Abstract
Background
Age-related macular degeneration (AMD) is the leading cause of irreversible blindness in older individuals. Our study aims to identify the key genes and upstream regulators in AMD.
Methods
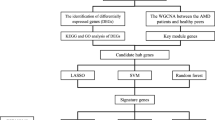
To screen pathogenic genes of AMD, an integrated analysis was performed by using the microarray datasets in AMD derived from the Gene Expression Omnibus (GEO) database. The functional annotation and potential pathways of differentially expressed genes (DEGs) were further discovered by Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analysis. We constructed the AMD-specific transcriptional regulatory network to find the crucial transcriptional factors (TFs) which target the DEGs in AMD. Quantitative real time polymerase chain reaction (qRT-PCR) was performed to verify the DEGs and TFs obtained by integrated analysis.
Results
From two GEO datasets obtained, we identified 1280 DEGs (730 up-regulated and 550 down-regulated genes) between AMD and normal control (NC). After KEGG analysis, steroid biosynthesis is a significantly enriched pathway for DEGs. The expression of 8 genes (TNC, GRP, TRAF6, ADAMTS5, GPX3, FAP, DHCR7 and FDFT1) was detected. Except for TNC and GPX3, the other 6 genes in qRT-PCR played the same pattern with that in our integrated analysis.
Conclusions
The dysregulation of these eight genes may involve with the process of AMD. Two crucial transcription factors (c-rel and myogenin) were concluded to play a role in AMD. Especially, myogenin was associated with AMD by regulating TNC, GRP and FAP. Our finding can contribute to developing new potential biomarkers, revealing the underlying pathogenesis, and further raising new therapeutic targets for AMD.
Similar content being viewed by others
Background
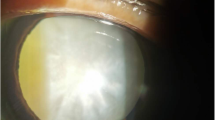
Age-related macular degeneration (AMD) is the leading cause of irreversible blindness in older individuals [1, 2]. Pathological deposits (drusen) between the Bruch’s membrane and retinal pigment epithelium (RPE) are closely associated with early stage AMD [3]. Late AMD can be classified into the dry form and the wet form [4]. Dry AMD is mainly caused by atrophy of RPE. Wet AMD is characterized by choroidal neovascularization (CNV), subretinal haemorrhage, photoreceptor loss, retinal detachment and visual loss [5, 6].
Age is the major risk factor associated with AMD, but beyond that, vascular endothelial growth factor (VEGF), oxidative stress, inflammation, complement system are associated with risk of AMD [7]. Despite many efforts for AMD research in recent decades, effective treatments remain absent [8, 9].
With advances in various high-throughput technologies, amounts of key genes which are associated with the process of disease were identified by microarray [10,11,12]. Using multiple microarray datasets, integrated analysis could identified differentially expressed genes (DEGs) with more accuracy, and increased the statistical power compared with a single microarray study. Exploring the upstream transcription factors (TFs) mediating abnormal gene expression in disease status can help to understand pathophysiological changes in complex diseases.
In this study, we performed integrated analysis of multiple microarray datasets to identify DEGs between AMD and normal control (NC) groups, which may be used as potential diagnostic biomarkers for AMD. In addition, we identified several crucial TFs which target the DEGs in AMD. The aim of this study is to better characterize the molecular events and pathways of AMD and to raise new strategies of treatment for AMD.
Methods
Eligible gene expression profiles of AMD
We selected gene expression datasets of AMD on the Gene Expression Omnibus database (GEO, http://www.ncbi.nlm.nih.gov/geo) which is the largest database of high-throughput gene expression data. Selected datasets should be whole-genome expression profile data in AMD patients and NC groups. Datasets with drug stimulation or transfection were excluded.
Identify DEGs in AMD compared to NC
Background correction was performed for the raw data. Differential expression p-values were calculated by two-tailed Student’s t-test, we combined these p-values by the inverse normal method. Finally, the DEGs between AMD and NC groups were identified with criterion of P-value < 0.05.
Functional annotation
To reveal the function and the potential pathway of DEGs, Gene Ontology (GO) classification (molecular functions, biological processes and cellular component) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment were performed by using the online software GeneCodis (http://genecodis.cnb.csic.es/analysis).FDR < 0.05 was defined as the criteria of statistical significance.
AMD-specific protein-protein interaction (PPI) network construction
To further research the biological functions of DEGs, the top 30 DEGs in AMD were used to construct the PPI network by using Biological General Repository for Interaction Datasets (BioGRID) (http://thebiogrid.org/) and Cytoscape. We used nodes and edges to represent the proteins and interactions between two proteins respectively.
Construction of AMD-specific transcriptional regulatory networks
TFs could regulate gene transcription by binding to specific DNA sequences generally located in the promoter region of genes. Based on the integrated analysis, the corresponding promoters of the top ten up-regulated or down-regulated DEGs were obtained by UCSC Genome Bioinformatics (http://genome.ucsc.edu).TheTFsinvolved in regulating these DEGs were derived from the match tools in TRANSFAC which is a database of transcription factor. The transcriptional regulatory network was constructed by Cytoscape software (http://www.cytoscape.org/).
qRT-PCR confirmation
Patients with wet AMD in evolutionary stage and sex- and age-matched normal controls were recruited in our study. The exclusion criteria for AMD patients were as follows: (1) Patients with other ocular organic disease; (2) Patients with glaucoma, polypoidal choroidal vasculopathy and other ocular lesions. The NCs with ocular lesions or other serious medical illness were excluded. The detailed characteristics of AMD patients were displayed in Table 1.
Blood samples from 3 ADM patients (Case 1–3) and 3 NCs were collected and frozen at 80 °C within 2 h after blood withdrawal. After thawing the frozen samples at room temperature, 1 ml of the sample was used to perform RNA isolation with Trizol reagent (Invitrogen, China) according to the manufacturer’s instructions. By using SuperScript® III Reverse Transcriptase (Invitrogen, China), we generated cDNA from 1μgextracted RNA. With Power SYBR® Green PCR Master Mix (Applied Biosystems, USA), we performed quantitative PCR in an ABI 7500 real-time PCR system. Relative gene expression was analyzed using 2-ΔΔCt method. The human 18srRNA was used as endogenous control for mRNA expression in analysis.
Results
Differential expression analysis of genes in AMD
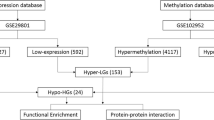
Two RNA-seq datasets (GSE90889 and GSE67898) of AMD were excluded due to that the data of these two datasets were obtained after treatment with nicotinamide and TGFβ receptor kinase inhibitor, A-83-01, respectively. Two gene expression microarray datasets (GSE50195, GSE29801) without drug stimulation or transfection were enrolled in this study (Table 2). Compared with the normal controls, 1280 DEGs in AMD were obtained with P < 0.05, among which, 730 genes were up-regulated and 550 genes were down-regulated. The top 30 most significantly up or down-regulated genes were listed in Table 3.The heat map of top 100 most significantly up or down-regulated genes (P-value < 0.05) in AMD was showed in Fig. 1.
Functional annotation
As the results of GO enrichment analysis (FDR < 0.05, Additional file 1: Table S1), the DEGs were significantly enriched in regulation of transcription, DNA-dependent (FDR = 4.74E-08), cellular nitrogen compound metabolic process (FDR = 1.25E-06), cholesterol biosynthetic process (FDR = 1.30E-06), membrane (FDR = 1.53E-31), cytoplasm (FDR = 2.17E-31), protein binding (FDR = 3.70E-30) and DNA binding (FDR = 4.60E-17). After the KEGG pathway enrichment analysis (FDR < 0.05, Table 4), several pathways were significantly enriched, including valine, leucine, isoleucine degradation (FDR = 4.19E-08), steroid biosynthesis (FDR = 1.74E-07) and WNT signaling pathway (FDR = 1.02E-05). 8 DEGs (DHCR7, FDFT1, CYP27B1, TM7SF2, SQLE andSOAT2) were significantly enriched in the steroid biosynthesis which are associated with AMD (Table 5 and Fig. 2).
AMD-specific protein-protein interaction (PPI) network
The PPI network of top 30 DEGs in AMD was consisted of 559 nodes and 583 edges (Fig. 3). The hub proteins were TRAF6 (degree = 225) and TP53BP1 (degree = 108).
The PPI network of top 30 significantly DEGs in AMD. The blue ellipses were represented the proteins encoded by down-regulated DEGs and the red ellipses were represented the proteins encoded by up-regulated DEGs. Among which, ellipses with red border were derived from the top 30 DEGs in AMD. The green ellipses were represented other proteins
Transcriptional regulatory network
Based on TRANSFAC, 43 TFs targeting 20 DEGs (top 10 up-regulated or down-regulated genes) were identified. AMD-specific transcriptional regulatory network was constructed, which consisted of 119 TF-target interactions (Fig. 4). Among of them, c-rel, myogenin, CDP and CCAAT were top 4 TFs covering the most downstream DEGs.
qRT-PCR confirmation
To verify the expression of integrated analysis, the expression of eight selected genes including Tenascin-C (TNC), fibroblast activation protein alpha (FAP), glutathione peroxidase 3 (GPX3), gastrin-releasing peptide (GRP), ADAM metallopeptidase with thrombospondin type 1 motif 5 (ADAMTS5), TNF receptor associated factor 6 (TRAF6), DHCR7 (7-dehydrocholesterol reductase) and FDFT1 (farnesyl-diphosphate farnesyl transferase 1) were selected to tested by qRT-PCR. Since steroid biosynthesis is a significantly enriched pathway in AMD (FDR = 1.74E-07), the expression of two DEGs (DHCR7 and FDFT1) enriched in steroid biosynthesis were selected to tested by qRT-PCR. The other 6 selected DEGs for qRT-PCR confirmation were derived from the top 30 DEGs. Moreover, TNC was the most significantly DEG in AMD and TRAF6 (degree = 225) was the hub gene based on the AMD-specific PPT network. Based on previous studies, TRAF6 and GPX3 were two AMD-related DEGs [13, 14], two DEGs (FAP and GRP) were choroidal neovascularization-related genes [15, 16] and ADAMTS5 was a retinal pigment epithelium-related DEG [17] which may be involved with AMD. Hence, these six DEGs were selected to be tested by qRT-PCR as well. Except for TNC and GPX3, the expression of other 6 selected genes in qRT-PCR was consistent with our integrated analysis (Fig. 5).
Discussion
To better reveal the pathogenesis and find more effective treatment for AMD, we performed this integrated analysis between AMD patients and NC groups. 1280 genes across the studies were consistently differentially expressed in AMD (730up-regulated and 550 down-regulated) with P<0.05. Among the top 30 up-regulated or down-regulated DEGs, we selected TNC, FAP, GPX3, GRP, ADAMTS5 and TRAF6 to verify their expression in AMD. Except for TNC and GPX3, the other 4 genes in qRT-PCR played the same pattern with that in our integrated analysis, adding evidences to the reliability of results in the integrated analysis.
As one of extracellular matrix glycol proteins produced by culture fibroblasts, TNC was reported to be up-regulated in AMD [5, 18]. According to our integrated analysis, TNC was increased as well. VEGF is a major pathogenic factor for wet AMD [18] which can promote angiogenesis, vascular permeability and induce macular eduma (ME) [19]. Animal studies have demonstrated that the up-regulation of VEGF is a cause of CNV in the RPE [20]. Since TNC can up-regulate the expression of VEGF, so we concluded that increased TNC may play a role in the process of AMD by regulating CNV. In addition, AMD is associated with degeneration of RPE [21], increased TNC may involve with AMD by repressing the adhesion and migration of RPE. However, the expression of TNC was down-regulated in the blood of AMD patients, larger scale of studies were needed.
FAP is known to be involved in the control of fibroblast growth, which was speculated to be a pioneer for the growth of corneal neovascularization [15]. The up-regulation of FAP detected in this study may be closely associated with AMD by influencing the CNV as well.
To our best knowledge, none of previous studies have reported the association between AMD and GRP. GRP was reported to be involved in the induction of angiogenesis during neuroblastoma progression [16], which showed up-regulation in AMD in our study. Hence, we suspected that increased GRP may play an important role in CNV of AMD.
ADAMTS5 (also known as ADAMTS11) is a member of ADAMTS family. The ADAMTS family has been reported to involve with embryonic development, angiogenesis and cartilage degradation [17]. Bevitt et al. reported the expression of ADAMTS genes in an ocular cell type, ARPE-19 and their regulation by TNF-α. TNF-α is known to play a role in the development of retinal neovascularisation and RPE migration in AMD [17]. Hence, ADAMTS genes may involve with AMD and other retinal pathologies by regulating the proteolytic modification of the retinal extracellular matrix (REM) [17]. According to our study, up-regulated ADAMTS5 was detected in AMD, which supported this hypothesis.
TRAF6 has been reported to involve with the process of AMD by regulating signal transduction pathway [13]. In our study, the expression of TRAF6 was down-regulated. The precise role of TRAF6 in AMD was not clear.
The expression of GPX3 has been reported to be up-regulated in the blood of late AMD patients which was presumably due to oxidative stress [14]. In our integrated analysis, the expression of GPX3 was increased. However, down-regulation of GPX3 was detected in the blood of AMD patients and further research was needed.
After function annotation analysis, we found that steroid biosynthesis was a significantly enriched pathway for DEGs. And previous studies have reported that steroids may play a role for the treatment of AMD [22, 23], while mechanism underlying was not clear [24]. As one of steroids, high level of cholesterol was suspected to increase the risk for AMD by promoting the formation of drusen [25,26,27], since drusen is a major hallmark of AMD which contains lipid such as cholesterol [28,29,30]. Both DHCR7 and FDFT1 are associated with cholesterol biosynthesis, which were up-regulated in AMD in our study. DHCR7 catalyzes the reduction of DHC7 to cholesterol and deficiency of DHCR7 results in decreased cholesterol and increased DHC7 levels in serum and tissue [31]. FDFT1 (also called squalene synthase) catalyzes the biosynthesis of squalene, a key cholesterol precursor [26]. So we concluded that both increased DHCR7 and FDFT1 may induce AMD by elevating the expression of cholesterol and formation of drusen.
According to the AMD-specific transcriptional regulatory networks, we identified myogenin was a common mediator of FAP, TNC and GRP, so we concluded that myogenin may be involved in AMD by regulating these target genes. As a member of Rel family, c-rel was reported to be an important mediator of various cytokine stimuli such as TNF-α [17] which suggested that c-rel may involve with the pathological process of AMD.
Conclusions
In our study, eight DEGs (TNC, FAP, GPX3, GRP, ADAMTS5, TRAF6, DHCR7 and FDFT1) were found to involve with the process of AMD by promoting the formation of drusen, regulating the process of CNV, REM and signal transduction pathway or against with oxidative stress. As a common mediator of TNC, FAP and GRP, myogenin may regulate the process of AMD and c-rel may involve with AMD by regulating TNF-α. Our finding could contribute to understanding the mechanism of AMD in molecular levels, providing clues to potential biomarkers and new therapeutic targets for the disease. The limitation of our study was that the number of samples for qRT-PCR confirmation was small. Hence, studies with larger sample size need to be performed to confirm this conclusion.
Abbreviations
- ADAMTS5:
-
ADAM metallopeptidase with thrombospondin type 1 motif 5
- AMD:
-
Age-related macular degeneration
- CNV:
-
choroidal neovascularization
- DEGs:
-
differentially expressed genes
- DHCR7:
-
7-dehydrocholesterol reductase
- FAP:
-
fibroblast activation protein alpha
- FDFT:
-
farnesyl-diphosphate farnesyl transferase 1.
- GEO:
-
Gene Expression Omnibus database
- GO:
-
Gene Ontology
- GPX3:
-
glutathione peroxidase 3
- GRP:
-
gastrin-releasing peptide
- KEGG:
-
Kyoto Encyclopedia of Genes and Genomes
- ME:
-
macular eduma
- RPE:
-
retinal pigment epithelium
- TFs:
-
transcription factors
- TNC:
-
Tenascin-C
- TRAF6:
-
TNF receptor associated factor 6
- VEGF:
-
vascular endothelial growth factor
References
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1419–31.
Bressler NM. Age-related macular degeneration is the leading cause of blindness. Jama J Am Med Asso. 2004;291(15):1900–1.
Hanus J, Anderson C, Wang S. RPE necroptosis in response to oxidative stress and in AMD. Ageing Res Rev. 2015;24:286–98.
Hau VS, London N, Dalton M. The treatment paradigm for the implantable miniature telescope. Ophthalmol Ther. 2016:1–10.
Afshari FT, Kwok JC, Andrews MR, Blits B, Martin KR, Faissner A, et al. Integrin activation or alpha 9 expression allows retinal pigmented epithelial cell adhesion on Bruch's membrane in wet age-related macular degeneration. Brain. 2010;133(Pt 2):448–64.
Lim LS, Mitchell P, Seddon JM, Holz FG, Wong TY. Age-related macular degeneration. Lancet. 2012;379(9827):1728–38.
Cai X, Mcginnis JF. Oxidative stress: the achilles' heel of neurodegenerative diseases of the retina. Front Biosci. 2012;17(5):1976–95.
Augustin AJ, Offermann I. Emerging drugs for age-related macular degeneration. Expert Opin on Emerg Dr. 2006;11(4):725–40.
Lin CH, Li CH, Liao PL, Tse LS, Huang WK, Cheng HW, et al. Silibinin inhibits VEGF secretion and age-related macular degeneration in a hypoxia-dependent manner through the PI-3 kinase/Akt/mTOR pathway. Br J Pharmacol. 2013;168(4):920–31.
Du JY, Yang H, Tian DR, Wang QM, He L. Identification and functional analysis of differentially expressed genes related to obesity using DNA microarray. Genet Mol Res. 2014;13(13):64–72.
Huang YD, Shan W, Zeng L, Wu Y. Screening of differentially expressed genes related to bladder cancer and functional analysis with DNA microarray. Asian Pac J Cancer P. 2013;14(8):4553–7.
Chen Y, Shi JX, Pan XF, Feng J, Zhao H. DNA microarray-based screening of differentially expressed genes related to acute lung injury and functional analysis. Eur Rev Med Pharmacol Sci. 2013;17(8):1044–50.
Hao Y, Weiss GM: Gene Selection from Microarray Data for Age-related Macular Degeneration by Data Mining.
Delcourt C, Cristol JP, Léger CL, Descomps B, Papoz L. Associations of antioxidant enzymes with cataract and age-related macular degeneration. The POLA study. Pathologies Oculaires Liees a l'Age. Ophthalmology. 1999;106(2):215–22.
Shi W, Liu J, Li M, Gao H, Wang T. Expression of MMP, HPSE, and FAP in stroma promoted corneal neovascularization induced by different etiological factors. Curr Eye Res. 2010;35(11):967–77.
Kang JH, Ishola TA, Baregamian N, Mourot JM, Rychahou PG, Evers BM, et al. Bombesin induces angiogenesis and neuroblastoma growth. Cancer Lett. 2007;253(2):273–81.
Bevitt DJ, Mohamed J, Catterall JB, Li Z, Arris CE, Hiscott P, et al. Expression of ADAMTS metalloproteinases in the retinal pigment epithelium derived cell line ARPE-19: transcriptional regulation by TNFalpha. Biochim Biophys Acta. 2003;1626(1–3):83–91.
Ishikawa K, Kannan R, Hinton DR. Molecular mechanisms of subretinal fibrosis in age-related macular degeneration. Exp Eye Res. 2015;142
Wong TY. Age-related macular degeneration: why should stroke physicians care? Stroke. 2010;41(4):575–6.
Bressler SB. Introduction: understanding the role of angiogenesis and Antiangiogenic agents in age-related macular degeneration. Ophthalmology. 2009;116(10 Suppl):S1–7.
Heller JP, Martin KR. Enhancing RPE cell-based therapy outcomes for AMD: the role of Bruch's membrane. Transl Vis Sci Technol. 2014;3(4):11–11.
Emerson MV, Lauer DAK. Emerging therapies for the treatment of Neovascular age-related macular degeneration and diabetic macular edema. BioDrugs. 2007;21(4):245–57.
Vanderbeek BL, Bonaffini SG, Ma L: The Association between Intravitreal Steroids and Post-Injection Endophthalmitis Rates. Ophthalmology 2015, 122(11):2311–2315.e2311.
Geltzer A, Turalba A, Vedula SS. Surgical implantation of steroids with antiangiogenic characteristics for treating neovascular age-related macular degeneration. Cochrane Db Syst Rev. 2013;1 (4):92 –92.
Green WR. Histopathology of age-related macular degeneration. Mol Vis. 1999;5(5):384.
Rudolf M, Curcio CA. Esterified cholesterol is highly localized to Bruch's membrane, as revealed by lipid histochemistry in wholemounts of human choroid. J Histochem Cytochem. 2009;57(8):731–9.
Mares-Perlman JA, Brady WE, Klein R, VandenLangenberg GM, Klein BE, Palta M. Dietary fat and age-related maculopathy. Arch Ophthalmol. 1995;113(6):743–8.
SHSFRACOFRCS MD. DRUSEN and their relationship to senile macular degeneration. Clin Experiment Ophthalmol. 1980;8(2):117–30.
Green WR. Enger C: Age-related macular degeneration histopathologic studies. The 1992 Lorenz E. Zimmerman Lecture. Retina. 1993;100(10):1519–35.
Curcio CA, Presley JB, Millican CL, Medeiros NE. Basal deposits and drusen in eyes with age-related maculopathy: evidence for solid lipid particles. Exp Eye Res. 2005;80(6):761–75.
Tierney E, Conley SK, Goodwin H, Porter FD. Analysis of short-term behavioral effects of dietary cholesterol supplementation in smith-Lemli-Opitz syndrome. Am J Med Genet A. 2010;152A(1):91–5.
Acknowledgements
None.
Funding
Not applicable.
Availability of data and materials
The datasets generated during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
BZ and JX contributed to the conception of the study. BZ, MYW and JX performed the data analyses.ML and YHY contributed the materials and performed the q-RT-PCR. BZ and MYW contributed significantly in writing the manuscript. All authors read and approved the final manuscript
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
All the participants’ informed consents were obtained and the research protocols were approved by the ethical committee of Affiliated hospital of Taishan medical college (No. 2016–056).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1: Table S1.
The top 15 most significantly enriched GO terms in AMD (DOC 120 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zhao, B., Wang, M., Xu, J. et al. Identification of pathogenic genes and upstream regulators in age-related macular degeneration. BMC Ophthalmol 17, 102 (2017). https://doi.org/10.1186/s12886-017-0498-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-017-0498-z