Abstract
Purpose:
To investigate the surgical results of the non-adjustable suture technique under general anesthesia for the correction of acute acquired comitant esotropia.
Study design:
Retrospective case study.
Methods:
Patients with acute acquired comitant esotropia who underwent corrective surgery from September 2008 to June 2018 were included. Surgical treatment was conducted based on the measured maximum angle after occlusion for at least 1 h; all surgeries were performed using the non-adjustable suture technique under general anesthesia. Motor success was categorized into three groups: good, ortho; fair, 2 to 8 prism diopters (PD); and poor, over 8 PD. Sensory success was divided into two groups: good (no diplopia with binocular vision) and poor (no stereopsis with diplopia).
Results:
40 patients (21 male and 19 female, 28.78 ± 15.32 years old) were included. Preoperative esodeviation was 28.0 ± 12.8 PD. Mean refractive error was − 2.5 ± 2.5 D (spherical equivalent). After the occlusion of one eye, 14 patients (35%) showed an esodeviation increase of more than 5 PD. There were 70% good, 25% fair, and 5% poor outcomes regarding motor success. 96% of the patients demonstrated good sensory success.
Conclusion:
The non-adjustable correction based on the maximum angle after 1 h had a relatively excellent motor and sensory success rate.
Similar content being viewed by others
Introduction
Acute acquired comitant esotropia (AACE) is an acute-onset esotropia with diplopia in older children and adults; notably, neurological examinations in these patients, including imaging tests, reveal negative results [1]. These features can distinguish AACE from other types of esotropia, such as infantile esotropia, accommodative esotropia, and paralytic strabismus.
Few reports of corrective surgical results have been published. Spierer reported that ten patients had good corrective surgical results [all patients were orthophoric or minimally esophoric and exhibited good stereopsis (40 s)] [2]. However, Sturm et al. revealed motor success within eight prism diopters (PD) in 92% of the patients; sensory success was present in only 60% [3]. Lee and Kim suggested that increasing the surgical dose is recommended to correct the sensory and motor success [4]. In order to increase the success rate, the adjustable suture technique is considerable. However, there is controversy regarding the success rates between adjustable and non-adjustable suture techniques [5]. Moreover, topical anesthesia has some side effects, including cardiac problems and pain [6, 7]. Therefore, we investigated the clinical features and surgical outcomes of the non-adjustable suture technique under general anesthesia in AACE patients.
Methods
The study was a non-randomized, retrospective review of the medical records of 40 patients who were diagnosed with acute acquired comitant esotropia at Kim’s Eye Hospital between 2008 and 2016.
All patients showed comitant deviation in alternating gaze. We excluded patients under ten years old or a history of any of the following: ocular surgery, abnormal central nervous system findings, amblyopia, or head trauma. In order to focus on the Franceschetti type of AACE, AACE that developed after occlusion and orthotropia at near distance was excluded. The study was approved by the Institutional Review Board of Kim’s Eye Hospital and was conducted in accordance with the tenets of the Declaration of Helsinki. The IRB board of Kim’s Eye Hospital waived the requirement to obtain informed consent.
Full ophthalmologic examinations were performed, including slit-lamp examination, cycloplegic refraction, and alternate cover test. One eye with higher refractive errors was chosen in each patient, in order to investigate the relationship between refractive errors and esodeviation. All surgeries were performed under general anesthesia by one surgeon. The non-adjustable suture technique was used.
In order to determine the angle of surgery, the maximum deviation was measured after 1 h of occlusion. Preoperative and postoperative horizontal deviations were measured from a distance by using the alternating prism cover test with correction. Surgical success was divided into the motor and sensory successes. Motor and sensory successes were defined as shown in Table 1. The deviation was measured at a far distance. Sensory testing was performed by the Lang I stereotest (Lang-Stereotest AG, Küsnacht, Switzerland); the stereopsis result was positive when the patients could distinguish all three figures.
Data were analyzed using SPSS 18.0 for Windows (SPSS Inc., Chicago, IL, USA). The Spearman correlation test was evaluated the relationship between refractive errors and postoperative deviation.
Results
A total of 40 patients (21 male and 19 female) were included [mean age, 28.8 years (12–68 years)). Thirty-three of 40 underwent bilateral medial rectus muscle recession (BMR), and unilateral lateral rectus muscle resection and medial rectus muscle recession (RNR) were performed in seven patients. The surgical dose was performed according to Parks’ table.
Preoperative esodeviation was 28.0 ± 12.8 prism diopters (PD) (Fig. 1); esodeviation increased more than 5 PD after 1-hour occlusion in 14 of 40 patients (35%). The increase in esodeviation after occlusion was an average of 9.5 PD (range, 5–35 PD).
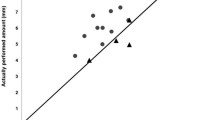
The mean refractive error was − 2.5 D ± 2.5 D (spherical equivalent). There were seven hyperopic patients, 27 mild myopic patients (less than − 5 diopters), and six highly myopic patients. Patients with higher myopia tend to exhibit greater esodeviation than both less myopic and hyperopic patients (r = 0.297, p = 0.026) (Fig. 2).
The mean follow-up period was 17.2 ± 3.4 months. Motor success was obtained in all 40 patients; we could investigate sensory success in 28. 95% of the patients showed more than fair motor success. In the all fail motor groups, two out of 40 patients underwent bilateral medial rectus recession. After surgery, the greatest esodeviation was 12 PD; however, this patient showed normal stereopsis (Fig. 3). 93% of the patients had good stereopsis after surgery, and two patients who had no stereopsis showed 10 PD esodeviation (Table 2).
Discussion
This study showed that the results of non-adjustable surgery under general anesthesia for AACE are favorable in both motor and sensory aspects.
AACE can be categorized into three types: [1, 8] (1) Swan type, which develops after occlusion; (2) Franceschetti type, which exhibits a minimal amount of hypermetropia without underlying causes; (3) Bielschowsky type, which is related to uncorrected myopia of -5 D or greater. The present study excluded AACE that developed after occlusion or orthotropia at near distance. Recently, a new classification for AACE has been implemented, in which seven types of AACE are suggested (1) acute accommodative, (2) decompensated monofixation syndrome, (3) idiopathic, (4) the intracranial disease, (5) occlusion-related, (6) different etiology, and (7) cyclic type) [9]. Initially, we excluded patients with intracranial disease, different etiology, occlusion-related, and cyclic AACE. Our results are somewhat ambiguous in that classification depended on the three classical types of AACE, but the present patients had the Franceschetti type of AACE. However, most patients could be categorized as idiopathic.
More myopic patients showed greater esodeviation, which could be due to excessive near distance requirement in the myopia group, according to Bielschowsky’s theory [10, 11]. Myopia patients were the most common group in a Chinese AACE study [12], and the present study showed a similar result. AACE in adults can be associated with myopia [2]. However, this myopic preponderance may be epidemiological bias [13]. In cases of AACE related to hyperopia, full correction with glasses would help restore binocularity [14]. Esodeviation was not corrected with glasses in any of the present cases. Lee and Kim also mentioned that refractive errors had no significant relation to success rate [4].
Surgical studies regarding AACE have revealed favorable surgical results [2, 14, 15]. In order to improve surgical results, variable methods such as increasing surgical dose, preoperative prism adaptation, consideration of surgical methods, and adjustable surgery could be considerate [4, 15, 16]. Williams and Hoyt reported that stereopsis could be achieved after surgical treatment of AACE without neurologic abnormalities [17]. However, the previous study involved surgery with the adjustable technique. Our surgical results under general anesthesia revealed a favorable outcome and targeting the maximum angle of esodeviation after occlusion is a pivotal factor in improving the success rate. In the present study, failure of motor success was not found in unilateral RNR patients. Even though unilateral RNR has a more favorable motor outcome, the number of patients seems to be insufficient to analyze the effect of surgical methods.
This study has some limitations. We could not directly compare topical anesthesia, adjustable suture technique, and general anesthesia. Although topical anesthesia has advantages, such as surgical time, cost, and superior surgical results [18, 19], it could allow the sensation of pain during surgery, and intraoperative bradycardia, tachycardia, and asystole by oculocardiac reflex [7, 20]. The adjustable technique may provide better surgical outcomes based on the refined realignment of ocular muscles; however, there was no evidence of improved surgical outcomes in patients undergoing adjustable surgery [5, 21]. In addition, this study had no control group. Therefore, it was impossible to study whether this method was better or worse than the other methods such as adjustable surgery or techniques using other measurements of strabismus angle.
Conclusion
A surgical correction based on the maximum angle after 1 h of occlusion showed a favorable motor and sensory success rate. Therefore, the non-adjustable suture technique under general anesthesia could be considered in AACE patients to avoid the side effects of topical anesthesia and the adjustable technique.
Availability of data and material
The data used to support the findings of this study are available from the corresponding author upon request.
References
Clark AC, Nelson LB, Simon JW, Wagner R, Rubin SE. Acute acquired comitant esotropia. Br J Ophthalmol. 1989;73:636–8.
Spierer A. Acute concomitant esotropia of adulthood. Ophthalmology. 2003;110:1053–6.
Sturm V, Menke MN, Knecht PB, Schoffler C. Long-term follow-up of children with acute acquired concomitant esotropia. J aapos. 2011;15:317–20.
Lee HJ, Kim SJ. Clinical characteristics and surgical outcomes of adults with acute acquired comitant esotropia. Jpn J Ophthalmol. 2019;63:483–9.
Hassan S, Haridas A, Sundaram V. Adjustable versus non-adjustable sutures for strabismus. Cochrane Database Syst Rev. 2018;3:Cd004240.
Gold RS, Pollard Z, Buchwald IP. Asystole due to the oculocardiac reflex during strabismus surgery: a report of two cases. Ann Ophthalmol. 1988;20:473–5, 477.
Gopal KSS, Kelkar JA, Arora ER. Our experience with strabismus surgery under topical anesthesia performed at a tertiary eye care center. Indian J Ophthalmol. 2018;66:342–3.
Burian HM, Miller JE. Comitant convergent strabismus with acute onset. Am J Ophthalmol. 1958;45:55–64.
Buch H, Vinding T. Acute acquired comitant esotropia of childhood: a classification based on 48 children. Acta Ophthalmol. 2015;93:568–74.
Hoyt CS, Good WV. Acute onset concomitant esotropia: when is it a sign of serious neurological disease? Br J Ophthalmol. 1995;79:498–501.
Cai C, Dai H, Shen Y. Clinical characteristics and surgical outcomes of acute acquired Comitant Esotropia. BMC Ophthalmol. 2019;19:173.
Chen J, Deng D, Sun Y, et al. Acute Acquired Concomitant Esotropia: Clinical features, Classification, and Etiology. Med (Baltim). 2015;94:e2273.
Lim HT, Yoon JS, Hwang SS, Lee SY. Prevalence and associated sociodemographic factors of myopia in Korean children: the 2005 third Korea National Health and Nutrition Examination Survey (KNHANES III). Jpn J Ophthalmol. 2012;56:76–81.
Lyons CJ, Tiffin PA, Oystreck D. Acute acquired comitant esotropia: a prospective study. Eye (Lond). 1999;13(Pt 5):617–20.
Kim DH, Noh HJ. Surgical outcomes of acute acquired comitant esotropia of adulthood. BMC Ophthalmol. 2021;21:45.
Velez FG, Rosenbaum AL. Preoperative prism adaptation for acquired esotropia: long-term results. J AAPOS. 2002;6:168–73.
Williams AS, Hoyt CS. Acute comitant esotropia in children with brain tumors. Arch Ophthalmol. 1989;107:376–8.
He X, Chen L, Pan X, Hu H, Shi Z. Application value of topical aneasthesia in children strabismus surgery. Eye Sci. 2012;27:134–7.
Seijas O, Gomez de Liano P, Merino P, Roberts CJ, Gomez de Liano R. Topical anesthesia in strabismus surgery: a review of 101 cases. J Pediatr Ophthalmol Strabismus. 2009;46:218–22.
Min SW, Hwang JM. The incidence of asystole in patients undergoing strabismus surgery. Eye (Lond). 2009;23:864–6.
Kamal AM, Abozeid D, Seif Y, Hassan M. A comparative study of adjustable and non-adjustable sutures in primary horizontal muscle surgery in children. Eye (Lond). 2016;30:1447–51.
Acknowledgements
None.
Funding
This research was supported by the Chung-Ang University Research Grants in 2022.
Author information
Authors and Affiliations
Contributions
USK: Conception of the study and supervision. SHL & YGL: data acquisition and analysis. YGL : writing the manuscript. All authors: Designing the work, interpretation of the data and substantive revision of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board of Kim’s Eye Hospital in Korea and followed the stipulations of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors have declared that no competing interests exist.
Financial interests
The authors have no financial interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lim, S.H., Lee, Y.G. & Kim, U.S. Non-adjustable surgery for acute acquired comitant esotropia under general anesthesia. BMC Ophthalmol 22, 416 (2022). https://doi.org/10.1186/s12886-022-02634-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-022-02634-1