Abstract
Background
Coxsackieviruses are members of a group of viruses called the enteroviruses, which may cause respiratory and gastrointestinal symptoms, erythema, meningoencephalitis, myocarditis, pericarditis, and myositis. Unilateral acute idiopathic maculopathy caused by coxsackievirus A16 has been associated with hand, foot, and mouth disease, but only a few reports describe retinitis associated with coxsackievirus serotype B3 or B4. We report a case of bilateral multifocal obstructive retinal vasculitis that developed after coxsackievirus A4 infection.
Case presentation
A 60-year-old woman was referred to our department with bilateral visual disturbance that developed following flu-like symptoms. At the initial examination, best corrected visual acuity was 20/200 in the right eye and 20/50 in the left eye. The critical flicker frequency (CFF) was 23 Hz in the right eye and 27 Hz in the left eye. Fine white keratic precipitates with infiltrating cells were presented in the anterior chamber of both eyes, and multifocal retinal ischemic lesions were observed in the macula and posterior pole of both eyes. The retinal lesions corresponded with scotomas observed in Goldmann visual field test. On spectral domain-optical coherence tomography (SD-OCT), retinal lesions were depicted as hyper-reflective regions in the inner retina layers in both eyes, and disruption of ellipsoid line in the left eye., Fluorescein angiography exhibited findings indicative of multifocal obstructive retinal vasculitis. The patient had a history of current hypertension treated with oral therapy and glaucoma treated with latanoprost eye drops. Blood test for coxsackievirus antibody titers revealed that A4, A6, A9, B1, B2, B3, and B5 were positive (titers: 8–32). Abdominal skin biopsy of necrotic tissue suggested vascular damage caused by coxsackievirus. The general symptoms improved after 6 weeks, and the multifocal retinal ischemic lesions were partially resolved with residual slightly hard exudates. Only coxsackievirus A4 antibody titer increased from 4 to 32-fold after 14 months. However, hyper-reflective regions and disruption of the inner retinal layers on SD-OCT persisted especially in the right eye, and residual paracentral scotoma was observed in the right eye.
Conclusion
The present case suggests that coxsackievirus A4 causes bilateral multifocal obstructive retinal vasculitis with irreversible inner retinal damage.
Similar content being viewed by others
Background
Coxsackieviruses belong to the enterovirus genus of the family Picornaviridae, and are classified into two groups: A and B. Group A coxsackieviruses cause flaccid paralysis, whereas group B coxsackieviruses cause spastic paralysis. Regarding concurrent coxsackievirus infection in the posterior segment of the eye, many reports have described an association of hand, foot, and mouth disease caused by coxsackievirus A16 with unilateral acute idiopathic maculopathy (UAIM) [1,2,3,4,5,6,7,8]. However, there are few reports of retinitis associated with coxsackievirus, and only serotype B3 or B4 was reported [9,10,11,12]. Herein, we report a patient with reduced visual acuity caused by coxsackievirus A4-induced bilateral multifocal obstructive retinal vasculitis, which was observed by multimodal imaging.
Case presentation
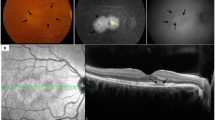
A 60-year-old female had flu-like symptoms from November 1, 2013, and subsequently developed fever, articular pain, retroauricular lymph node swelling, erythema, and dizziness with gait disturbance 4 days later. The patient was admitted to the Department of Internal Medicine at National Defense Medical College Hospital for detailed examination. Nine days after onset, the patient complained of bilateral visual disturbance and was referred to our department. She has a history of current hypertension treated with oral therapy and glaucoma treated with latanoprost eye drops. At the initial ophthalmological examination, best corrected visual acuity was 20/200 in the right eye and 20/50 in the left eye, and intraocular pressure was normal in both eyes. The critical flicker frequency (CFF) was 23 and 27 Hz for the right and left eye, respectively, and a relative afferent pupil defect was noted in the right eye. Slit lamp examination showed fine white keratic precipitates with infiltrating cells in the anterior chamber in both eyes. Funduscopy revealed multifocal retinal ischemic lesions around the macula and posterior pole in both eyes. (Fig. 1a and b). Scotoma areas corresponding with the retina lesions were observed by Goldmann visual field test (Fig. 2). On SD-OCT, multifocal white retinal lesions were depicted as hyper-reflective regions in the inner retina layers of both eyes, and disruption of ellipsoid line was observed in the left eye (Fig. 1c and d). Fluorescein angiography (FA) showed bilateral filling defects corresponding to the retinal lesions, which were surrounded by dye leakage from retinal capillaries (Fig. 3a and b). Indocyanine green angiography depicted no abnormalities in both eyes (Fig. 3c and d). Brain and orbital MRI were also performed, but the result was not particular.
Fundus photographs and SD-OCT images at the initial examination. a and b Fundus photographs show multifocal ischemic lesions around the macula and posterior pole in both right (a) and left (b) eyes. c and d SD-OCT reveals hyper-reflective regions in the inner retina layers in both right (c) and left (d) eyes, and disruption of ellipsoid line in the left eye
Fluorescein and indocyanine green angiography. a and b Fluorescein angiography reveals filling defect in the affected part of the retina with leakage of fluorescence dye from the surrounding retinal blood vessels in both right (a) and left (b) eyes. c and d Indocyanine green angiography reveals no abnormalities in both right (c) and left (d) eyes
On day 12 after onset of ocular symptoms, aqueous humor sample was collected and tested using multiplex polymerase chain reaction (PCR) for human herpes virus (HHV) 1–8, toxoplasma, toxascaris, bacterial 16srDNA, and fungal 28srDNA, all of which were negative. On the same day, treatment with betamethasone and phenylephrine tropicamide eye drops was initiated. Blood test for coxsackievirus antibody titers revealed that A4, A6, A9, B1, B2, B3, and B5 were positive (titers: 8–32; Table 1). An abdominal skin biopsy of necrotic tissue suggested vascular damage caused by coxsackievirus. On the other hand, since the patient fulfilled the diagnostic criteria for polymyalgia rheumatic (PMR), oral corticosteroid (15 mg/day prednisolone) was initiated on November 25, 2013.
The general symptoms improved after 6 weeks, and the multifocal retinal ischemic lesions were partially resolved and residual exudates were slightly hard. (Fig. 4a and b). However, hyper-reflective regions and disruption of the inner retinal layers on SD-OCT persisted, especially in the right eye (Fig. 4c and d). The steroid dose was tapered, and from March 2015, the patient was put under follow-up observation with prednisolone 1 mg/day. After 14 months, the coxsackievirus A4 antibody titer increased by 32-fold (Table 1). Corrected visual acuity was 20/25 in the right eye and 20/15 in the left eye, and residual paracentral scotoma was observed in the right eye (Fig. 5).
Fundus photographs and SD-OCT image after 14 months. (a and b) The fundus photographs show slightly hard exudates in both right (a) and left (b) eyes. (c and d) Hyper-reflective regions and disruption of the inner retinal layers persist in both right (c) and left (d) eyes, especially in the right eye
Conclusions
Although coxsackievirus is apparently a rare cause of multifocal obstructive retinal vasculitis, it should be considered in the appropriate clinical setting. Since it has become more convenient to detect several HHV by multiplex PCR using ocular fluid, reports of HHV-related ocular diseases are increasing [13]. However, such convenient tests are not available for the detection of coxsackieviruses, and currently diagnosis still depends on clinical signs such as flu-like symptoms and changing antibody titers after resolution of the infection. When molecular biological techniques become a standard method for the detection of coxsackieviruses, more cases of coxsackievirus-associated ocular disease may be diagnosis with a heightened level of suspicion.
In the present case, obstructive retinal vasculitis appeared to be induced via immune response to virus infection, similar to the clinical conditions of acute retinal necrosis caused by HHV1, HHV2 or HHV3, and the skin necrosis probably resulted from impaired blood flow because of the same mechanism. Several cases of retinitis associated with coxsackievirus have been reported [8,9,10,11]. Takeuchi et al. [9] reported a case of coxsackievirus B4 infection causing iridocyclitis and obstructive retinal vasculitis. Other case reports described coxsackievirus-associated macular lesion with posterior segment inflammation, similar to UAIM [8, 10, 11]. However, the serotype of coxsackievirus in all the above cases was “B”, and most of the lesions were reversible. Coxsackievirus A4-associated retinitis leads to bilateral irreversible retinal damage has not been reported previously.
In summary, we have described the clinical features of coxsackievirus A4-associated retinitis and bilateral obstructive vasculitis causing irreversible retinal damage. Abnormalities on FA and SD-OCT suggest the critical role of inflammation at the level of inner retinal layers. SD-OCT was especially valuable for monitoring partial changes of the entire retinal layers.
Abbreviations
- CFF:
-
Critical flicker frequency
- HHV:
-
Human herpes virus
- PCR:
-
Polymerase chain reaction
- PMR:
-
Polymyalgia rheumatic
- SD-OCT:
-
Spectral domain-optical coherence tomography
- UAIM:
-
Unilateral acute idiopathic maculopathy
References
Beck AP, Jampol LM, Glaser DA, Pollack JS. Is coxsackievirus the cause of unilateral acute idiopathic maculopathy? Arch Ophthalmol 2004;122(1):121-123. Epub 2004/01/14. doi: 10.1001/archopht.122.1.121. PubMed PMID: 14718310.
Meyerle CB, Yannuzzi LA. Acute positive titers of antibody to coxsackievirus in acute idiopathic maculopathy. Retin Cases Brief Rep. 2008;2(1):34-35. Epub 2008/01/01. doi: 10.1097/01.iae.0000243065.91330.e0. PubMed PMID: 25389612.
Hughes EH, Hunyor AP, Gorbatov M, Ho IV. Acute idiopathic maculopathy with coxsackievirus infection. Retin Cases Brief Rep. 2012;6(1):19-21. Epub 2012/01/01. doi: 10.1097/ICB.0b013e3181f7f7ee. PubMed PMID: 25390701.
Jung CS, Payne JF, Bergstrom CS, Cribbs BE, Yan J, Hubbard GB, 3rd, et al. Multimodality diagnostic imaging in unilateral acute idiopathic maculopathy. Arch Ophthalmol. 2012;130(1):50–56. doi: 10.1001/archophthalmol.2011.359. PubMed PMID: 22232475; PubMed Central PMCID: PMCPMC4116109.
Demirel S, Batioglu F, Ozmert E, Batioglu F. Unilateral acute maculopathy related to hand, foot, and mouth disease: OCT and fluorescein angiography findings of a very rare disease. Eur J Ophthalmol 2014;24(1):131-133. Epub 2013/05/11. doi: 10.5301/ejo.5000288. PubMed PMID: 23661540.
Vaz-Pereira S, Macedo M, De Salvo G, Pal B. Multimodal imaging of exudative maculopathy associated with hand-foot-mouth disease. Ophthalmic Surg Lasers Imaging Retina. 2014;45 Online:e14–e17. doi: 10.3928/23258160-20140331-01. PubMed PMID: 24695047.
Tandon M, Gupta A, Singh P, Subathra G. Unilateral hemorrhagic maculopathy: An uncommon manifestation of hand, foot, and mouth disease. Indian J Ophthalmol. 2016;64(10):772–4. doi:10.4103/0301-4738.195014.
Haamann P, Kessel L, Larsen M. Monofocal outer retinitis associated with hand, foot, and mouth disease caused by coxsackievirus. Am J Ophthalmol. 2000;129(4):552–553. doi: http://dx.doi.org/10.1016/S0002-9394(99)00440-7.
Takeuchi M, Sakai J, Usui M. Coxsackievirus B4 associated uveoretinitis in an adult. Br J Ophthalmol. 2003;87(4):501–2. doi:10.1136/bjo.87.4.501.
Kadrmas E, Buzney S. Coxsackievirus B4 as a cause of adult chorioretinitis. Am J Ophthalmol. 1999;127(3):347–349. doi: http://dx.doi.org/10.1016/S0002-9394(98)00322-5.
Hirakata K, Oshima T, Azuma N. Chorioretinitis induced by coxsackievirus B4 infection. Am J Ophthalmol 1990;109(2):225-227. Epub 1990/02/15. PubMed PMID: 2154107.
Hollsten JE, McClintock M, Samy H, Peden M, Kay CN. Fulminant chorioretinitis and papillitis secondary to coxsackievirus B presenting as acute posterior multifocal placoid pigment epitheliopathy with positive response to intravenous immunoglobulin. Retin Cases Brief Rep 2013;7(3):225-231. Epub 2013/07/01. doi: 10.1097/ICB.0b013e31828993c6. PubMed PMID: 25391111.
Sugita S, Ogawa M, Shimizu N, Morio T, Ohguro N, Nakai K, et al. Use of a comprehensive polymerase chain reaction system for diagnosis of ocular infectious diseases. Ophthalmology 2013;120(9):1761-1768. doi: 10.1016/j.ophtha.2013.02.020. PubMed PMID: 23664179.
Acknowledgements
None.
Funding
No funding was received by any of the authors for writing of this manuscript.
Availability of data and materials
The fundus photographs, visual fields, and serial optical coherence tomography images supporting the results of this article are included within the article.
Author information
Authors and Affiliations
Contributions
IM made substantial contributions to conception and design, or acquisition of data. MT1 and IM analyzed and interpreted the data. IM and YS have been involved in drafting the manuscript. MT1 and MT2 revised the manuscript critically for important intellectual content. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for individual case presentation is not required by the ethics committee of National Defense Medical College, Japan. Informed consent was obtained after an explanation of the nature and possible consequences of the study.
Consent for publication
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Mine, I., Taguchi, M., Sakurai, Y. et al. Bilateral idiopathic retinal vasculitis following coxsackievirus A4 infection: a case report. BMC Ophthalmol 17, 128 (2017). https://doi.org/10.1186/s12886-017-0523-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-017-0523-2