Abstract
Background
Norovirus (NoV) GII.4 is the most common genotype for norovirus gastroenteritis worldwide. New variants or subgenotypes are continuously emerging, thus posing a serious threat to child health.
Methods
We compared retrospectively the clinical manifestations and complications of norovirus gastroenteritis in children from April, 2004 through December, 2012. NoV variants were analyzed to investigate the association of circulating viral strains with the complications. A modified disease severity score system based on Vesikari score system was devised and to evaluate disease severity.
Results
Compared to the outbreak in 2004/2005 winter, significant higher incidence of complications in the later periods are: convulsive disorder (p < 0.001) in 2006/2007 winter gastrointestinal hemorrhage (p = 0.047) and severe abdominal pain or irritability (p = 0.033) in 2008/09/10 winter; gastrointestinal hemorrhage (p = 0.030), severe abdominal pain or irritability (p = 0.014), and prominent hyperthermia (fever >39 °C, p = 0.001) in 2011/2012 winter. GII.4 Den_Haag_2006b, GII.4 2010, GII.4 Sydney 2012, and GII.4 2012b were the predominant strains in the outbreaks after 2006. By the modified severity score system, severe norovirus disease occurred in 28.5 %, 32 %, 33.3 %, and 30.2 % of the patients in the four periods. A longer duration of hospitalization (p = 0.02) were found in those with high score irrespective of the year of admission.
Conclusions
Our study demonstrated NoV outbreaks in northern Taiwan caused by different GII.4 variants that were associated with specific complications and uncommon clinical presentations. A modified severity score system first proposed in this study was able to identify severe cases with a longer hospital stay in NoV-infected children.
Similar content being viewed by others
Background
Acute gastroenteritis (AGE) is one of the most common infectious diseases and still a major cause of pediatric morbidity and mortality worldwide. The two most important viral agents in children are rotaviruses and noroviruses [1]. Norovirus (NoV) is genetically classified into 6 established genogroups (GI-GVI), while tentative genogroup GVII is proposed, and of which GI, GII, and GIV cause diseases in humans [2]. NoV GII.4 has emerged as the predominant genotype causing outbreaks of AGE worldwide. In multivariate analysis, NoV GII.4 were associated with higher hospitalization and mortality rates [3]. In the United States and Europe, NoV are responsible for approximately 50 % of all reported gastroenteritis outbreaks [4]. Similar to rotavirus infection, the main symptoms caused by norovirus infection are diarrhea, vomiting, fever, and even severe dehydration that needs hospitalization. Complications of norovirus AGE in children, such as convulsion, severe dehydration, malnutrition, bowel obstruction and even death were sporadically reported [5, 6]. Significant clinical features correlated with different viral strains has been documented recently, and after implementing rotavirus vaccination, norovirus infection has become one of the most important enteric pathogens threatening human health [3, 7]. Our recent study showed that in Taiwan under suboptimal use of rotavirus vaccines, a significant increase of norovirus infection was observed in the post- rotavirus vaccine era [8].
Disease severity score system for AGE was established previously [9]. The severity score for different clinical features and complications caused by emerging enteric viruses such as NoV is lacking. The purpose of this study was to investigate the clinical features and complications with norovirus infection in hospitalized pediatric patients supposed to have moderate to severe illness, compared to children treated in the community setting, and furthermore, we proposed a disease scoring system modified from Vesakari score system for evaluation of norovirus disease with variable severity in hospitalized patients.
Methods
Patient selection and identification of norovial infection
From April of 2004 through December of 2012, pediatric patients with the diagnosis of AGE hospitalized in the Division of Pediatric Gastroenterology, Chang Gung Children’s Hospital (CGCH) were randomly enrolled. Their fecal specimens were collected in a clean container within 3 days of hospitalization with guardian’s informed consent in this study with exclusion of those with major underlying diseases. Norovirus infection was confirmed by the detection of NoV using RT-PCR from fecal specimens of the patients with diarrheal disease [10]. The patient enrollment was irrespective of age, sex, ethnicity, and hospitalization wards. The symptoms were determined and documented in electronic medical records to determine how patient-reported symptoms were addressed by clinicians and clinical data of the patients enrolled were collected retrospectively from the chart records. These studies were approved by the Institutional Review Board of the Chang Gung Memorial Hospital.
Norovirus genome sequencing and genotyping
Viral nucleic acid extraction from fecal samples was performed using a kit according to the manufacturer’s recommendations (QIAamp Viral RNA Mini Kit; Qiagen, Hilden, Germany). The PCR primers and conditions used for determining NoV genotypes were described previously [10]. The cDNA products were cloned into a plasmid (pCR-XL-TOPO® vector; Invitrogen), and the recombinant plasmid was transferred into competent Escherichia coli (Topo® XL PCR Cloning kit; Invitrogen). The sequences of different PCR products from the same specimen were used to reconstruct the near-full-length norovirus genome using the Vector NTi software package (Invitrogen). The reference genome sequences of NoV used for comparison were all obtained from the National Center for Biotechnology Information database (http://www.ncbi.nlm.nih.gov/).
Complications of norovirus infection
The complication was recognized and defined as the occurrence of extraintestinal or unusual presentations of viral AGE during hospitalization including abdominal pain or irritability, gastrointestinal (GI) hemorrhage, electrolyte imbalance (hyponatremia: serum sodium level < 135 mmol/L; hypokalemia: serum potassium level < 3.5 mmol/L; or hypochloremia: serum chloride level < 98 mmol/L), prominent hyperthermia (body temperature > 39 °C), convulsive disorder (upward gaze, loss of consciousness, involuntary tonic or clonic manifestations), hypotension or hypovolemic shock (systolic blood pressure < 70 mmHg), hypoglycemia (serum sugar level < 70 mg/dL).
Modified score system for severity of norovirus infection
We evaluated the disease severity of norovirus infection by the Vesikari score system (total score < 7, mild; 7-≦10, moderate, and >10, severe. total maximum score 20) [9] and a modified score system based on clinical information from the hospitalized patients (Table 1). The modified severity score system has a 0–24 point numerical score, including the assessment for the presence of unusual clinical features, such as gastrointestinal hemorrhage (gross bloody stool or occult blood ≧ 2+ in stool), convulsion, and additional presentations such as abdominal pain or flatulence and prolonged or high fever. The modified system has a more simple stratification of general AGE symptoms from 3 points to 2 points hence with a total maximum score of 24. In our 24 points score system, mild degree is as less than 1/3 maximum score (8) and severe degree is half score or higher (12), that is score, < 8, mild; 8-≦11, moderate, and >11 (12 or higher) severe. The differences of the two score systems are listed in Table 1.
Statistical analysis
The chi-squared test or Fisher’s exact test was applied to dichotomous variable analysis, and the unpaired-sample student’s t-test was used for continuous variable analysis. A p value of < 0.05 was considered statistically significant. All the tests were analyzed using SAS system software version 8 for Windows.
Results
Outbreaks of norovirus acute gastroenteritis
During the period from 2004 to 2012, there were 957 hospitalized pediatric patients fulfilled study criteria initially enrolled. After the exclusion of 11 with bacterial infection, 7 finally diagnosed as specific disease other than infections, and 19 with incomplete clinical data collection, a total of 920 pediatric patients were finally enrolled. Among them, 207 (22.5 %) were positive for NoV in their fecal samples by RT-PCR method and 189 after excluding 18 with mixed infections, including 10 with rotavirus, 3 with astrovirus, 2 with enteric adenovirus, 1 with sapovirus, 1 with rotavirus and astrovirus, and 1 with Salmonella. The age distridution of the 920 enrolled children was 18 day- 247 months old (Mean: 31.6 months, median: 24 months), and of norovirus infection was 1–240 months old (mean 26.7 months, median: 17 months). Norovirus infection was confirmed in patients admitted in the four major outbreaks of 2004/2005 winter, 2006/2007 winter, 2008/09/10 winter, and 2011/2012 winter in 35 (11.6 %), 75 (41.4 %), 36 (15.9 %), and 43 (20.5 %) patients, respectively.
Complications of norovirus infection in different time periods
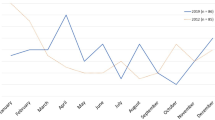
Figure 1 and Table 2 demonstrate the complications of norovirus infection observed in different time periods. From 2004 to 2005 winter, the most common complications were electrolyte imbalance (14.3 %) and hypoglycemia (11.4 %). From 2006 to 2007 winter, the most common complications were 28 % for convulsive disorder and 20 % for hypoglycemia. In 2008/09/10 winter, major complications including GI hemorrhage (22.2 %) and prominent hyperthermia (13.8 %) were observed. In the latest period from 2011 to 2012 winter, norovirus infection caused prominent hyperthermia (34.9 %) and GI hemorrhage (23.3 %) of the patients that were the most common complications.
Complications in different periods of norovirus outbreaks in northern Taiwan. The total numbers of hospitalized patients with confirmed norovirus infection during each outbreak are 35 in 2004–2005, 75 in 2006/2007 winter, 36 in 2008/09/10 winter, and 101 in 2011/12 winter. The most common complications are electrolyte imbalance (14.3 %) in 2004/2005 winter, convulsion (28 %) 2006/2007 winter, gastrointestinal (GI) hemorrhage (22.2 %) 2008/09/10 winter, and high fever (34.9 %) 2011/12 winter
Compared to norovirus infection in 2004/2005 winter, significant higher incidence of complications in the later periods are: in 2006/2007 winter, convulsive disorder (p < 0.001); in 2008/09/10 winter, GI hemorrhage (p = 0.047) and severe abdominal pain or irritability (p = 0.033); in 2011/2012 winter, GI hemorrhage (p = 0.030), severe abdominal pain or irritability (p = 0.014), and prominent hyperthermia (fever >39 °C) (p = 0.001).
Circulating NoV strains and complications
According to the genomic analysis of NoV, GII.4 was the most common genotype in all time periods; the major circulating NoV subgenotype or variant in 2006/2007 winter, GII.4 Den_Haag_2006b (28 of 70, 40 %), caused most complications of convulsion (19 of 28, 67.9 %) in infected children. The major subgenotype in 2008/09/10 winter, GII.4 2010 (New Orleans) (16 in 33, 48.5 %), caused GI hemorrhage (6, 37.5 %). Furthermore, GII.4 2012 subgenotypes (21 in 37, 56.8 %), the predominat NoV strains in 2011/2012 winter, caused more high fever (12, 57.1 %) and GI hemorrhage (7, 33.3 %).
Disease severity assessment by a modified score system compared to Vesikari score system
With regards to assessment using Vesikari score system, the overall distribution of patients’ disease severity was mild (score < 7) in 58 patients (30.6 %), moderate (7 ≦ score ≦ 10) 83 (43.9 %), and severe (score > 10) 49 (25.9 %). The proportions of patients with severe disease were 22.9 %, 26.6 %, 30.6 %, and 23.3 % in the four periods, and it was usually lower than 30 % (in 3 of the 4 periods). Hospital stays related to disease severity (median durations with interquartile ranges) are shown in Table 3: mild level, 5 (4–5) days; moderate, 4 (3–6) days; and severe, 4 (4–5) days, with the longest hospitalization in mild level group (Table 3). Under the assessment by modified score method (Table 1), the distribution of patients’ disease severity is mild (score < 8) in 50 (26.5 %), moderate (8 ≦ score ≦ 11) in 80 (42.3 %), and severe (score > 11) in 59 (31.2 %). The proportions of severe status are 28.5 %, 32 %, 33.3 %, and 30.2 % with the highest found in 2008/09/10 winter. Hospital stay according to severity assessed by modified score system (median durations with interquartile ranges) were: mild disease, 3 (3–4) days; moderate, 5 (4–6) days; and severe, 5 (4–7) days, with the longest hospitalization in severe disease group (p = 0.002) (Table 3). A longer duration of hospitalization (p = 0.02) in those with a high score under modified Vesikari score system rather than by the original Vesikari score system was observed.
Discussion
NoV is one of the emerging pathogens causing enteric infections in humans, and the associated clinical presentations are diverse [11–14]. Other than gastrointestinal symptoms, norovirus infection is associated with several extraintestinal or unusual complications, including benign infantile convulsion [5], necrotizing enterocolitis [15], and exacerbations of inflammatory bowel disease [16], as well as chronic, serious outcomes in immunocompromised patients [17, 18]. Comprehensive genotyping methods have been applied to monitor the molecular epidemiology of norovirus infections worldwide. Association of a given genotype or subgenotype with the occurrence of complications following gastroenteritis has been reported: GII.4 Den_Haag_2006b subtype caused infantile seizure following gastroenteritis during 2006–2007 outbreaks in Taiwan and GII.3 infection caused necrotizing enterocolitis and neonatal death in a neonatal intensive-care unit in 1998 in the United States [5, 15]. Although the specific NoV subgenotypes related to severe infection and complications was only sporadically reported, the rapid genetic evolution of NoV is believed to be the main factor driving the changing clinical manifestations in the infected patients. On the other hand, there is an unmet need that we need an objective disease severity score system specifically for the assessment of the severity of norovirus infection, as the Vesikari score used in rotavirus vaccine trials [19, 20]. Recently, a modified Vesikari score system for severity assessment of AGE in children in the emergency departments has been devised [21]. This is a simplified version of Vesikari score system by the deletion of dehydration status as a score item. Nevertheless, the evidence-based guidelines in Europe highlighted that enteric infectious agent is frequently associated with dehydration which reflects severity of disease and should be monitored by established severity score systems [22]. Complications of AGE and dehydration usually require aggressive management in norovirus infection. Thus, the addition of clinical complications as score items to form a modified system for severity assessment of norovirus infection is necessary. Based on this, we constructed such a modified system and verified its performance in assessing norovirus infection in different outbreaks in this study. A longer hospitalization in patients classified into mild severity in Veskari score system could be due to a prolonged course of fever, and presence of complications, abdominal pain and flatulence not included in Vesikari score system. These symptoms may cause poor appetite and delayed recovery of activity that require intravenous hydration. Furthermore, a significantly longer hospital stay in the higher-scored patients was found as practically expected because it is complication-weighted. Thus, the newly devised modified score system could be a useful tool in clinical practice.
There are several limitations in our study. First of all, our study enrolled hospitalized children usually having a moderate or severe illness rather than children with mild illness treated in a community setting. Secondly, with regards to the NoV subgenotypes, we could only verify the major strains circulating in each outbreak. Thirdly, although all the fecal samples were tested for bacterial pathogens and viruses, and NoV was found the only agent positive in these specimens, still other pathogens that may be associated with the clinical manifestations are not included in the panel. Fourthly, in spite of the presence of the complications in norovirus AGE, the mechanisms for the occurrence of such intestinal or extra-intestinal complications remain to be determined.
Conclusions
Vaccine development for the prevention of norovirus infection is currently under way and a more objective assessment of the infection is of paramount importance [23–27]. This study demonstrated that different circulating NoV subgenotypes were associated with different complications and uncommon presentations in a series of outbreaks over time in northern Taiwan. The stratification of hospitalized patients by assessment of the severity of their disease severity using a modified severity score system is possible, suggesting that the system is useful for future outbreak investigation. NoV is a rapidly evolving virus with the circulating genotypes or subgenotypes varying over time.
Abbreviations
- AGE:
-
Acute gastroenteritis
- CGCH:
-
Chang Gung Children’s Hospital
- GI:
-
Gastrointestinal
- NoV:
-
Norovirus
References
Matthews JE, Dickey BW, Miller RD, Felzer JR, Dawson BP, Lee AS, et al. The epidemiology of published norovirus outbreaks: a review of risk factors associated with attack rate and genogroup. Epidemiol Infect. 2012;140:1161–72.
Vinjé J. Advances in laboratory methods for detection and typing of norovirus. J Clin Microbiol. 2015;53:373–81.
Desai R, Hembree CD, Handel A, Matthews JE, Dickey BW, McDonald S, et al. Severe outcomes are associated with genogroup 2 genotype 4 norovirus outbreaks: a systematic literature review. Clin Infect Dis. 2012;55:189–93.
Patel MM, Hall AJ, Vinje J, Parashar UD. Noroviruses. A comprehensive review. J Clin Virol. 2009;44:1–8.
Chen SY, Tsai CN, Lai MW, Chen CY, Lin KL, Lin TY, et al. Norovirus infection as a cause of diarrhea-associated benign infantile seizures. Clin Infect Dis. 2009;48:849–55.
Kawano G, Oshige K, Syutou S, Koteda Y, Yokoyama T, Kim BG, et al. Benign infantile convulsions associated with mild gastroenteritis: a retrospective study of 39 cases including virological tests and efficacy of anticonvulsants. Brain Dev. 2007;29:617–22.
Tsai CN, Lin CY, Lin CW, Shih KC, Chiu CH, Chen S. Clinical relevance and genotypes of circulating noroviruses in northern Taiwan, 2006–2011. J Med Virol. 2014;86:335–46.
Chen SY, Tsai CN, Chen CL, Chao HC, Lee YS, Lai MW, et al. Severe viral gastroenteritis in children after suboptimal rotavirus immunization in Taiwan. Pediatr Infect Dis J. 2013;32:1335–9.
Vesikari T, Rautanen T, Varis T, Beards GM, Kapikian AZ. Rhesus Rotavirus candidate vaccine. Clinical trial in children vaccinated between 2 and 5 months of age. Am J Dis Child. 1990;144:285–9.
Bok K, Abente EJ, Realpe-Quintero M, Mitra T, Sosnovtsev SV, Kapikian AZ, et al. Evolutionary dynamics of GII.4 noroviruses over a 34-year period. J Virol. 2009;83:11890–901.
Buesa J, Montava R, Abu-Mallouh R, Fos M, Ribes JM, Bartolome R, et al. Sequential evolution of genotype GII.4 norovirus variants causing gastroenteritis outbreaks from 2001 to 2006 in Eastern Spain. J Med Virol. 2008;80:1288–95.
Eden JS, Hewitt J, Lim KL, Boni MF, Merif J, Greening G, et al. The emergence and evolution of the novel epidemic norovirus GII.4 variant Sydney 2012. Virology. 2014;450–451:106–13.
Mahar JE, Bok K, Green KY, Kirkwood CD. The importance of intergenic recombination in norovirus GII.3 evolution. J Virol. 2013;87:3687–98.
Zakikhany K, Allen DJ, Brown D, Iturriza-Gomara M. Molecular evolution of GII-4 Norovirus strains. PLoS One. 2012;7:e41625.
Turcios-Ruiz RM, Axelrod P, St John K, Bullitt E, Donahue J, Robinson N, et al. Outbreak of necrotizing enterocolitis caused by norovirus in a neonatal intensive care unit. J Pediatr. 2008;153:339–44.
Khan RR, Lawson AD, Minnich LL, Martin K, Nasir A, Emmett MK, et al. Gastrointestinal norovirus infection associated with exacerbation of inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2009;48:328–33.
Atmar J, Mullen E. Norovirus in immunocompromised patients. Oncol Nurs Forum. 2013;40:434–6.
Bok K, Green KY. Norovirus gastroenteritis in immunocompromised patients. N Engl J Med. 2012;367:2126–32.
Ruiz-Palacios GM, Perez-Schael I, Velazquez FR, Abate H, Breuer T, Clemens SC, et al. Safety and efficacy of an attenuated vaccine against severe rotavirus gastroenteritis. N Engl J Med. 2006;354:11–22.
Vesikari T, Matson DO, Dennehy P, Van Damme P, Santosham M, Rodriguez Z, et al. Safety and efficacy of a pentavalent human-bovine (WC3) reassortant rotavirus vaccine. N Engl J Med. 2006;354:23–33.
Schnadower D, Tarr PI, Gorelick MH, O'Connell K, Roskind CG, Powell EC, et al. Validation of the modified Vesikari score in children with gastroenteritis in 5 US emergency departments. J Pediatr Gastroenterol Nutr. 2013;57:514–9.
Guarino A, Ashkenazi S, Gendrel D, Lo Vecchio A, Shamir R, Szajewska H. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition/European Society for Pediatric Infectious Diseases evidence-based guidelines for the management of acute gastroenteritis in children in Europe: update 2014. J Pediatr Gastroenterol Nutr. 2014;59:132–52.
Atmar RL, Bernstein DI, Harro CD, Al-Ibrahim MS, Chen WH, Ferreira J, et al. Norovirus vaccine against experimental human Norwalk Virus illness. N Engl J Med. 2011;365:2178–87.
Bok K, Parra GI, Mitra T, Abente E, Shaver CK, Boon D, et al. Chimpanzees as an animal model for human norovirus infection and vaccine development. Proc Natl Acad Sci U S A. 2011;108:325–30.
Tan M, Huang P, Xia M, Fang PA, Zhong W, McNeal M, et al. Norovirus P particle, a novel platform for vaccine development and antibody production. J Virol. 2011;85:753–64.
Tan M, Jiang X. Norovirus P particle: a subviral nanoparticle for vaccine development against norovirus, rotavirus and influenza virus. Nanomedicine (Lond). 2012;7:889–97.
Treanor JJ, Atmar RL, Frey SE, Gormley R, Chen WH, Ferreira J, et al. A novel intramuscular bivalent norovirus VLP vaccine candidate - reactogenicity, safety and immunogenicity in a phase I trial in healthy adults. J Infect Dis. 2014;210:1763–71.
Acknowledgements
We are grateful to our colleagues in the Department of Pediatrics, Chang Gung Memorial Hospital, Taoyuan, Taiwan, for their help in this study.
Funding
The research was supported by grants from Chang Gung Memorial Hospital (CMRPG4C0041 and CMRPG4C0042) and Ministry of Science and Technology (NSC101-2314-B-182A-047), Taiwan.
Availability of data and materials
Data and materials are not available because of a policy set by the Institutional Review Board, Chang Gung Memorial Hospital. More information is available from the corresponding author on request.
Authors’ contributions
P-LW, S-YC, and C-HC designed the study, enrolled the cases, and collected and analyzed the data. C-NT and C-LC carried out genetic experiments. H-CC, M-WL, and Y-JC helped to enroll cases and analyzed the data. P-LW, S-YC, and C-HC drafted the manuscript. P-L Wang and S-Y Chen contributed equally as the first author. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
The authors grant the publisher permission to publish their work.
Ethics approval and consent to participate
The Institutional Review Board of Chang Gung Memorial Hospital approved the study protocol (No. 98-3759B and 100-4283A3). All patients’ legal guardians signed the informed consent form when patients were enrolled.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wang, PL., Chen, SY., Tsai, CN. et al. Complicated norovirus infection and assessment of severity by a modified Vesikari disease score system in hospitalized children. BMC Pediatr 16, 162 (2016). https://doi.org/10.1186/s12887-016-0699-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-016-0699-2