Abstract
Background
Primary intraocular lymphoma (PIOL) is a rare malignancy with a poor prognosis, but its optimal therapy remains unclear. Herein, we aimed to analyze the epidemiology and survival outcomes of PIOL patients based on a population-based cancer registry in the United States.
Methods
Patients diagnosed with PIOL between 1992 and 2018 were identified from the Surveillance Epidemiology and End Results program. The patients were divided into two groups: those aged < 60 years and ≥ 60 years. We used the chi-squared test to analyze the differences between the two groups. Descriptive analyses were performed to analyze epidemiological characteristics and treatment. The likely prognostic factors were analyzed by Kaplan–Meier curves and Cox proportional hazards models.
Results
The overall incidence of PIOL was 0.23/1,000,000, which was steadily increasing from 1992 to 2018, with an annual percentage change of 2.35. In total, 326 patients (mean age, 66.1 years) with PIOL were included in this study, 72.1% were aged ≥ 60 years, 84.4% were White, and 60.4% were female. The most common pathological type was diffuse large B-cell lymphoma (DLBCL), but in patients aged < 60 years, extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue was the most common. The disease-specific survival rates were 74.2% and 61.5% 5 and 10 years after diagnosis, respectively. Survival analysis found that surgery, radiation, and chemotherapy did not lead to better prognosis.
Conclusions
PIOL is a rare disease with poor prognosis, and its incidence has been increasing for nearly 30 years. It usually affects people aged ≥ 60 years, and DLBCL is the most common pathological type of PIOL. Patients aged < 60 years and with non-DLBCL type have improved survival. Survival of PIOL has improved in recent years.
Similar content being viewed by others
Background
Primary intraocular lymphoma (PIOL) is a rare heterogeneous malignancy and considered a subset of primary central nervous system lymphoma (PCNSL), with lymphoma cells initially existing only in the eyes [1, 2]. As PIOL is a rare subset of PCNSL, most of its epidemiology data are deduced from studies on PCNSL, whose incidence rate has increased fivefold over the past 40 years, with its peak incidence occurring in those aged 75–84 years [3,4,5]. Between 15 to 25% of PCNSL patients have or will eventually develop ocular lymphoma [5]. Approximately 60–80% of PIOL patients develop central nervous system (CNS) disease within a mean of 29 months, which causes extremely poor prognosis [6,7,8]. PIOL primarily arises from the retina and vitreous body, in a few cases arising from the uveal and optic nerve [9, 10]. The most common histological subtype of PIOL is diffuse large B-cell lymphoma (DLBCL); rarely, T-cell lymphoma can be detected [11]. Patients often complain of floaters and blurred vision, and less commonly of red eye, photophobia, and ocular pain [12,13,14]. Establishing the diagnosis of PIOL is challenging as it usually presents as masquerade syndrome, imitates chronic uveitis, and may even respond to steroid treatment [15, 16]. The mean time from first symptom onset to definitive diagnosis ranges from 6 to 40 months [17, 18]. Histopathological analysis remains a cornerstone of diagnosing PIOL; however, rapid cell degeneration, small number of cells, and interfering impurity in the samples continue to make the analysis difficult [19]. The accuracy of PIOL diagnosis has been improved via immunocytochemistry, biochemical finding of elevated interleukin (IL)-10 levels with an IL-10:IL-6 ratio > 1.0, flow cytometry, and cellular microdissection with polymerase chain reaction amplification [16, 20]. When a diagnosis of PIOL is established, a patient should be referred to an oncologist, and a complete system review, especially CNS evaluation, should be performed [21].
Due to its rarity, the understanding of PIOL is mainly derived from small-sample retrospective studies [5,6,7]. Few epidemiological studies have reported on the incidence, demography, clinicopathology, and survival outcomes of PIOL. The Surveillance, Epidemiology, and End Results (SEER) database, which collects the incidence and survival information of cancer patients covering almost 28% of the population in the United States (US), provides valuable information on tumor characteristics and survival outcomes and is an especially vital resource for studies of rare cancers [22, 23].
Methods
Data source and study population
Study data were obtained from the SEER registry of the National Cancer Institute using the SEER*Stat software (version 8.4.0.1). To increase the representativeness of this study, PIOL patients were extracted from two databases from SEER: those diagnosed between 2000 and 2018 were extracted through the SEER 18 registry data [24], and patients diagnosed between 1992 and 1999 were extracted through the SEER 13 registry data [25]. The International Classification of Diseases for Oncology histological codes (9590–9599, 9650–9669, 9670–9729, 9735, 9737, 9738, 9811–9815, 9823, 9827, and 9837) were used for lymphoma combined with primary site codes (C69.2, C69.3, C69.4 and C69.9) to identify lymphoma primarily limited intraocular. The site eye, not otherwise specified (NOS) (C69.9), was used to refer to the vitreous. The patients were diagnosed by microscopic confirmation. The exclusion criteria were as follows: (1) patients who had prior cancer diagnoses, (2) patients diagnosed at autopsy or death certificate or without active follow-up, (3) patients who survived for 0 months or whose survival time was unknown, and (4) patients aged < 16 years in survival analysis, because the treatment modalities for children differ from those for adults (only two patients). As the SEER database is publicly available and all information is anonymized, this study was exempt from any institutional review board approval.
Study variables
The following variables were extracted from the SEER: patient ID, age at diagnosis, year of diagnosis, sex (female and male), race (White and others), primary site, laterality, histological type, surgery at the primary site (yes, no/unknown), radiation code (yes, no/unknown), chemotherapy code (yes, no/unknown), cause of death, survival month, Ann Arbor stage (AAS), and vital status.
The annual incidence of PIOL from 1992 to 2018 was calculated from the SEER 13 registry data to study the tendency of the incidence, and all incidence rates were standardized to the 2000 US standard population.
Statistical analyses
The incidence rates were calculated per 1,000,000 persons and were age-adjusted to the standard population of the US in 2000 using SEER*Stat version 8.4.0.1. The annual percentage change (APC) and 95% confidence interval (CI) were also calculated using the SEER*Stat software. The incidence of PIOL was statistically compared based on age, sex, and race using the chi-squared test.
Descriptive statistics were computed for all variables. All variables were converted to categorical variables, and presented as frequencies. We divided the patients into two groups, aged < 60 years and ≥ 60 years, and evaluated the differences in patients’ demographic and clinicopathological characteristics using the chi-squared test. Statistical significance was set to P < 0.05. Kaplan–Meier curves were used to analyze disease-specific survival (DSS), and the differences were estimated using the log-rank test. Univariate Cox proportional hazards models were applied in survival analysis. P values < 0.05 were considered statistically significant. Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS version 26.0, IBM SPSS statistics, IBM Corporation, Armonk, NY, USA) and R software (version 4.2.1).
Results
Incidence of PIOL
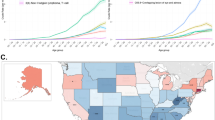
The overall incidence of PIOL was 0.23, which steadily increased from 1992 to 2018, with an APC of 2.35 (95% CI, 0.355–4.393; P < 0.05) (Fig. 1). The age-adjusted incidences of PIOL were 0.27 in 1992 and 0.19 in 1993. The incidences were 0.23 and 0.27 in 2017 and 2018, respectively. The incidence of PIOL increased with age, with the incidence significantly higher in patients aged ≥ 60 years (1.07) than in patients < 60 years (0.06). The incidence in men (0.24) was slightly higher than that in women (0.21), but the difference was not significant. Among the White population, the incidence was 0.24, which was significantly higher than that among other races (0.18) (Table 1).
Clinicopathological characteristics
In total, data from 326 patients were extracted from the SEER database, 197 (60.4%) of whom were female and 275 (84.4%) were White. The mean age of the patients at diagnosis was 66.1 ± 14.2 years, with a wide range of 8–97 years, and 235 (72.1%) patients were aged ≥ 60 years. The vitreous (68.7%) was the most common primary site, followed by the ciliary body (20.2%), choroid (7.4%), and retina (3.7%). Among diverse pathological types, the most common type was DLBCL (30.4%), followed by mucosa-associated lymphoid tissue (MALT) lymphoma (27%), others/unclassified types (25.5%), and non-Hodgkin lymphoma (NHL) (17.2%). The pathological types between the groups aged < 60- and ≥ 60 were significantly different. In the younger group, MALT lymphoma (40.7%) was the most common pathological type, whereas in the elderly group, DLBCL (34.5%) was the most common. Based on AAS, patients with stage I and II were the most common, accounting for 64.1%, and 9.5% of the patients had stage III and IV. The remaining patients (26.4%) had unknown stage. More unilateral lesions (84%) than bilateral lesions (13.5%) were observed in patients at first presentation, and laterality was unknown in 2.5% of the patients. Patients’ baseline characteristics are summarized in Table 2.
Survival analysis
The DSS of all PIOL patients is shown in Fig. 2. Up to 156 patients died by the end of follow-up, and 90 of them died of PIOL. The 1-, 5-, and 10-year DSS rates were 92.9%, 74.2%, and 61.5%, respectively. Survival curves stratified by age, years of diagnosis, sex, race, laterality, primary site, pathological type, AAS, and treatment modality were constructed according to the Kaplan–Meier survival analysis. The analysis revealed that age ≥ 60 years was significantly associated with poor DSS (Fig. 3a). The DSS rates of patients diagnosed in 2003 − 2012 and 2013 − 2018 were significantly higher than that of patients diagnosed in 1992–2002 (both P < 0.05) (Fig. 3b). However, sex (Fig. 3c) and race (Fig. 3d) had no effect on DSS. According to primary sites, patients with lymphoma in the retina had the worst prognosis, whereas patients with lymphoma in the choroid had longer DSS (Fig. 4a). Among the various histological subtypes of PIOL, MALT lymphoma was associated with better DSS than other subtypes, and DLBCL had the worst DSS (Fig. 4b). The survival analysis revealed that laterality and AAS had no effect on DSS (Fig. 4c and d). In terms of treatment strategies, surgery (Fig. 5a), radiation (Fig. 5b), and chemotherapy (Fig. 5c) did not lead to better prognosis.
The whole cohort was analyzed using log-rank tests and univariate Cox proportional hazards models, which revealed that age, years of diagnosis, primary site, pathological type, and chemotherapy had an effect on DSS. The result of the log-rank tests stratified by age is shown in Table 3. Variables that exhibited P < 0.05 in the univariate Cox regression analysis were included in the multivariable Cox regression analysis, identified that age, pathological type, and chemotherapy were independent prognostic factors for the DSS of PIOL (Table 4).
Discussion
Considering the rarity of PIOL, few population-based studies of PIOL have been conducted. The current study used the SEER database, a prominent resource for research on rare malignancies, to conduct this population-based cohort study of PIOL and obtain an in-depth understanding of this disease.
This study found that the overall age-adjusted incidence of PIOL in the US was 0.23, with an upward trend over three decades, and the incidence in 2018 was 0.27. The increasing trend may be attributed to the increased numbers of immunodeficient and immunosuppressed patients, prolonged life expectancy, and advances in diagnostic methods [15].
In line with previous studies [26], this study revealed a mean age at diagnosis of 66.1 years. The youngest patient in this study was only 8 years old; such a young age is extremely rare in PIOL. The incidence of PIOL in individuals aged ≥ 60 years was nearly 18 times higher than in those aged < 60 years. Meanwhile, advanced age was related to worse DSS. Elderly people often have more comorbidities than younger individuals do and so cannot endure intensive treatments with high toxicity; this has an adverse effect on prognosis [27, 28]. Consistent with previous studies, DLBCL was the most common histological subtype of PIOL, followed by MALT lymphoma, and DLBCL was more common in the elderly than in younger individuals, which may affect the survival time of these patients [5, 11, 29, 30].
Compared with lymphomas in other primary sites of PIOL, those in the choroid and ciliary body have better prognoses, which is mainly due to the radiation sensitivity and less aggressive clinical course of those sites [31,32,33]. Meanwhile, lymphomas in the retina and vitreous were associated with poor prognosis because they usually present as high-grade lymphomas and are often associated with CNS lymphoma [33, 34]. Unilateral PIOL did not correlate with better survival and may require positive treatments, similar to patients with bilateral disease, which conforms with the guidelines of the British Neuro-Oncology Society [35].
There are no uniform treatment protocols or guidelines for PIOL. Available treatments aim to remit the intraocular disease to preserve patients’ visual acuity and prevent CNS involvement, which is a major cause of death in PIOL patients [5, 18]. The comprehensive treatment strategies for PIOL include local treatment, such as ocular radiotherapy and intravitreal chemotherapy; systemic treatment, mainly depending on high doses of methotrexate; and a combination of both. The International Primary Central Nervous System Lymphoma Collaborative Group (IPCG) recommends local therapy for unilateral PIOL. If both eyes are involved, there is still a preference for local treatment, and systemic treatment should also be applied, if necessary [5]. However, the British Neuro-Oncology Society suggests ocular irradiation combined with systemic chemotherapy [36].
Radiation was the most commonly used therapy in our study. The radiation regimen for lymphoma localized in the eye usually varies from 30 to 45 Gy in approximately 15 fractions, and radiation should be performed in both eyes because PIOL always develops bilaterally [5, 37]. Although ocular irradiation may cause cataract, radiation retinopathy, or optic neuropathy, its benefits outweigh its complications [8, 36].
Intravitreal chemotherapy was proposed and used as a local treatment for PIOL in the 1990s, which improved the treatment outcomes of PIOL and decreased its morbidity [38]. Methotrexate (dose, 400 μg in 0.1 ml) is the main drug for intravitreal chemotherapy, and the number of total injections can be modulated according to the patient’s clinical response [39,40,41]. A single-center retrospective study in China including 16 patients (28 eyes) with intraocular lymphoma reported that local therapy may preserve visual acuity [42]. Rituximab has also been used for intravitreal injections, which may necessitate fewer injections and entail lower toxicity [43,44,45].
Systemic chemotherapy with methotrexate, a treatment mainly based on experience with PCNSL, is considered when the disease develops in both eyes or involves the CNS [18, 46]. However, the efficacy of combination therapy, namely, systemic chemotherapy combined with local treatment, to decrease the risk of CNS relapse remains controversial due to the inconsistent results of retrospective studies on PIOL [17, 18]. The IPCG analyzed the treatment outcomes in PCNSL patients with ocular involvement and concluded that ocular treatment prolonged disease control, but did not affect the prognosis or ocular recurrence risk [47]. Other studies also reported that local treatment was effective in eliminating tumor cells in the eyes, but it could not control CNS relapse [18]. However, a meta-analysis of 83 studies suggested that intravitreal injection combined with systemic chemotherapy could prolong survival in patients with CNS involvement, and that combining it with radiotherapy further reduced recurrence and mortality rates [48].
Via multivariable Cox regression analysis, our study identified chemotherapy as an independent risk factor for prognosis. Our additional analyses revealed that the proportion of DLBCL in patients who received chemotherapy was high (P < 0.001), which might have caused biases [18, 48]. Different chemotherapeutic modalities may affect the prognosis of PIOL patients; however, detailed information on chemotherapy cannot be extracted from the SEER database. Thus, further analysis of chemotherapy is not feasible.
The survival of PIOL patients has been improving, partly due to the development of diagnostic tools, including imaging, blood testing, immunocytological/histological evaluation, biochemical analysis, and more optimal diagnostic panels, namely, the combination of cytologic smears, immunohistochemistry, and cytokine analysis [49,50,51]. Melphalan, temozolomide, lenalidomide with or without rituximab, and ibrutinib have also shown promising results for PIOL [52,53,54,55,56].
This study had some limitations. First, this retrospective study was based on the SEER data, which might have caused unavoidable biases. Due to the rarity of PIOL, a large prospective study seems impractical. Second, detailed data on radiotherapy administration protocols, chemotherapy regimens, and surgical approaches are missing from the SEER database. Thus, specific treatment regimens could not be accurately determined. Third, the SEER program provided limited information on the extension of lymphoma in PIOL patients, and CNS progression is believed to prominently affect the survival of these patients. Fourth, the SEER database does not have a specialized code for the vitreous, so this study used the site “eye, NOS” to denote the vitreous, because other sites have separate codes and this particular site has been considered the vitreous in previous studies [57]. Overall, these limitations are common in studies based on SEER data. Nonetheless, the SEER remains a significant source for studying rare tumors, taking these limitations into account. The present study provides important insights for PIOL and valuable information on the incidence, prognostic factors, and survival outcomes in PIOL.
Conclusions
The present study shows that PIOL is a rare type of lymphoma with a poor prognosis and an increasing incidence trend. It mostly affects individuals aged ≥ 60 years, and DLBCL is its most common pathological type. For PIOL patients, survival analysis showed that age < 60 years and non-DLBCL pathological types are associated with good survival. The survival of patients with PIOL has improved over years.
Availability of data and materials
Data can be extracted from the SEER database after completing their agreement form and requesting access from their website (https://seer.cancer.gov).
Change history
09 February 2023
A Correction to this paper has been published: https://doi.org/10.1186/s12886-023-02781-z
Abbreviations
- PIOL:
-
Primary intraocular lymphoma
- PCNSL:
-
Primary central nervous system lymphoma
- CNS:
-
Central nervous system
- DLBCL:
-
Diffuse large B-cell lymphoma
- IL:
-
Interleukin
- SEER:
-
Surveillance, Epidemiology, and End Results
- AAS:
-
Ann Arbor stage
- APC:
-
Annual percentage change
- CI:
-
Confidence interval
- DSS:
-
Disease-specific survival
- MALT:
-
Mucosa-associated lymphoid tissue
- NHL:
-
Non-Hodgkin lymphoma
- IPCG:
-
International Primary Central Nervous System Lymphoma Collaborative Group
References
Buggage RR, Chan CC, Nussenblatt RB. Ocular manifestations of central nervous system lymphoma. Curr Opin Oncol. 2001;13(3):137–42. https://doi.org/10.1097/00001622-200105000-00001.
Faia LJ, Chan CC. Primary intraocular lymphoma. Arch Pathol Lab Med. 2009;133(8):1228–32. https://doi.org/10.1043/1543-2165-133.8.1228.
Lv C, et al. Primary central nervous system lymphoma in the United States, 1975–2017. Ther Adv Hematol. 2022;13:20406207211066170. https://doi.org/10.1177/20406207211066166.
Mendez JS, et al. The elderly left behind-changes in survival trends of primary central nervous system lymphoma over the past 4 decades. Neuro Oncol. 2018;20(5):687–94. https://doi.org/10.1093/neuonc/nox187.
Chan CC, et al. Primary vitreoretinal lymphoma: a report from an International Primary Central Nervous System Lymphoma Collaborative Group symposium. Oncologist. 2011;16(11):1589–99. https://doi.org/10.1634/theoncologist.2011-0210.
Ma WL, et al. Clinical outcomes of primary intraocular lymphoma patients treated with front-line systemic high-dose methotrexate and intravitreal methotrexate injection. Ann Hematol. 2016;95(4):593–601. https://doi.org/10.1007/s00277-015-2582-x.
Chan CC, Wallace DJ. Intraocular lymphoma: update on diagnosis and management. Cancer Control. 2004;11(5):285–95. https://doi.org/10.1177/107327480401100502.
Berenbom A, et al. Treatment outcomes for primary intraocular lymphoma: implications for external beam radiotherapy. Eye (Lond). 2007;21(9):1198–201. https://doi.org/10.1038/sj.eye.6702437.
Levy-Clarke GA, Chan CC, Nussenblatt RB. Diagnosis and management of primary intraocular lymphoma. Hematol Oncol Clin North Am. 2005;19(4):739–49. https://doi.org/10.1016/j.hoc.2005.05.011 (viii).
Touhami S, et al. Neoplasia and intraocular inflammation: From masquerade syndromes to immunotherapy-induced uveitis. Prog Retin Eye Res. 2019;72:100761. https://doi.org/10.1016/j.preteyeres.2019.05.002.
Hoffman PM, et al. Intraocular lymphoma: a series of 14 patients with clinicopathological features and treatment outcomes. Eye (Lond). 2003;17(4):513–21. https://doi.org/10.1038/sj.eye.6700378.
Gill MK, Jampol LM. Variations in the presentation of primary intraocular lymphoma: case reports and a review. Surv Ophthalmol. 2001;45(6):463–71. https://doi.org/10.1016/s0039-6257(01)00217-x.
Velez G, Chan CC, Csaky KG. Fluorescein angiographic findings in primary intraocular lymphoma. Retina. 2002;22(1):37–43. https://doi.org/10.1097/00006982-200202000-00007.
Abu Samra K, et al. Intraocular Lymphoma: Descriptive Data of 26 Patients Including Clinico-pathologic Features, Vitreous Findings, and Treatment Outcomes. Ocul Immunol Inflamm. 2018;26(3):347–52. https://doi.org/10.1080/09273948.2016.1193206.
Tang LJ, Gu CL, Zhang P. Intraocular lymphoma. Int J Ophthalmol. 2017;10(8):1301–7. https://doi.org/10.18240/ijo.2017.08.19.
Sagoo MS, et al. Primary intraocular lymphoma. Surv Ophthalmol. 2014;59(5):503–16. https://doi.org/10.1016/j.survophthal.2013.12.001.
Grimm SA, et al. Primary intraocular lymphoma: an International Primary Central Nervous System Lymphoma Collaborative Group Report. Ann Oncol. 2007;18(11):1851–5. https://doi.org/10.1093/annonc/mdm340.
Soussain C, Malaise D, Cassoux N. Primary vitreoretinal lymphoma: a diagnostic and management challenge. Blood. 2021;138(17):1519–34. https://doi.org/10.1182/blood.2020008235.
Coupland SE, et al. Evaluation of vitrectomy specimens and chorioretinal biopsies in the diagnosis of primary intraocular lymphoma in patients with Masquerade syndrome. Graefes Arch Clin Exp Ophthalmol. 2003;241(10):860–70. https://doi.org/10.1007/s00417-003-0749-y.
Sugita S, et al. Diagnosis of intraocular lymphoma by polymerase chain reaction analysis and cytokine profiling of the vitreous fluid. Jpn J Ophthalmol. 2009;53(3):209–14. https://doi.org/10.1007/s10384-009-0662-y.
Hoang-Xuan K, et al. Diagnosis and treatment of primary CNS lymphoma in immunocompetent patients: guidelines from the European Association for Neuro-Oncology. Lancet Oncol. 2015;16(7):e322-32. https://doi.org/10.1016/S1470-2045(15)00076-5.
Xiao M, et al. The incidence and survival outcomes of patients with primary cardiac lymphoma: A SEER-based analysis. Hematol Oncol. 2020;38(3):334–43. https://doi.org/10.1002/hon.2741.
Lin S, et al. Clinicopathological characteristics and survival outcomes in breast carcinosarcoma: A SEER population-based study. Breast. 2020;49:157–64. https://doi.org/10.1016/j.breast.2019.11.008.
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence - SEER Research Plus Data, 18 Registries, Nov 2020 Sub (2000–2018) - Linked To County Attributes - Total U.S., 1969–2019 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2021, based on the November 2020 submission.
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence - SEER Research Plus Data, 13 Registries, Nov 2020 Sub (1992–2018) - Linked To County Attributes - Total U.S., 1969–2019 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2021, based on the November 2020 submission.
Mochizuki M, Singh AD. Epidemiology and clinical features of intraocular lymphoma. Ocul Immunol Inflamm. 2009;17(2):69–72. https://doi.org/10.1080/09273940902957305.
Daras M, DeAngelis LM. Management of elderly patients with primary central nervous system lymphoma. Curr Neurol Neurosci Rep. 2013;13(5):344. https://doi.org/10.1007/s11910-013-0344-5.
Siegal T, Bairey O. Primary CNS Lymphoma in the Elderly: The Challenge. Acta Haematol. 2019;141(3):138–45. https://doi.org/10.1159/000495284.
Hormigo A, et al. Ocular presentation of primary central nervous system lymphoma: diagnosis and treatment. Br J Haematol. 2004;126(2):202–8. https://doi.org/10.1111/j.1365-2141.2004.05028.x.
Chiappella A, et al. Diffuse Large B-cell Lymphoma in the elderly: standard treatment and new perspectives. Expert Rev Hematol. 2017;10(4):289–97. https://doi.org/10.1080/17474086.2017.1305264.
Coupland SE, et al. Diagnosis of a primary uveal extranodal marginal zone B-cell lymphoma by chorioretinal biopsy: case report. Graefes Arch Clin Exp Ophthalmol. 2005;243(5):482–6. https://doi.org/10.1007/s00417-004-1050-4.
Cockerham GC, et al. Re-evaluation of “reactive lymphoid hyperplasia of the uvea”: an immunohistochemical and molecular analysis of 10 cases. Ophthalmology. 2000;107(1):151–8. https://doi.org/10.1016/s0161-6420(99)00025-1.
Coupland SE, Heimann H, Bechrakis NE. Primary intraocular lymphoma: a review of the clinical, histopathological and molecular biological features. Graefes Arch Clin Exp Ophthalmol. 2004;242(11):901–13. https://doi.org/10.1007/s00417-004-0973-0.
Coupland SE, Damato B. Understanding intraocular lymphomas. Clin Exp Ophthalmol. 2008;36(6):564–78. https://doi.org/10.1111/j.1442-9071.2008.01843.x.
British Neuro-Oncology Society; National Cancer Action Team. Rare Brain and CNS Tumours Guidelines: Guidelines on the Diagnosis and Management of Adult Pineal Area Tumours. Published June 2011. http://www.bnos.org.uk/wp-content/uploads/2015/08/Guidelines-on-the-Diagnosis-and-Management.pdf. Accessed 6 Apr 2016.
Davis JL. Intraocular lymphoma: a clinical perspective. Eye (Lond). 2013;27(2):153–62. https://doi.org/10.1038/eye.2012.250.
Isobe K, et al. Treatment of primary intraocular lymphoma with radiation therapy: a multi-institutional survey in Japan. Leuk Lymphoma. 2006;47(9):1800–5. https://doi.org/10.1080/10428190600632881.
Fishburne BC, et al. Intravitreal methotrexate as an adjunctive treatment of intraocular lymphoma. Arch Ophthalmol. 1997;115(9):1152–6. https://doi.org/10.1001/archopht.1997.01100160322009.
Frenkel S, et al. Intravitreal methotrexate for treating vitreoretinal lymphoma: 10 years of experience. Br J Ophthalmol. 2008;92(3):383–8. https://doi.org/10.1136/bjo.2007.127928.
Pulido JS, et al. The diagnosis and treatment of primary vitreoretinal lymphoma: a review. Int J Retina Vitreous. 2018;4:18. https://doi.org/10.1186/s40942-018-0120-4.
Klimova A, et al. Combined treatment of primary vitreoretinal lymphomas significantly prolongs the time to first relapse. Br J Ophthalmol. 2018;102(11):1579–85. https://doi.org/10.1136/bjophthalmol-2017-311574.
Di Y, et al. Clinical features and treatment outcomes of intraocular lymphoma: a single-center experience in China. Int J Ophthalmol. 2021;14(4):574–81. https://doi.org/10.18240/ijo.2021.04.15.
Raja H, et al. Effect of intravitreal methotrexate and rituximab on interleukin-10 levels in aqueous humor of treated eyes with vitreoretinal lymphoma. PLoS One. 2013;8(6):e65627. https://doi.org/10.1371/journal.pone.0065627.
Itty S, Pulido JS. Rituximab for intraocular lymphoma. Retina. 2009;29(2):129–32. https://doi.org/10.1097/IAE.0b013e318192f574.
Larkin KL, et al. Use of intravitreal rituximab for treatment of vitreoretinal lymphoma. Br J Ophthalmol. 2014;98(1):99–103. https://doi.org/10.1136/bjophthalmol-2013-304043.
Hearne E, Netzer OT, Lightman S. Learning points in intraocular lymphoma. Eye (Lond). 2021;35(7):1815–7. https://doi.org/10.1038/s41433-021-01500-6.
Grimm SA, et al. Primary CNS lymphoma with intraocular involvement: International PCNSL Collaborative Group Report. Neurology. 2008;71(17):1355–60. https://doi.org/10.1212/01.wnl.0000327672.04729.8c.
Zhao XY, et al. Clinical Features, Diagnosis, Management and Prognosis of Primary Intraocular Lymphoma. Front Oncol. 2022;12:808511. https://doi.org/10.3389/fonc.2022.808511.
Jahnke K, et al. Diagnosis and management of primary intraocular lymphoma: an update. Clin Ophthalmol. 2007;1(3):247–58.
Takhar JS, Doan TA, Gonzales JA. Primary vitreoretinal lymphoma: empowering our clinical suspicion. Curr Opin Ophthalmol. 2019;30(6):491–9. https://doi.org/10.1097/ICU.0000000000000620.
Santos MC, et al. Vitreoretinal Lymphoma: Optimizing Diagnostic Yield and Accuracy. Am J Ophthalmol. 2022;236:120–9. https://doi.org/10.1016/j.ajo.2021.09.032.
Baron M, et al. Temozolomide is effective and well tolerated in patients with primary vitreoretinal lymphoma. Blood. 2020;135(20):1811–5. https://doi.org/10.1182/blood.2019003073.
Ghesquieres H, et al. Lenalidomide in combination with intravenous rituximab (REVRI) in relapsed/refractory primary CNS lymphoma or primary intraocular lymphoma: a multicenter prospective “proof of concept” phase II study of the French Oculo-Cerebral lymphoma (LOC) Network and the Lymphoma Study Association (LYSA)dagger. Ann Oncol. 2019;30(4):621–8. https://doi.org/10.1093/annonc/mdz032.
Hou K, et al. Efficacy and safety of ibrutinib in diffuse large B-cell lymphoma: A single-arm meta-analysis. Crit Rev Oncol Hematol. 2020;152:103010. https://doi.org/10.1016/j.critrevonc.2020.103010.
Rubenstein JL, et al. Phase 1 investigation of lenalidomide/rituximab plus outcomes of lenalidomide maintenance in relapsed CNS lymphoma. Blood Adv. 2018;2(13):1595–607. https://doi.org/10.1182/bloodadvances.2017014845.
Shields CL, et al. Intravitreal Melphalan for Treatment of Primary Vitreoretinal Lymphoma: A New Indication for an Old Drug. JAMA Ophthalmol. 2017;135(7):815–8. https://doi.org/10.1001/jamaophthalmol.2017.1810.
Ahmed AH, Foster CS, Shields CL. Association of Disease Location and Treatment With Survival in Diffuse Large B-Cell Lymphoma of the Eye and Ocular Adnexal Region. JAMA Ophthalmol. 2017;135(10):1062–8. https://doi.org/10.1001/jamaophthalmol.2017.3286.
Acknowledgements
Not applicable.
Funding
This work was supported by grants of National Natural Science Foundation of China (81570885 and 81770959), and Talent Development Program of Changzheng Hospital (YQ722).
Author information
Authors and Affiliations
Contributions
Rui-li Wei designed and supervised the study. Lin-feng He and Jin-di Zhang extracted the data and performed the statistical analyses. Xin-xin Chen and Lin-feng He drafted the manuscript. All authors approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was evaluated by the Ethics Committee of Changzheng Hospital and deemed not to require ethics approval.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: “The article has been updated to correct Figs. 5B, 5C, Tables 2,3,4, Results and Discussion sections.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
He, Lf., Zhang, Jd., Chen, Xx. et al. Epidemiology and survival outcomes of patients with primary intraocular lymphoma: a population-based analysis. BMC Ophthalmol 22, 486 (2022). https://doi.org/10.1186/s12886-022-02702-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-022-02702-6