Abstract
Objectives
Pan-immune-inflammation value (PIV) is defined by the neutrophil, platelet, monocyte, and lymphocyte counts and is associated with immune-checkpoint inhibitor (ICI) therapy outcomes in advanced non-small cell lung cancer (aNSCLC). However, PIV is dynamic under therapy and its longitudinal assessment may help predict efficacy. This study investigated the impact of baseline PIV and its dynamics on ICI efficacy and its immune-related adverse events (irAEs). The study additionally attempted to understand the biological significance of PIV.
Patients and methods
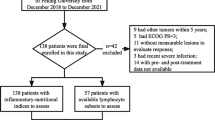
This retrospective study analyzed the clinical data of 269 consecutive patients with aNSCLC. PIV was calculated at baseline and at weeks 3–4 to determine its association with overall survival (OS), progression-free survival (PFS), and irAEs.
Results
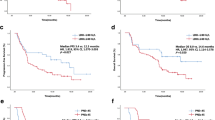
Results revealed that low baseline PIV was positively correlated with the incidence of irAEs. Moreover, a low PIV at baseline was significantly associated with a prolonged PFS (median PFS: 10 vs. 7 months, p = 0.0005) and OS (median OS: 29 vs. 21 months, p < 0.0001). When the PIV at baseline and weeks 3–4 was considered together, its low dynamics correlated with a higher incidence of irAEs (p = 0.001), a longer PFS (median PFS, 9 vs. 6 months, p = 0.012), and a longer OS (median OS; 28 vs. 21 months, p = 0.002).
Conclusion
Thus, PIV at baseline and its dynamics are novel and potent predictors of irAEs, PFS, and OS in patients with aNSCLC receiving immunotherapy. Moreover, the PIV dynamics may be an effective, novel surrogate marker to dynamically observe the efficacy of immunotherapy.
Similar content being viewed by others
Introduction
Lung cancer is the second most commonly occurring tumor and is the leading cause of cancer-related mortality worldwide [1]. Particularly, non-small cell lung cancer (NSCLC) accounts for 85% of all lung cancers [2, 3]. Compared with surgery, radiotherapy, or chemotherapy, immunotherapy has become a hot topic for treating NSCLC owing to the considerable, recent advancements in this therapy. Moreover, it has been shown that patients with advanced NSCLC (aNSCLC) treated with immunotherapy have longer progression-free survival (PFS) and overall survival (OS) than those treated with conventional chemotherapy [4, 5].
Despite its advantages, immunotherapy still is a double-edged sword. Unlike traditional anti-tumor drugs, immunotherapy does not directly kill tumor cells; instead, it regulates the body’s immune function [6]. By changing the inherent relationship between immune and tumor cells, immunotherapy alters the tumor microenvironment (TME) such that immune cells kill cancer cells [7, 8]. However, immunotherapy is associated with a unique set of adverse events, called immune-related adverse events (irAEs) [9,10,11]. These result from treatment-induced over-activation of the immune system, which causes injury to normal tissues, resulting in more serious treatment complications and thus limiting the clinical use of immune-checkpoint inhibitors (ICIs). To add to this dilemma, there is a lack of biomarkers to predict the occurrence and severity of irAEs. Studies have shown that in the process of immunotherapy for non-small cell lung cancer, there is a correlation between the occurrence of irAEs and good survival [12]. Therefore, if alternative biomarkers for predicting irAEs can be found and the advantages and disadvantages of immunotherapy can be weighed before treatment, patients will benefit from it, reducing the occurrence of immune adverse events and get the possibility of personalized immunotherapy. Thus, more studies are required to identify factors associated with irAEs.
It is well known that inflammation impacts every step of tumorigenesis, from initiation and tumor promotion to metastatic progression. Reportedly, liquid biopsy is a promising tool for identifying predictive biomarkers for immunotherapy [13]. According to previous studies, peripheral blood parameters may efficiently predict responses to ICIs in multiple malignancies. Particularly, inflammation-related markers, such as the systemic inflammation immune index (SII) [14], neutrophil-to-lymphocyte ratio (NLR) [15], platelet-to-lymphocyte ratio (PLR), monocyte-to-lymphocyte ratio (MLR) [16], and derived NLR (dNLR) [17] can all be used as potential markers of tumor response to ICIs.
Recently, the dynamics of biomarkers have been studied to some extent for determining the prognosis of cancer treatments [18,19,20,21]. In the context of immunotherapy for NSCLC, several factors have been reported for monitoring efficacy and predicting clinical prognosis; these factors include multiple mechanisms, including dynamic immune TME profiles [22], PD-L1 expression [23], radiomics [24], tumor mutation burden, and immunoinflammatory indicators [25, 26]. Therefore, unlike in the past, when pathological biopsy of primary tumor or blood tests were performed before treatment, studying the dynamics of peripheral blood biomarkers is worthy of recognition and further investigation in the prognostic assessment of immunotherapy for NSCLC.
More recently, a new comprehensive marker called the pan-immune-inflammatory value (PIV) [27], which incorporates neutrophil, platelet, monocyte, and lymphocyte counts, showed a strong association with PFS and OS. Moreover, PIV was found to outperform other well-established immune biomarkers, such as NLR and PLR, in predicting patient outcomes [28]. In addition, a study has validated the role of PIV dynamics for disease monitoring in patients with metastatic colorectal cancer [29]. Therefore, the present study aimed to assess the predictive value of PIV and its dynamics in patients with aNSCLC.
Patients and methods
Patients
The study retrospectively enrolled patients with aNSCLC who were consecutively treated at the Affiliated Hospital of Nantong University, China, between January 2019 and December 2022. All patients had undergone immunotherapy with nivolumab 3 mg/kg every 2 weeks or pembrolizumab 200 mg every 3 weeks until unacceptable toxicity, or death from any cause. Patients who only received other antitumor therapies, such as chemotherapy, targeted therapy, or radiotherapy, were excluded from the study. Only patients with a minimum follow-up of 12 months (until December 2022) were enrolled, owing to the high probability of developing irAEs within the 1– 6 months of immunotherapy [30] and the need for sufficient time for survival assessment.
Data collection
Data on the following patients’ characteristics were extracted: age, sex, smoking history, histology, cancer stage, and the number of metastatic sites. In addition, laboratory data such as complete blood cell counts (e.g., neutrophils, lymphocytes, monocytes, and platelets) at baseline (within 7 days before the administration of immunotherapy, defined as T1) and at the endpoint (3–4 weeks after the first dose, defined as T2) were extracted from the electronic medical records. PIV was calculated as (neutrophil count × platelet count × monocyte count)/lymphocyte count. SII was calculated as (neutrophil count × platelet count)/lymphocyte count. NLR was calculated as neutrophil count /lymphocyte, and PLR was calculated as platelet count/lymphocyte count. MLR was calculated as monocyte count/lymphocyte count and d-NLR as neutrophil count/(leucocytes count – neutrophil count). The cutoff values for PIV, SII, NLR, PLR, MLR, and d-NLR at baseline as dichotomous variables were intercepted according to the receiver-operating characteristic curve (PIV < 288.1; SII < 784.1; NLR < 3.163; PLR < 0.420; dNLR < 2.316). The dynamic change in PIV was calculated by subtracting PIV (T1) from the absolute PIV (T2). The cutoff values for the dynamic changes in PIV as dichotomous variables were determined using the X-title software (PIV dynamics < 608.2). PFS was determined as the duration from the date of treatment initiation to the date of disease progression or patient death from any cause. OS was defined as the duration from the date of treatment initiation to the date of death from any cause. Tumor responses were assessed using the Response Evaluation Criteria in Solid Tumors guidelines (version 1.1) every 10 ± 2 weeks. This study was approved by the board/ethics committee of the Affiliated Hospital of Nantong University, and exception to the requirement of informed consent was approved (Ethic Number: 2018-K020).
Statistical analysis
Variability was compared using Fisher’s exact test for categorical variables and Mann-Whitney or Wilcoxon signed-rank tests for continuous variables. Box charts and line charts were used to illustrate the differences and trends between the two important time points of PIV. The association between blood biomarkers and the onset of irAEs was analyzed by logistic regression models. For data with binary data as the outcome variable, the cut-off value of the continuous independent variable is generally determined by ROC analysis. For dichotomous outcome variables with temporal dimensions, we use X-title to determine the cut-off value [31]. Cox regression models were used to determine the risk factors for PFS and OS. Moreover, PFS and OS were estimated using the Kaplan-Meier method and were compared using the log-rank test. Statistical significance was defined as a two-sided p-value of < 0.05. All statistical analyses were performed using X-tile versions 3.6.1, SPSS 20.0 (SPSS Inc., Chicago, IL) and GraphPad Prism version 9.2.0 (GraphPad Inc., San Diego, CA).
Results
Clinical characteristics
The clinical characteristics of 269 patients are outlined in Table 1. The median age of patients was 67 (41–87) years, with 232 (86.2%) patients being male. The most common histological type of NSCLC was adenocarcinoma (n = 164; 61.0%), followed by squamous carcinoma (n = 104; 38.6%) and a rare type of sarcoma (n = 1; 0.4%). Of all patients, 18 (6.7%) had an Eastern Cooperative Oncology Group performance status of 2. Overall, 215 (55.2%) patients had undergone testing for tumor PD-L1 expression; of these, 147 (68.4%) and 68 (31.6%) patients tested positive and negative for PD-L1, respectively. The median number of times patients underwent treatment at baseline was five, with 168 (62.5%) patients being treated with pembrolizumab and 101 (37.5%) with nivolumab. For blood biomarkers, the median PIV was 387 (17.8–9420), NLR was 3.37 (0.844–79.7), PLR was 164 (36.4–1490), SII was 682 (142.0–17300.0), PLR was 164 (36.4–1490), and dNLR was 2.07 (-1.34–31.4).
Summary of irAEs
In total, 89 (33%) patients reported irAEs (Table 2), with the most common being hyperthyroidism/hypothyroidism (19.7%), skin-related events (17.4%), liver injury (15.1%), and enteritis/diarrhea (15.1%). Among organ-related toxicities, dermatological and endocrine toxicities were the most commonly reported irAEs, followed by hepatologic and digestive disorders. A total of 89 events of all-grade irAEs were documented, of which 12 were grade ≥ 3 in severity. The most common grade ≥ 3 irAEs were rash and adrenal insufficiency. The grade ≥ 4 irAEs included myocarditis and complex infections because of hypoimmunity. However, very few grade ≥ 4 events were observed; but these may be resulted in death. The majority of patients with grade ≥ 3 irAEs were treated with steroids, and for a few patients with higher grade irAEs, immunotherapy was discontinued permanently. All patients who received immunosuppressive therapies achieved alleviation of their irAEs.
Univariate and multivariate analyses of risk factors for irAEs
Findings regarding the association of irAE onset with baseline clinical features and with blood parameters are listed in Table 3. None of the baseline clinical features affected the overall risk of irAEs. For example, an increased number of treatment cycles was not significantly associated with a higher probability of developing irAEs (odds ratio [OR]: 0.969; 95% confidence interval [CI]: 0.917–1.024; p = 0.262). Moreover, no association was noted between PD-L1 expression and irAE onset (OR: 0.787; 95% CI: 0.406–1.524; p = 0.477). However, the following blood markers showed a significant correlation with the occurrence of irAEs: L-PIV (OR: 0.112; 95% CI: 0.062–0.202; p < 0.001), L-SII (OR: 0.129; 95% CI: 0.067–0.250; p < 0.001), L-NLR (OR, 0.294; 95% CI, 0.171–0.504; p < 0.001), L-PLR (OR: 0.164; 95% CI: 0.092–0.293; p < 0.001), L-MLR (OR: 0.229; 95% CI: 0.129–0.407; p < 0.001), and L-dNLR (OR: 0.299; 95% CI: 0.165–0.541; p < 0.001). Finally, multivariate analysis confirmed that L-PIV (OR: 0.235; 95% CI: 0.117–0.472; p < 0.001; Table 3), L-SII (OR: 0.393; 95% CI: 0.175–0.883; p = 0.024), and L-PLR (OR: 0.483; 95% CI: 1.055–4.500; p = 0.035) were the independent predictors of irAEs.
In addition, determining collinearity using the variance inflation factor (PIV: 1.976; SII: 2.511; NLR: 2.777; PLR: 1.571; MLR: 1.691; dNLR: 2.391) revealed the absence of multicollinearity for blood biomarkers (Table 3).
Impact of peripheral blood parameters on PFS and OS
Specific variables identified as by univariate analysis included the number of treatments with ICIs, PIV, SII, NLR, PLR, MLR, and dNLR (p < 0.05; Table 4). These variables were further analyzed using the multivariate model. Finally, only the number of treatments with ICIs (HR = 0.950, 95% Cl: 0.920–0.982, p = 0.002) and higher PIV (HR = 1.707, 95% Cl: 1.275–2.286, p < 0.001) were the independent prognostic factors for poor median PFS (Table 4).
A total of 196 tumor progression events were observed in 1 year of follow-up, with the median PFS being 7 months. The tumor progression events rate was 72.9%, with the median PFS being significantly longer in patients with low PIV (10 months, 95% CI: 8.6–11.4; Fig. 1A).
Univariate analysis demonstrated that stage, number of metastatic sites, PIV, SII, NLR, PLR, MLR, and dNLR were associated with OS (p < 0.05, Table 4). However, in multivariate analysis, only low PIV (HR = 2.414, 95% Cl: 1.509–3.862, p < 0.0001) and the number of metastatic sites (< 3, HR = 0.602, 95% Cl: 0.375–0.966, p = 0.035) were independently associated with longer survival outcomes (Table 4).
A total of 88 deaths occurred during the follow-up period, with the OS rate being 67.3%. The median OS for patients with low PIV was 29 months compared with 21 months in patients with high PIV (95% CI: 19.4–22.5, p < 0.0001; Fig. 1B).
PIV dynamics
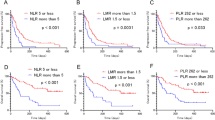
A box plot plotted for comparing irAEs patients with PIV at T1 and T2 revealed a mean of 191.6 vs. 219.4 and an interquartile range (IQR) of 176.9 vs. 539.7. Moreover, the box plot suggested a significant difference in the association of PIV with irAEs between T1 and T2 (Fig. 2A, p = 0.006). For patients with no irAEs, the median of the box plot at T1 and T2 was 527.5 and 409.5, with the IQR being 620.8 and 727.9, respectively; however, these values did not significantly differ between the two time points (p = 0.056; Fig. 2B). In addition, PIV dynamics were compared between patients with irAEs and without irAEs using box plot analysis. The median obtained for patients with irAEs and without irAEs was 190.0 and 317.0, with an IQR of 447.6 and 550.3, respectively. This indicated a significant difference in PIV dynamics between the two groups (p = 0.001; Fig. 2C). The line chart (Fig. 2D) shows the changes in PIV with follow-up. The average change in PIV in patients with irAEs was 350 (Fig. 2D) and in those without irAEs was 678 (Fig. 2E). PIV dynamics were significantly lower in patients with irAEs than in those without irAEs.
PIV dynamic changes during the immunotherapy.(A) Comparison of PIV at baseline and week 3–4 from irAEs patients. (B) Comparison of PIV at baseline and week 3–4 from no irAEs patients. (C) Comparison of PIV dynamics between the irAEs and no irAEs patients. (D) PIV dynamics during baseline and week 3–4 in irAEs patients. (1 data point is outside the axis limits) (E) PIV dynamics during baseline and week 3–4 in no irAEs patients. (13 data points are outside the axis limits)
The median PFS was longer for patients with a smaller PIV change (9 months; 95% CI: 7.9–10.0) than for patients with a greater PIV change (6 months; 95% CI: 4.8–7.1; log-rank test p = 0.0119; Fig. 1C). Likewise, median OS was significantly longer for patients with a smaller PIV change (28 months; 95% CI: 24.3–31.8) than for patients with a greater PIV change (21.6 months; 95% CI: 18.6–23.3; log-rank test p = 0.0021; Fig. 1D).
Discussion
As a newly emerging biomarker, PIV integrates neutrophil, platelet, monocyte, and lymphocyte counts, thus reflecting the systemic and intratumoral inflammatory/ immune system status. The present retrospective study suggested that among the assessed hematological markers, only low PIV was an independent and significant factor affecting the occurrence of irAEs. Moreover, low PIV at baseline was the only independent prognostic factor of both PFS and OS, and the change in PIV dynamic before and after treatment was directly associated with the occurrence of irAEs and with clinical prognosis.
The underlying mechanisms and rationale of each peripheral blood marker are different. NLR is composed of neutrophil-to-lymphocyte ratio, PLR is composed of platelet-to-lymphocyte ratio, MLR is composed of monocyte-to-lymphocyte ratio, and SII is a comprehensive marker calculated from the three indicators of neutrophils, lymphocytes, and platelets. However, the dNLR is composed of leukocytes and neutrophilsIn. In addition, platelets play an important role in hemostasis and thrombosis; however, tumor cells may bind to platelets to escape from the immune system [32, 33]. Moreover, activated platelets release a variety of factors that promote tumor development and invasion [34]. Similar to platelets, monocytes are closely related to the occurrence and development of cancer. Studies have shown that peripheral blood monocytes can indirectly interact with tumor-associated macrophages in the TME [35], and M2 macrophages can promote the growth of tumor cells [36]. Similarly, neutrophils play a role in tumor progression by releasing reactive oxygen species and secreting pro-tumor cytokines, which induce angiogenesis, invasion, and immunosuppression [37, 38]. In contrast, lymphocytes suppress tumorigenesis, and CD8 + and CD4 + T cells in the TME mediate antitumor effects [39]. Neutrophils, platelets, and monocytes all show cancer-related inflammatory responses of patients, while lymphocytes represent the immunomodulatory status of patients in cancer treatment. Overall, in addition to dNLR, which is the main specific parameter of inflammatory response [40], the other four types of peripheral blood biomarkers are indicators of the balance between immunity and inflammation, and have certain clinical value in immunotherapy of patients with NSCLC.
The difference between the four types of indicators mentioned above is that PIV integrates neutrophils, monocytes, platelets and lymphocytes, covering as many peripheral blood parameters as possible. In theory, PIV is a more objective indicator of the complex immune and inflammatory status of the body compared with individual systemic inflammatory indicators such as SII and PLR. As PIV represents all these parameters, it is an external manifestation of a state that reflects the balance between pro-tumor and anti-tumor factors in the TME.
Notably, a previous study has shown that PIV is associated with irAEs in patients with gastrointestinal tumors; however, this role of PIV has not been discussed in patients with NSCLC. In line with this, the present study found that many blood biomarkers were correlated with the occurrence of irAEs, with PIV exhibiting a significant correlation. Unfortunately, other clinicopathological characteristics of patients, such as age, sex, and pathological subtype, were not correlated with the incidence of irAEs. Moreover, a low PIV indicated a greater anti-tumor activity. This implies that immune supplementation using ICIs would ultimately lead to increased incidence of irAEs.
The use of PIV as a predictor of cancer prognosis has been previously investigated and confirmed in a few studies [41, 42]. The present retrospective analysis supports the value of PIV in survival analysis. In addition, the Cox multifactorial analysis further confirmed that PIV is the only independent factor affecting PFS and OS. This is because PIV may capture the complexity of the immune environment and its many components more comprehensively than individual blood cell parameters or other combined statistics. Thus, a low PIV at baseline implies stronger immunity prior to treatment, which reflects the suppression of tumor growth and invasion, ultimately prolonging survival.
In fact, there have been many studies demonstrating the prognostic value of blood biomarker kinetic studies in immunotherapy [43, 44]. When patients with non-small cell lung cancer receive immunotherapy for the first time, the immune and inflammatory reactions of the body are the most intense. And the occurrence of irAEs often occurs in the process of early immunotherapy. Therefore, evaluating the immune and inflammatory response in vivo by analyzing the changes in peripheral blood parameters of patients before and after the first immunotherapy is an important indicator to determine whether patients are suitable for immunosuppressants. However, the focus of this study is not limited to pre-treatment baseline PIV. It is necessary and valuable to assess the dynamic changes in PIV, owing to its correlation with irAEs and clinical prognosis in patients with NSCLC. Cancer is a progressive disease, and baseline PIV can only describe the inflammatory/immune status of a patient over a particular time point. Our results further demonstrate that a smaller PIV change is significantly associated with the incidence of irAEs, and these patients with smaller PIV change have longer PIV and OS. Therefore, a kinetic study of PIV may reflect the variation in the inflammatory/immune system status during the short-term treatment, which theoretically provides a better picture of disease progression and treatment status. Hence, PIV kinetic studies can be used for predicting clinical survival, real-time monitoring of immunotherapy efficacy, and dynamic monitoring of TME homeostasis.
However, our study has a few limitations. This was a retrospective study and lacked prospective validation. In addition, the follow-up period was short (median follow-up: 17 months). And many clinical indicators will still affect the results, such as concomitant diseases, complications, and even the process of processing clinical specimens may affect the serum concentration of each indicator. Therefore, in this study, we tried to strictly standardize the inclusion of the population and the course of treatment as much as possible, and exclude the relevant bias as much as possible. At the same time, from a methodological point of view, we analyzed scientifically and comprehensively, and tried not to lose any valuable indicators. Even a single baseline indicator may have errors, we tried to analyze PIV from the perspective of dynamics, intercepting the test indicators at two time points before and after treatment, analyzing the changes in immunological and inflammatory values before and after treatment, so as to assess the efficacy, and exclude the possibility of data error or bias as much as possible.
This study successfully validated the role of PIV in predicting irAEs and determining clinical prognosis in patients with NSCLC receiving immunotherapy. Finally, the PIV dynamic evaluation time needs to be extended, and PIV needs to be assessed at multiple time points. This will better reflect the balance between the pro-tumor and anti-tumor factors in TME. In conclusion, the use of PIV as a blood biomarker for clinical regression and prognostic assessment in immunotherapy-treated patients with NSCLC should be further explored in prospective clinical trials with larger sample sizes and longer follow-up periods. In fact, there have been many studies combining blood biomarkers as clinical factors with other markers, such as radiomics, proteogenomics, etc. [45], and even creating reliable nomograms for the prediction of clinical immunotherapy and risk stratification [46]. Therefore, from our point of view as clinicians, our future work is to try to incorporate more clinical data, conduct multi-omics joint studies, and establish reliable predictive models for clinical decision-making with the help of PIV and PIV kinetics.
Conclusion
In patients with NSCLC, PIV at the baseline and its dynamics can be used as early, surrogate markers to monitor immunotherapy efficacy, determine irAEs, and predict survival. The clinical application of dynamic changes in immunoinflammatory markers merits further investigation.
Data Availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Parkin DM, Pisani P, Ferlay J. Global cancer statistics. Ca-cancer j clin. 1999;49(1):33–64.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. Ca-cancer j clin. 2021;71(3):209–49.
Duma N, Santana-Davila R, Molina JR. Non-Small Cell Lung Cancer: Epidemiology, Screening, diagnosis, and treatment. Mayo clin proc. 2019;94(8):1623–40.
Liao D, Yu L, Shangguan D, Zhang Y, Xiao B, Liu N, Yang N. Recent advancements of Monotherapy, Combination, and Sequential Treatment of EGFR/ALK-TKIs and ICIs in Non-Small Cell Lung Cancer. Front Pharmacol. 2022;13(null):905947.
Majem M, Cobo M, Isla D, Marquez-Medina D, Rodriguez-Abreu D, Casal-Rubio J, Bueno TM, Bernabé-Caro R, Parente DP, Ruiz-Gracia P, et al. PD-(L)1 inhibitors as Monotherapy for the First-Line treatment of Non-Small-Cell Lung Cancer patients with high PD-L1 expression: a Network Meta-Analysis. J Clin Med. 2021;10(7):null.
Pulendran B, Davis MM. The science and medicine of human immunology. Science. 2020;369(6511):null.
Sadeghirad H, Bahrami T, Layeghi SM, Yousefi H, Rezaei M, Hosseini-Fard SR, Radfar P, Warkiani ME, O’Byrne K, Kulasinghe A. Immunotherapeutic targets in non-small cell lung cancer. Immunology. 2023;168(2):256–72.
Genova C, Dellepiane C, Carrega P, Sommariva S, Ferlazzo G, Pronzato P, Gangemi R, Filaci G, Coco S, Croce M. Therapeutic implications of Tumor Microenvironment in Lung Cancer: Focus on Immune Checkpoint Blockade. Front Immunol. 2021;12(null):799455.
Khan S, Gerber DE. Autoimmunity, checkpoint inhibitor therapy and immune-related adverse events: a review. Sem Cancer Biol. 2020;64(null):93–101.
Morad G, Helmink BA, Sharma P, Wargo JA. Hallmarks of response, resistance, and toxicity to immune checkpoint blockade. Cell. 2022;185(3):576.
Wang Y, Zhou S, Yang F, Qi X, Wang X, Guan X, Shen C, Duma N, Vera Aguilera J, Chintakuntlawar A, et al. Treatment-related adverse events of PD-1 and PD-L1 inhibitors in clinical trials: a systematic review and Meta-analysis. Jama Oncol. 2019;5(7):1008–19.
Rizwan S, Alhamad K, Abel S, Bakalov V, Rodriguez R, Sethi A, Khan T, Attah A, Yasir M, Shankar K, et al. Impact of immune-related adverse events on survival in patients with advanced non-small cell lung cancer treated with immune checkpoint inhibitors: a real-world perspective. J Clin Oncol. 2021;39(15suppl):e21213–3.
Malapelle U, Pisapia P, Addeo A, Arrieta O, Bellosillo B, Cardona AF, Cristofanilli M, De Miguel-Perez D, Denninghoff V, Durán I, et al. Liquid biopsy from research to clinical practice: focus on non-small cell lung cancer. Expert rev mol Diagn. 2021;21(11):1165–78.
Palmer J, Cao Y, Ibrahim S, Dhawan N, Afzal M, Shirai K. Baseline systemic inflammatory immune index may predict overall survival and progression-free survival in patients with non-small cell lung cancer patients on immune checkpoint inhibitors. J Clin Oncol. 2021;39(15suppl):e21202–2.
Randall M, Basu S, Kollipara R, Batus M, Bonomi P, Moudgalya H, Borgia J, Fidler M. Associations between longitudinal pretreatment BMI and neutrophil/lymphocyte ratio(NLR) and progression-free(PFS) and overall survival(OS) in advanced NSCLC patients treated with single agent anti-PD-1/anti-PDL1 monoclonal antibodies(mAbs). J Clin Oncol. 2021;39(15suppl):e21189–9.
Basher F, Saravia D, Lopes G. Prognostic value of systemic inflammatory markers in first- and subsequent-line immunotherapy and durability of response in NSCLC. J Clin Oncol. 2021;39(15suppl):e21210–0.
Dennehy C, McMahon E, Power D, O’Reilly S, Collins D, O’Mahony D, Horgan A, O’Connor M, Jordan E, Calvert P, et al. Clinical haematological biomarkers: derived neutrophil-to-lymphocyte ratio (dNLR), platelet-to-lymphocyte ratio (PLR), and prognostic nutritional index (PNI) and their relationship to survival outcomes in non small cell lung cancer (NSCLC) treated with immunotherapy: a multicenter review. J Clin Oncol. 2019;37(15suppl):e20704–4.
Clarke R, Lucas M, Ryan N, Walsh S, Mahon S, Kelly C. Neutrophil-lymphocyte ratio and prediction of pathological complete response to neoadjuvant treatment in breast cancer. J Clin Oncol. 2022;40(16suppl):e12627–7.
Russo A, Franchina T, Ricciardi G, Battaglia A, Schifano S, Schifilliti M, Scimone A, Toscano G, Zanghì M, Adamo V. Dynamic changes of neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and lactate dehydrogenase (LDH) during treatment with immune checkpoint inhibitors (ICIs) in non-small cell lung cancer (NSCLC). J Clin Oncol. 2019;37(15suppl):2596–6.
Yuan Z, Baker K, Redman MW, Wang L, Adams SV, Yu M, Dickinson B, Makar K, Ulrich N, Böhm J, et al. Dynamic plasma microRNAs are biomarkers for prognosis and early detection of recurrence in colorectal cancer. Brit j cancer. 2017;117(8):1202–10.
Rodriguez-Pascual J, Cubillo A. Dynamic biomarkers of response to Antiangiogenic Therapies in Colorectal Cancer: a review. Curr Pharmacogenomics Person Med. 2017;15(2):81–5.
Lin A, Wei T, Meng H, Luo P, Zhang J. Role of the dynamic tumor microenvironment in controversies regarding immune checkpoint inhibitors for the treatment of non-small cell lung cancer (NSCLC) with EGFR mutations. Mol Cancer. 2019;18(1):139.
Yang Q, Chen M, Gu J, Niu K, Zhao X, Zheng L, Xu Z, Yu Y, Li F, Meng L, et al. Novel biomarkers of dynamic blood PD-L1 expression for Immune checkpoint inhibitors in Advanced Non-Small-Cell Lung Cancer Patients. Front Immunol. 2021;12(null):665133.
Yang DM, Palma DA, Kwan K, Louie AV, Malthaner R, Fortin D, Rodrigues GB, Yaremko BP, Laba J, Gaede S, et al. Predicting pathological complete response (pCR) after stereotactic ablative radiation therapy (SABR) of lung cancer using quantitative dynamic [18F]FDG PET and CT perfusion: a prospective exploratory clinical study. Radiation Oncol (London England). 2021;16(1):11.
Micaela R, Lucas C, Franco C, Federico C, Agustín D, David S. Dynamic perioperative variation of neutrophil-to-lymphocyte ratio as an independent prognosis factor following lobectomy for NSCLC. Updates surg. 2021;73(4):1567–74.
Rosner S, Forde P, Naidoo J, Marrone K, Reuss J, Feliciano J, Levy B, Hann C, Velculescu V, Brahmer J, et al. Early shifts in immune cell subsets to predict response to immune checkpoint blockade in non-small cell lung cancer (NSCLC). J Clin Oncol. 2019;37(8suppl):105–5.
Fucà G, Guarini V, Antoniotti C, Morano F, Moretto R, Corallo S, Marmorino F, Lonardi S, Rimassa L, Sartore-Bianchi A, et al. The Pan-Immune-Inflammation Value is a new prognostic biomarker in metastatic colorectal cancer: results from a pooled-analysis of the Valentino and TRIBE first-line trials. Brit j cancer. 2020;123(3):403–9.
Guven DC, Sahin TK, Erul E, Kilickap S, Gambichler T, Aksoy S. The Association between the Pan-Immune-Inflammation Value and Cancer Prognosis: a systematic review and Meta-analysis. Cancers (Basel). 2022;14(11):null.
Pérez-Martelo M, González-García A, Vidal-Ínsua Y, Blanco-Freire C, Brozos-Vázquez EM, Abdulkader-Nallib I, Álvarez-Fernández J, Lázare-Iglesias H, García-Martínez C, Betancor YZ, et al. Clinical significance of baseline Pan-Immune-Inflammation Value and its dynamics in metastatic colorectal cancer patients under first-line chemotherapy. Sci Rep. 2022;12(1):6893.
Eigentler TK, Hassel JC, Berking C, Aberle J, Bachmann O, Grünwald V, Kähler KC, Loquai C, Reinmuth N, Steins M, et al. Diagnosis, monitoring and management of immune-related adverse drug reactions of anti-PD-1 antibody therapy. Cancer Treat rev. 2016;45(null):7–18.
Camp RL, Dolled-Filhart M, Rimm DL. X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin cancer res. 2004;10(21):7252–9.
Bambace NM, Holmes CE. The platelet contribution to cancer progression. J Thromb Haemost. 2011;9(2):237–49.
Stone RL, Nick AM, McNeish IA, Balkwill F, Han HD, Bottsford-Miller J, Rupairmoole R, Armaiz-Pena GN, Pecot CV, Coward J, et al. Paraneoplastic thrombocytosis in ovarian cancer. N Engl J Med. 2012;366(7):610–8.
Sharma D, Brummel-Ziedins KE, Bouchard BA, Holmes CE. Platelets in tumor progression: a host factor that offers multiple potential targets in the treatment of cancer. J Cell Physiol. 2014;229(8):1005–15.
Petty AJ, Yang Y. Tumor-associated macrophages: implications in cancer immunotherapy. Immunotherapy. 2017;9(3):289–302.
Liu J, Geng X, Hou J, Wu G. New insights into M1/M2 macrophages: key modulators in cancer progression. Cancer Cell Int. 2021;21(1):389.
Dumitru CA, Lang S, Brandau S. Modulation of neutrophil granulocytes in the tumor microenvironment: mechanisms and consequences for tumor progression. Sem Cancer Biol. 2013;23(3):141–8.
Eruslanov EB. Phenotype and function of tumor-associated neutrophils and their subsets in early-stage human lung cancer. Cancer Immunol Immunotherapy. 2017;66(8):997–1006.
Kagamu H, Kitano S, Yamaguchi O, Yoshimura K, Horimoto K, Kitazawa M, Fukui K, Shiono A, Mouri A, Nishihara F, et al. CD4 + T-cell immunity in the peripheral blood correlates with response to Anti-PD-1 therapy. Cancer Immunol Res. 2020;8(3):334–44.
Yang T, Hao L, Yang X, Luo C, Wang G, Lin Cai C, Qi S, Li Z. Prognostic value of derived neutrophil-to-lymphocyte ratio (dNLR) in patients with non-small cell lung cancer receiving immune checkpoint inhibitors: a meta-analysis. BMJ Open. 2021;11(9):e049123.
Corti F, Lonardi S, Intini R, Salati M, Fenocchio E, Belli C, Borelli B, Brambilla M, Prete AA, Quarà V, et al. The Pan-Immune-Inflammation Value in microsatellite instability-high metastatic colorectal cancer patients treated with immune checkpoint inhibitors. Eur j cancer. 2021;150(null):155–67.
Zeng R, Liu F, Fang C, Yang J, Luo L, Yue P, Gao B, Dong Y, Xiang Y. PIV and PILE Score at Baseline Predict Clinical Outcome of Anti-PD-1/PD-L1 Inhibitor Combined With Chemotherapy in Extensive-Stage Small Cell Lung Cancer Patients. Front Immunol 2021, 12(null):724443.
Mezquita L, Preeshagul I, Auclin E, Saravia D, Hendriks L, Rizvi H, Park W, Nadal E, Martin-Romano P, Ruffinelli JC, et al. Predicting immunotherapy outcomes under therapy in patients with advanced NSCLC using dNLR and its early dynamics. Eur j cancer. 2021;151(null):211–20.
Chen Y, Wen S, Xia J, Du X, Wu Y, Pan B, Zhu W, Shen B. Association of dynamic changes in peripheral blood indexes with response to PD-1 inhibitor-based combination therapy and survival among patients with Advanced Non-Small Cell Lung Cancer. Front Immunol. 2021;12(null):672271.
Farina B, Guerra ADR, Bermejo-Peláez D, Miras CP, Peral AA, Madueño GG, Jaime JC, Vilalta-Lacarra A, Pérez JR, Muñoz-Barrutia A, et al. Integration of longitudinal deep-radiomics and clinical data improves the prediction of durable benefits to anti-PD-1/PD-L1 immunotherapy in advanced NSCLC patients. J Transl Med. 2023;21(1):174.
Wang L, Dong T, Xin B, Xu C, Guo M, Zhang H, Feng D, Wang X, Yu J. Integrative nomogram of CT imaging, clinical, and hematological features for survival prediction of patients with locally advanced non-small cell lung cancer. Eur Radiol. 2019;29(6):2958–67.
Acknowledgements
Not applicable.
Funding
This study was supported by National Natural Science Foundation of China (No. 82273955, 82204504); Scientific research project of Jiangsu Provincial Health Commission (No. M2022080); Nantong Science and technology project (No. MS22021025, MS22022025); Multicenter Study Project of Affiliated Hospital of Nantong University (No. LCYJ-A10).
Author information
Authors and Affiliations
Contributions
YQC, LYG, PYG, YWH, YFS, SSN, XYZ and ZYT contributed to the study conception and design. Data collection and statistical analysis were performed by YQC, YWH and PYG. The first draft of the manuscript was written by YQC and LYG. Funding was obtained by SSN, XYZ and ZYT and they supervised the manuscript. YFS helped in the process of revising the article. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All the procedures followed were in accordance with the ethical guidelines of the Helsinki Declaration. This retrospective study was approved by the Affiliated Hospital of Nantong University Institutional Review Board, and exception to the requirement of informed consent was approved (Affiliated Hospital of Nantong University Institutional Review Board No.2018-K020).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, Y., Gong, L., Gu, P. et al. Pan-immune-inflammation and its dynamics: predictors of survival and immune-related adverse events in patients with advanced NSCLC receiving immunotherapy. BMC Cancer 23, 944 (2023). https://doi.org/10.1186/s12885-023-11366-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-11366-4