalence of acute respiratory infections (ari) and their determinants in under five children in urban and rural areas of Kancheepuram district, South India. Ann Trop Med Public Health. 2013;6(5):513.
Pinzón-Rondón ÁM, Aguilera-Otalvaro P, Zárate-Ardila C, Hoyos-Martínez A. Acute respiratory infection in children from developing nations: a multi-level study. Paediatr Int Child Health. 2016;36:1–7.
Opatowski L, Varon E, Dupont C, Temime L, van der Werf S, Gutmann L, et al. Assessing pneumococcal meningitis association with viral respiratory infections and antibiotics: insights from statistical and mathematical models. Proc R Soc B Biol Sci. 2013;280(1764):20130519.
Murdoch DR, Jennings LC. Association of respiratory virus activity and environmental factors with the incidence of invasive pneumococcal disease. J Infect. 2009;58(1):37–46.
Kim PE, Musher DM, Glezen WP, Barradas MCR, Nahm WK, Wright CE. Association of invasive pneumococcal disease with season, atmospheric conditions, air pollution, and the isolation of respiratory viruses. Clin Infect Dis. 1996;22(1):100–6.
Jansen AG, Sanders EA, van der Ende A, van Loon AM, Hoes AW, Hak E. Invasive pneumococcal and meningococcal disease: association with influenza virus and respiratory syncytial virus activity? Epidemiol Infect. 2008;136(11):1448–54.
Watson M, Gilmour R, Menzies R, Ferson M, McIntyre P, Network NSWP. The association of respiratory viruses, temperature, and other climatic parameters with the incidence of invasive pneumococcal disease in Sydney, Australia. Clin Infect Dis. 2006;42(2):211–5.
Krasinski K, Nelson JD, Butler S, Luby JP, Kusmiesz H. Possible association of mycoplasma and viral respiratory infections with bacterial meningitis. Am J Epidemiol. 1987;125(3):499–508.
Hovi T, Ollgren J, Savolainen-Kopra C. Intensified hand-hygiene campaign including soap-and-water wash may prevent acute infections in office workers, as shown by a recognized-exposure-adjusted analysis of a randomized trial. BMC Infect Dis. 2017;17(1):47.
Little P, Stuart B, Hobbs F, Moore M, Barnett J, Popoola D, et al. An internet-delivered handwashing intervention to modify influenza-like illness and respiratory infection transmission (PRIMIT): a primary care randomised trial. Lancet. 2015;386(10004):1631–9.
Kim HS, Ko RE, Ji M, Lee J-H, Lee C-S, Lee H. The usefulness of hand washing during field training to prevent acute respiratory illness in a military training facility. Medicine. 2018;97(30).
Merk H, Kühlmann-Berenzon S, Linde A, Nyrén O. Associations of hand-washing frequency with incidence of acute respiratory tract infection and influenza-like illness in adults: a population-based study in Sweden. BMC Infect Dis. 2014;14(1):509.
Acknowledgments
The authors are grateful for study participants, University of Gondar, supervisors and data collectors.
Funding
No funding agent.
Author information
Authors and Affiliations
Contributions
HD (MSc), ZA (MSc), BD (MSc) and AAT (MPH) involved in the proposal development, analysis, and write-up. HD participated in statistical analysis and manuscript preparation. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Ethical Review Committee of Environmental and Occupational Health and Safety department, the University of Gondar with ethical approval number EOHS/815/2011. After explaining the purpose of the study, written consent was obtained from mothers of under-five years’ children. Mothers gave permission for their children to participate in the study. Any potential identifiers were eliminated to ascertain confidentiality.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dagne, H., Andualem, Z., Dagnew, B. et al. Acute respiratory infection and its associated factors among children under-five years attending pediatrics ward at University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia: institution-based cross-sectional study. BMC Pediatr 20, 93 (2020). https://doi.org/10.1186/s12887-020-1997-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-020-1997-2