Abstract
Background
Low cardiac output syndrome (LCOS) is an important complication of cardiac surgery. It is associated with increased morbidity and mortality. The incidence of LCOS after surgery is high in patients with congenital heart disease (CHD). Therefore, determining the risk factors of LCOS has clinical significance for the management of CHD. This study aimed to analyze the risk factors of LCOS.
Methods
We conducted a retrospective analysis of children with CHD who underwent cardiac surgery at Shanghai Children’s Medical Center between January 1, 2014, and December 31, 2017. Demographic characteristics and baseline data were extracted from the health data resource center of the hospital, which integrates clinical routine data including medical records, diagnoses, orders, surgeries, laboratory tests, imaging, nursing, and other subsystems. Logistic regressions were performed to analyze the risk factors of LCOS.
Results
Overall, 8660 infants with CHD were included, and 864 (9.98%) had LCOS after surgery. The multivariate regression analysis identified that age (OR 0.992, 95% CI: 0.988–0.997, p = 0.001), tricuspid regurgitation (1.192, 1.072–1.326, p = 0.001), Risk Adjustment in Congenital Heart Surgery-1 risk grade (1.166, 1.011–1.345, p = 0.035), aortic shunt (left-to-right: 1.37, 1.005–1.867, p = 0.046; bi-directional: 1.716, 1.138–2.587, p = 0.01), atrial shunt (left-to-right: 1.407, 1.097–1.805, p = 0.007; right-to-left: 3.168, 1.944–5.163, p < 0.001; bi-directional: 1.87, 1.389–2.519, p < 0.001), ventricular level shunt (left-to-right: 0.676, 0.486–0.94, p = 0.02; bi-directional: 2.09, 1.611–2.712, p < 0.001), residual shunt (3.489, 1.502–8.105, p = 0.004), left ventricular outflow tract obstruction (3.934, 1.673–9.254, p = 0.002), right ventricular outflow tract obstruction (3.638, 1.225–10.798, p = 0.02), circulating temperature (mild hypothermia: 1.526, 95% CI: 1.205–1.934, p < 0.001; middle and low temperature: 1.738, 1.236–2.443, p = 0.001), duration of cardiopulmonary bypass (1.009, 1.006–1.012, p < 0.001), myocardial preservation using histidine-tryptophan-ketoglutarate (1.677, 1.298–2.167, p < 0.001), and mitral insufficiency (1.714, 1.239–2.37, p < 0.001) were independent risk predictors of LCOS.
Conclusions
The incidence of postoperative LCOS in CHD children remains high. Circulation temperature, myocardial preservation using histidine-tryptophan-ketoglutarate, and usage of residual shunt after surgery were independent risk predictors for LCOS.
Similar content being viewed by others
Background
Low cardiac output syndrome (LCOS) is the most common complication following cardiac surgeries. The incidence of LCOS in the surgical treatment of congenital heart disease (CHD) has been reported to be 25–60% [1], associated with a significant risk of mortality among patients [2, 3]. LCOS is associated with a decreased ejection fraction and decreased oxygen supply, which may cause hypoxia. The patients are often at a high risk of mortality and require more intensive care such as extended stay in the intensive care unit (ICU) and ventilatory support.
The etiology of postoperative LCOS is multifactorial [4]. Pathologically, endothelial dysfunction and myocardial stunning, acute changes in the loading conditions of the myocardium, use of cardioplegia, activation of the inflammatory and complement cascade caused by cardiopulmonary bypass (CPB), and the residual hemodynamic burden of uncorrected defects [5] have been suggested to be the causes of LCOS. The most commonly reported clinical predictors of LCOS include left ventricular ejection fraction < 20%, surgical history, female gender, and increasing age [2, 6, 7]. Prediction models based on clinical data, such as EuroSCORE, have been proposed [8]. However, the risk factors of LCOS are varied in the literature according to the population and surgery categories included [2, 9,10,11].
To date, only a few studies presented the detailed analysis of the risk factors for postoperative LCOS and the further complications in children with CHD. This study aimed to analyze the risk factors for LCOS and to determine their association with the incidence of postoperative death, extended ICU stay, and the duration of mechanical ventilator support in Chinese children with and without LCOS.
Methods
Study design and population
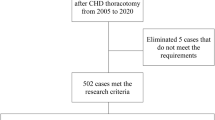
In this retrospective study, patients with CHD who underwent cardiac surgery at Shanghai Children’s Medical Center from January 1, 2014, to December 31, 2017, were included. Patients aged ≥18 years, on CPB, who had undergone general thoracic surgery not involving cardiotomy, or with uncertain in-hospital survival records were excluded from the study. The study was approved by the Ethical Committee of Shanghai Children’s Medical Center. Demographic characteristics and baseline data were extracted from the health data resource center of the hospital, which integrated clinical routine data including medical records, diagnoses, orders, operations, laboratory tests, imaging, nursing, and other subsystems.
Patients were classified into two groups, based on whether they developed LCOS into the LCOS and non-LCOS groups. The baseline characteristics and intraoperative features of the two groups were compared. Associations of these characteristics with LCOS were analyzed using regression analysis. In addition, the mortality, extended ICU stay, and duration of mechanical ventilator support were compared between the two groups.
Outcomes
LCOS is characterized by clinical signs or symptoms including elevated blood lactate or rapid increase in blood lactate, decreased central venous oxygen saturation, increased arterial to central venous oxygen saturation difference, decreased urine output, increased peripheral skin temperature to core body temperature difference, and low echocardiographic Doppler-derived cardiac index, high inotrope requirement [12]. In-hospital mortality was defined as death during the same hospitalization regardless of cause. Prolonged ICU stay was defined as > 3 days of ICU stay, and extended duration of mechanical ventilation support was defined as > 48 h’ ventilatory support [13].
Risk factors
The risk factors of LCOS analyzed in this study include baseline and demographic data, pre-operative Doppler echocardiography characteristics, characteristics of surgery and CPB, as well as postoperative measures of CHD. The body mass index (BMI), as categorical data percentiles varied according to age groups, which were age-adjusted according to the pediatric BMI reference data for China [14]. Moreover, the Risk Adjustment in Congenital Heart Surgery-1 (RACHS-1) score was defined as ordinal data; an increase in the RACHS-1 score can indicate the risk of LCOS [15]. Nutrition status has been recognized as an important risk factor of postoperative complications in CHD surgery. In this study, the incidences of LCOS in CHD children with different nutrition status were analyzed separately.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation (SD) (normally distributed) or median (IQR) (non-normally distributed). Categorical variables are presented as frequency (%). Depending on the distributions, the t-test or Mann-Whitney U test was used to compare the continuous variables between the groups. In addition, a chi-squared test or Fisher’s exact test was used for the comparison of categorical variables.
Univariate logistic regressions with LCOS as an outcome were analyzed first. Then, the Variance Inflation Factor was calculated to explore the independence of the selected variables. The results are listed in Supplemental Table 1, and there is no evidence to show dependence among the selected factors. Therefore, the significant variables were entered into multiple logistic regressions without an interaction term, and the stepwise variable selection method was used to identify the potential risk factors of LCOS. All tests were two-sided, and P < 0.05 was considered as statistically significant. All analyses were performed using SAS software, version 9.4 (SAS Institute INC).
Results
Demographic characteristics of CHD children
Overall, 8660 children were included in the study, with 864 (9.98%) LCOS cases after surgery. The demographic characteristics at baseline including age (p < 0.001) and body mass index (BMI) <5th percentile (p = 0.016) were significantly different between the CHD children with LCOS and those without LCOS (Table 1).
Preoperative Doppler echocardiography characteristics of CHD children
When Doppler echocardiography characteristics were compared between the CHD children in the two groups, it was found that aortic shunt (p < 0.001), atrial shunt (p < 0.001), ventricular level shunt (p < 0.001), aortic insufficiency (p = 0.035), pulmonary insufficiency (p = 0.007), tricuspid regurgitation (TR) (p = 0.001), and mitral insufficiency (p = 0.044) of LCOS patients were significantly different from those of non-LCOS patients (Table 1).
Characteristics of surgery and cardiopulmonary bypass of CHD children
In LCOS patients, operation characteristics (p < 0.001), procedure complexity (represented by RACHS-1 risk grade) (p < 0.001), CPB duration (p < 0.001), aortic clamping time (< 0.001), history of heart surgery (p < 0.001), circulating temperature (p < 0.001), circulation method (< 0.001), and myocardial preservation (p < 0.001) were significantly different from those without LCOS (Table 1).
Postoperative measures of CHD children
There were significant differences in postoperative residual shunt (p < 0.001), left ventricular outflow tract obstruction (LVOTO, p < 0.001), right ventricular outflow tract obstruction (RVOTO, p < 0.001), and postoperative rhythm of the heart (p < 0.001) between LCOS and non-LCOS patients (Table 1).
Logistic regression analysis
Univariate analysis identified that age, aortic insufficiency, pulmonary insufficiency, TR, RACHS-1 risk grade, aortic shunt, atrial shunt, ventricular level shunt, emergency extracorporeal surgery, history of heart surgery, residual shunt, LVOTO, RVOTO, abnormal circulation temperature, circulation method (except for parallel CPB and cardio-cerebral perfusion), duration of CPB, aortic clamping time, postoperative rhythm of the heart (III°AVB, II°AVB), difficult to wean from CPB, myocardial preservation using histidine-tryptophan-ketoglutarate (HTK), BMI <5th percentile, and mitral insufficiency were significantly associated with LCOS in CHD children (Table 2).
Multivariate analysis of these variables found age (OR 0.992, 95% CI: 0.988–0.997, p = 0.001), TR (OR 1.192, 95% CI 1.072–1.326, p = 0.001), RACHS-1 risk grade (OR 1.166, 95% CI 1.011–1.345, p = 0.035), aortic shunt (left-to-right: OR 1.37, 95% CI 1.005–1.867, p = 0.046; bi-directional: OR 1.716, 95% CI 1.138–2.587, p = 0.01), atrial shunt (left-to-right: OR 1.407, 95% CI 1.097–1.805, p = 0.007; right-to-left: OR 3.168, 95% CI 1.944–5.163, p < 0.001; bi-directional: OR 1.87, 95% CI 1.389–2.519, p < 0.001), ventricular level shunt (left-to-right: OR 0.676, 95% CI 0.486–0.94, p = 0.02; bi-directional: OR 2.09, 95% CI 1.611–2.712, p < 0.001), residual shunt (OR 3.489, 95% CI 1.502–8.105, p = 0.004), LVOTO (OR 3.934, 95% CI 1.673–9.254, p = 0.002), RVOTO (OR 3.638, 95% CI 1.225–10.798, p = 0.02), circulating temperature (mild hypothermia: OR 1.526, 95% CI 1.205–1.934, p < 0.001; middle and low temperature: OR 1. 738, 95% CI 1.236–2.443, p = 0.001), duration of CPB (OR 1.009, 95% CI 1.006–1.012, p < 0.001), myocardial preservation using HTK (OR 1.677, 95% CI 1.298–2.167, p < 0.001), and mitral insufficiency (OR 1.714, 95% CI 1.239–2.37, p < 0.001) were independent risk predictors of LCOS (Table 2).
Postoperative mortality, prolonged ICU stay, and extended medical ventilator support in LCOS and non-LCOS CHD children
The mortality rate (7.18% vs. 1.08%, p < 0.001), ICU stay > 3 days (89.24% vs. 33.35%, p < 0.001), and duration of mechanical ventilator support > 48 h (93.21% vs. 44.5%, p < 0.001) of LCOS children were significantly higher than those of non-LCOS children (Table 3).
Incidence of postoperative LCOS in children with CHD of different nutritional status
In CHD children with BMI <5th percentile, the incidences of LCOS showed a gradually decreasing trend in neonates aged > 3 months. In neonates aged 3–6 months, the incidence increased, declined in children aged 6 months to > 3 years old. In patients with BMI 5th~95th percentile and > 95th percentile, the incidences of LCOS showed a gradually decreasing trend. (Table 4).
Discussion
In our study, the incidence of LCOS was 9.98%, which is higher than that in adult patients postoperatively (2.4–9.1%) [2, 3, 7], but lower than that of another study on newborns, in which the LCOS incidence at 36 h after surgery was 25.9, 17.5, and 11.7% of infants (median age, 3 months) on placebo, low-dose milrinone, and high-dose milrinone, respectively [16]. In a secondary retrospective analysis of a prospective randomized trial, LCOS occurred in 32 of 76 (42%) neonates (median age, 7 days) after cardiac surgery [17]. This difference was attributed to the probable difference in age. Neonatal myocardium is physiologically immature [18,19,20,21] and every procedure affects the incidence of LCOS differently [22]. The age range of children included in this study was larger (1–6457 days), and we included different types of cardiac surgery. This could be the main reason why the LCOS incidence was higher than that in adults and lower than that in newborns.
We found that age, aortic shunt (left-to-right and bi-directional), atrial shunt, ventricular level shunt (left-to-right and bi-directional), circulation temperature, and myocardial preservation using HTK were independent predictors of LCOS.
The risk for LCOS was higher for neonates given that their myocardial development is not complete. The effect of age on the risk of LCOS in adults has been confirmed earlier. In a prospective study, multivariate analysis showed that age was an independent predictor of LCOS [9] and a retrospective study ascertained that increasing age is an independent predictor of LCOS [2].
By preoperative Doppler echocardiography characteristics of CHD children, aortic shunt (left-to-right and bi-directional), atrial shunt, ventricular level shunt (left-to-right and bi-directional) were deduced as significant risk factors for LCOS. Left-to-right shunt before surgery may result in right heart failure, leading to low cardiac output. Xiong et al. found that preoperative right-left shunt ventricular septal defect was a risk factor of LCOS [23]. Ischemic mitral valve pathology was found as an independent predictor for LCOS after isolated mitral valve surgery [3].
We also found that the circulation temperature (mild hypothermia, middle and low temperature) and the proportion of myocardium preserved using HTK were independent predictors of LCOS. During routine hypothermic CPB, the heart is damaged by hypothermia, ischemia-reperfusion, or hyperkalemia, which is associated with an excess risk of postoperative LCOS and severe arrhythmia [24]. Yau et al. found that during hypothermic CPB, the myocardium acquires energy through anaerobic metabolism, leading to the accumulation of lactic acid. After reperfusion, aerobic metabolism cannot be resumed immediately in cardiomyocytes owing to low temperature, but still anaerobic metabolism can occur for a short period. Whereas, patients with mild hypothermia CPB are less affected [25]. The study found that the inflammatory response mediated by CPB caused pulmonary vascular endothelial damage, which changed the pulmonary vascular reactivity. These cause excessive thromboxane production and reduced endogenous nitric oxide production, which can lead to pulmonary vasoconstriction and formation of pulmonary microthrombus. Further, these changes could induce pulmonary vascular resistance, which increases after CPB [26]. Then, the right ventricular afterload increases, which is significantly associated with right ventricular dysfunction and LCOS.
Obesity or high BMI is a common factor associated with poor prognosis. A propensity score-matched analysis found that obese (BMI, ≥30 kg/m2) patients who underwent surgery for type A acute aortic dissection had higher postoperative mortality rates. Moreover, a previous report stated that obesity was significantly associated with increased risk of LCOS and other postoperative morbidities [27]. However, in our study, there was no significant correlation between BMI and LCOS risk after cardiac surgery in CHD children. This correlation is different from the results of the abovementioned study on adults and we ascertain that the ‘obesity paradox’ may explain this inconsistency. The BMI of the CHD children in our study may be lower than that of the general population, and the patients with BMI > P95 percentile did not have such high obesity levels.
LCOS is associated with significantly high morbidity and mortality. In our study, the mortality rate (7.18% vs. 1.08%, p < 0.001), ICU stay > 3 days (89.24% vs. 33.35%, p < 0.001) and the duration of mechanical ventilator support > 48 h (93.21% vs. 44.5%, p < 0.001) were significantly higher in LCOS children compared to those without LCOS. A previous study showed that LCOS was associated with significantly high morbidity and mortality in adults [3].
Therefore, cardiac surgery can cause LCOS in children with CHD and result in poorer postsurgical outcomes. In the current study, we confirmed the impact of LCOS on postoperative clinical outcomes in CHD children.
Limitations
This study had certain limitations. First, this is a retrospective study; the correlations may not confirm a causal relationship between the risk factors and LCOS. Second, we included patients from a single center only; hence, the application of these findings on other populations and institutions need to be reproduced in further large-scale multi-center studies. Since this is a single-center study, the impact of surgery outcomes and hospitalizations from other centers was not considered.
Conclusion
In conclusion, our study provides clinically significant evidence to indicate a significant association of LCOS with postoperative clinical outcomes (including mortality, prolonged ICU stay, and extended mechanical ventilator support) in children with CHD. Circulation temperature, myocardial preservation using HTK, and usage of residual shunt after surgery were independent risk predictors for LCOS. Further multi-center studies toned to be conducted with a larger sample size to confirm our study results.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are not publicly available due to the hospital regulation.
Abbreviations
- BMI:
-
Body mass index
- CHD:
-
Congenital heart disease
- CPB:
-
Cardiopulmonary bypass
- HTK:
-
Histidine-tryptophan-ketoglutarate
- ICU:
-
Intensive care unit
- LCOS:
-
Low cardiac output syndrome
- LVEF:
-
Left ventricular ejection fraction
- LVFS:
-
Left ventricular fractional shortening
- LVOTO:
-
Left ventricular outflow tract obstruction
- MR:
-
Mitral regurgitation
- RACHS-1:
-
Risk Adjustment in Congenital Heart Surgery-1
- RVOTO:
-
Right ventricular outflow tract obstruction
- TR:
-
Tricuspid regurgitation
References
Yuerek M, Rossano JW, Mascio CE, Shaddy RE. Postoperative management of heart failure in pediatric patients. Expert Rev Cardiovasc Ther. 2016;14(2):201–15.
Maganti MD, Rao V, Borger MA, Ivanov J, David TE. Predictors of low cardiac output syndrome after isolated aortic valve surgery. Circulation. 2005;112(9 Suppl):I448–52.
Maganti M, Badiwala M, Sheikh A, Scully H, Feindel C, David TE, Rao V. Predictors of low cardiac output syndrome after isolated mitral valve surgery. J Thorac Cardiovasc Surg. 2010;140(4):790–6.
Masse L, Antonacci M. Low cardiac output syndrome: identification and management. Crit Care Nurs Clin North Am. 2005;17(4):375–83 x.
Hoffman TM, Wernovsky G, Atz AM, Bailey JM, Akbary A, Kocsis JF, Nelson DP, Chang AC, Kulik TJ, Spray TL, et al. Prophylactic intravenous use of milrinone after cardiac operation in pediatrics (PRIMACORP) study. Prophylactic intravenous use of Milrinone after cardiac operation in pediatrics. Am Heart J. 2002;143(1):15–21.
Rao V, Ivanov J, Weisel RD, Ikonomidis JS, Christakis GT, David TE. Predictors of low cardiac output syndrome after coronary artery bypass. J Thorac Cardiovasc Surg. 1996;112(1):38–51.
Algarni KD, Maganti M, Yau TM. Predictors of low cardiac output syndrome after isolated coronary artery bypass surgery: trends over 20 years. Ann Thorac Surg. 2011;92(5):1678–84.
Nashef SA, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR, Lockowandt U. EuroSCORE II. Eur J Cardio-Thorac Surg. 2012;41(4):734–44 discussion 744-735.
Balderas-Munoz K, Rodriguez-Zanella H, Fritche-Salazar JF, Avila-Vanzzini N, Juarez Orozco LE, Arias-Godinez JA, Calvillo-Arguelles O, Rivera-Peralta S, Sauza-Sosa JC, Ruiz-Esparza ME, et al. Improving risk assessment for post-surgical low cardiac output syndrome in patients without severely reduced ejection fraction undergoing open aortic valve replacement. The role of global longitudinal strain and right ventricular free wall strain. Int J Cardiovascular Imaging. 2017;33(10):1483–9.
Ding W, Ji Q, Shi Y, Ma R. Predictors of low cardiac output syndrome after isolated coronary artery bypass grafting. Int Heart J. 2015;56(2):144–9.
Sa MP, Nogueira JR, Ferraz PE, Figueiredo OJ, Cavalcante WC, Cavalcante TC, Silva HT, Santos CA, Lima RO, Vasconcelos FP, et al. Risk factors for low cardiac output syndrome after coronary artery bypass grafting surgery. Revista brasileira de cirurgia cardiovascular : orgao oficial da Sociedade Brasileira de Cirurgia Cardiovascular. 2012;27(2):217–23.
Burkhardt BE, Rucker G, Stiller B. Prophylactic milrinone for the prevention of low cardiac output syndrome and mortality in children undergoing surgery for congenital heart disease. Cochrane Database Syst Rev. 2015;3:Cd009515.
Qu J, Liang H, Zhou N, Li L, Wang Y, Li J, Cui Y. Perioperative NT-proBNP level: potential prognostic markers in children undergoing congenital heart disease surgery. J Thorac Cardiovasc Surg. 2017;154(2):631–40.
Li H, Ji C, Zong X, Zhang Y. Body mass index growth curves for Chinese children and adolescents aged 0 to 18 years. Zhonghua Er Ke Za Zhi. 2009;47(7):493–8.
Cavalcante CT, de NMG S, Júnior PVC, Branco KM, Pompeu RG, Teles AC, Cavalcante RC, de Andrade GV. Analysis of Surgical Mortality for Congenital Heart Defects Using RACHS-1Risk Score in a Brazilian Single Center. Brazilian J Cardiovascular Surg. 2016;30(3):1 219–225.
Hoffman TM, Wernovsky G, Atz AM, Kulik TJ, Nelson DP, Chang AC, Bailey JM, Akbary A, Kocsis JF, Kaczmarek R, et al. Efficacy and safety of milrinone in preventing low cardiac output syndrome in infants and children after corrective surgery for congenital heart disease. Circulation. 2003;107(7):996–1002.
Butts RJ, Scheurer MA, Atz AM, Zyblewski SC, Hulsey TC, Bradley SM, Graham EM. Comparison of maximum vasoactive inotropic score and low cardiac output syndrome as markers of early postoperative outcomes after neonatal cardiac surgery. Pediatr Cardiol. 2012;33(4):633–8.
Balaguru D, Haddock PS, Puglisi JL, Bers DM, Coetzee WA, Artman M. Role of the sarcoplasmic reticulum in contraction and relaxation of immature rabbit ventricular myocytes. J Mol Cell Cardiol. 1997;29(10):2747–57.
Hatem SN, Sweeten T, Vetter V, Morad M. Evidence for presence of Ca2+ channel-gated Ca2+ stores in neonatal human atrial myocytes. Am J Phys. 1995;268(3 Pt 2):H1195–201.
Maylie JG. Excitation-contraction coupling in neonatal and adult myocardium of cat. Am J Phys. 1982;242(5):H834–43.
Nassar R, Reedy MC, Anderson PA. Developmental changes in the ultrastructure and sarcomere shortening of the isolated rabbit ventricular myocyte. Circ Res. 1987;61(3):465–83.
Lomivorotov VV, Efremov SM, Kirov MY, Fominskiy EV, Karaskov AM. Low-cardiac-output syndrome after cardiac surgery. J Cardiothorac Vasc Anesth. 2017;31(1):291–308.
LQ-s XIONG H-h, Xiao-hua XU, et al. Studying the velocities and timings across the Large VSD to predict the surgery effect of tetralogy of fallot by color M-mode and color flow Imaging. cta Academiae Medicinae Jiangxi. 2008;48(4):65–70.
Warner KG, Khuri SF, Kloner RA, Josa M, Dalecki-Chipperfield KM, Butler MD, Assousa SN, Lee SS, Barsamian EM, Seiler M. Structural and metabolic correlates of cell injury in the hypertrophied myocardium during valve replacement. J Thorac Cardiovasc Surg. 1987;93(5):741–54.
Yau TM, Ikonomidis JS, Weisel RD, Mickle DA, Ivanov J, Mohabeer MK, Tumiati L, Carson S, Liu P. Ventricular function after normothermic versus hypothermic cardioplegia. J Thorac Cardiovasc Surg. 1993;105(5):833–43 discussion 843-834.
Lam CF, Peterson TE, Croatt AJ, Nath KA, Katusic ZS. Functional adaptation and remodeling of pulmonary artery in flow-induced pulmonary hypertension. Am J Phys Heart Circ Phys. 2005;289(6):H2334–41.
Lio A, Bovio E, Nicolò F, Saitto G, Scafuri A, Bassano C, Chiariello L, Ruvolo G: Influence of Body Mass Index on Outcomes of Patients Undergoing Surgery for Acute Aortic Dissection: A Propensity-Matched Analysis. Tex Heart Inst J 2019;46(1):\–13.
Acknowledgments
Extremely grateful to all the staff who contributed to the study. Thankful to Shanghai Synyi Medical Technology Co., Ltd. for providing the data analysis and statistical platform.
Funding
The research was funded by the Fund of Shanghai Jiao Tong University (No: YG2015QN23).
Author information
Authors and Affiliations
Contributions
XD acquired the data, implemented the research, revised the article, and approved the final version of the manuscript for publication. HC was responsible for data acquisition, data cleaning, analysis and interpretation of data, and finalizing the manuscript for publication. XS was responsible for data review, data analysis, manuscript revision, and finalizing the manuscript for publication. SW was responsible for supervision of the project execution (ensuring the accuracy or integrity of any part of the work), acquisition of data, data analysis and interpretation, approving the final version of the manuscript to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. ZH was responsible for analysis and interpretation of data, drafting the article, and approving the final manuscript to be published. LY was responsible for the statistical analysis of the research data, revising the article, and approving the final manuscript to be published. ZL was responsible for the determination of the research direction, the design of the research program, summarizing the research questions, analysis, data interpretation, final approval of the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The author(s) read and approved the final manuscript
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our retrospective study is in accordance with the ethical principles of the “Declaration of Helsinki” and the “International Ethical Guidelines for Biomedical Research Involving Human Subjects” enforced by the Council for International Organizations of Medical Science. Therefore, the ethical committee of the hospital decided to exempt the study from informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:
Table S1. The Variance Inflation Factor of selected variables.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Du, X., Chen, H., Song, X. et al. Risk factors for low cardiac output syndrome in children with congenital heart disease undergoing cardiac surgery: a retrospective cohort study. BMC Pediatr 20, 87 (2020). https://doi.org/10.1186/s12887-020-1972-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-020-1972-y