Abstract
Background
Transforming growth factor (TGF) is a cytokine that acts on the proliferation, migration, differentiation, and apoptosis of cells and the accumulation of extracellular matrix components. Very few studies have precisely evaluated the concentration of TGF-β in the aqueous humour (AH) of diabetic and cataract (DMC) eyes due to the low expression of proteins in the AH or other reasons. The concentrations of TGF-β1, -β2, and -β3 in the AH of the DMC group were compared with those of the age-related cataract (ARC) group.
Methods
We collected AH and lens epithelium samples from 33 DMC patients and 36 ARC patients. Luminex liquid suspension chip detection was applied to detect the concentration of TGF-β1, -β2, and -β3 in the AH samples. The expression of TGFB1/2/3 in lens epithelium samples was determined by quantitative real-time polymerase chain reaction (qRT-PCR).
Results
The concentrations of TGF-β1 and TGF-β2 in AH samples of DMC eyes were higher than those of ARC eyes. The differences in TGF-β1 and TGF-β2 between the two groups were statistically significant (P value = 0.001 for TGF-β1, P value = 0.023 for TGF-β2). The difference of the correlation between TGF-β1 and glycosylated haemoglobin was significant (P value = 0.011, and Pearson correlation coefficient = 0.306). The difference of the correlation between TGF-β2 and glycosylated haemoglobin was significant (P value = 0.026, and Pearson correlation coefficient = 0.269). The mRNA expression levels of TGFB1 and TGFB2 were upregulated in DMC epithelium samples compared with ARC epithelium samples. The differences in TGFB1 and TGFB2 between the two groups were statistically significant (P value for TGFB1 = 0.041, P value for TGFB2 = 0.021).
Conclusions
The concentrations of TGF-β1 and TGF-β2 in AH samples were significantly higher in DMC eyes than in ARC eyes. The higher the glycosylated haemoglobin was, the higher the concentrations of TGF-β1 and -β2 were. The mRNA expression of TGFB1 and TGFB2 was significantly upregulated in DMC epithelial samples compared with ARC epithelial samples, suggesting the proinflammatory status of the anterior chamber of DMC eyes.
Similar content being viewed by others
Introduction
Opacification of crystalline lenses, which is called cataracts, can be caused by many factors. Diabetes is a complex metabolic disorder involving small blood vessels that can cause widespread damage to tissues, including the eyes. Patients with diabetes often suffer from cataracts. Bilateral cataracts occasionally occur with rapid onset in severe juvenile diabetes and are called true diabetic cataracts. However, true diabetic cataracts are rare. Senile cataracts in people with diabetes, which are called diabetes and cataracts in our study, are more common. The potential mechanisms for the pathogenesis of diabetic cataracts are complicated and include the p38-MAPK signalling pathway [1, 2], polyol pathway [3], and changes in inflammatory cytokines [4,5,6,7,8,9,10]. However, the precise mechanism of diabetes and cataracts remains unclear.
TGF-β was related to many ocular diseases, including diabetic cataracts, glaucoma, and diabetic retinopathy. It was reported that the expression of TGF-β was increased after exposure to high glucose, which might be related to the development of diabetic cataracts [11]. It was also found that the aqueous humour levels of TGF-β1 and TGF-β2 were evaluated in the eyes of patients with acute primary angle closure [12], and the TGF-β2 concentration was significantly elevated in patients with concurrent open-angle glaucoma, and complicating diabetes [13,14,15,16], as well as in patients with neovascular glaucoma secondary to proliferative diabetic retinopathy [17]. TGF-β has important roles in epithelial–mesenchymal transition
[18]. TGF-β2-mediated fibrosis of lens epithelial cells during posterior capsule opacification could be promoted by advanced glycation end product formation [19]. In addition, TGF-β2 could effectively attenuate the activation of the MAPK/ERK/JNK and PI3K/Akt/GSK3β pathways [20]. Jagged-1/Notch signalling was reported to be activated in TGF-β2-stimulated epithelial–mesenchymal transition, and blockade of Notch signalling reversed lens epithelial cell epithelial–mesenchymal transition and lens fibrosis [21]. The miR-26a-5p/ITGAV/TGF-β/Smad3 axis was also reported to be involved in cell viability, migration and epithelial–mesenchymal transition in diabetic cataracts [22]. TGF-β was additionally reported to function in promoting epithelial–mesenchymal transition of lens epithelial cells under high glucose conditions, and the c-Src/TGF-β signalling axis in the epithelial–mesenchymal transition of lens epithelial cells might be a potential novel therapeutic target for the prevention of diabetic subcapsular cataracts [23].
Although TGF-β might play important roles in the development of diabetes and cataracts, very few studies have precisely evaluated the concentration of TGF-β in the AH of DMC eyes due to the low expression of proteins in the AH or other reasons. Recently, Luminex liquid suspension chip detection was applied to detect a large number of selected biomarkers on one membrane for samples containing very low protein concentrations [24, 25].
Therefore, we used Luminex liquid suspension chip detection to detect the concentrations of TGF-β1, -β2, and -β3 in the AH of the DMC group compared with the ARC group. In addition, we adopted qRT-PCR to test the mRNA expression of the TGFB1, TGFB2 and TGFB3 genes between DMC and ARC epithelium samples.
Methods and Materials
Ethics statement
The use of human AH and lens epithelium samples from cataract eyes during surgery was approved by the Institutional Review Board of Eye and ENT Hospital of Fudan University. This study was performed in accordance with the tenets of the Declaration of Helsinki for research involving human subjects. Written informed consent was obtained from every enrolled participant.
Collection of AH and human lens epithelium samples
We collected AH (50–100 µl from each patient) and human lens epithelium samples from 33 patients with diabetes (Type 2) and cataracts (mean age 69.85 ± 6.85, aged from 55–86 years old, HbA1c 7.15 ± 1.03%, free of other ocular diseases, free of diabetes-related microvascular and macrovascular complications, no intravitreal steroids used, taking oral medications to control sugar, and lenticular opacity ranging from C3-4, NO2-3, NC2-3, and P2-3 by LOCSIII) and 36 patients with age-related cataracts (mean age 70.36 ± 8.08, aged from 54–87 years old, HbAlc 5.90 ± 0.57%, free of other ocular diseases, and C3-4, NO2-3, NC2-3, and P1-2 by LOCSIII) before cataract surgery at Eye and ENT Hospital of Fudan University. After swabbing the eyelids and the surrounding skin with disinfectant, we created a corneal paracentesis and gently inserted a 26 G needle through the paracentesis to aspirate the AH (50–100 µl) before commencing cataract surgery. All AH and human lens epithelium samples were stored in a freezer at -80 ℃ until the next step.
Luminex liquid suspension chip detection
Luminex liquid suspension chip detection (Catalogue Number: TGFBMAG-64 K-03) was performed by Wayen Biotechnology (Shanghai, China). The TGF-β1, -β2, and -β3 Magnetic Bead Kit was used in accordance with the manufacturer’s instructions. In brief, 25 µL of each AH sample was incubated in 96-well plates embedded with TGF-β1, -β2, and -β3 magnetic beads overnight at 4 ℃, and was then incubated with detection antibody for 1 h at room temperature. Then, streptavidin-PE was added to each well for 30 min, and the values were read using the Luminex 200 system (Luminex Corporation, Austin, TX, USA).
RNA extraction of epithelium samples and qRT-PCR
Epithelium samples were divided into 3 groups due to the low amount of RNA from the lens epithelium, among which 8 to 12 epithelium samples were pooled together in the ARC group and 9 to 13 epithelium samples were pooled together in the DMC group. Total RNA from all epithelium samples was extracted using TRIzol reagent (15,596,026, Invitrogen, Carlsbad, CA, USA) and reverse transcribed with the RT reagent Kit (RR014A, Takara Bio, Inc, Japan) according to the manufacturer’s protocol. mRNA expression was detected using a SYBR Green detection kit (RR820A, Takara, Japan) on a LightCycler 480II Real-Time PCR System (Roche, Switzerland). GAPDH was detected as the internal control. RNA expression was determined by the 2−ΔΔCT method.
The forward primer of TGBF1 mRNA was GAAATTGAGGGCTTTCGCCTTAG, and the reverse primer of TGBF1 mRNA was GGTAGTGAACCCGTTGATGTCCA. The forward primer of TGBF2 mRNA was AAGCCAGAGTGCCTGAACAA, and the reverse primer of TGBF2 mRNA was GCGCTGGGTTGGAGATGTTA. The forward primer of TGBF3 mRNA was TGCCAAAGAAATCCATAAATTCGAC, and the reverse primer of TGBF3 mRNA was AGGTAATTCCTTTAGGGCAGACAGC.
Statistical analyses
All data are shown as the mean ± standard deviation. The detections of mRNA expression in each group were repeated three times, and the interval was one week between each time. Statistical significance was analysed by two-tailed Student’s t test or the chi-square test using IBM SPSS 25.0 (USA). The correlations of differences between TGF-β1, -β2, -β3 and fasting glucose and glycosylated haemoglobin were analysed by Pearson correlation analysis. A P value < 0.05 was considered statistically significant.
Results
Patient characteristics in the DMC and ARC groups
Sixty-nine eyes were enrolled in the two groups, among which there were 33 eyes in the DMC group and 36 eyes in the ARC group. In the DMC group, there were 9 males and 24 females and 23 right eyes and 10 left eyes. The mean age, mean fasting glucose and glycosylated haemoglobin of the DMC group were 69.85 ± 6.85 years old, 7.58 ± 1.90 mmol/L and 7.15 ± 1.03%, respectively. In the ARC group, there were 8 males and 28 females and 25 right eyes and 11 left eyes. The mean age, mean fasting glucose and glycosylated haemoglobin of ARC group were 70.36 ± 8.08 years old, 5.88 ± 0.75 mmol/L and 5.90 ± 0.57%, respectively. There were no statistically significant differences in gender, right or left eye, or age between the two groups (Table 1). The fasting glucose and glycosylated haemoglobin levels between the two groups were statistically significant (Table 1).
Different concentrations of TGF-β1, TGF-β2 and TGF-β3 in AH samples of the DMC and ARC groups
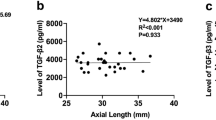
We used a Luminex liquid suspension chip to detect the concentrations of TGF-β1, TGF-β2 and TGF-β3 in AH samples of the DMC and ARC groups. This detection revealed that the concentration of TGF-β1 was 27.11 ± 7.58 pg/ml in AH samples of the DMC group and 20.13 ± 9.28 pg/ml in AH samples of the ARC group; the differences between the two groups were statistically significant (P value = 0.001) (Fig. 1a). The concentration of TGF-β2 was 2630.55 ± 550.90 pg/ml in AH samples of the DMC group and 2281.39 ± 681.72 pg/ml in AH samples of the ARC group; the differences between the two groups were statistically significant (P value = 0.023) (Fig. 1b). The concentration of TGF-β3 was 3.81 ± 1.64 pg/ml in AH samples of the DMC group and 3.35 ± 1.61 pg/ml in AH samples of the ARC group; however, the differences between the two groups were not statistically significant (P value = 0.249) (Fig. 1c).
The correlations of differences between TGF-β1, -β2, -β3 and fasting glucose and glycosylated haemoglobin analysed by Pearson correlation analysis
Results from Pearson correlation analysis between TGF-β1, -β2, -β3 and fasting glucose and glycosylated haemoglobin were shown in Table 2. According to Table 2, The difference of the correlation between TGF-β1 and glycosylated haemoglobin was significant (P value = 0.011, and Pearson correlation coefficient = 0.306). In addition, the difference of the correlation between TGF-β2 and glycosylated haemoglobin was significant (P value = 0.026, and Pearson correlation coefficient = 0.269).
We then made regression analysis of differences between TGF-β1 and glycosylated haemoglobin (P value = 0.026)(Fig. 2a), and between TGF-β2 and glycosylated haemoglobin (P value = 0.011)( Fig. 2b).
Differential TGFB1 and TGFB2 expression between DMC and ARC epithelium samples
qRT-PCR was adopted to test the mRNA expression of the TGFB1, TGFB2 and TGFB3 genes between DMC and ARC epithelium samples. The expression of TGFB1 and TGFB2 was significantly upregulated in DMC epithelium samples compared with ARC epithelium samples (P value in TGFB1 = 0.041, P value in TGFB2 = 0.021) (Fig. 3). Expression of TGFB3 was upregulated in DMC epithelium samples compared with ARC epithelium samples; however, the difference between the two groups was not statistically significant (P value = 0.171) (Fig. 3).
Discussion
Patients with diabetes are more likely to have cataracts. The progression of cataracts with diabetes is more rapid than that of cataracts without diabetes, although their symptoms are similar. Diabetes has long been recognized as an inflammation-related disease, and high expression of TGF-β is related to diabetes and diabetes-related ocular complications, such as diabetic retinopathy [13,14,15,16,17]. In the current study, we found increased expression of TGF-β1 and TGF-β2 in the AH of DMC patients compared with ARC patients by using a Luminex liquid suspension chip, suggesting a proinflammatory status in the anterior segment of DMC eyes.
TGF-β is a cytokine reported to be increased in complicating diabetes, eyes with acute primary angle closure, neovascular glaucoma secondary to proliferative diabetic retinopathy [12,13,14,15,16,17], and posterior capsule opacification [19]. AH contains numerous cytokines, including TGF-β. TGF-β was reported to be related to tissue fibrosis and epithelial–mesenchymal transition [20, 21]. Although TGF-β might play important roles in the development of diabetes and cataracts, very few studies have precisely evaluated the concentration of TGF-β in the AH of DMC eyes due to low expression of proteins in the AH or other reasons. Luminex liquid suspension chip detection could detect a large number of selected biomarkers on one membrane for samples containing very low protein concentrations [24, 25].
In our study, we used a Luminex liquid suspension chip to detect the concentrations of TGF-β1, TGF-β2 and TGF-β3 in AH samples of DMC and ARC eyes. The concentrations of TGF-β1, TGF-β2 and TGF-β3 in AH samples of DMC eyes were all higher than those of ARC eyes. However, only the differences in TGF-β1 and TGF-β2 between the two groups were statistically significant. In addition, the concentration of TGF-β2 was much higher than that of TGF-β1 and TGF-β3, which indicated that TGF-β2 might play an important role in the mechanism of diabetes and cataracts. TGF-β2 is related to fibrosis of lens epithelial cells promoted by advanced glycation end product formation [19] and is involved in several signalling pathways activated in epithelial–mesenchymal transition, such as the MAPK/ERK/JNK and PI3K/Akt/GSK3β pathways, Jagged-1/Notch signalling, and the miR-26a-5p/ITGAV/TGF-β/Smad3 axis [20,21,22]. Besides, TGF-β1 and -β2 were correlated with glycosylated haemoglobin, which indicated that TGF-β1 and -β2 might have important roles in diabetes and diabetes related complications. Therefore, the precise functions and mechanisms of TGF-β2 in diabetes and cataracts need to be investigated in future studies.
In addition, we tested the mRNA expression of TGFB1, TGFB2 and TGFB3 between DMC and ARC epithelium samples, which can translate TGF-β1, TGF-β2 and TGF-β3. We found that the mRNA expression levels of TGFB1, TGFB2 and TGFB3 were all upregulated in DMC epithelium samples compared with ARC epithelium samples. However, only the differences in TGFB1 and TGFB2 between the two groups were statistically significant, which was equivalent to the TGF-β1 and TGF-β2 results between the two groups. TGF-β1, -β2 and -β3 were translated by TGFB1, TGFB2 and TGFB3 genes. However, the precise reasons causing the increasing of TGF-β1 and -β2 in the AH of the DMC group remained unclear. In our future study, if possible, detection of TGF-β1, -β2 and -β3 concentrations in the vitreous humour of DMC group and a correlation analysis of TGF-β1, -β2 and -β3 concentrations between the AH and the vitreous humour might be significant.
In our previous study, we successfully isolated abundant exosomes from AH samples in the DMC and ARC groups and found that exosomal miRNAs could target the mRNAs of certain genes to affect the viability and apoptosis of human lens epithelial cells. For example, high expression of miR-551b could downregulate CRYAA expression, thus decreasing the transparency of the lens [26], and low expression of miR-29b could upregulate CACNA1C expression, resulting in an increased concentration of Ca2+ in the AH of DMC eyes [27]. The miR-26a-5p/ITGAV/TGF-β/Smad3 axis was also reported to be involved in cell viability, migration and epithelial–mesenchymal transition in diabetic cataracts [22]. These results indicated that increased TGF-β in the AH of DMC eyes might be activated by other factors, such as exosomal miRNAs, which might have important roles in the formation and development of diabetes and cataracts.
In conclusion, we found that the concentrations of TGF-β1 and TGF-β2 in AH samples were significantly higher in DMC eyes than in ARC eyes, and TGF-β1 and -β2 were correlated with glycosylated haemoglobin. The mRNA expression of TGFB1 and TGFB2 was significantly upregulated in DMC epithelial samples compared with ARC epithelial samples. These findings suggest that the anterior chamber of DMC eyes is characterized by a proinflammatory state that may predispose them to the occurrence of certain inflammation-related complications.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary files.
Abbreviations
- TGF:
-
Transforming growth factor
- AH:
-
Aqueous humour
- DMC:
-
Diabetes and cataracts
- ARC:
-
Age-related cataracts
- qRT-PCR:
-
Quantitative real-time polymerase chain reaction
References
Collins JG, Corder CN. aldose reductase and sorbitol dehydrogenase distribution in substructures of normal and diabetic rat lens. Invest Ophthalmol Vis Sci. 1977;16(3):242.
Weifeng G, Guangyue Z, Jie L, Xin Y. lncRNA MALAT1 promotes the apoptosis and oxidative stress of human lens epithelial cells via p38MAPK pathway in diabetic cataract. Diabetes Res Clin Pract. 2018;144:314–21.
Qi M, Elion EA. MAP kinase pathways. J Cell Sci. 2005;118(16):3569–72. https://doi.org/10.1242/jcs.02470.
Hailiang W, De-Kuang H, Xudong S, Yong T. association between aqueous cytokines and diabetic retinopathy stage. J Ophthalmol. 2017;2017:1–8.
Takeuchi M, Sato T, Sakurai Y, Taguchi M, Harimoto K, Karasawa Y, Ito M. association between aqueous humor and vitreous fluid levels of Th17 cell-related cytokines in patients with proliferative diabetic retinopathy. PLoS ONE. 2017;12(5): e0178230. https://doi.org/10.1371/journal.pone.0178230.
Kuzmin A, Lipatov D, Chistyakov T, Smirnova O, Arbuzova M, Ilin A, Shestakova M, Dedov I. vascular endothelial growth factor in anterior chamber liquid patients with diabetic retinopathy, cataract and neovascular glaucoma. Ophthalmol Ther. 2013;2(1):41–51. https://doi.org/10.1007/s40123-013-0014-3.
Hamid S, Gul A, Hamid Q. relationship of cytokines and AGE products in diabetic and non-diabetic patients with cataract. Int J Health Sci. 2016;10(4):507. https://doi.org/10.12816/0048891.
Neumann S, Linek J, Loesenbeck G, Schüttler J, Gaedke S. TGF-β1 serum concentrations and receptor expressions in the lens capsular of dogs with diabetes mellitus. Open Vet J. 2017;7(1):12–5. https://doi.org/10.4314/ovj.v7i1.2.
Iongh RUD, Gordon-Thomson C, Chamberlain CG, Hales M, Avoy JWMC. TGFβ receptor expression in lens: implications for differentiation and cataractogenesis. Exp Eye Res. 2001;72(6):649–59. https://doi.org/10.1006/exer.2001.1001.
Lovicu FJ, Schulz MW, Hales AM, Vincent LN, Overbeek PA, Chamberlain CG, McAvoy JW. TGFbeta induces morphological and molecular changes similar to human anterior subcapsular cataract. Br J Ophthalmol. 2002;86(2):220–6. https://doi.org/10.1136/bjo.86.2.220.
Li D, Liu GQ, Lu PR. high glucose: activating autophagy and affecting the biological behavior of human lens epithelial cells. Int J Ophthalmol. 2019;12(7):1061–6.
Chen Y, Yan H, Li G, Zhang Y. higher TGF-β1, TGF-β2, MMP-2, and TIMP-1 Levels in the Aqueous Humor of Patients with Acute Primary Angle Closure. Ophthalmic Res. 2021;64:62–7.
Yamamoto N, Itonaga K, Marunouchi T, Majima K. concentration of transforming growth factor ß2 in aqueous humor. Ophthalmic Res. 2005;37:29–33.
Zhang H, Liang L, Huang R, Wu P, He L. comparison of inflammatory cytokines levels in the aqueous humor with diabetic retinopathy. Int Ophthalmol. 2020;40:2763–9.
Khuu LA, Tayyari F, Sivak JM, Flanagan SJG, Singer S, Brent MH, Huang D, Tan O, Hudson C. Aqueous humour concentrations of TGF-β, PLGF and FGF-1 and total retinal blood flow in patients with early non-proliferative diabetic retinopathy. Acta Ophthalmol. 2017;95(3):e206–11. https://doi.org/10.1111/aos.13230.
Ochiai Y, Ochiai H. Higher concentration of transforming growth factor-β in aqueous humor of glaucomatous eyes and diabetic Eyes. Jpn J Ophthalmol. 2002;46(3):249–53.
IshikawaKohnoMoriMurakamiNakaoAkiyamaYoshidaSonoda KRIKYSMSKH. increased expression of periostin and tenascin-C in eyes with neovascular glaucoma secondary to PDR. Graefes Arch Clin Exp Ophthalmol. 2020;258:2.
KuboShibataSinghSasaki ETDH. roles of TGF β and FGF signals in the Lens: tropomyosin regulation for posterior capsule opacity[J]. Int J Mol Sci. 2018;19:10.
Raghavan CT, Smuda M, Smith A, Howell S, Smith D, Singh A, Gupta P, Glomb M, Wormstone IM, Nagaraj R. ages in human lens capsule promote the TGFβ2-mediated EMT of lens epithelial cells: implications for age-associated fibrosis[J]. Aging Cell. 2016;15(3):465–76.
Shukal D, Bhadresha K, Shastri B, Mehta D, Vasavada A, Johar SR K. dichloroacetate prevents TGFβ-induced epithelial-mesenchymal transition of retinal pigment epithelial cells[J]. Exp Eye Res. 2020;197:108072.
Chen X, Xiao W, Chen W, Liu X, Wu M, Bo Q, Luo Y, Ye S, Cao Y, Liu Y. microRNA-26a and -26b inhibit lens fibrosis and cataract by negatively regulating Jagged-1/Notch signaling pathway[J]. Cell Death Differ. 2017;1:12.
Liu J, Dong Y, Wen Y, Shi L, Zhu Z, Ke G, Gu Y. LncRNA KCNQ1OT1 knockdown inhibits viability, migration and epithelial-mesenchymal transition in human lens epithelial cells via miR-26a-5p/ITGAV/TGF-beta/Smad3 axis[J]. Exp Eye Res. 2020;200:108251.
Han Z, Fang W, Wang F, Liu Q, Zhou J. regulation of transforming growth factor β-mediated epithelial-mesenchymal transition of lens epithelial cells by c-Src kinase under high glucose conditions[J]. Exp Ther Med. 2018;16:1520–8.
Zhu X, Zhang K, He W, Yang J, Sun X, Jiang C, Dai J, Lu Y. proinflammatory status in the aqueous humor of high myopic cataract eyes[J]. Exp Eye Res. 2016;142:13–8.
Liu W, Wang W, Wang X, Xu C, Zhang N, Di W. cisplatin-stimulated macrophages promote ovarian cancer migration via the CCL20-CCR6 axis[J]. Cancer Lett. 2020;472:59–69.
Gao C, Fan F, Liu X, Yang J, Zhou X, Mei H, Lin X, Luo Y. exosomal miRNA analysis of aqueous humour of diabetes and cataract patients. Curr Eye Res. 2021;46(3):324–32.
Gao C, Liu X, Fan F, Yang JN, Zhou XY, Mei HJ, Lin XL, Luo Y. exosomal miR-29b found in aqueous humour mediates calcium signaling in diabetic patients with cataract. Int J Ophthalmol. 2021;14(10):484–1491.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Natural Science Foundation of China (81870645), including the fund of materials and the use of instruments mentioned in the study. The funding bodies played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
Chao Gao designed the study, conducted part of experiments, analyzed part of data, and was a major contributor in writing the article. Xiaolei Lin designed the study, conducted part of experiments, collected samples, analyze part of data, and write part of the article.Fan Fan conducted part of experiments, collected samples, and write part of the article.Xin Liu conducted part of experiments, helped collected samples, and proofread part of the article.Huijuan Wan conducted part of experiments, helped collected samples, and proofread part of the article.Ting Yuan conducted part of experiments, helped collected samples, and proofread part of the article.Xinrong Zhao conducted part of experiments, helped collected samples, and proofread part of the article.Yi Luo was the corresponding author, designed the study, proofread and approved the final version of the article. All authors have read and approved the study.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The use of AH samples from cataract eyes during surgery was approved by the Institutional Review Board of Eye and ENT hospital of Fudan University. This study was performed in accordance with the tenets of the Declaration of Helsinki for research involving human subjects. Written informed consent was obtained from every enrolled participant.
Consent for publication
Not applicable.
Competing interests
There are no competing interests in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gao, C., Lin, X., Fan, F. et al. Status of higher TGF-β1 and TGF-β2 levels in the aqueous humour of patients with diabetes and cataracts. BMC Ophthalmol 22, 156 (2022). https://doi.org/10.1186/s12886-022-02317-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-022-02317-x