Abstract
Background
Xen is a device for minimally invasive glaucoma surgery, and is used to treat POAG, pseudoexfoliative or pigmentary glaucoma, as well as refractory glaucoma. The efficacy of XEN in treating glaucoma remains to be confirmed and clarified. Hence, we conducted a systematic review and meta-analysis to examine the efficacy and associated complication of XEN implantations.
Methods
We conducted a literature search in PubMed, EMBASE, the Cochrane Library of Systematic Reviews, Web of Science, China National Knowledge Infrastructure, WanFang and SinoMed databases to identify studies, published before May 15, 2021, which evaluated XEN in glaucoma, and parameters for measurements included intra-ocular pressure (IOP), number of anti-glaucoma medications (NOAM), and bleb needling rate. We compared the measurements of XEN-only procedure between phaco-XEN and trabeculectomy, and we also did sub-analysis based on time points, glaucoma types, ethnics, etc. Sensitivity analyses and publication bias were conducted for evaluating bias.This study followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA 2020) reporting guideline.
Results
We identified 78 eligible studies, analysis revealed obvious IOP reduction after XEN stent implantation (SMD: 1.69, 95% CI 1.52 to 1.86, p value < 0.001) and NOAM reduction (SMD: 2.11, 95% CI 1.84 to 2.38, p value < 0.001). Sub-analysis showed no significant difference with respect to time points, ethnicities, and economic status. No significant difference was found between XEN treatment effect on POAG and PEXG eyes and between pseudo-phakic and phakic eyes. Also no significant difference was found between XEN and phaco-XEN surgery in terms of IOP after surgery (SMD: -0.01, 95% CI -0.09 to 0.08, p value 0.894). However, NOAM (after publication bias correction) and bleb needling rate (RR: 1.45, 95% CI 1.06to 1.99, p value 0.019) were lower in phaco-XEN group compared to XEN only group. Compared to trabeculectomy, XEN implantation had similar after-surgery IOP, however bleb needling rate (RR: 2.42, 95% CI 1.33 to 4.43, p value 0.004) was higher.
Conclusion
Our results confirmed that XEN is effective in lowering both IOP and NOAM till 48 months after surgery. It is noteworthy that XEN implantation leads to higher needling rate, compared to phaco-XEN or trabeculectomy. Further research, studying complications of XEN on non-European ethnicities, especially on Asian, are in urgent need before XEN is widely applied.
Similar content being viewed by others
Introduction
Glaucoma is known as the global leading cause of irreversible blindness [1], and statistics shows that people of African ancestry are more sensitive to primary open angle glaucoma (POAG) than people of European ancestry [2].Intra-ocular pressure(IOP) lowering-laucoma treatments include anti-glaucoma medications, laser, surgery, and the combinations. Surgery is required when medications fail to control IOP or visual loss has reached a serious threshold.
Trabeculectomy and drainage device implantation are two methods widely adopted by clinicians. Trabeculectomy has become a standard surgical for glaucoma [3], it bypasses trabecular mesh and builds a drainage to help aqueous humor flow from anterior chamber to subconjunctival space. However, it can lead to high rates of complications including hypotony, anterior chamber hyphemia [4], etc. Minimally invasive glaucoma surgery (MIGS) has become surgical trend in recent years. As a type of MIGS, XEN Gel Stent (Allergan INC, Dublin, Ireland) implantations mimic the subconjunctival drainage of trabeculectomy, and are applied in real world since FDA approval in 2016. XEN implant is a 6-mm tube, made of porcine-gelatin cross-linked with glutaraldehyde, and has advantages of non-degrading and no tissue reaction [5] XEN45, the type of XEN that is now being merchandised, is designed to prevent hypotony and to maintain IOP around 6-8 mmHg with inner diameter of 45 μm [6]. XEN45 and XEN63, which is the new type of XEN, also have the indication of treating refractory POAG, and other types of OAG including pseudo-exfoliative glaucoma (PEXG). However, there are, currently, different opinions on the efficacy of XEN compared to traditional surgery in glaucoma according to previous studies [7,8,9], and its complications are also remain to be further investigated.
XEN is much easier to operate than trabeculectomy, thus it may help ophthalmologists, not specialists to treat glaucoma. Still, more evidence is required on the efficacy and complications of XEN before the device is widely applied. In this review, we did the most comprehensive meta-analysis on qualified clinical trials on this theme. With the data extracted, we did analysis to compare IOP-lowering and medication-lowering efficacy of XEN-only to XEN combined with phacoemulsification (phaco-XEN) and trabeculectomy surgeries respectively. Needling rate in different surgeries was also compared to study complications. Sub-analyses were carried out according to different study design, type of glaucoma, ethnicities, populations, economic status, and time points of follow-up to reduce confounding from those factors.
Material and method
This review is written according to Preferred Reporting Items for Systematic Reviews statement for reporting systematic reviews and meta-analyses [10] (Additional file 1: Appendix 1).
Search strategy
Electronic databases, including PubMed, EMBASE, the Cochrane Library of Systematic Reviews, Web of Science, China National Knowledge Infrastructure, WanFang and SinoMed databases were searched up to May 2021 for all clinical studies assessing XEN implant in glaucoma. The search strategy included the Medical Subject Headings terms and/or text words. The following combined search term was used: (XEN implant, XEN Gel Stent, gelatin stent) and (Glaucoma) (for the full search strategy, see the Additional file 2: Appendix 2 in the Supplement). The studies were restricted to human, but not restricted by date, language, or publication status.
Study selection
Studies were selected by two independent reviewers (Xiang Yang andYang Zhao using following criteria:
-
1)
patients were clearly diagnosed with glaucoma (no matter for POAG or PEXG, etc.);
-
2)
the study had a control design;
-
3)
XEN stent (XEN-45 or XEN-63) was used;
-
4)
sufficient information to calculate the effect size was available;
-
5)
the manuscript was published in a peer-reviewed journal as a full paper.
And criteria for excluding studies were:
-
1)
Animal studies;
-
2)
No original studies (case report, letter and response, review and meta-analysis or meeting abstract)
In the first stage, the titles and abstracts of all retrieved articles were screened. Disagreements were referred to a third reviewer (Yu Zhong) to achieve a resolution. In the second stage, full texts of the potentially relevant studies were retrieved and reviewed using the same methods as in first stage.
Data extraction and quality assessment
The following information was independently extracted from the included studies by two investigators (Xiang Yang andYang Zhao) and jointly verified for accuracy: author, year of publication, country of study, eyes included, female/male ratio, age, surgical implantation, follow-up period, etc. We contacted authors when there was unclear information. JADAD Scale [11] (for Randomized Controlled Trials) or Newcastle–Ottawa Scale [12] (for non-randomized Studies) were used for evidence quality assessment.
Outcome measures
The final included outcomes were: IOP before and after surgery; number of antiglaucoma medications (NOAM); bleb needling rate.
Statistical analysis
The pooled relative risk (RR) or standardized mean difference (SMD) in the meta-analysis were calculated by weighting individual risk ratio (RR)/SMD by the inverse of their variance. The RRs as well as 95% CIs were calculated using the random-effects model as it assumes that true effect might vary from study to study and thus, estimates the mean of a distribution of true effects, assigning a more balanced weight to each study. All tests were two-tailed with a p value < 0.05 considered statistically significant. Analysis using the fixed-effects model was carried out in the absence of heterogeneity. The Cochran’s Q test was used to test for heterogeneity (p value < 0.10 is indicative of heterogeneity). Given that the power of this statistical test is low when a meta-analysis includes a small number of studies, the Higgins test (I2) was also used, that describes the percentage of total variation across studies due to heterogeneity rather than chance (low heterogeneity: < 25%, moderate heterogeneity: 25–75% and high heterogeneity: > 75%) [13]. Leave-one-out sensitivity as well as stratified analyses were conducted to assess statistical robustness and to detect the possible causes of heterogeneity between studies. The Begg rank correlation [14] and Egger regression asymmetry test [15] were used to examine publication bias (P < 0.05 was considered statistically significant). If publication bias was confirmed, a trim-and-fill method developed by Duval and Tweedie was implemented to adjust the bias. Then, we replicated the funnel plot with their ‘‘missing’’ counterparts around the adjusted summary estimate. All those were conducted with the software Stata 15.0.
Results
Literature search
The search strategy for this meta-analysis yielded 725 publications, and 429 studies were excluded because of duplication. After reading the titles and abstracts, 57 studies were excluded. 239 possible full-text studies were carefully reviewed (Animal study [n = 4]; Case report [60]; Letter and Response [n
= 8]; Review and meta-Analysis [n = 64]; Meeting abstract [n = 25]). Finally, 78 trials were included for quantitative analysis [5, 16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92] (Fig. 1). The characteristics of included lectures are summarized in Table 1.
PRISMA 2009 flow diagram. The search strategy for this meta-analysis yielded 725 publications, and 429 studies were excluded because of duplication. After reading the titles and abstracts, 57 studies were excluded. Two hundred and thirty-nine possible full-text studies were carefully reviewed (Animal study [n = 4]; Case report [60]; Letter and Response [n = 8]; Review and meta-Analysis [n = 64]). Finally, 78 trials were included for quantitative analysis
Efficacy of XEN standalone surgery for the management of glaucoma
6554 eyes from 65 studies and 4385 eyes from 42 studies were included for IOP and NOAM analysis before and after XEN standalone procedure. There were no significant differences in IOP or NOAM between prospective and retrospective study (SFig1 and SFig2). Therefore, we combined them in the further analyses.
The total study sample included 3432 eyes before surgery and 3122 eyes after surgery. Overall analysis showed IOP had an obvious improvement after XEN stent implantation (SMD: 1.69, 95% CI 1.52 to 1.86, p value < 0.001) (sFig3). Fewer NOAM was also achieved in glaucoma patients after XEN standalone procedure (SMD: 2.11, 95% CI 1.84 to 2.38, p value < 0.001) (sFig4). Based on the follow-up duration, studies were divided into six categories: 6 m, 12 m, 18 m, 24 m, 36 m and 48 m. Considering IOP, no big difference was found at different time point (sFig5). As for NOAM, the difference became less and less with time, although significance was still not reached (sFig6). 6 studies addressing the IOP-lowering effect of XEN in Asian populations (168 eyes in before-surgery group and 160 eyes in after-surgery group), 8 studies addressing the treatment effect of XEN in North American populations (351 eyes in before surgery group and 284eyes in after surgery group) and 45 studies addressing this association in European populations (2913 eyes in before surgery group and 2678 eyes in after surgery group), were included in the stratified analyses by ethnicity (SFig7). Subgroup was further done by developed vs. developing country (SFig8). No statistical difference was found in different gene background and medical care, the patients could get. NOAM reduction had no difference indeveloped vsdeveloping country subgroup analysis (SFig9) orethnicity subgroup analysis (SFig10). Heterogeneity was high in most of the stratified analyses.
Given that differences in the pseudo-exfoliation glaucoma (PEXG) and primary open angle glaucoma (POAG) could potentially bias the current meta-analysis, analyses by different glaucoma were also conducted. Three studies with 237 POAG eyes and 118 PEXG eyes were included. Interestingly, no different treatment effect was found in these analyses on IOP and Medication (SFig11-14). Furthermore, analysis was conducted in patients with or without prior interventional therapies and patients with pseudophakic and phakic eyes. IOP before and after XEN surgery, medication before and after procedure and bleb needling rate shown no difference in pseudophakic and phakic eyes (SFig15-19).
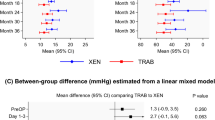
Efficacy and safety of XEN combined with cataract surgery for glaucoma patients
In some centers, cataract surgery was done at the same time when XEN stent was being implanted (phaco-XEN). In glaucoma patients IOP dropped significantly after phaco-XEN surgery irrespective of ethnicity (SFig20) or follow-up duration (SFig21). Medication needed for lowering IOP also had a clear reduction (SFig22). Further comparison was done between XEN standalone surgery and phaco-XEN surgery on IOP and medication. After procedure, there was no significant difference in IOP (SMD: -0.01, 95% CI -0.09 to 0.08, p value 0.894) (sFig23) and NOAM (SMD: 0.09, 95% CI -0.04 to 0.23, p value 0.170) (Fig. 2) between two group. Stratified analysis was also done by ethnicity and follow-up duration for IOP. In Asian population a clear difference of after-surgery IOP was found between two procedures (SMD: 0.57, 95% CI 0.23 to 0.91), which was absent in both European and North American patients (SFig24). On different follow-up time points, patients in different procedures shared a similar IOP (Fig. 3). Nevertheless, lower IOP before surgery was found in phaco-XEN group when baseline was analyzed (SMD: 0.31, 95% CI 0.15to 0.47, p value < 0.001), especially in European population (SFig25). Patients whose IOP achieved < 18 mmHg, < 15 mmHg, < 12 mmHg or had a reduction > 20% from baseline were counted and RR of success rate was obtained, which showed no difference in efficacy of treatment between XEN alone and phaco-XEN (data not shown). For considering complications, bleb needling rate was compared. Although similar IOP reduction was found in XEN alone and phaco-XEN group, bleb needling rate was significantly high in XEN standalone group (RR: 1.45, 95% CI 1.06to 1.99, p value 0.019) (Fig. 4).
Meta-analysis of XEN-only surgery compared with phaco-XEN for NOAM after surgery. The total study sample included 618 eyes undergoing XEN only and 415 eyes undergoing phaco-XEN. Overall analysis of NOAM after surgery (SMD: 0.09, 95% CI -0.04 to 0.23, p value 0.170)had no difference between two groups
Meta-analysis of XEN-only surgery compared with phaco-XEN for IOP by follow-up duration after surgery. The total study sample included 1314 eyes undergoing XEN-only surgery and 1160 eyes undergoing phaco-XEN. Overall analysis of IOP after surgery (SMD: -0.01, 95% CI -0.09 to 0.08, p value 0.894)had no difference between two groups
Meta-analysis of XEN-only surgery compared with phaco-XEN for bleb needing rate. The total study sample included 220 eyes undergoing XEN-only surgery and 443 eyes undergoing phaco-XEN surgery. Overall bleb needling rate was significantly high in XEN-only group (RR: 1.45, 95% CI 1.06to 1.99, p value 0.019)
Efficacy and safety comparisons between XEN standalone and trabeculectomy procedure
Besides comparing to phaco-XEN, XEN standalone procedure was also compared with trabeculectomy surgery. A preference of assigning patients of higher IOP to trabeculectomy group was found when checking baseline (SMD: -0.33, 95% CI -0.49 to -0.16, p value < 0.001) (Fig. 5). After surgery, IOP showed no difference between two groups (Fig. 6), while patients underwent trabeculectomy had lower bleb needling rate (RR: 2.42, 95% CI 1.33 to 4.43, p value 0.004) (Fig. 7).
Meta-analysis of XEN surgery compared with trabeculectomy procedure for IOP before surgery. The total study sample included 281 eyes undergoing XEN-only surgery and 332 eyes undergoing trabeculectomy procedure. Overall analysis of IOP before surgery (SMD: -0.33, 95% CI -0.49 to -0.16, p value < 0.001) was lower in trabeculectomy procedure group
Meta-analysis of XEN surgery compared with trabeculectomy procedure for IOP after surgery. The total study sample included 281 eyes undergoing XEN-only surgery and 332 eyes undergoing trabeculectomy procedure. Overall analysis of IOP after surgery (SMD: 0.14, 95% CI -0.18 to 0.46, p value < 0.388) had no difference between two groups
Meta-analysis of XEN surgery compared with trabeculectomy procedure for bleb needing rate. The total study sample included 371 eyes undergoing XEN-only surgery and 363 eyes undergoing trabeculectomy procedure. Overall bleb needling rate was significantly high in XEN-only group (RR: 2.42, 95% CI 1.33 to 4.43, p value 0.004)
Sensitivity analyses and publication bias
When leave-one-out sensitivity analyses were conducted, all the results remained statistically robust (Table 2, SFig26-33). Egger and Begg test was applied to test publication bias. Publication bias was found in IOP and medication comparison before and after phaco-XEN surgery. Publication bias was also found in after-surgery medication comparison of XEN standalone vs. phaco-XEN groups (Table 2). By trim and fill method, both the results of fixed and random effects model are the same with original result (Additional file 3: Appendix 3, SFig34-36), except for after-surgery medication comparison of XEN standalone vs. phaco-XEN groups.
Discussion
By screening through 725 research records and finally going into details of 78 clinical trials concerning XEN gel stent implantation in glaucoma, we conducted the most comprehensive meta-analysis ever since, in our knowledge. In this study, quantitative analyses were done to generate consolidated results, however, with no randomized clinical trial (RCT) available, elaborately designed RCTs should be carried out in the future for more convincing conclusions.
In this study, we were able to statistically evaluate the efficacy of XEN implantation in glaucoma in terms of IOP and NOAM. Both the measurements were effectively controlled within six months of XEN surgery and according to Lenzhofer. et al. [54] and Teus. et al. [87], IOP was maintained at a level of 13.40 ± 3.10 mmHg and 10.20 ± 5.20 mmHg 48 months after surgery. NOAM seems to increase with longer time points, follow-up period over 48 months is required to find out whether this is significant. Although there is genetic heterogeneity among different ethnicities concerning glaucoma morbidity, we did not find any difference when evaluating IOP or NOAM reduction efficacy of XEN surgery among African, European, North American, Oceanian, or Asian. Currently, most trials are on European and more clinical studies are in urgent need in other areas, especially for China mainland.
Besides POAG, XEN implantation is indicated to treat refractory POAG when previous treatments failed, and also for special types of OAG including PEXG, pigmentary glaucoma, juvenile glaucoma, and uveitic glaucoma. Studies stated that XEN is effective in treating both refractory glaucoma [93] and uveitic glaucoma [94], with bleb fibrosis, being the most common complications, which requires bleb needling. We did analysis on the four trials comparing XEN efficacy in POAG and PEXG and the results further confirmed that XEN implantation can reduce IOP and NOAM in PEXG as powerful as POAG.
Phacoemulsification is often combined with traditional filtering surgery such as TB, and phaco-XEN is possibly considered by clinicians while deciding the surgery. Whether phaco-XEN is superior to XEN-only or not has drawn attentions from a lot of studies. Thirty studies with totally over 1,000 eyes in each group were included in our analysis and we found no significant difference in IOP-lowering effect between XEN-only and phaco-XEN groups at the last follow-up. When we go into sub-analysis of various time points, XEN-only reveals lower after-surgery IOP than phaco-XEN in the short time points of 6 months and 12 months, the gap narrows with time, although this trend is of no significance. Lim. et al. [8] and Bo. et al. [9] did meta-analysis for closer time points of 1 day, 1 week, 1 month, 3 months, and 6 months, they showed that XEN-only has significant lower IOP than the combined group. Considering the time point of 6 months, our results are consistent with the above two meta-analysis that XEN-only has significant lower IOP than the combined group. We also found that NOAM and bleb needling rate was significantly lower in phaco-XEN than XEN-only, which indicates fewer fibrosis in combined group and phaco-XEN can be adopted with patients in high-risk of fibrosis. Traditional TB also showed lower bleb needling rate than XEN implantation, thus in our opinion, this new type of MIGS leads to worse bleb fibrosis although the gel is compatible in human tissue. It is also noteworthy that the endothelial cell density reduction in the phaco-XEN group was larger than in the XEN-onlygroup [63], and TB lose more endothelial cells than XEN [66].
Although our study shown that XEN is effective in lowering IOP till 48 months, at least three outstanding issues remain: Firstly, although we have tried but no unpublished data was found, so all included studies were published data. But Egger test showed no publication bias for most outcomes. Secondly, heterogeneity was high in some outcomes. Subgroup analysis was carried out, however, the source of heterogeneity is still not fully understood. Thirdly, the quality of included studies is relatively low. So long-term randomized control trials with large sample size are still in great need. The definition of outcomes are inconsistent in the 78 trials, which makes up publication bias and possible misinterpretation. Some trials reach complete success (expected IOL reduction without medications) when evaluating the XEN/phaco-XEN effects, while some reach qualified success (expected IOL reduction with medications). Besides, IOP targets of those trials are not same, for example, someIOP reduction > 30% while some targets of IOPreduction > 20%.These publication inconsistencies may lead to confoundings when comparing XEN/phaco-XEN effects.
Conclusion
In this meta-analysis including 78 trials with thousands of eyes, we did the most comprehensive exploration ever on the efficacy of XEN implantation in treating glaucoma. To conclude, XEN is effective in both lowering IOP and NOAM till 48 months after surgery. It is also as effective in patients of PEXG as those of POAG, in terms of IOP, NOAM, and needling rate. Phaco-XEN may require fewer medications for patients after surgery, however the final IOP is similar to XEN-only surgery. It is noteworthy that XEN implantation leads to higher bleb fibrosis and needling rate, and phaco-XEN or TB may be a better choice to prevent filtering failure. Further studies on vision-threatening complications such as hypotony, choroidal leakage, and bleb infection comparing to other surgeries are in urgent need for evaluating safety of XEN implantation. Also, clinical trials on Asians are quite limited which restricts the application of XEN to a wider part of the world.
Availability of data and materials
Not published or shown elsewhere yet, not deposited in online database yet.
References
Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA. 2014;311(18):1901–11.
Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081–90.
The AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130(4):429–40.
Jampel HD, Musch DC, Gillespie BW, Lichter PR, Wright MM, Guire KE. Perioperative complications of trabeculectomy in the collaborative initial glaucoma treatment study (CIGTS). Am J Ophthalmol. 2005;140(1):16–22.
Sheybani A, Lenzhofer M, Hohensinn M, Reitsamer H, Ahmed II. Phacoemulsification combined with a new ab interno gel stent to treat open-angle glaucoma: pilot study. J Cataract Refract Surg. 2015;41(9):1905–9.
Yu DY, Morgan WH, Sun X, Su EN, Cringle SJ, Yu PK, et al. The critical role of the conjunctiva in glaucoma filtration surgery. Prog Retin Eye Res. 2009;28(5):303–28.
Poelman HJ, Pals J, Rostamzad P, Bramer WM, Wolfs RCW, Ramdas WD. Efficacy of the XEN-implant in glaucoma and a meta-analysis of the literature. J Clin Med. 2021;10(5):1118.
Lim SY, Betzler BK, Yip LWL, Dorairaj S, Ang BCH. Standalone XEN45 Gel Stent implantation versus combined XEN45-phacoemulsification in the treatment of open angle glaucoma-a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol. 2021;259(11):3209–19.
Wang B, Leng X, An X, Zhang X, Liu X, Lu X. XEN gel implant with or without phacoemulsification for glaucoma: a systematic review and meta-analysis. Ann Transl Med. 2020;8(20):1309.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Arad T, Hoffmann EM, Prokosch-Willing V, Pfeiffer N, Grehn F. XEN-augmented baerveldt implantation for refractory childhood glaucoma: a retrospective case series. J Glaucoma. 2019;28(11):1015–8.
Arnljots TS, Kasina R, Bykov VJN, Economou MA. Needling with 5-Fluorouracil (5-FU) after XEN gel stent implantation: 6-month outcomes. J Glaucoma. 2018;27(10):893–9.
Barão RC, José P, Teixeira FJ, Ferreira NP, Sens P, Pinto LA. Automated gonioscopy assessment of XEN45 gel stent angle location after isolated XEN or combined Phaco-XEN procedures: clinical implications. J Glaucoma. 2020;29(10):932–40.
Başer EF, Seymenoğlu RG. Results of fluorouracil-augmented Xen45 implantation in primary open-angle and pseudoexfoliation glaucoma. Int Ophthalmol. 2020;41(3):945–55.
Bravetti GE, Mansouri K, Gillmann K, Rao HL, Mermoud A. XEN-augmented Baerveldt drainage device implantation in refractory glaucoma: 1-year outcomes. Graefes Arch Clin Exp Ophthalmol. 2020;258(8):1787–94.
Buffault J, Graber M, Bensmail D, Bluwol É, Jeanteur MN, Abitbol O, et al. Efficacy and safety at 6 months of the XEN implant for the management of open angle glaucoma. Sci Rep. 2020;10(1):4527.
Busch T, Skiljic D, Rudolph T, Bergström A, Zetterberg M. Learning curve and one-year outcome of XEN 45 gel stent implantation in a Swedish population. Clin Ophthalmol. 2020;14:3719–33.
Chao Y-J, Ko Y-C, Chen M-J, Lo K-J, Chang Y-F, Liu CJ-L. XEN45 Gel Stent implantation in eyes with primary open angle glaucoma: a study from a single hospital in Taiwan. J Chin Med Assoc. 2021;84(1):108–13.
Cutolo CA, Iester M, Bagnis A, Bonzano C, Negri L, Olivari S, et al. Early postoperative intraocular pressure is associated with better pressure control after XEN implantation. J Glaucoma. 2020;29(6):456–60.
Dar N, Sharon T, Hecht I, Kalev-Landoy M, Burgansky-Eliash Z. Efficacy and safety of the ab interno gelatin stent in severe pseudoexfoliation glaucoma compared to non-pseudoexfoliation glaucoma at 6 months. Eur J Ophthalmol. 2020;30(5):1028–33.
De Gregorio A, Pedrotti E, Russo L, Morselli S. Minimally invasive combined glaucoma and cataract surgery: clinical results of the smallest ab interno gel stent. Int Ophthalmol. 2018;38(3):1129–34.
Do A, McGlumphy E, Shukla A, Dangda S, Schuman JS, Boland MV, et al. Comparison of clinical outcomes with open versus closed conjunctiva implantation of the XEN45 gel stent. Ophthalmol Glaucoma. 2021;4(4):343–9.
Fea AM, Bron AM, Economou MA, Laffi G, Martini E, Figus M, et al. European study of the efficacy of a cross-linked gel stent for the treatment of glaucoma. J Cataract Refract Surg. 2020;46(3):441–50.
Fea AM, Spinetta R, Cannizzo PML, Consolandi G, Lavia C, Aragno V, et al. Evaluation of bleb morphology and reduction in IOP and glaucoma medication following implantation of a novel gel stent. J Ophthalmol. 2017;2017:9364910.
Fernández-García A, Zhou Y, García-Alonso M, Andrango HD, Poyales F, Garzón N. Comparing medium-term clinical outcomes following XEN® 45 and XEN® 63 device implantation. J Ophthalmol. 2020;2020:4796548.
Fernández-García A, Zhou Y, García-Alonso M, Andrango HD, Poyales F, Garzón N. Medium-term clinical outcomes following Xen45 device implantation. Int Ophthalmol. 2020;40(3):709–15.
Gabbay IE, Allen F, Morley C, Pearsall T, Bowes OM, Ruben S. Efficacy and safety data for the XEN45 implant at 2 years: a retrospective analysis. Br J Ophthalmol. 2020;104(8):1125–30.
Galal A, Bilgic A, Eltanamly R, Osman A. XEN glaucoma implant with mitomycin C 1-year follow-up: result and complications. J Ophthalmol. 2017;2017:5457246.
Gillmann K, Bravetti GE, Mermoud A, Rao HL, Mansouri K. XEN gel stent in pseudoexfoliative glaucoma: 2-year results of a prospective evaluation. J Glaucoma. 2019;28(8):676–84.
Gillmann K, Bravetti GE, Rao HL, Mermoud A, Mansouri K. Combined and stand-alone XEN 45 gel stent implantation: 3-year outcomes and success predictors. Acta Ophthalmol. 2020;99(4):e531–9.
Gillmann K, Bravetti GE, Rao HL, Mermoud A, Mansouri K. Bilateral XEN stent implantation: a long-term prospective study of the difference in outcomes between first-operated and fellow eyes. J Glaucoma. 2020;29(7):536–41.
Grover DS, Flynn WJ, Bashford KP, Lewis RA, Duh Y-J, Nangia RS, et al. Performance and safety of a new ab intern gelatin stent in refractory glaucoma at 12 months. Am J Ophthalmol. 2017;183:25–36.
Heidinger A, Schwab C, Lindner E, Riedl R, Mossböck G. A retrospective study of 199 Xen45 stent implantations from 2014 to 2016. J Glaucoma. 2019;28(1):75–9.
Hengerer FH, Auffarth G, Conrad-Hengerer I. Comparison of minimally invasive XEN45 gel stent implantation in glaucoma patients without and with prior interventional therapies. Ophthalmol Ther. 2019;8(3):447–59.
Hengerer FH, Auffarth GU, Yildirim TM, Conrad-Hengerer I. Ab interno gel implant in patients with primary open angle glaucoma and pseudoexfoliation glaucoma. BMC Ophthalmol. 2018;18(1):339.
Hengerer FH, Kohnen T, Mueller M, Conrad-Hengerer I. Ab interno gel implant for the treatment of glaucoma patients with or without prior glaucoma surgery: 1-year results. J Glaucoma. 2017;26(12):1130–6.
Hohberger B, Welge-Luessen U-C, Laemmer R. MIGS: therapeutic success of combined Xen Gel Stent implantation with cataract surgery. Graefes Arch Clin Exp Ophthalmol. 2018;256(3):621–5.
Hong K, Lind J, Sheybani A. Safety and efficacy outcomes of the Xen45 Gel Stent use for refractory glaucoma: a surgery series from surgeon trainees at a tertiary teaching hospital. Eye Vis (Lond). 2020;7:5.
Hu JY, Ang BCH, Yip LW. Efficacy of the XEN gel stent on intraocular pressure lowering in East Asian eyes. Int Ophthalmol. 2020;40(5):1191–9.
Ibáñez-Muñoz A, Soto-Biforcos VS, Chacón-González M, Rúa-Galisteo O, Arrieta-Los Santos A, Lizuain-Abadía ME, et al. One-year follow-up of the XEN® implant with mitomycin-C in pseudoexfoliative glaucoma patients. Eur J Ophthalmol. 2019;29(3):309–14.
Ibáñez-Muñoz A, Soto-Biforcos VS, Rodríguez-Vicente L, Ortega-Renedo I, Chacón-González M, Rúa-Galisteo O, et al. XEN implant in primary and secondary open-angle glaucoma: a 12-month retrospective study. Eur J Ophthalmol. 2020;30(5):1034–41.
Ilveskoski L, Tuuminen R. Combined microinvasive glaucoma and cataract surgery in patients with pseudoexfoliation glaucoma: clinical results of a gel stent. J Cataract Refract Surg. 2017;43(8):1124–5.
Kalina AG, Kalina PH, Brown MM. XEN (R) gel stent in medically refractory open-angle glaucoma: results and observations after one year of use in the United States. Ophthalmol Therapy. 2019;8(3):435–46.
Karimi A, Hopes M, Martin KR, Lindfield D. Efficacy and safety of the ab-interno Xen gel stent after failed trabeculectomy. J Glaucoma. 2018;27(10):864–8.
Karimi A, Lindfield D. Is a day 1 postoperative review following ab interno Xen gel stent surgery for glaucoma needed? Clin Ophthalmol. 2018;12:2331–5.
Laborda-Guirao T, Cubero-Parra JM, Hidalgo-Torres A. Efficacy and safety of XEN 45 gel stent alone or in combination with phacoemulsification in advanced open angle glaucoma patients: 1-year retrospective study. Int J Ophthalmol. 2020;13(8):1250–6.
Laroche D, Nkrumah G, Ng C. Real-World retrospective consecutive study of ab interno XEN 45 gel stent implant with mitomycin C in black and afro-latino patients with glaucoma: 40% required secondary glaucoma surgery at 1 year. Middle East Afr J Ophthalmol. 2019;26(4):229–34.
Lavin-Dapena C, Cordero-Ros R, D’Anna O, Mogollón I. XEN 63 gel stent device in glaucoma surgery: A 5-years follow-up prospective study. Eur J Ophthalmol. 2020;31(4):1829–35.
Lenzhofer M, Kersten-Gomez I, Sheybani A, Gulamhusein H, Strohmaier C, Hohensinn M, et al. Four-year results of a minimally invasive transscleral glaucoma gel stent implantation in a prospective multi-centre study. Clin Exp Ophthalmol. 2019;47(5):581–7.
Lenzhofer M, Strohmaier C, Hohensinn M, Hitzl W, Steiner V, Baca B, et al. Change in visual acuity 12 and 24 months after transscleral ab interno glaucoma gel stent implantation with adjunctive Mitomycin C. Graefes Arch Clin Exp Ophthalmol. 2019;257(12):2707–15.
Lenzhofer M, Strohmaier C, Sperl P, Hohensinn M, Hitzl W, Steiner V, et al. Effect of the outer stent position on efficacy after minimally invasive transscleral glaucoma gel stent implantation. Acta Ophthalmol. 2019;97(8):e1105–11.
Linton E, Au L. Technique of xen implant revision surgery and the surgical outcomes: a retrospective interventional case series. Ophthalmol Ther. 2020;9(1):149–57.
Mansouri K, Bravetti GE, Gillmann K, Rao HL, Ch’ng TW, Mermoud A. Two-year outcomes of XEN gel stent surgery in patients with open-angle glaucoma. Ophthalmol Glaucoma. 2019;2(5):309–18.
Mansouri K, Gillmann K, Rao HL, Guidotti J, Mermoud A. Prospective evaluation of XEN gel implant in eyes with pseudoexfoliative glaucoma. J Glaucoma. 2018;27(10):869–73.
Mansouri K, Guidotti J, Rao HL, Ouabas A, D’Alessandro E, Roy S, et al. Prospective evaluation of standalone XEN gel implant and combined phacoemulsification-XEN gel implant surgery: 1-year results. J Glaucoma. 2018;27(2):140–7.
Marcos Parra MT, Salinas Lopez JA, Lopez Grau NS, Maria Ceausescu A, Perez Santonja JJ. XEN implant device versus trabeculectomy, either alone or in combination with phacoemulsification, in open-angle glaucoma patients. Graefes Arch Clin Exp Ophthalmol. 2019;257(8):1741–50.
Marques RE, Ferreira NP, Sousa DC, Pinto J, Barata A, Sens P, et al. Glaucoma gel implant learning curve in a Teaching Tertiary Hospital. J Glaucoma. 2019;28(1):56–60.
Midha N, Gillmann K, Chaudhary A, Mermoud A, Mansouri K. Efficacy of needling revision after XEN gel stent implantation: a prospective study. J Glaucoma. 2020;29(1):11–4.
Midha N, Rao HL, Mermoud A, Mansouri K. Identifying the predictors of needling after XEN gel implant. Eye (Lond). 2019;33(3):353–7.
Oddone F, Roberti G, Posarelli C, Agnifili L, Mastropasqua L, Carnevale C, et al. Endothelial cell density after XEN implant surgery: short term data from the Italian XEN glaucoma treatment registry (XEN-GTR). J Glaucoma. 2021;30(7):559–65.
Olate-Pérez Á, Pérez-Torregrosa VT, Gargallo-Benedicto A, Neira-Ibáñez P, Cerdà-Ibáñez M, Osorio-Alayo V, et al. Prospective study of filtering blebs after XEN45 surgery. Arch Soc Esp Oftalmol. 2017;92(8):366–71.
Olgun A, Aktas Z, Ucgul AY. XEN gel implant versus gonioscopy-assisted transluminal trabeculotomy for the treatment of open-angle glaucoma. Int Ophthalmol. 2020;40(5):1085–93.
Olgun A, Duzgun E, Yildiz AM, Atmaca F, Yildiz AA, Sendul SY. XEN Gel Stent versus trabeculectomy: Short-term effects on corneal endothelial cells. Eur J Ophthalmol. 2020;31(2):346–53.
Ozal SA, Kaplaner O, Basar BB, Guclu H, Ozal E. An innovation in glaucoma surgery: XEN45 gel stent implantation. Arq Bras Oftalmol. 2017;80(6):382–5.
Pérez-Torregrosa VT, Olate-Pérez Á, Cerdà-Ibáñez M, Gargallo-Benedicto A, Osorio-Alayo V, Barreiro-Rego A, et al. Combined phacoemulsification and XEN45 surgery from a temporal approach and 2 incisions. Arch Soc Esp Oftalmol. 2016;91(9):415–21.
Post M, Lubinski W, Sliwiak D, Podboruczynska-Jodko K, Mularczyk M. XEN Gel Stent in the management of primary open-angle glaucoma. Doc Ophthalmol. 2020;141(1):65–76.
Qureshi A, Jones NP, Au L. Urgent management of secondary glaucoma in uveitis using the Xen-45 gel stent. J Glaucoma. 2019;28(12):1061–6.
Rather PA, Vold S, McFarland M. Twelve-month outcomes of an ab interno gelatin stent combined with cataract surgery or as a standalone procedure in pseudophakic eyes with open-angle glaucoma. J Cataract Refract Surg. 2020;46(8):1172–7.
Rauchegger T, Angermann R, Willeit P, Schmid E, Teuchner B. Two-year outcomes of minimally invasive XEN Gel Stent implantation in primary open-angle and pseudoexfoliation glaucoma. Acta Ophthalmol. 2020;99(4):369–75.
Reitsamer H, Sng C, Vera V, Lenzhofer M, Barton K, Stalmans I. Two-year results of a multicenter study of the ab interno gelatin implant in medically uncontrolled primary open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 2019;257(5):983–96.
Reitsamer H, Vera V, Ruben S, Au L, Vila-Arteaga J, Teus M, et al. Three-year effectiveness and safety of the XEN gel stent as a solo procedure or in combination with phacoemulsification in open-angle glaucoma: a multicentre study. Acta Ophthalmol. 2021;100(1):e233–45.
Schargus M, Theilig T, Rehak M, Busch C, Bormann C, Unterlauft JD. Outcome of a single XEN microstent implant for glaucoma patients with different types of glaucoma. BMC Ophthalmology. 2020;20(1):490.
Scheres LMJ, Kujovic-Aleksov S, Ramdas WD, de Crom R, Roelofs LCG, Berendschot T, et al. XEN(®) gel stent compared to PRESERFLO™ microshunt implantation for primary open-angle glaucoma: two-year results. Acta Ophthalmol. 2021;99(3):e433–40.
Schlenker MB, Gulamhusein H, Conrad-Hengerer I, Somers A, Lenzhofer M, Stalmans I, et al. Standalone ab interno gelatin stent versus trabeculectomy: postoperative interventions, visual outcomes, and visits. Ophthalmol Glaucoma. 2018;1(3):189–96.
Sharpe R, Pham G, Chang P. Comparison of ab interno XEN gelatin stent vs trabeculectomy with mitomycin c: a retrospective study. J Curr Glaucoma Pract. 2020;14(3):87–92.
Sheybani A, Dick HB, Ahmed II. Early clinical results of a novel ab interno gel stent for the surgical treatment of open-angle glaucoma. J Glaucoma. 2016;25(7):e691–6.
Smith M, Charles R, Abdel-Hay A, Shah B, Byles D, Lim LA, et al. 1-year outcomes of the Xen45 glaucoma implant. Eye (Lond). 2019;33(5):761–6.
Sng CC, Wang J, Hau S, Htoon HM, Barton K. XEN-45 collagen implant for the treatment of uveitic glaucoma. Clin Exp Ophthalmol. 2018;46(4):339–45.
Tan NE, Tracer N, Terraciano A, Parikh HA, Panarelli JF, Radcliffe NM. Comparison of safety and efficacy between ab interno and ab externo approaches to XEN gel stent placement. Clin Ophthalmol. 2021;15:299–305.
Tan SZ, Walkden A, Au L. One-year result of XEN45 implant for glaucoma: efficacy, safety, and postoperative management. Eye (Lond). 2018;32(2):324–32.
Teixeira FJ, Sousa DC, Machado NM, Caiado F, Barão R, Sens P, et al. XEN-augmented baerveldt surgical success rate and comparison with the ahmed valve. Acta Ophthalmol. 2020;98(7):e870–5.
Teus MA, Paz Moreno-Arrones J, Castaño B, Castejon MA, Bolivar G. Optical coherence tomography analysis of filtering blebs after long-term, functioning trabeculectomy and XEN® stent implant. Graefes Arch Clin Exp Ophthalmol. 2019;257(5):1005–11.
Theillac V, Blumen-Ohana E, Akesbi J, Hamard P, Sellam A, Brasnu E, et al. Cataract and glaucoma combined surgery: XEN® gel stent versus nonpenetrating deep sclerectomy, a pilot study. BMC Ophthalmol. 2020;20(1):231.
Urcola A, Garay-Aramburu G. Safety and efficacy of bilateral simultaneous XEN implant surgery: a pilot study. Int Ophthalmol. 2021;41(3):859–66.
Wałek E, Przeździecka-Dołyk J, Helemejko I, Misiuk-Hojło M. Efficacy of postoperative management with 5-fluorouracil injections after XEN gel stent implantation. Int Ophthalmol. 2020;40(1):235–46.
Widder RA, Dietlein TS, Dinslage S, Kuehnrich P, Rennings C, Roessler G. The XEN45 gel stent as a minimally invasive procedure in glaucoma surgery: success rates, risk profile, and rates of re-surgery after 261 surgeries. Graefes Arch Clin Exp Ophthalmol. 2018;256(4):765–71.
Widder RA, Lappas A, Rennings C, Hild M, Dietlein TS, Roessler GF. Primary versus posttrabeculectomy XEN45 gel stent implantation: comparison of success rates and intraocular pressure-lowering potential in pseudophakic eyes. J Glaucoma. 2020;29(12):1115–9.
De Gregorio A, Pedrotti E, Stevan G, Bertoncello A, Morselli S. XEN glaucoma treatment system in the management of refractory glaucomas: a short review on trial data and potential role in clinical practice. Clin Ophthalmol. 2018;12:773–82.
Morgan WH, Yu DY. XEN-45 gelatin microfistula for uveitic glaucoma. Clin Exp Ophthalmol. 2018;46(4):323–4.
Acknowledgements
We are grateful for Dr. Saikat Majumder, from Division of Rheumatology and Clinical Immunology, Department of Medicine, University of Pittsburgh, Pittsburgh PA, USA for language editing.
Precis
Our study revealed that XEN-only implantation procedure is as effective as phaco-XEN and trabeculectomy in lowering IOP in glaucoma. However, XEN procedure leads to higher bleb needling rate than trabeculectomy.
Data and materials availability
All data needed to evaluate the conclusions in the paper are present in the paper or the Supplementary Materials.
Funding
Natural Science Foundation of Changsha, China (Grant No. kq2202494 to XY), Clinical Research Institute Foundation of Aier Eye Hospital Group, China (Grant No. AR2106D2 to XY). Science and Technology Foundation of Changsha, Hunan, China (Grant No. kh1801229 to XD), Natural Science Foundation of Hunan Province, China (Grant No. 2019JJ40001 to XD).
Author information
Authors and Affiliations
Contributions
Xiang Yang composed the manuscript and did the literature searching and screening. Yang Zhao did the literature searching, screening, and data extraction. Zhong Yu was in charge of checking the involved publications and data. Xuanchu Duan came up with the idea and supervised the whole process. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All authors consented to participate in the work.
Consent for publication
All authors consented to participate in the work.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix 1.
PRISMA 2020 Checklist.
Additional file 4:
SFig1. Meta analysis of IOP by study design before and after XEN surgery. SFig2. Meta analysis of NOAM by study design before and after XEN surgery. sFig3. Meta analysis of IOP before and after XEN surgery. sFig4. Meta analysis of NOAM before and after XEN surgery. sFig5. Meta analysis of IOP by follow-up duration before and after XEN surgery. sFig6. Meta analysis of NOAM by follow-up duration before and after XEN surgery. sFig7. Meta analysis of IOP by ethnicity before and after XEN surgery. sFig8. Meta analysis of IOP by developed and developing country and after XEN surgery. sFig9. Meta analysis of NOAM by developed and developing country before and after XEN surgery. sFig10. Meta analysis of NOAM by ethnicity before after XEN surgery. sFig11. Meta analysis of IOP before XEN surgery betweem POAG and PEXG. sFig12. Meta analysis of IOP after XEN surgery betweem POAG and PEXG. sFig13. Meta analysis of NOAM before XEN surgery betweem POAG and PEXG. sFig14. Meta analysis of NOAM after XEN surgery betweem POAG and PEXG. sFig15. Meta analysis of IOP after XEN surgery between those with and without prior interventions. sFig16. Meta analysis of NOAM after XEN surgery between those with and without prior interventions. sFig17. Meta analysis of bleb needling rate between those with and without prior interventions. sFig18. Meta analysis of IOP after XEN surgery between phakic and pseudophakic eyes. sFig19. Meta analysis of NOAM after XEN surgery between phakic and pseudophakic eyes. sFig20. Meta analysis of IOP by ethnicity before and after phaco-XEN surgery. sFig21. Meta analysis of IOP by follow-up duration before and after phaco-XEN surgery. sFig22. Meta analysis of NOAM before and after phaco-XEN surgery. sFig23. Meta analysis of IOP after surgery between XEN-only and phaco-XEN surgery. sFig24. Meta analysis of IOP after surgery by ethnicity between XEN-only and phaco-XEN surgery. sFig25. Meta analysis of IOP before surgery by ethnicity between XEN-only and phaco-XEN surgery. sFig26. sensitive analysis of IOP before and after XEN surgery. sFig27. sensitive analysis of NOAM before and after XEN surgery. sFig28. sensitive analysis of IOP before and after phaco-XEN surgery. sFig29. sensitive analysis of NOAM before and after phaco-XEN surgery. sFig30. sensitive analysis of IOP before XEN surgery and phaco-XEN surgery. sFig31. sensitive analysis of IOP after XEN surgery and phaco-XEN surgery. sFig32. sensitive analysis of NOAM before XEN surgery and phaco-XEN surgery. sFig33. sensitive analysis of NOAM after XEN surgery and phaco-XEN surgery. sFig34. filled funnel plot of IOP before and after phaco-XEN surgery. sFig35. filled funnel plot of NOAM before and after phaco-XEN surgery. sFig36. filled funnel plot of NOAM after XEN and phaco-XEN surgery.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, X., Zhao, Y., Zhong, Y. et al. The efficacy of XEN gel stent implantation in glaucoma: a systematic review and meta-analysis. BMC Ophthalmol 22, 305 (2022). https://doi.org/10.1186/s12886-022-02502-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-022-02502-y