Abstract
Background
The objective of the study was to describe the baseline health-related quality of life (HRQOL) in a cohort of children and adolescents with type 1 diabetes mellitus (T1DM), and analyze its associated clinical and sociodemographic factors, assessing HRQOL through internet.
Methods
This was a descriptive study of 136 patients with T1DM from 5 hospitals in Catalonia, Spain (72 girls, mean age 13.4 years (range 8–19). Inclusion criteria were more than 6 months from diagnosis, more than 8 years old and without cognitive problems. Sociodemographic (age, sex, family level of education, type of family and origin) and clinical variables (type of insulin therapy, duration of disease, adherence to treatment, body mass index and HbA1c) were collected. HRQOL was assessed using the EuroQol-5D (EQ-5D-Y) and KIDSCREEN, collected via web. Mental health status was assessed using the Strengths and Difficulties Questionnaire. Multiple linear regression models were adjusted.
Results
Physical-well-being mean scores were lower (worse) than the European average (<50) and especially in girls, older children (>11 years old), those from single-parent families, and those with low adherence. Older children and patients with poor metabolic control (HbA1c >7,5% [58 mmol/mol]) showed worse scores in the KIDSCREEN-10 index. Similar results were observed with the EQ-5D-Y. Multivariate models showed that age, single-parent families, adherence and mental health were the most influential factors.
Conclusions
Diabetic patients report similar HRQOL than the population of the same age with slightly worse physical well-being. The study shows some factors to be taken into account to improve HRQOL, and also the feasibility of using web to collect information in clinical practice.
Similar content being viewed by others
Background
There is a growing interest in the study of health-related quality of life (HRQOL), which has become an important end-point measure from the clinical and epidemiological point of view [1].
Type 1 Diabetes Mellitus (T1DM) is a chronic disease that affects all aspects of patient’s life and especially psychologically and therefore HRQOL. The management of T1DM is complex, requiring a high degree of responsibility and self-control to achieve an adequate metabolic control. Key aspects to succeed are the support of a multidisciplinary team, education in disease management with decision-making capacity, and exploit the possibilities offered by new technologies without forgetting the emotional sphere of the patient and family. In fact, treatment guidelines recommend routine screening for emotional status and family relationships [2]. On the other hand, hormonal and psychosocial changes that occur during puberty make this stage a difficult time with high metabolic instability, and many adolescents experience deterioration in metabolic control [3, 4].
Assessment of HRQOL in clinical practice is important in order to evaluate the course of the disease, early detection of problems, and to determine what type of insulin therapy would be adequate to maintain acceptable metabolic control with less impact on HRQOL in each patient [2, 4].
Previous studies have shown that girls, older children, and specific sociodemographic factors such as single-parenthood, lower family income or minority status would be associated with poor metabolic control and worse HRQOL [2]. Studies addressed to analyze emotional and psychosocial aspects such as self-management and self-esteem, resilience, and parenting showed a positive influence on HRQOL, although interventions need to be tailored to the specific needs of children and families [5]. A systematic review assessed HRQOL in children with T1DM [6] and its potential help in clinical management. This review describes HRQOL in groups of patients comparing with control groups, and also analyzing HRQOL with specific instruments. The results of this review show that overall diabetic children have similar HRQOL compared to healthy peers but reported disease specific problems. Gender and age differences were also found. Studies included in this review were mainly descriptive and no studies were included comparing with general population data.
A few studies were carried out in Spain addressing HRQOL in children with T1DM [7], Studies analyzing clinical factors associated with HRQOL in patients with T1DM, and on the use of internet to collect information [8] and its usefulness on clinical practice [9–11] were carried out in other contexts.
The aim of this study was to describe the HRQOL in Spanish children and adolescents with T1DM and analyze its associated clinical and sociodemographic factors, assessing HRQOL through internet. This study represents the baseline assessment of an intervention to evaluate use of generic HRQOL measures administered via internet in clinical practice. According to previous studies it was expected that children from vulnerable families, with poor metabolic control, and/or poor mental health would show worse HRQOL.
Methods
Participants and procedures
Patients were consecutively recruited from a list of 205 potential candidates (104 girls) between 8 and 19 years old with T1DM attending outpatient pediatric endocrinology of 5 hospitals in the Barcelona province area, Spain (7 pediatric endocrinologists participated in the study), between July and December 2014. Exclusion criteria were less than 6 months from diagnosis of T1DM, less than 8 years old at the time of recruitment, cognitive problems that prevented comprehension of the questionnaires, and patients who declined to participate in the study.
Families that fulfilled inclusion criteria were provided with a letter explaining the characteristics of the project and the need to access to digital questionnaires 48 h before the follow-up visits. After agreeing to participate in the study, parents answered a paper questionnaire administered during this visit including information on sociodemographics and family’s variables. Before the next quarterly routine visit, a reminder was sent by email and/or telephone to the family and patient.
Study variables
Sociodemographic variables were collected from parents, clinical variables came from clinical records, and HRQOL, mental health and adherence to treatment came from the self-administered online questionnaire.
Sociodemographic variables were: age, sex, and the highest family level of education (primary, secondary or university). The variable family origin (native vs immigrant status) was based on the country where the child and parents were born. It was considered as immigrants if the child and/or both parents were born in a developing country (Asia, Africa, Latin America, or Eastern European country). Family type (single-parent vs bi-parental family), and hospital were also collected.
Clinical variables analyzed were: type of insulin therapy (multiple daily injections [MDI] or pump therapy, only in 2 cases); use of insulin bolus calculator or not; and time since diagnoses (in years). Decompensation in the last 3 months was assessed as significant hypoglycemia (<60 mg/dl with decreased level of consciousness requiring glucagon or the help of others to be reversed), and significant hyperglycemia (>400-450 mg/dl which required action by the professionals). Diabetes ketoacidosis was also collected. The HbA1c was used as a measure of metabolic control by determination in capillary blood (DCA 2000 Bayer/Siemens®) or serum in an analytical laboratory (HPLC). Weight, height and body mass index (BMI, Z score) [12] was also collected.
The web-version of the questionnaires was developed through a generic internet tool using Ruby on Rails applications and MySQL database (http://rubyonrails.org).
The self-administered questionnaire included the internet versions of the Euroqol-5D-Y (EQ-5D-Y) and KIDSCREEN-27 and KIDSCREEN-10 index as measures of HRQOL.
The self-reported EQ-5D-Y [13] descriptive system consists of 5 dimensions (mobility, self-care, usual activities, pain-discomfort and anxiety-depression) with 3-levels Likert response scales (no problems, moderate problems and serious problems) and a visual analogue scale (VAS) on the general health status from 0 (worst health status) to 100 (best health status possible). The Internet Catalan and Spanish versions of the eEQ-5D-Y have demonstrated acceptable reliability and validity in the Spanish population, and similar to the paper version [14].
The self-reported KIDSCREEN-27 [15] was assessed by its 5 dimensions: physical well-being (5 items), psychological well-being (7 items), autonomy and relationships with parents (7 items), social support and relationship with friends (4 items) and school environment (4 items). Responses were categorized into 5 options Likert scales that assess the frequency or intensity of the attribute, with a recall-period of 1 week in most questions. The scores are standardized to a mean of 50 and a standard deviation (SD) 10, from a reference sample of 22,000 European children and adolescents. The KIDSCREEN-10 index was also included as a summary measure. The internet Spanish and Catalan versions of the questionnaire have demonstrated acceptable reliability and validity in this population, similar to the paper version [16].
Children’s mental health status was assessed using the Strengths and Difficulties Questionnaire (SDQ), a brief behavioral screening questionnaire for children and adolescents that asks about their mental health symptoms and positive attitudes [17]. The instrument consists of 25 items measuring 5 dimensions. All items are scored on a three point scale (0 = not true, 1 = somewhat true, and 2 = certainly true). Items in the 4 problem dimensions are summed to give a total difficulties score ranging from 0 (no problems) – 40 (maximum problems). Higher scores indicate more problems. The Spanish and catalan versions have been shown to be reliable and valid [18].
Adherence to treatment in the month prior to the interview was assessed by two questions: How often have you checked your blood sugar?; and: How often did you do a blood sugar check within 2–3 h after a meal? Both questions included 7 and 5 frequency Likert-scale answer categories, respectively. Patients were categorized into high adherence if they answered a frequency of control of glucose level 3 or more times per day, and also a frequency of blood sugar check within 2–3 h after a meal at least 3 or more times a week.
Statistical analysis
Mean scores of the KIDSCREEN-27 dimensions and KIDSCREEN-10 index and its 95% confidence interval (95% CI) were computed and compared with the average of European population. The distribution of health states were also analyzed according to the descriptive system of EQ-5D-Y. Mean scores of HRQOL, both the KIDSCREEN and VAS score, according to sociodemographic factors, adherence and control of diabetes, and clinical variables were assessed by Student t test, Mann–Whitney U, or ANOVA according to the characteristics of analyzed variables. Standardized mean differences (effect size, ES) estimated as the difference between the means divided by pooled standard deviation, were computed to analyze the magnitude of differences [19].
Effect sizes of 0.2–0.5 were considered small; those between 0.51 and 0.8 moderate, and those over 0.8 were considered large.
Multiple linear regression models were adjusted to analyze the influence of factors associated with HRQOL controlling for socio-demographic, clinical factors, and mental health. Interactions terms between clinical and sociodemographic factors were also explored. Results of regressions in terms of B coefficients can be interpreted as a modification (increase [+] or decrease [−]) on the dependent variable (a given dimension of HRQOL) for every unit of change in the predictor variable (e.g. age). Bonferroni correction was used to control for multiple comparisons. Program STATA.11 software versions were used in the analysis.
Results
One hundred thirty six patients were included in the study (participation rate 65.5%). Sixty one patients were not included due to change of address, transfer to the adult unit, or not attending follow-up visits, while 8 patients rejected their participation in the study. There were no significant differences in terms of age, gender or years of disease progression among patients who entered in the study and those not included.
Table 1 shows the clinical and demographic characteristics of the sample. The average age of participants was 13.4 years; 52.9% were girls; 15.7% came from single-parent families; 6% of immigrant families, and 19.4% of parents had university degree. In 4 cases the questionnaires were filled out in a waiting time previous to the visit given the absence of internet at home.
The mean time of disease progression was 5 years, with 39.7% (n = 54) longstanding (>5 years), and 19.9% less than 1 year. The average HbA1c level was 7.65% (SD ± 1.3; 60 mmol/mol; SD ± 13.2); 52.2% of patients had good metabolic control (HbA1c <7.5%; 58 mmol/ml), with an average of 8.64% (SD ±1.22; 71 mmol/ml) in those with poor metabolic control and 6.74% (SD ± 0.59; 50 mmol/ml) in those with good metabolic control; 1.5% of patients used pump therapy, the rest received MDI therapy; 81.5% of patients had no significant change in insulin therapy during the 3 months prior to baseline assessment. Five percent started to use an insulin bolus calculator, and 52.9% had a high level of adherence to treatment. There were 3 cases of significant hypoglycemia in the last three months. Mean score on mental health (SDQ total difficulties score) was 10.65.
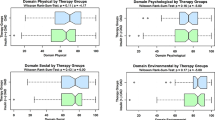
The results of the KIDSCREEN-27 and the KIDSCREEN-10 mean scores, and VAS are shown in Table 2. Physical-well-being scores were lower than the European average (<50) and especially in girls, older children (>11y), those from single-parent families, and those with low adherence to the treatment. Older children (>11y = 48.3, [95% CI] 46.7–49.9), and patients with poor metabolic control (48.0; 95% CI 46.3–49.6) presented worse scores in the KIDSCREEN-10 index. On the other hand, patients with good metabolic control and shorter duration of disease (<5 years), showed better scores. Similar results were observed with the VAS. Table 3 shows the magnitude of differences (ES) on HRQOL according to sociodemographic and clinical variables. Large ES were seen on age, changes on treatment during the last 3 months, hyperglycemia and hypoglycemia.
Children and adolescents showed relatively few health problems in the EQ-5D-Y dimensions, although 33.6% reported having pain or discomfort and 26.1% reported having anxiety or depression; 50% of children scored the best possible health state on to the descriptive EQ-5D-Y system (data not shown).
Multivariate models of HRQOL are shown in Table 4. Age, single-parent families, adherence to treatment, and mental health were the influential factors on HRQOL. Statistically significant associated factors to the KIDSCREEN-10 were age (B coefficient = −0.93); single-parent families (B = −15.2); and mental health (B = −0.7). An interaction was found between age and type of family, so older ages showed less influence of single parent families on the KIDSCREEN-10 index of HRQOL (B = 1.02 for age and type of family interaction).
Discussion
This study shows that children and adolescents with T1DM report similar HRQOL than the general population of the same age and gender, although slightly worse physical well-being than their peers. The study shows that the type of family, mental health and treatment adherence should be taken into account to improve HRQOL in these patients. It also shows the feasibility of assessing HRQOL via Internet, and its use as a daily clinical practice tool in a cohort of children, reinforcing the results of previous research [9, 10].
In general, HRQOL were similar than the general population, as it was shown in a previous systematic review [6]. In our study, younger patients had better HRQOL scores; and girls had lower HRQOL scores in virtually all dimensions, indicating greater vulnerability and similar results than in other studies [20, 21]. Thus, the study suggests the need to assess and monitor potential problems, especially in adolescence. Moreover, recent guidelines from ISPAD have recommended routine assessment of HRQOL with adequate tools [2]. Comparing our results with Spanish general population data Physical well-being dimension score was 0.5 standard deviation lower (worse) than the reference population, which represent a meaningful difference [22].
Other studies had already linked a worse HRQOL in children with specific characteristics such as those from single-parent families or families with disadvantaged socioeconomic status [23, 24]. The results of the present study reinforce this finding and the importance of knowing the social situation of the patient. One of the main findings indicates the need to provide special reinforcement in monoparental families at younger ages.
Evidence shows that better HRQOL is associated with better metabolic control although this relationship is modest [20, 21, 25, 26]. In our study it was also found an association between HRQOL and HbA1c; nevertheless, it is not possible to establish the directionality of association given the cross-sectional design of the analysis. Some studies suggest that the experience of having suffered severe hypoglycemia can affect HRQOL for fear of their recurrence [27]. In our study patients who had suffered significant hypoglycemia showed better scores in almost all dimensions of HRQOL, although these data are not valuable because of the small number of patients experiencing hypoglycemia. On the other hand, in general almost all patients were well controlled as it was reflected by the relatively few patients in the higher extreme of the curve distribution of HbA1c. This fact could be associated to the almost universal healthcare coverage and easy access to healthcare services and programmes in Spain, which facilitates disease control.
Adherence to treatment is very important to achieve a good metabolic control and it could be associated to HRQOL [21]. Our study shows similar results than a prospective study, with worse HRQOL in patients with a lower level of adherence [28]. Moreover, patients on pump therapy, requiring a very high level of adhesion, have been linked to improved quality of life [29, 30]. In our case we have not been able to analyze the characteristics of this treatment given the small number of patients.
Patients with poor mental health also show lower HRQOL scores in our study. This figures are similar than other studies in which diabetic patients have a high incidence of depression, anxiety and other psychological problems [24, 31, 32]. In this sense, the role of clinical psychologist could be important in order to reinforce those positive emotional and psychological aspects that are potentially modifiable in this group of patients [33]. Mental health and adherence were among the factors associated with HRQOL, therefore, are aspects to consider and evaluate regularly in diabetic patients, in addition to metabolic control.
The study has several limitations. Firstly, 35% of patients who did not enter the study could lead to a selection bias. Although there were no differences between these patients and those who participated in terms of age or years of evolution of the disease, we didn’t know the metabolic control of some of them. Perhaps some had higher levels of HbA1c and therefore would not participate. Secondly, patients were recruited from 5 different centers, so that personal characteristics, clinical factors and treatment received may vary the results. However, no significant differences were found in the multivariate models when entering the center or pediatrician (data not shown). Thirdly, the results, in part may be related to the HRQOL instruments used in each study. HRQOL studies in pediatric patients with T1DM have used different measurement instruments, some disease-specific, such as diabetes DISABKIDS module [34], or the Peds-QL [35].
One of the strengths of the study is the use of the KIDSCREEN and the EQ-5D-Y simultaneously, two generic HRQOL instruments for children. Thus, it has been possible to compare the HRQOL of this group of patients with the normative KIDSCREEN Spanish and European data and allowed us to estimate the impact comparing with the general population of the same age and sex. Moreover, it is currently not possible to calculate the Quality Adjusted Life Years (QALYs) or a similar indicator necessary to carry out a cost-effectiveness analysis due to the lack of developed preference-values in the Spanish population of this age group. The present study attempts to provide initial data to carry out such studies, which are scarce and necessary in childhood population. On the other hand, it was not included a specific HRQOL instrument in T1DM due to the lack of such instruments adapted into Spanish population of this age group. However both the KIDSCREEN and the EQ-5D-Y as generic instruments have been widely used in general healthy population as well as various health problems. Both instruments have demonstrated acceptable discrimination ability to study the impact of health problems on HRQOL. In addition, the availability of reference values has allowed us to use the European general population norms of the KIDSCREEN and compare with the sample with acceptable accuracy and easy interpretation. Finally, it has not been possible to include a standardized adherence measure given the lack of instruments adapted in Spain. However the variables used have yielded an assessment of adherence acceptably. Future studies should incorporate valid and reliable measures of this factor with potential utility in the daily clinical management.
Conclusions
In summary, HRQOL in children and adolescents with T1DM were similar than the general population of the same age and gender, with slightly lower physical well-being. We have demonstrated the feasibility to assess HRQOL through the use of new technologies such as the Internet, which could provide essential elements in routine visits in the pediatric and adolescent diabetic patients.
Abbreviations
- DKA:
-
Diabetes ketoacidosis
- HbA1c:
-
Glycated haemoglobin
- HRQOL:
-
Health-related quality of life
- MDI:
-
Multiple daily injections
- T1DM:
-
Type 1 Diabetes Mellitus
References
Ravens-Sieberer U, Erhart M, Wille N, Wetzel R, Nickel J, Bullinger M. Generic health-related quality-of-live assessment in children and adolescents: methodological considerations. Pharmacoeconomics. 2006;24:1199–220.
Delamater AM, de Wit M, McDarby V, Malik J, Acerini CL. ISPAD Clinical Practice Consensus Guidelines 2014 Compendium. Psychological care of children and adolescents with type 1 diabetes. Pediatr Diabetes. 2014;15 Suppl 20:232–44.
King PS, Berg CA, Butner J, Drew LM, Foster C, Donaldson D, et al. Longitudinal trajectories of metabolic control across adolescence: associations with parental involvement, adolescents’ psychosocial maturity, and health care utilization. J Adolesc Health. 2012;50:491–6.
Lustman PJ, Anderson RJ, Freedland KE, de Groot M, Carney RM, Clouse RE. Depression and poor glycemic control: a meta-analytic review of the literature. Diabetes Care. 2000;23:934–42.
Cameron FJ, de Beaufort C, Aanstoot HJ, Hoey H, Lange K, Castano L, et al. Lessons from the Hvidoere International Study Group on childhood diabetes: be dogmatic about outcome and flexible in approach. Pediatr Diabetes. 2013;14:473–80.
Nieuwesteeg A, Pouwer F, van der Kamp R, van Bakel H, Aanstoot HJ, Hartman E. Quality of life of children with type 1 diabetes: a systematic review. Curr Diabetes Rev. 2012;8:434–43.
Miranda Velasco MJ, Domínguez Martína E, Arroyo Díez FJ, Méndez Pérez P, González de Buitrago J, Amigo J. Calidad de vida relacionada con la salud en la diabetes mellitus tipo 1. An Pediatr (Barc). 2012;77(5):329–33.
Varni JW, Limbers CA, Burwinkle TM, Bryant WP, Wilson DP. The ePedsQL in Type 1 and Type 2 Diabetes. Feasibility, reliability, and validity of the Pediatric Quality of Life Inventory™ Internet administration. Diabetes Care. 2008;31:672–7.
de Wit M, de Waal HA D-v, Bokma JA, Bokma JA, Haasnoot K, Houdijk MC, et al. Monitoring and discussing health-related quality of life in adolescents with type 1 diabetes improve psychosocial well-being: a randomized controlled trial. Diabetes Care. 2008;31:1521–6.
Haverman L, Engelen V, van Rossum MAJ, Heyman HAS, Grootenhuis MA. Monitoring health-related quality of life in paediatric practice: development of an innovative web-based application. BMC Pediatr. 2011;11:3.
Eilander M, de Wit M, Rotteveel J, Maas-van Schaaijk N, Roeleveld-Versteegh A, Snoek F. Implementation of quality of life monitoring in Dutch routine care of adolescents with type 1 diabetes: appreciated but difficult. Pediatr Diabetes. 2016;17:112–9.
Carrascosa Lezcano A, Fernández García JM, Fernández Ramos C, Ferrández Longás A, López-Siguero JP, Sánchez González E, et al. Estudio transversal español de crecimiento 2008. Parte II: valores de talla, peso e índice de masa corporal desde el nacimiento a la talla adulta. An Pediatr (Barc). 2008;68:552–69.
Gusi N, Badia X, Herdman M, Olivares PR. Traducción y adaptación cultural de la versión española del cuestionario EQ-5D-Y en niños y adolescentes. Aten Primaria. 2009;41:19–23.
Robles N, Rajmil L, Rodriguez-Arjona D, Azuara M, Codina F, Raat H, et al. Development of the web-based Spanish and Catalan versions of the Euroqol 5D-Y (EQ-5D-Y) and comparison of results with the paper version. Health Qual Life Outcomes. 2015;13:72. doi:10.1186/s12955-015-0271-z.
Ravens-Sieberer U, Erhart M, Rajmil L, Herdman M, Auquier P, Bruil J, et al. Reliability, construct and criterion validity of the KIDSCREEN-10 score: a short measure for children and adolescents’ well-being and health-related quality of life. Qual Life Res. 2010;19:1487–500.
Rajmil L, Robles N, Rodriguez-Arjona D, Azuara M, Codina F, Raat H, et al. Comparison of the Web-Based and Digital Questionnaires of the Spanish and Catalan Versions of the KIDSCREEN-52. PLoS One. 2014;9(12):e114527. doi:10.1371/journal.pone.0114527.
Goodman R. The strengths and difficulties questionnaire: A research note. J Child Psychol Psychiatr. 1997;38:581–6.
Pardo CY. El desenvolupament de la personalitat psicopàtica: pràctiques educatives parentals i altres variables familiars (Thesis). Barcelona: Universitat Autònoma de Barcelona; 2007.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale: Lawrence Erlbaum Associated; 1988.
Hoey H, Aanstoot HJ, Chiarelli F, Daneman D, Danne T, Dorchy H, et al. Good metabolic control is associated with better quality of life in 2,101 adolescents with type 1 diabetes. Diabetes Care. 2001;24:1923–8.
Wagner VM, Muller-Godeffroy E, von Sengbusch S, Hager S, Thyen U. Age, metabolic control and type of insulin regime influences health-related quality of life in children and adolescents with type 1 diabetes mellitus. Eur J Pediatr. 2005;164:491–6.
Tebe C, Berra S, Herdman M, Aymerich M, Alonso J, Rajmil L. Fiabilidad y validez de la versión española del KIDSCREEN-52 para población infantil y adolescente. Med Clin (Barc). 2008;130:650–4.
Delamater AM, Shaw KH, Aplegate EB, Pratt IA, Eidson M, Lancelotta GX, et al. Risk for metabolic control problems in minority youth with diabetes. Diabetes Care. 1999;22:700–5.
Silverstein J, Cheng P, Ruedy KJ, Craig Kollman C, Beck RW, Klingensmith GJ, et al. for the pediatric Diabetes Consortium. Depressive symptoms in youth with type 1 or type 2 diabetes: results of the pediatric diabetes consortium screening assessment of depression in diabetes study. Diabetes Care. 2015 DOI: 10.2337/dc15-0982
Guttmann-Bauman I, Flaherty BP, Strugger M, McEvoy RC. Metabolic control and quality-of-life self-assessment in adlescents with IDDM. Diabetes Care. 1998;21:915–8.
Hesketh KD, Wake MA, Cameron FJ. Health-related quality of life and metabolic control in children with type 1 diabetes: a prospective cohort study. Diabetes Care. 2004;27:415–20.
Nordfeldt S, Ludvigsson J. Fear and other disturbances of severe hypoglycaemia in children and adolescents with type 1 diabetes mellitus. J Pediatr Endocrinol Metab. 2005;18:83–91.
Hilliard ME, Mann KA, Peugh JL, Hood KK. How poorer quality of life in adolescence predicts subsequent type 1 diabetes management and control. Patient Educ Couns. 2013;91:120–5.
Lawrence JM, Yi-Frazier JP, Black MH, Anderson A, Hood K, Imperatore G, et al. Demographic and clinical correlates of diabetes-related quality of life among youth with type 1 diabetes. J Pediatr. 2012;161:201–207e2.
McMahon SK, Airey FL, Marangou DA, McElwee KJ, Carne CL, Clarey AJ, et al. Insulin pump therapy in children and adolescents: improvements in key parameters of diabetes management including quality of life. Diabet Med. 2005;22:92–6.
Reynolds KA, Helgeson VS. Children with diabetes compared to peers: depressed? Distressed? Ann Behav Med. 2011;42:29–41.
Lawrence JM, Standiford DA, Loots B, Klingensmith GJ, Williams DE, Ruggiero A, et al. Prevalence and correlates of depressed mood among youth with diabetes: the SEARCH for diabetes in youth study. Pediatrics. 2006;117:1348–58.
Butwicka A, Fendler W, Zalepa A, Szadkowska A, Zawodniak-Szalapska M, Gmitrowicz A. Psychiatric Disorders and Health-Related Quality of Life in Children With Type 1 Diabetes Mellitus. Psychosomatics. 2016;57:185–93.
Hanberger L, Ludvingsson J, Nordfeldt S. Health-related quality of life in intensively treated young patients with type 1 diabetes. Pediatr Diabetes. 2009;10:374–81.
Varni JW, Burwinkle TM, Jacobs JR, Gottschalk M, Kaufman F, Jones KL. The PedsQL in type 1 and type 2 diabetes: reliability and validity of the Pediatric Quality of Life Inventory Generic Core Scales and type 1 Diabetes Module. Diabetes Care. 2003;26:631–7.
Acknowledgements
Not applicable.
Funding
The study was partially funded by Fondo de Investigación Sanitaria, Spanish Ministry of Health, contract N° 12/01296. The funding agency had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript.
Availability of data and materials
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
Authors’ contribution
MM participated in the design and coordination of the study, carried out the fieldwork and wrote the first draft of the manuscript. JB participated in the design of the study, and carried out the fieldwork. DRA participated in the design and coordination of the study, carried out the fieldwork and statistical analysis. JP participated in the design of the study, and carried out the fieldwork. RC participated in the design and coordination of the study, and carried out the fieldwork. GC participated in the design and coordination of the study, and carried out the fieldwork. XH participated in the design and coordination of the study, and carried out the fieldwork. JMM participated in the design and coordination of the study, and carried out the fieldwork. URS conceived the study and participated in the design and coordination of the study. HR conceived the study and participated in the coordination of the study. LR conceived the study, participated in the design and coordination, carried out the fieldwork and statistical analysis, and wrote the first draft of the manuscript. All authors read and approved the final manuscript as submitted.
Competing interest
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by the ethics committee of each participant hospital: Clinical Research Ethical Committees (CEIC) of Parc de Salut Mar, Barcelona; Germans Trias i Pujol Hospital, Badalona; Sant Creu i Sant Pau Hospital, Barcelona, Parc Taulí Hospital, Sabadell; Calella and Blanes Hospitals; in accordance with national and international guidelines (code of ethics, Helsinki Declaration), as well as to the legislation on data confidentiality (Organic Law 15/1999 of December 13 Data Protection character staff). Written signed consent to participate was requested from parents of all participating children. Written consent was also requested from children over 12 years old, while in younger children the assent to participate was verbal. The collection and transfer of data was carried out according to strict security and data encryption.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Murillo, M., Bel, J., Pérez, J. et al. Health-related quality of life (HRQOL) and its associated factors in children with Type 1 Diabetes Mellitus (T1DM). BMC Pediatr 17, 16 (2017). https://doi.org/10.1186/s12887-017-0788-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-017-0788-x