Abstract
Background
Parry-Romberg syndrome (PRS) is a rare disorder characterized by unilateral facial atrophy affecting the skin, subcutaneous tissue, muscles, and sometimes extending to the osteocartilaginous structures. Ocular involvement is relatively rare.
Case presentation
We present a case of a 23-year-old female caucasian patient with Parry Romberg syndrome and extensive ocular involvement: enophthalmos, uveitis, iris atrophy. Ultrasound biomicroscopy (UBM) demonstrated hypotrophy of the ciliary body. The ciliary body atrophy has been previously reported just once and can be an explanation for the hypotony, frequently present in these patients.
Conclusions
Parry Romberg syndrome is a rare multidisciplinary disease. Our case presents a full spectrum of ocular manifestations. The pathogenesis of hypotonia is discussed.
Similar content being viewed by others
Background
Parry-Romberg syndrome (PRS) is a rare disorder characterized by unilateral facial atrophy affecting the skin, subcutaneous tissue, muscles, and sometimes extending to the osteocartilaginous structures [1–4]. Ophthalmic involvement is uncommon with the most frequent finding being enophthalmos [5–11].
We present a case of PRS with enophthalmos, uveitis, ciliary body hypotrophy and phacodonesis.
Case presentation
23 years old lady with 16 years history of Parry Romberg syndrome was referred to our clinic. The family history was positive for autoimmune diseases: her father was affected by rheumatoid arthritis and her first degree aunt by cutaneous psoriasis. No other cases of PRS were reported in the family. She did not report previous trauma, but had a Varicella Zoster virus (VZV) infection when she was 5 years old. When 6 years old, she developed a dermal hyperpigmented lesion in the left side of the neck. One year later she presented signs of left hemifacial atrophy. She progressively developed atrophy of cutaneous and subcutaneous fat tissue with maxillary-mandibular asimmetry and enophthalmos. The nasal septum and the mouth were deviated (Fig. 1). The disease progression stopped when she was 15 years old. She then underwent two autologous fat injections which reabsorbed after a few months. She didn’t undergo further surgical interventions. The disease is presently stable (Fig. 2). She complained migraine, but no other neurological symptoms. Serological tests were positive for anti-streptolysin O titre (369 U/ml; range 0-250 U/ml), rheumatoid factor (101 U/ml; range 0-40 U/ml), antibodies against nucleic (>1:640; range < 1:160) and against double strain DNA (42 U/ml; range < 30 - >50). The rheumatologic examination was negative. TSH was mildly elevated (4.27 UI/ml; range 0.2-4 UI/ml), but T3 and T4 were still in the normal range (T3:3.29 pg/ml; range 2.35-4.55 pg/ml and T4: 13.12 pg/ml; range 6.95-18.20 pg/ml), suggesting a subclinical hypothyroidism.
The ocular involvement started simultaneous to the development of facial atrophy. She first reported intense photofobia and she presented with multiple episodes of left iridocyclitis in the following years. She was diagnosed with Fuchs heterochromic iridocyclitis.
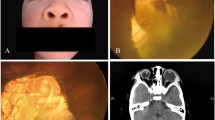
She presented to our Clinic with left enophthalmos and pseudoptosis. Her best corrected visual acuity was 20/20 in the right eye and 20/60 in the left eye. The anterior segment examination showed bilateral non-pigmented endothelial deposits (Fig. 3a and b), but no flare. The left iris was atrophic with partial aniridia, the pupil was non reactive to light (Fig. 4). The anterior chamber depth was reduced in periphery. Gonioscopy showed a narrow angle grade 1‐2 (Shaffer) (Fig. 5a and b) and ultrasound biomicroscopy (UBM) demonstrated a narrow angle at 3,6 and 12 o’clock and a closed angle at 9 o’clock. Unexpectedly during this exam, the ciliary body was atrophic (Fig. 6a,b,c,d). The right eye UBM reported a dystrophic ciliary body (Fig. 6e).
The lens showed phacodonesis. The intraocular pressure (IOP) measured with Goldmann applanation tonometry was 12 mmHg in the right eye and 10 mmHg in the left eye. Fundus examination was normal in both eyes.
Conclusions
Parry-Romberg syndrome (PRS) is a rare disorder characterized by atrophy of cutaneous, subcutaneous fatty tissue, muscle tissue and rarely bone structures. It is more common in women, it usually involves one side of the face, the ipsilateral involvement of the body is rare and 20 % of cases are bilateral [9]. PRS usually begins in the first decade of life [1–3, 12], although some cases with a late onset have been described [12], and is slowly progressive over two to twenty years and then stabilizes [1, 2, 13–16]. Our patient shows a typical onset in childhood and the progression was slow in the following ten years.
PRS etiology in still unknown: traumatic, genetic, immune mediated processes, hormonal disregulation, infection (Herpes and Borrelia burgdorferi mostly involved [17–19]) and sympathetic dysfunction have been proposed. In our case we found an history of familial genetic predisposition to develop autoimmune disease, a serological assessment demonstrated a potential immune and hormonal disregulation, and a positive history of Varicella Zoster Virus infection preceding the PRS.
As referred in literature, an early sign of PRS is a frontal hypo or hyperpigmented skin lesion known as “frontal linear scleroderma en coupe de sabre”, a localised form of sclerodermia. In our case the only sign preceding the developement of the atrophy was a hyperpigmented neck lesion. Frontal linear sclerodermia (LSCS) and PRS have the same starting age, disease progression, ocular and neurological involvement and predominantly affect women. The prevalence of LSCS in conjunction with PRS is uncertain, but has been reported to range from 36.6 % to 53.6 % [20]. For this reason it has been suggested that PRS is a form of scleroderma, although some Authors believe that they are separate entities [20–23].
PRS often coexists with neurological, cardiac, ophtalmological, rheumatological, endocrine, maxillo-facial and orthodontal disorders [7]. Neurological involvement is the most common association [24, 25] including migraine, hemiplegia, brain atrophy, and intracranial vascular anomalies. For this reasons some Authors consider the PRS as a neuro-cutaneous syndrome [24, 25]. In our case migraine was the only neurological symptom presented by the patient.
Several ophthalmologic associations have been previously described, affecting 10-30 % of patients, the most common being enophthalmos, eyelid atrophy, uveitis, retinal vasculitis, oculo-motor defects and glaucoma. Other findings are presented in Table 1.
Our patient had an extensive ophthalmologic involvement: enophthalmos, pseudoptosis, uveitis, iris atrophy and partial aniridia, narrow angle, phacodonesis and ciliary body hypotrophy. Phacodonesis has never been reported before and ciliary body atrophy has recently been reported by Ashwini Kini et al. (2015) [26].
The ciliary body hypotrophy should have led to ocular hypotony, but the IOP was similar in both eyes. The presence of the narrow angle and thus a reduction of outflow may compensate for the decrease of inflow. Alternatively, the ciliary body, although atrophic, might be still functional and its production of acqueous humor sufficient to prevent hypotonia.
Previous Authors reported occurrence of hypotony or glaucoma in patients with the Parry Romberg Syndrome. Hypotony is generally considered as consequent to an edema of the ciliary body due to uveitis [27]. The occurrence of glaucoma has been considered secondary to uveitis or angle closure [28].
Our findings of ciliary body hypotrophy was occasional. We were evaluating the chamber angle with UBM and we came across this novel finding.
UBM examination is in general seldom used in the ophthalmic practice and ciliary hypotrophy might be more frequent than expected in this Syndrome, which affects mesodermic and ectodermic tissues.
We suggest that UBM examination should be further used in anterior segment malformations associated with the Parry Romberg syndrome.
Consent
Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images. A copy of the written consent is available for review by the Editor of this Journal.
Abbreviations
- PRS:
-
Parry-Romberg syndrome
- LSCS:
-
Frontal linear sclerodermia
- IOP:
-
Intraocular pressure
- UBM:
-
Ultrasound biomicroscopy
References
Longo D, Paonessa A, Specchio N, Delfino LN, Claps D, Fusco L, et al. Parry-Romberg syndrome and Rasmussen encephalitis: possible association; clinical and neuroimaging features. J Neuroimaging. 2009;20:1–6.
Duymaz A, Karabekmez FE, Keskin M, Tosun Z. Parry-Romberg syndrome: facial atrophy and its relationship with other regions of the body. Ann Plast Surg. 2009;63:457–61.
Pinheiro TP, Silva CC, Silveira CS, Botelho PC, Pinheiro MG. Progressive hemifacial atrophyecase report. Med Oral Patol Oral Cir Bucal. 2006;11:112–4.
Anderson PJ, Molony D, Haan E, David DJ. Familial Parry‐Romberg disease. Int J Pediatr Otorhinol. 2005;69:705–8.
Leao M, da Silva ML. Progressive hemifacial atrophy with agenesis of the head of the caudate nucleus. J Med Genet. 1994;31:969–71.
Asher SW, Berg BO. Progressive hemifacial atrophy: report of three cases, including one observed over 43 years, and computed tomographic findings. Arch Neurol. 1982;39:44–6.
El KJ, Abbas O, Rubeiz M. A review of Parry Romberg syndrome. J Dermatol. 2012;67:769–84.
Kaya M, Sel Yilmaz C, Kurtaran H, Gunduz M. Chronologic presentation of a severe case of progressive hemifacial atrophy (Parry-Romberg syndrome) with the loss of an eye. Case Rep Otolaryngol. 2014;1-6.
Balan P, Gogineni SB, Shetty SR, D'souza D. Three-dimensional imaging of progressive facial hemiatrophy (Parry-Romberg syndrome) with unusual conjunctival findings. Imaging Sci Dent. 2011;41:183–7.
Stone J. Parry Romberg syndrome. Pract Neurol. 2006;6:185–8.
Rangare AL, Babu SG, Thomas PS, Shett SR. Parry Romberg syndrome: a case report. J Oral Maxillofac Res. 2011;2:e5.
Carreno M, Donaire A, Barcelo MI, Rumia J, Falip M. Parry Romberg syndrome and linear scleroderma in coup de sabre mimicking Rasmussen encephalitis. Neurol. 2007;68:1308–10.
Mendonca J, Viana SL, Freitas F, Lima G. Late-onset progressive facial hemiatrophy (Parry-Romberg syndrome). Postgrad Med. 2005;51:135–6.
Parry CH. Collections from the unpublished medical writings of the late Caleb Hillier Parry. London: Underwoods; 1825. p: 478-480.
Mazzeo N, Fisher JG, Mayer MH, Mathieu GP. Progressive hemifacial atrophy (Parry-Romberg syndrome). Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79:30–5.
Moore MH, Wong KS, Proudman TW, David DJ. Progressive hemifacial atrophy (Romberg’s disease): skeletal involvement and treatment. Br J Plast Surg. 1993;46:39–44.
Sahin MT, Baris S, Karaman A. Parry-Romberg syndrome: a possible association with borreliosis. J Eur Acad Dermatol Venereol. 2004;18:204–7.
Sommer A, Gambichler T, Bachrach-Buhles M, von Rothenburg T, Altmayer P, Kreuter A. Clinical and serological characteristics of progressive facial hemiatrophy: a case of patients. J Dermatol. 2006;54:227–33.
Stern HS, Elliott LF, Beegle Jr PH. Progressive hemifacial atrophy associated with Lyme disease. Plast Reconstr Surg. 1992;90:479–83.
Tollefson MM, Witman PM. En coup de sabre morphea and Parry-Romberg syndrome: a retrospective review of 54 patients. J Dermatol. 2007;56:257–63.
Rogers BO. Progressive facial hemiatrophy: Romberg’s disease, a review of 772 cases. In: Broadbent TR, Anderson B, editors. Transactions of the third international congress of plastic surgery. International congress series 66. Amsterdam: Excerpta Medica; 1963. p. 681–9.
Lehman TJA. The Parry Romberg syndrome of progressive facial hemiatrophy and linear scleroderma en coup de sabre: mistaken diagnosis or overlapping conditions? J Rheumatol. 1992;19:844–5.
Auvinet C, Glacet-Bernard A, Coscas G, Cornelis P, Cadot M, Meyringnac C. Parry‐Romberg progressive facial hemiatrophy and localized scleroderma: nosologic and pathogenic problems [in French]. J Fr Ophtalmol. 1989;12:169–73.
Taylor HM, Robinson R, Cox T. Progressive facial hemiatrophy: MRI appearances. Dev Med Child Neurol. 1997;39:484–6.
Aynaci FM, Sen Y, Erdeol H, Ahmetoglu A, Elmas R. Parry-Romberg syndrome associated with Adie’s pupil and radiologic findings. Ped Neurol. 2001;25:416–8.
Ashwini Kini T, Prakash VS, Puthalath S, Bhandari PL. Progressive hemifacial atrophy with ciliary body atrophy and ocular hypotony. Indian J Ophthalmol. 2015;63:61–3.
Hung S, Rutar T, Lin S, et al. Severe hypotony associated with Parry-Romberg syndrome. Ophthalmic Surg Lasers Imaging Retina. 2010;9:1–3.
Ibarra PC. Parry-Romberg syndrome with glaucoma and pregnancy. Gac Med Mex Vol. 2001;137:289.
Paprocka J, Jamroz E, Adamek D, Marszal E, Mandera M. Difficulties in differentiation of Parry-Romberg syndrome, unilateral facial sclerodermia, and Rasmussen syndrome. Childs Nerv Syst. 2006;22:409–15.
Aracena T, Roca FP, Barragan M. Progressive hemifacial atrophy (Parry‐Romberg syndrome): report of two cases. Ann Ophthalmol. 1979;11:953–8.
Derex L, Isnard H, Revol M. Progressive facial hemiatrophy with multiple benign tumors and hamartomas. Neuroped. 1995;26:306–9.
Bandello F, Rosa N, Ghisolfi F, Sebastiani A. New findings in the Parry-Romberg syndrome: a case report. Eur J Ophthalmol. 2002;12:556–8.
Miller MT, Sloane H, Goldberg MF, Grisolano J, Frenkel M, Mafee MF. Progressive hemifacial atrophy (Parry-Romberg disease). J Pediatr Ophthalmol Strabismus. 1987;24:27–36.
Stone J. Parry-Romberg syndrome: a global survey of 205 patients using the Internet. Neurology. 2003;61:674–6.
Kee C, Hwang JM. Parry-Romberg syndrome presenting with recurrent exotropia and torticollis. J Pediatr Ophthalmol Strabismus. 2008;45:368–70.
Khan AO. Restrictive strabismus in Parry-Romberg syndrome. J Pediatr Ophthalmol Strabismus. 2007;44:51–2.
Ousterhout DK. Correction of enophthalmos in progressive hemifacial atrophy: a case report. Ophtal Plast Reconstr Surg. 1996;12:240–2.
Grayson M, Pieroni D. Progressive facial hemiatrophy with bullous and band-shaped keratopathy. Am J Ophthalmol. 1970;70:42–4.
Galanopoulos A, McNab AA. Hemifacial atrophy: an unusual cause of upper eyelid retraction. Ophtal Plast Reconstr Surg. 1995;11:278–80.
Ford JG, Busbee B, Reed JW, Yu D. Hemifacial atrophy and primary corneal endothelial failure. Arch Ophthalmol. 1998;116:1246–8.
Banks TL, Sugar HS. Ocular manifestations of facial hemiatrophy. J Mt Sinai Hosp N Y. 1963;11:83.
Moloney G, Lehman A, Shojania K, Ross M, McCarthy M. Corneal findings in Parry-Romberg syndrome. Can J Ophthalmol. 2014;49:e2–5.
Preechawat P, Phuchantuk P, Leelawongs K. Ocular abnormalities in Parry-Romberg syndrome. Thai J Ophthalmol. 2011;25:43–8.
Park DH, Kim IT. Patient with Parry-Romberg syndrome complicated by Coats’ syndrome. Jpn J Ophthalmol. 2008;52:520–2.
Ong K, Billson FA, Pathirana DS, Clifton-Bligh P. A case of progressive hemifacial atrophy with uveitis and retinal vasculitis. Aust N Z J Ophthalmol. 1991;19:295–8.
Yildirim O, Dinc E, Oz O. Parry-Romberg syndrome associated with anterior uveitis and retinal vasculitis. Can J Ophthalmol. 2010;45:289–90.
Miller MT, Spencer MA. Progressive hemifacial atrophy: a natural history study. Trans Am Ophthalmol Soc. 1995;93:203–15.
Detilleux JM, Zanen J. Progressive facial hemiatrophy (Parry-Romberg disease) with chorioretinal lesions. Bull Soc Belge Ophtalmol. 1970;156:608–18.
Ehmann D, Riyaz R, Greve M. Central retinal artery occlusion in a child with Parry-Romberg syndrome. Can J Ophthalmol. 2014;49:e9–10.
Acknowledgements
We would like to thank Paolo Fogagnolo for having referred us the patient.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
AMF and FG conceived the study, participated in the design of the study, drafted and revised the manuscript. VA partecipated in the design of the study, drafted the manuscript and carried out the ophthalmologic evaluation. CB, MF and DP carried out parts of the ophthalmologic evaluation and drafted the manuscript. CB revised the english grammatical errors. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Fea, A.M., Aragno, V., Briamonte, C. et al. Parry Romberg syndrome with a wide range of ocular manifestations: a case report. BMC Ophthalmol 15, 119 (2015). https://doi.org/10.1186/s12886-015-0093-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-015-0093-0