Abstract
Background
The World Health Organization recommends that mothers should exclusively breastfeed their infants until 6 months of age due to the benefits for the mother and the child. There is documented evidence on exclusive breastfeeding from Ethiopia, but not specifically from Samara-Logia city administration. This study aimed to assess the factors associated with early termination of exclusive breastfeeding among mother-infant dyads in Samara-Logia, Ethiopia.
Methods
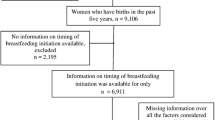
A cross-sectional study was conducted in March 2018. Data were collected on 484 randomly selected mother-infant dyads. The Kaplan Meier curve with the log-rank test was used to compare the survival difference. Cox regression models were used to identify the predictors of early termination of exclusive breastfeeding.
Results
The cumulative proportion of survival probability of exclusive breastfeeding to 6 months was 64.5%, with the median duration of 6 months. Mothers having partners with formal education [Adjusted hazard ratio (AHR): 0.58; 95% confidence interval (CI): 0.39, 0.85], receiving counseling on exclusive breastfeeding at antenatal check-up [AHR: 0.62; 95% CI: 0.43, 0.91], giving birth in a health institution [AHR: 0.50; 95% CI: 0.28, 0.88], initiating breastfeeding within the first hour [AHR: 0.41; 95% CI: 0.24, 0.68], and perceiving breast milk adequate for the first 6 months [AHR: 0.17; 95% CI: 0.12, 0.25] were associated with lower hazard of discontinuing exclusive breastfeeding before 6 months.
Conclusion
This study showed that the cumulative proportion of survival probability on exclusive breastfeeding was low in Samara-Logia city administration. Educating husbands to support their partners, strengthening infant feeding counseling, promoting institutional delivery, educating women about the benefit of early initiation of breastfeeding, and expanding urban health extension program are important to improve the duration of exclusive breastfeeding in Ethiopia.
Similar content being viewed by others
Background
Breastfeeding provides young infants with the nutrients for growth, development, and health [1]. Human milk is uniquely suited to the infant, both in its nutritional composition and in the non-nutritive bioactive factors, which include cells, anti-infectious, and anti-inflammatory agents and growth factors that promote child survival and healthy child development [2].
International organizations such as the United Nations International Children’s Emergency Fund (UNICEF) and the World Health Organization (WHO) recommend infants should be exclusively breastfed in the first 6 months, and thereafter be given nutritious complementary foods coupled with continued breastfeeding up to the age of 2 years or beyond [3]. Exclusive breastfeeding (EBF) is an infant’s breast milk consumption without supplementation of any type of foods and/or drinks (including water), except for vitamins, minerals and necessary medications up to the age of 6 months [1].
EBF is adequate in quality as well as quantity in terms of the nutrients required by the baby [4]. It eliminates contamination which makes it especially important in resource-poor setting communities [5]. Lack of EBF is associated with infant and childhood morbidity and mortality including lifelong impact on school performance, productivity, and intellectual development [6], and overall health during adolescence and adulthood [7]. Hence, breastfeeding in general, EBF in particular, is among the best interventions in the first 1000 days [8, 9].
Globally, about 40% of infants received exclusively breastfeeding in the first 6 months [10]. In Ethiopia, breastfeeding is nearly universal; about 97% of children are ever breastfeed. However, 58% of infants receive breast milk exclusively with a median duration of 3.1 months. This is lower than the health sector transformation plan of Ethiopia [11], and international recommendations [12].
The government of Ethiopia emphasizes on EBF and has declared ‘the annual exclusive breastfeeding day’ [13]. The health extension program aims at improving proper infant and young child nutrition, for instance, the promotion of EBF in Ethiopia [14]. Besides, nongovernmental organizations are working towards the improvement of optimal breastfeeding in the country [15].
In Ethiopia, particularly in Samara-Logia, there is no adequate evidence on the factors associated with early termination of EBF. Furthermore, health information on child feeding practices is limited among pastoral communities. Therefore, this study aimed to investigate the predictors of EBF duration in Samara-Logia city administration, Afar National Regional State, Ethiopia.
Methods
Study setting
A cross-sectional study was employed, in March 2018, on mothers of infants aged 6 up to 12 months in Samara-Logia city administration. The city administration is located at 574 km from Addis Ababa (the capital of Ethiopia). Evidence from Afar National Regional State Health Bureau showed that 57, 285 total population of Samara-Logia. Of which about 13,079 are women in reproductive age group, with 6530 are children aged less than 5 years, and 797 are infants aged 6 to 12 months. There are 13 ketenas (the smallest administrative units next to kebele) in the city administration. There are also two health centers and 13 private clinics.
Sample size determination
A total of 484 study participants were determined using Open Epi Version 2.3, having the following assumptions: 77.1 and 65.2% magnitude of EBF among women who initiated breastfeeding within the first hour and after the first hour of birth, respectively [14]. Two-sided significance level was set to 95%, power as 80%, and the ratio of sample size (Unexposed/Exposed) =1.
Sampling procedure and study participants
First, Samara-Logia was purposively selected since there is no evidence on the duration of EBF. Second, all 13 ketenas were included in the study. Thirdly, the total number of study participants was proportionally allocated to all ketenas. Then, simple random sampling was used to select the study participants using a health extension logbook as a sampling frame. However, infants whose mothers were unable to speak, and infants living with non-biological mothers were excluded from the study.
Data collection process and instrument
Data were collected using an interviewer-administered questionnaire. First, it was developed in English from the Ethiopia demographic and health survey (EDHS) [16] and other literatures [17,18,19,20]. Then, the questionnaire was pretested in Dubti town, and the findings were incorporated into the final questionnaire. The final English version of the questionnaire is provided as “Additional file 1” with this article. Finally, the Amharic version was used to collect the data. Six diploma holders in nursing and two public health professionals were recruited as data collectors and supervisors, respectively. Two days training on the data collection procedures was given to data collectors and supervisors.
Study variables
The outcome variable was the duration of EBF in a month. It was assessed using a ‘since birth’ recall approach. Study participants were asked “What was the age (in months) of this baby (“Name”) when you first tried semi-solids or solids or liquids (including water) other than your breast milk?” Then, mothers who exclusively breastfeed their infants to less than 6 months were considered as “events” and those who feed infants to 6 months and beyond were “censored”.
The independent variables were: socio-demographic variables (maternal age, educational status, occupational status, religion, ethnicity, marital status, birth order, number of children, family size, infant’s gender, infant’s age, head of the household, family monthly income), maternal and infant health service-related variables (antenatal check-up (ANC), place and mode of delivery, postnatal check-up (PNC), infant feeding advice at ANC and PNC check-ups, source of information on breastfeeding); and infant feeding (early initiation of breastfeeding, prelacteal feeding, colostrum discarding, bottle feeding, and perceived adequacy of breast milk).
Data management and analysis
Data were entered using Epi data version 3.02 and exported to SPSS version 20 for statistical analysis. Model fitness was checked by the proportionality hazard assumption test using log (−log) versus log (time) graph and time-dependent Cox model. In both tests, the model was fulfilled.
Descriptive statistics were used to describe the study variables. The Kaplan-Meier survival curve with a log-rank test was used to compare the survival of infants on EBF. The univariable Cox regression model was used to assess the effect of each independent variable on the duration of EBF. Then, variables with p-value < 0.25 in the univariable model were included in the final model. In both models, p-value < 0.05 was used to declare statistical significance.
Results
Characteristics of the study participants
A total of 465 mother-infant dyads participated in the study (the response rate was 96.07%). The mean (+Standard deviation (SD)) of maternal age was 27.72 (+ 4.46) years. Three hundred sixty-two (77.8%) of the respondents were aged less than 30 years, and 411(88.4%) were Muslims by religion. Three hundred seven (66%) were Afar by ethnicity (Table 1).
Maternal and infant health service utilization
Four hundred sixty (98.9%) of the study mothers had attended at least one antenatal (ANC) check-up. Of mothers who had received ANC check-up, about 29% had received counseling on infant feeding (Table 2).
Infant feeding practices
Four hundred sixty-four (99.8%) of the respondents had breastfed their infants at any point in time, with about 87.7% (n = 407) initiated breastfeeding within the first hour of birth. Three hundred ninety-one mothers (84.1%) believed that breastfeeding is enough for the first 6 months (Table 3). The cumulative survival probability of EBF to 6 months was 64.5%, with a median duration of 6 months. In addition, the range of EBF duration was from 0 to 6 months, respectively (Table 4).
Factors affecting the duration of exclusive breastfeeding
Kaplan-Meier curve showed that women’s perceived adequacy of breast milk significantly affected the duration of EBF. The survival curve of women who perceived adequacy of their breast milk was constantly above the survival curve of the other group (log-rank test, p < 0.001) (Fig. 1). Women who gave birth in a health institution were more likely to exclusively breastfeed their infants to 6 months as compared to those who gave birth at home (log-rank test, p < 0.05) (Fig. 2). The survival probability of EBF was significantly higher among women who had received infant feeding counseling at ANC check-up as compared to those who had deprived of counseling (log-rank test, p < 0.05) (Fig. 3).
Univariable Cox regression analysis showed that maternal education, maternal occupation, partner’s education, infant feeding counseling at ANC check-up, attending postnatal check-up (PNC), early initiation of breastfeeding, perceived adequacy of breast milk, mode of delivery, place of delivery, and colostrum avoidance were significant at p < 0.25. In the multivariable Cox regression model partner’s education, infant feeding counseling at ANC check-up, place of delivery, early initiation of breastfeeding, and perceived adequacy of breastmilk were statistically significant at p < 0.05 (Table 5).
Women whose partners had attended formal education were less likely to discontinue EBF before 6 months as compared to those without formal education [AHR: 0.58; 95% CI: 0.39, 0.85]. Infant feeding counseling at ANC check-up was positively associated with EBF duration. Mothers who received counseling on infant feeding at ANC check-up were less likely to discontinue EBF before 6 months as compared to those who did not receive counseling [AHR: 0.62; 95% CI:0.43, 0.91].
Mothers who gave birth in a health institution were less likely to terminate EBF before 6 months as compared to those who gave birth at home [AHR: 0.50; 95% CI:0.28, 0.88]. Women who initiated breastfeeding within the first hour of birth were less likely to cease EBF as compared to those who had initiated lately [AHR: 0.41; 95% CI: 0.24, 0.68]. Women who reported adequacy of their milk were less likely to terminate EBF early as compared to those who perceived inadequate [AHR: 0.17, 95% CI: 0.12, 0.25] (Table 5).
Discussion
This study revealed that the median duration of EBF was 6 months which is similar to the international recommendation [3]. The cumulative survival probability of EBF to 4 months and 6 months was declined by 13 and 20%, respectively, from birth. In Ethiopia, traditional postpartum care is given at home by their family members in the first 6 to 12 weeks after delivery [21]. This condition increases the likelihood of mothers and infants to stay together at home which might decrease the hazard of early termination of EBF. In addition, the current study showed that the cumulative survival probability of EBF to 6 months was 64.5%. This finding is lower than the findings from previously conducted studies in Ethiopia [22,23,24]. This difference may be due to the age of the study participants.
In this study, partner educational status significantly affected the duration of EBF. Women whose partners had attended formal education were at lower hazard of terminating EBF as compared to those who had no formal education. This may be partners without formal education might enforce their wives to give additional foods early as compared to those with formal education. Similar findings were found in Gondar town where women who receive social support were more likely to practice EBF as compared to those without support [13]. This is also consistent with the finding in Australia [25, 26].
This study revealed that counseling on infant feeding at ANC check-up was significantly associated with the duration of EBF. Women who received counseling on infant feeding at ANC check-up were less likely to terminate EBF compared to those who did not receive counseling. This finding is consistent with the previous studies in Ethiopia [18, 19, 27], and Tanzania [28]. This shows that antenatal check-up is an appropriate time to provide essential messages about proper infant feeding practices. Furthermore, the initiation of an urban health extension program in Afar has a great contribution to the access of ANC services including breastfeeding counseling.
Women who delivered a baby in health facilities were less likely to cease EBF as compared to those who delivered a baby at home. Similar findings were reported from different parts of Ethiopia [29,30,31,32]. This may be explained in such a way that institutional delivery provides a favorable environment for the early initiation of breastfeeding. This is a key factor that could favor exclusive breastfeeding.
Furthermore, early initiation of breastfeeding was associated minimum hazard of EBF termination as compared to late initiation of breastfeeding. This finding is consistent with the previous Ethiopian studies [17, 20, 23, 27, 33]. This is because initiating breastfeeding within 1 h may lead to increased newborn-mother bonding and sufficient breast milk secretion. This may, in turn, lead to late initiation of additional foods other than breast milk.
Compared to women who perceived inadequacy of breast milk for the first 6 months, those who perceived adequate were less likely to cease EBF. In line with this finding, in the Gurage zone, mothers who perceived adequacy of breast milk were less likely to cease EBF earlier as compared to those who perceived inadequate [24].
The study could be subjected to recall bias. Besides, the study is conducted in the urban area, therefore, might not be a true reflection of the entire Afar community.
Conclusions
The cumulative survival probability of EBF to 6 months was 64.5%. Women whose partners had formal education, received counseling on infant feeding at ANC check-up, gave birth in a health institution, initiated breastfeeding early, and perceived breast milk adequate for the first 6 months were less likely to terminate EBF before 6 months. Therefore, health promotion interventions should be targeted at educating fathers and involve them in breastfeeding decisions. It is also important to encourage fathers to support their partners and participate in ANC check-ups. Furthermore, strengthening infant feeding counseling both at community and institution level, encouraging institutional delivery, and educating mothers about the importance of early initiation of breastfeeding is important to improve the duration of EBF in pastoralist communities of Ethiopia.
Availability of data and materials
The findings were declared from the available data sources. All possible required information is included in the manuscript. In addition, the data are available from the corresponding author.
Abbreviations
- AHR:
-
Adjusted hazard ratio
- ANC:
-
Antenatal check-up
- CI:
-
Confidence interval
- EBF:
-
Exclusive breastfeeding
- EDHS:
-
Ethiopia demographic and health survey
- PNC:
-
Postnatal check-up
- RERC:
-
Research Ethics Review Committee
- SD:
-
Standard deviation
- SPSS:
-
Statistical package for the social sciences
- UNICEF:
-
United Nations International Children’s Emergency Fund
- WHO:
-
World Health Organization
References
Saarinen UM, Kajosaari M. Breastfeeding as prophylaxis against atopic disease: prospective follow-up study until 17 years old. Lancet. 1995;346(8982):1065–9.
Oftedal OT. The evolution of milk secretion and its ancient origins. Animal. 2012;6(3):355–68.
Kramer MS, Kakuma R. The optimal duration of exclusive breastfeeding: a systematic review. Geneva: World Health Organization (WHO/NHD/01.08; WHO/FCH/01.23); 2001. Available at https://www.who.int/nutrition/publications/infantfeeding/WHO_NHD_01.08/en/
WHO. Nutrient adequacy of exclusive breastfeeding for the term infant during the first six months of life. Geneva; 2002. Available at http://whqlibdoc.who.int/publications/9241562110.pdf
Kathryn A, Dorothy J, et al. Cultural barriers to exclusive breastfeeding by mothers in a rural area of cameroon. Afr J Midwifery Womens Health. 2005;50:324–8.
Hall J. Effective community-based interventions to improve exclusive breast feeding at four to six months in low- and low–middle-income countries: a systematic review of randomized controlled trials. J Hall / Midwifery. 2011;27:Epub 502.
Infant and young child feeding practices: collecting and using data: a step-by-step guide, cooperative for assistance and relief everywhere Inc. (CARE). 2010. Available at http://nutritioncluster.net/wp-content/uploads/sites/4/2013/12/final-iycf-guide-iycf-practices_eng.pdf
Schwarzenberg SJ, Georgieff MK, AAP COMMITTEE ON NUTRITION. Advocacy for improving nutrition in the first 1000 days to support childhood development and adult health. Pediatrics. 2018;141(2):e20173716.
Moore TG, Arefadib N, Deery A, West S. The first thousand days: an evidence paper. Parkville: Centre for Community Child Health, Murdoch Children’s Research Institute; 2017. Available at https://www.rch.org.au/uploadedFiles/Main/Content/ccchdev/CCCH-The-First-Thousand-Days-An-Evidence-Paper-September-2017.pdf
UNICEF and WHO. Global breastfeeding scorecard: tracking progress for breastfeeding policies and programmes. 2017. Available at https://www.who.int/nutrition/publications/infantfeeding/global-bf-scorecard-2017.pdf
The Federal Democratic Republic of Ethiopia Ministry of Health. Health sector transformation plan: 2015/16–2019/20. 2015. Available at https://www.globalfinancingfacility.org/sites/gff_new/files/Ethiopia-health-system-transformation-plan.pdf
WHO. Implementation guidance: protecting, promoting and supporting Breastfeeding in facilities providing maternity and newborn services: the revised Baby-Friendly Hospital Initiative. Geneva; 2018. Available at https://www.who.int/nutrition/publications/infantfeeding/bfhi-implementation-2018.pdf
Chekol DA, Biks GA, Gelaw YA, Melsew YA. Exclusive breastfeeding and mothers’ employment status in Gondar town, Northwest Ethiopia: a comparative cross sectional study. Int Breastfeed J. 2017;12:27.
Fetene N, Linnander E, Fekadu B, Alemu H, Omer H, Canavan M, Smith J, Berman P, Bradley E. The Ethiopian health extension program and variation in health systems performance: what matters? PLoS One. 2016;11:5.
Kim SS, Rawat R, Mwangi EM, Tesfaye R, Abebe Y, Baker J, Frongillo EA, Ruel MT, Menon P. Exposure to large-scale social and behavior change communication interventions is associated with improvements in infant and young child feeding practices in Ethiopia. PLoS One. 2016;11:10.
Ethiopia Demographic Health Survey 2016, Central Statistical Agency Addis Ababa. The DHS Program ICF. Rockville; 2017. Available at https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf
Lenja A, Demissie T, Yohannes B, Yohannis M. Determinants of exclusive breastfeeding practice to infants aged less than six months in Offa district, Southern Ethiopia: a cross-sectional study. Int Breastfeed J. 2016;11:32.
Mekuria G, Edris M. Exclusive breastfeeding and associated factors among mothers in DebreMarkos, Northwest Ethiopia: a cross-sectional study. Int Breastfeed J. 2015;10:1.
Tewabe T, Mandesh A, Gualu T, Alem G, Mekuria G, Zeleke H. Exclusive breastfeeding practice and associated factors among mothers in Motta town, east Gojjam zone, Amhara regional state, Ethiopia, 2015: a cross-sectional study. Int Breastfeed J. 2017;12:12.
Liben ML, Gemechu YB, Adugnew M, Asrade A, Adamie B, Gebremedin E, Melak Y. Factors associated with exclusive breastfeeding practices among mothers in Dubti town, afar regional state, northeast Ethiopia: a community based cross-sectional study. Int Breastfeed J. 2016;11:4.
Belachew T, Taye A, Belachew T. Postnatal care service utilization and associated factors among mothers in Lemo Woreda, Ethiopia. J Womens Health Care. 2016;e 5:318.
Yeneabat T, Belachew T, Haile M. Determinants of cessation of exclusive breastfeeding in Ankesha Guagusa Woreda, Awi zone, Northwest Ethiopia: a cross-sectional study. BMC Pregnancy Childbirth. 2014;14:262.
Gizaw Z, Woldu W, Bitew BD. Exclusive breastfeeding status of children aged between 6 and 24 months in the nomadic population of Hadaleala district, Afar Region, northeast Ethiopia. Int Breastfeed J. 2017;12:38.
Kasahun AW, Wako WG, Gebere MW, Neima GH. Predictors of exclusive breastfeeding duration among 6–12 month aged children in Gurage zone, South Ethiopia: a survival analysis. Int Breastfeed J. 2017;12:20.
Arora, et al. Determinants of breastfeeding initiation among mothers in Sydney, Australia: findings from a birth cohort study. Int Breastfeed J. 2017;12:39.
Ogbo, et al. Prevalence and determinants of cessation of exclusive breastfeeding in the early postnatal period in Sydney, Australia. Int Breastfeed J. 2017;12:16.
Woldie TG, Kassa AW, Edris M. Assessment of exclusive breast feeding practice and associated factors in Mecha district, north west Ethiopia. Sci J Public Health. 2014;2(4):330–6.
Maonga AR, Mahande MJ, Damian DJ, Msuya SE. Factors affecting exclusive breastfeeding among women in Muheza district Tanga northeastern Tanzania: a mixed method community based study. Matern Child Health J. 2016;20:77–87.
Egata G, Berhane Y, Worku A. Predictors of non-exclusive breastfeeding at 6 months among rural mothers in east Ethiopia: a community-based analytical cross-sectional study. Int Breastfeed J. 2013;8:8.
Adugna B, Tadele H, Reta F, Berhan Y. Determinants of exclusive breastfeeding in infants less than six months of age in Hawassa, an urban setting, Ethiopia. Int Breastfeed J. 2017;12:45.
Asemahagn MA. Determinants of exclusive breastfeeding practices among mothers in Azezo district, northwest Ethiopia. Int Breastfeed J. 2016;11:22.
Musa A, Edris M, Negese D. Prevalence of exclusive breastfeeding practices and associated factors among mothers in Bahir Dar city, Northwest Ethiopia: a community based cross-sectional study. Int Breastfeed J. 2013;8:14.
Setegn T, Belachew T, Gerbaba M, Deribe K, Deribew A, Biadgilign S. Factors associated with exclusive breastfeeding practices among mothers in Goba district, south east Ethiopia: a cross-sectional study. Int Breastfeed J. 2012;7:17 Available at http://www.internationalbreastfeedingjournal.com/content/7/1/17.
Acknowledgments
The Authors thank Samara University and the study subjects.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
AMB and MLL participated in conceiving and designing the study. AMB supervised data collection. AMB and MLL performed data analysis and interpretation. MLL drafted the manuscript. AA assisted in data analysis and interpretation, and critically edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Research Ethics Review Committee (RERC) of Samara University (Reference number ERC/0087/2018). An official letter was written from Afar Regional Health Bureau to the city administration. Then, support letters were written to all ketenas. The participants enrolled in the study were informed about the study objectives, expected outcomes, benefits and the risks associated with it. Finally, written informed consent was taken from the participants before the interview. Furthermore, confidentiality was maintained throughout the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Questionnaire to assess factors associated with the early termination of exclusive breastfeeding.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Beyene, A.M., Liben, M.L. & Arora, A. Factors associated with the early termination of exclusive breastfeeding among mother-infant dyads in Samara-Logia, Northeastern Ethiopia. BMC Pediatr 19, 428 (2019). https://doi.org/10.1186/s12887-019-1803-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-019-1803-1