Abstract
Background
The COVID-19 pandemic was managed in Aotearoa New Zealand (NZ) by a COVID-19 elimination policy, involving border closure and an initial national lockdown. This was different to most other countries including Northern Ireland (NI) and the Netherlands (NED). We quantify the effect of these policies on the diagnosis of three major cancers, comparing NZ with these two European countries.
Method
Data from NED, NZ and NI population-based cancer registries were used to assess trends in all pathologically diagnosed (PD) lung, breast, and colorectal cancers from March to December 2020 (pandemic period) and compared to the similar pre-pandemic period (2017–2019). Trend data were also collated on COVID-19 cases and deaths per 100,000 in each population.
Results
Comparing the pre-pandemic period to the pandemic period there were statistically significant reductions in numbers of lung (↓23%) and colorectal (↓15%) PD cancers in NI and numbers of breast (↓18%) and colorectal cancer (↓18.5%) diagnosed in the NED. In NZ there was no significant change in the number of lung (↑10%) or breast cancers (↑0.2%) but a statistically significant increase in numbers of colorectal cancer diagnosed (↑5%).
Conclusion
The impact of COVID-19 on cancer services was mitigated in NZ as services continued as usual reflecting minimal healthcare disruption and protected cancer services linked with the elimination approach adopted. The reduction in PD cases diagnosed in NED and NI were linked with higher COVID-19 rates and reflect societal restrictions which resulted in delayed patient presentation to primary and secondary care, disruption to screening and healthcare services as a result of COVID-19 infections on staff and the need to shift intensive care to COVID-19 patients. Reductions in PD cancers in NI and the NED and in particularly lung cancers in NI, highlight the need for targeted public health campaigns to identify and treat ‘missing’ patients. Protecting cancer services should be a priority in any future pandemic or systemic healthcare system disruption.
Similar content being viewed by others
Background
The World Health Organisation (WHO) declared the novel coronavirus COVID-19 pandemic on 11th March 2020 [1]. The pandemic has had a substantial and ongoing impact on all aspects of society including education, commerce and healthcare systems [2]. As of 28th February 2023 over 758 million cases and over 6.8 million deaths had been reported worldwide [3]. The approach to the pandemic differed between the countries studied with NZ adopting a COVID-19 elimination policy, which involved border closure and an initial national lockdown, [4] while NI and NED adopted a containment and mitigation policy involving only limited travel and quarantine measures [5].
Cancer patients have been adversely impacted during the COVID-19 pandemic due to delays and rescheduling of cancer treatments and appointments [6]. In addition to the impact on current cancer patients, non-critical care such as cancer screening services were also disrupted. Although cessation of cancer screening was for a relatively short period, on reopening these services had to manage the backlog created and most were unable to operate at pre-pandemic capacity due to enhanced infection prevention and control and cleaning procedures, staff absence and redeployment associated with high levels of COVID-19 community transmission [7]. The impact of COVID-19 on screening varied across countries in this study. In NI breast, colorectal and cervical screening services were paused for a period of four months [8], in NED, faecal immunochemical testing (FIT) for colorectal cancer was paused for a period of 11 weeks [7] while breast screening was paused for a period of 12 weeks [9]. In NZ bowel, breast and cervical screening programmes were paused for 4 weeks in March and April 2020 [4]. Apart from temporary cessation of their screening programmes, disruption to health care services in NZ were minimal due to NZ’s strict COVID-19 elimination strategy,
The purpose of this study is to investigate the impact of COVID-19 on three common cancers (lung, breast, colorectal) in three high-income countries (NZ, NED and NI), which had different approaches to COVID-19 containment using population level data between the pre-pandemic period (2017–2019 average) and the initial pandemic period (2020).
Research in context
Evidence before this study
A previous study found NI experienced a 23% reduction in the number of pathologically diagnosed cancers between 1st March and 12th September 2020 compared to the previous three years (2017–2019) [10]. Although Hamilton et al. reported some recovery between August and September, the number of PD lung cancers remained well below pre-COVID-19 levels. An observational study from the NED Cancer Registry (NCR) also found fewer PD cancers (average weekly reduction 20%, range 9 − 27%) in the initial seven weeks of the pandemic (weeks 9 to 15, Feb 24th to April 12th) compared to the preceding seven weeks (weeks 2 to 8) [11]. In NZ there was a decline in cancer registrations during the initial national lockdown period (March-April 2020); however registrations returned to pre-shutdown levels over the subsequent months [4]. Previous studies investigated the impact of COVID-19 on colorectal and breast cancers. Gathani et al. [12] found that during the first six months of 2020 in England, there was a 28% reduction in breast cancer referrals and a 16% decrease in patients receiving their first treatment, compared to the same period in 2019. A study by Filipe et al. [13] found that pausing of the breast screening programme in NED led to a reduction in breast surgery for earlier stage cancers. A population-based study in England reported 3500 fewer colorectal cancer patients diagnosed in April-October 2020 compared to the same period in 2019 and found a 31% relative reduction in surgery in April 2020 [14]. Thirty six hospitals across the UK and Ireland reported deviation from national guidelines for colorectal cancer at all points of the patient care pathway during the first part of the COVID-19 pandemic [15].
Added value of this study
This study identifies, using population-based data, the impact of the first period of the COVID-19 pandemic on healthcare services. It compares for the first time the impact of different approaches to pandemic management on cancer services and identifies the scale of ‘lost cases’.
The impact on breast and colorectal cancers includes that from alterations to screening services, while for lung cancers the overlap of respiratory symptoms with COVID-19 posed problems for case identification, investigation, and treatment.
Methods
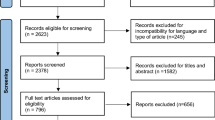
National cancer registries in each country provided population level data on pathologically diagnosed cancers for the pre-pandemic period (2017–2019) and the pandemic period (2020). Information was also collated on the number of COVID-19 cases and deaths per 100,000 population in each country – in the NED from the government coronavirus dashboard [16], in NZ from the Ministry of Health’s COVID-19 Dashboard [17], and in NI from the Department of Health Website [18].
The International Classification of Diseases, 10th revision (ICD10) codes used to identify cancers in NI were as follows; lung (C33-C34) female breast (C50) and colorectal (C18-C20). These data were derived from pathology data provided monthly to NICR [19]. For the NED the Cancer Registry (NCR) was also the source of pathologically diagnosed cancers and the ICD10 codes used were as follows; breast including male and female cancer (C50) and Ductal Carcinoma in situ (DCIS) (D05), lung including thymus and pleura (C33, C34, C37 and C38.4) and colorectal (C18-C20). The NZ data was from the NZ Cancer Registry (NZCR), with colorectal classification (C18-C20) similar to NED and NI, breast including male and female cases (C50) and lung (C30 – C39) including nasal cavity, (although the majority (94.2%) were classified as lung cancer (C33-C34)).
COVID-19 cases and deaths per 100,000 were calculated using midterm population estimates. Comparisons were made between average monthly pathology samples for the pre-pandemic period (2017–2019) and the pandemic period (2020) with differences expressed as percentages.
Inclusion and exclusion criteria
The same inclusion and exclusion criteria were applied to both the pre-pandemic and pandemic periods. In NI, pathology samples processed by private laboratories were excluded, this makes up a very small number of samples processed in NI. Where a patient has more than one pathology sample of the same cancer type this was counted once, except in cases where the pathology samples are separated by a period greater than two years. In NED, where a patient has more than one pathology sample of the same cancer type this was counted once. Only the first diagnosis per patient is included for incidence of invasive breast cancer, but all diagnoses for DCIS are included. One laboratory was excluded from data provided by NED due to delayed pathology notifications. In NZ, where a patient has more than one pathology sample of the same cancer type this was counted once.
Statistical analysis
Data analysis was completed using SPSS (IBM SPSS Statistics V25). Mann-Whitney U tests were performed to compare the number of cancer cases in the pre-pandemic period (2017–2019) and the pandemic period (2020) (two independent samples). Correlations were also calculated between monthly COVID-19 deaths and monthly cancer cases in each country.
Results
In 2020 highest monthly COVID-19 cases in NI was 1386/100K in October, in the NED it was 1571/100K in December, while in NZ it was 14/100K in March. Lower COVID-19 cases were recorded in mid-2020 following severe initial lockdown measures in all countries, with national minimum case numbers of 12/100K in NI in July, 22/100K in the NED in June and 0.3/100K in NZ in May. The highest number of deaths per month were reported in April in each country (NI (16.8), the NED (21.9) and NZ (0.4)) and the lowest number of deaths were reported in July and August in NI (both 0.3) and in July in the NED (0.3), with NZ recording no deaths for most months (Fig. 1).
Breast cancers
In 2020 there was a 10% reduction overall in PD breast cancer diagnoses in NI compared to the pre-pandemic period with greatest reductions in April (40%) and May (52%), with broad recovery from August onward. NED reported a similar pattern to NI with an overall reduction in pathologically diagnosed breast cancers of 18.2%, greatest reductions in April (52%) and May (46%) and recovery by September 2020. In contrast, NZ recorded a very small (0.2%) increase in PD breast cancers in 2020 compared to the pre-pandemic period with initial large decreases in April (51%) and May (34%) followed by early recovery by June 2020 with PDs consistently at or above pre-pandemic levels (Fig. 2).
Lung cancer
Although long-term global trends predicted lung cancer incidence would increase in 2020 [20] with the onset of the COVID-19 pandemic reductions in PD lung cancers were recorded in some countries. NI experienced an overall reduction of 23% during 2020 with the greatest reduction in April (53%) and only partial recovery for the rest of the year. Between March and December 2020, the reduction in number of lung cancer diagnoses was statistically significant (p = 0.001) in NI compared to the pre-COVID period. The NED experienced a very small overall reduction in pathologically diagnosed lung cancers (1%) with the greatest reductions in April and May (both 20%) but broad recovery by June 2020. In contrast, NZ recorded a 10% overall increase in lung cancers in 2020 compared to the pre-pandemic period, with only very slight reductions recorded in August and November (Fig. 3) and an increase recorded in the period between March and June 2020.
Colorectal (CR) cancers
The overall reduction in PD CR cancers during 2020 in NI was 15% with the greatest reductions in April (54%) and May (47%) (Fig. 3). There was good recovery between June and September, with PD cancers returning to at least pre-pandemic levels, although this was followed by reductions again in October and November. The NED recorded an overall reduction of 18.5% in 2020, with the greatest reductions in April and May (both 37%) and only partial recovery by July, with levels remaining about 20% lower than pre-pandemic levels up to Nov 2020. Again, in contrast, NZ recorded a 5% overall increase in PD CR cancers in 2020 compared to the pre-pandemic period, with a 31% reduction in April followed by an immediate recovery by May with this rebound sustained for the rest of the year and PD were generally above pre-pandemic levels (Fig. 4).
Discussion
Colorectal, breast and lung cancer are three of the most common cancers (excluding Non-Melanoma Skin Cancers) and this study reports the impact of different national pandemic control mechanisms on levels of these PD cancers. Prior to the pandemic, cancer trends predicted increases in new cancer rates, due in part to the ageing population and population growth, except where screening has been shown to decrease colorectal cancer levels [2]. Therefore, the lower levels found in this study were unexpected and can be directly linked to the COVID-19 pandemic.
Although long term global trends predicted lung cancer incidence would increase in 2020 [20], only NZ recorded an increase in PD lung cancers. NZ also recorded slight increases in breast and colorectal cancer despite the initial reductions at the start of the pandemic.
In NZ the FIT bowel screening programme began in July 2017, with the last regions joining in June 2022 [21]. The increase in colorectal cancer registrations in NZ may be linked to the introduction of bowel screening. Increases in cancer registrations were not found for any cancers in either the NED or NI.
The response to COVID-19 imposed sudden major change on health services as they rapidly adapted to meet the demands of the novel coronavirus. Primary care interactions switched from in-person to virtual consultations with multiple levels of telephone triage [22, 23]. Non-essential services such as cancer screening were paused and staff redeployed to care for COVID-19 patients, who had longer stays in high dependency and intensive care facilities compared to other respiratory conditions such as influenza [24]. In NI and NED, COVID-19 responses included legislation to restrict population mixing, ‘stay at home messaging’ and school and non-essential workplace closures, while in NZ the elimination approach entailed more severe restrictions including border closure and mandatory quarantine.
The impact of COVID-19 on breast, colorectal and lung cancers differed. Breast and colorectal cancers have population-based screening programmes in all countries included in this study. Screening accounts for approximately 30% of new breast cancers and 8% of colorectal cancers diagnosed in NI [25]. It is likely that pauses in cancer screening contributed to reduction in patient presentations during 2020, however this impact varies across the countries studied and there would not have had a uniform effect due to the differences in the screening ages and testing used. In NED, FIT has been fully implemented in the population since 2019 for those aged 55–75 years old [7]. Until 2021, NI used the faecal occult blood test (FOBT) for adults aged 60 to 74 and has since moved to FIT which is potentially more accurate, in part due to better patient acceptability and fewer false negatives [26].
Lung cancer was particularly impacted in NI with an overall reduction of 23% compared to just 1% in NED. While there is currently no population-based screening for lung cancer, some countries have piloted lung cancer screening for those most at risk of developing lung cancer. In NED, the NELSON study, a Dutch-Belgian Randomized Lung Cancer Screening Trial was conducted between 2004 and 2015 to investigate screening for high-risk subjects and found that there was a decrease in 10-year lung cancer mortality of at least 25% compared to the control group. However there was no statistically significant difference in all-cause mortality at 10 years between the screened and unscreened groups [27]. NZ does not have any lung cancer screening at present and there were no pilots during the study period (Personal communication, 2023). In the UK, there have been pilot lung cancer screening programs, however these are less developed in NI compared to England (UK Lung Cancer Coalition (UKLCC), 2020). During the initial first wave of the pandemic, there were significant pressures on respiratory teams to lead the diagnosis and treatment of COVID-19 patients which may have reduced their capacity to manage possible lung cancer diagnoses [28]. There were also concerns that Computerised Tomography (CT) imaging findings of COVID-19 may be radiologically indistinguishable from patients with lung cancer who have developed pneumonia [29].
The respiratory symptoms of lung cancer and COVID–19, including new persistent cough and breathlessness overlap. There were concerns regarding conflicting public health messaging from governments, with the UK government urging people to “Stay at Home” whilst simultaneously promoting better lung cancer awareness [28]. Across the UK the UKLCC reported a 75% reduction in urgent lung cancer referrals during the first wave of the pandemic [30], suggesting patients may have decided to self-isolate instead of seeking medical care when respiratory symptoms began. As a result of the reduction in urgent referrals for suspected lung cancer cases and pathology samples, some have called for lung cancer screening to be included in follow-up appointments for COVID-19 patients who have residual respiratory symptoms after the infection has cleared [31]. Lung cancer patients are also at increased risk of COVID-19, which may have led to missed or delayed diagnoses of lung cancers when a COVID-19 diagnosis may have been suspected, especially with high COVID-19 prevalence at the early stages of the pandemic [32]. In stark contrast, NZ had a 10% increase in the number of PD lung cancers detected in 2020 which occurred against a background of very low levels of COVID-19 and high levels of testing. There was a considerable dedication of resources to ensure the continuation of cancer services in NZ, with monitoring and evaluation of service delivery at the local level. Particular attention was placed on ensuring no further exacerbation of existing health inequalities for Māori and Pacific peoples [33]. This suggests that in NZ patients were more likely to attend healthcare settings as the likelihood of COVID-19 infection was low and also that lung cancer symptoms such as a persistent cough and breathlessness were perhaps investigated more thoroughly.
In NI, it is estimated that there were about 77 ‘missing’ lung cancer patients when cancer registrations were complete [34], which are likely to lead to later disease stage at presentation and may translate to reductions in survival. This ‘missing’ figure takes into account the other methods of diagnosis and not just PD cancers. In addition, a recent study conducted by Monari et al. [35] found that patients with cancer were at increased risk of hospitalisation and/or death from COVID-19. There may therefore be patients who had an undiagnosed cancer who went on to die from COVID-19 due to their increased vulnerability. Cancer Registries will be key to monitoring the impact of COVID-19 for many years.
Conclusions
COVID-19 had a lasting impact on detection and treatment of cancer patients, the full extent of which has yet to be quantified. This study has identified a concerning reduction in the number of lung cancers identified pathologically in NI compared to both NED and NZ. This is likely to be due to reductions in patient interaction with primary and hospital care and the overlap of lung cancer symptoms with COVID-19, possibly resulting in people not seeking medical attention.
It has been reported that countries which sought to eliminate COVID-19, like NZ, registered fewer deaths, had fewer restrictions and lockdowns and likely had much less disruption of healthcare and cancer services [5]. Our study found that in NZ, a country which sought to eliminate COVID-19 in the early stages of the pandemic and had very low rates of COVID-19 transmission during 2020, experienced very little change in levels of pathologically diagnosed breast, colorectal and lung cancers. In contrast two European countries (NI and NED) which adopted COVID-19 policies focused on containment and mitigation, rather than elimination, had high rates of COVID-19 transmission and experienced substantial reductions in pathologically diagnosed cancers. NI experienced reductions of 10%, 15% and 23% in breast, colorectal and lung cancers respectively while the NED experienced reductions of 18%, 19% and 1% in these same cancers. Longer term follow-up studies are required to assess the extent of recovery in cancer diagnoses across these countries.
Strengths
The strengths of this study include the use of national population-based cancer registry data and comparison with an average of three previous years to reduce inter-year variability.
Limitations
As pathological data was used, these will not be as complete or rigorously validated as finalised cancer registration data. However, data for 2017–2019 was also based on pathological diagnoses of cancer to ensure consistency of comparator data. As bowel screening roll-out was not uniform across NZ during the period of study, this may present a challenge in interpreting changes in colorectal cancer registrations during this time.
Also, the proportion of cancers that have a pathological diagnosis (microscopically verified) varies by cancer type. For example, in 2018 in the UK, 99% of breast cancers, 89% of colorectal cancers and 70% of lung cancers were microscopically verified (UKIACR, 2021). In NED 99.8% of breast cancers, 96% of colorectal cancers and 82% of lung cancers were microscopically verified.
The ICD10 codes used to define each cancer site varied slightly between the three countries investigated. For example, the NED included in-situ breast (D05) within their breast cancer cases while NZ included thymus, pleura, and nasal cavity (C30 – C39) in their lung cancer case numbers. Therefore, direct comparisons of cancer case numbers between countries should be interpreted with caution and percentage changes within each country over the period of investigation has been used throughout.
Data Availability
The datasets generated and/or analysed during the current study are not publicly available due the limits of the ethical approval granted to the NICR, NCR and NZCR to share patient level data. Anonymised, non-patient level data can be made available from the corresponding author on reasonable request.
Abbreviations
- CR:
-
Colorectal cancer
- CT:
-
Computerised tomography
- DCIS:
-
Ductal carcinoma in situ
- FIT:
-
Faecal immunochemical test
- FOBT:
-
Faecal occult blood test
- ICD10:
-
International Classification of Diseases, 10th revision
- NCR:
-
Netherlands Cancer Registry
- NED:
-
Netherlands
- NI:
-
Northern Ireland
- NICR:
-
Northern Ireland Cancer Registry
- NZ:
-
Aotearoa New Zealand
- NZCR:
-
Aotearoa New Zealand Cancer Registry
- PD:
-
Pathologically diagnosed
- UKLCC:
-
UK Lung Cancer Coalition
References
WHO. WHO Director-General’s opening remarks at the media briefing on COVID-19–11 March 2020 [Internet]. 2020 [cited 2022 Oct 25]. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
Mishra NTP, Das SS, Yadav S, Khan W, Afzal M, Alarifi A et al. Global impacts of pre- and post-COVID-19 pandemic: Focus on socio-economic consequences. Sensors Int [Internet]. 2020;1:100042. Available from: https://www.sciencedirect.com/science/article/pii/S2666351120300425.
WHO. WHO Coronavirus (COVID-19). Dashboard [Internet]. 2023 [cited 2023 Mar 1]. Available from: https://covid19.who.int/.
Gurney JK, Millar E, Dunn A, Pirie R, Mako M, Manderson J et al. The impact of the COVID-19 pandemic on cancer diagnosis and service access in New Zealand–a country pursuing COVID-19 elimination. Lancet Reg Heal - West Pacific. 2021;10.
Oliu-Barton M, Pradelski BSR, Aghion P, Artus P, Kickbusch I, Lazarus JV et al. SARS-CoV-2 elimination, not mitigation, creates best outcomes for health, the economy, and civil liberties. Lancet [Internet]. 2021;397(10291):2234–6. Available from: https://doi.org/10.1016/S0140-6736(21)00978-8.
Kutikov A, Weinberg DS, Edelman MJ, Horwitz EM, Uzzo RG, Fisher RI. A War on Two Fronts: Cancer Care in the Time of COVID-19. Ann Intern Med [Internet]. 2020;172(11):756–8. Available from: https://doi.org/10.7326/M20-1133.
Kortlever TL, de Jonge L, Wisse PHA, Seriese I, Otto-Terlouw P, van Leerdam ME, et al. The national FIT-based colorectal cancer screening program in the Netherlands during the COVID-19 pandemic. Prev Med (Baltim). 2021;151:106643.
Public Health Agency. Covid 19 Impact on Breast Cancer Screening Programme [Internet]. 2020. Available from: https://www.publichealth.hscni.net/directorate-public-health/service-development-and-screening/breast-screeninghtm.
Eijkelboom AH, de Munck L, Lobbes MBI, van Gils CH, Wesseling J, Westenend PJ et al. Impact of the suspension and restart of the Dutch breast cancer screening program on breast cancer incidence and stage during the COVID-19 pandemic. Prev Med (Baltim) [Internet]. 2021;151:106602. Available from: https://www.sciencedirect.com/science/article/pii/S0091743521001869.
Hamilton AC, Donnelly DW, Loughrey MB, Turkington RC, Fox C, Fitzpatrick D et al. Inequalities in the decline and recovery of pathological cancer diagnoses during the first six months of the COVID-19 pandemic: a population-based study. Br J Cancer. 2021.
Dinmohamed AG, Visser O, Verhoeven RHA, Louwman MWJ, van Nederveen FH, Willems SM et al. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. Lancet Oncol [Internet]. 2020;21(6):750–1. Available from: https://doi.org/10.1016/S1470-2045(20)30265-5.
Gathani T, Clayton G, MacInnes E, Horgan K. The COVID-19 pandemic and impact on breast cancer diagnoses: what happened in England in the first half of 2020. Br J Cancer. 2021;124(4).
Filipe MD, van Deukeren D, Kip M, Doeksen A, Pronk A, Verheijen PM et al. Effect of the COVID-19 Pandemic on Surgical Breast Cancer Care in the Netherlands: A Multicenter Retrospective Cohort Study. Clin Breast Cancer [Internet]. 2020;20(6):454–61. Available from: https://www.sciencedirect.com/science/article/pii/S152682092030207X.
Morris EJA, Goldacre R, Spata E, Mafham M, Finan PJ, Shelton J et al. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: a population-based study. Lancet Gastroenterol Hepatol [Internet]. 2021;6(3):199–208. Available from: https://www.sciencedirect.com/science/article/pii/S2468125321000054.
CRC COVID Research Collaborative. The impact of the COVID-19 pandemic on colorectal cancer service provision. Br J Surg [Internet]. 2020;107(11):e521–2. Available from: https://doi.org/10.1002/bjs.11990.
Rijksoverheid. Coronavirus Dashboard [Internet]. 2021. Available from: https://coronadashboard.government.nl/landelijk/positief-geteste-mensen.
Institute of Environmental Science and Research Ministry of Health - New Zealand. NZ COVID-19 Dashboard [Internet]. 2021. Available from: https://nzcoviddashboard.esr.cri.nz/#!/.
Northern Ireland Statistics and Research Agency. Coronavirus (COVID-19) Statistics [Internet]. 2021. Available from: https://www.nisra.gov.uk/statistics/ni-summary-statistics/coronavirus-covid-19-statistics.
NICR. The impact of the COVID-19 on cancer diagnosis [Internet]. 2021 [cited 2021 Jun 21]. Available from: https://www.qub.ac.uk/research-centres/nicr/Publications/ImpactofCovid19onCancerDiagnosis/.
McIntyre A, Ganti AK. Lung cancer—A global perspective. J Surg Oncol [Internet]. 2017;115(5):550–4. Available from: https://doi.org/10.1002/jso.24532.
Ministry of Health – Manatū Hauora. National Bowel Screening Programme [Internet]. 2022 [cited 2023 Jan 23]. Available from: https://www.health.govt.nz/our-work/preventative-health-wellness/screening/national-bowel-screening-programme#:~:text=The free National Bowel Screening,for screening every 2 years.
Majeed A, Maile EJ, Bindman AB. The primary care response to COVID-19 in England’s National Health Service. J R Soc Med. 2020;113(6):208–10.
Gerada C. Primary care has transformed into a “dial-in” or “Click First” service. Health Serv J. 2020;27.
Ludwig M, Jacob J, Basedow F, Andersohn F, Walker J. Clinical outcomes and characteristics of patients hospitalized for influenza or COVID-19 in Germany. Int J Infect Dis. 2021;103:316–22.
Bannon F, McKenna H, Donnelly C, Mayock M, Harbinson A, Mathieson S et al. Pathways to a Cancer Diagnosis: Monitoring the variation in the patient journey across Northern Ireland. 2020.
Mousavinezhad M, Majdzadeh R, Sari AA, Delavari A, Mohtasham F. The effectiveness of FOBT vs. FIT: a meta-analysis on colorectal cancer screening test. Med J Islam Repub Iran. 2016;30:366.
Adams SJ, Stone E, Baldwin DR, Vliegenthart R, Lee P, Fintelmann FJ. Lung cancer screening. Lancet [Internet]. 2023;401(10374):390–408. Available from: https://www.sciencedirect.com/science/article/pii/S0140673622016944.
Gourd E. Lung cancer control in the UK hit badly by COVID-19 pandemic. Lancet Oncol [Internet]. 2020;21(12):1559. Available from: https://doi.org/10.1016/S1470-2045(20)30691-4.
Calabrò L, Peters S, Soria J-C, Di Giacomo AM, Barlesi F, Covre A, et al. Challenges in lung cancer therapy during the COVID-19 pandemic. Lancet Respir Med. 2020;8(6):542–4.
UK Lung Cancer Coalition. COVID-19 Matters [Internet]. 2020. Available from: https://www.uklcc.org.uk/our-reports/october-2020/covid-19-matters.
George PM, Barratt SL, Condliffe R, Desai SR, Devaraj A, Forrest I, et al. Respiratory follow-up of patients with COVID-19 pneumonia. Thorax. 2020;75(11):1009–16.
Singh AP, Berman AT, Marmarelis ME, Haas AR, Feigenberg SJ, Braun J et al. Management of Lung Cancer During the COVID-19 Pandemic. JCO Oncol Pract [Internet]. 2020;16(9):579–86. Available from: https://doi.org/10.1200/OP.20.00286.
Millar E, Gurney J, Beuker S, Goza M, Hamilton MA, Hardie C et al. Maintaining cancer services during the COVID-19 pandemic: the Aotearoa New Zealand experience. Lancet Reg Heal - West Pacific. 2021;11.
NICR. Impact of COVID-19 on incidence, survival and mortality of lung cancer in Northern Ireland [Internet]. 2022. Available from: https://www.qub.ac.uk/research-centres/nicr/FileStore/OfficialStats2020/Filetoupload,1321783,en.pdf.
Monari C, Sagnelli C, Maggi P, Sangiovanni V, Numis FG, Gentile I et al. More severe COVID-19 in patients with active Cancer: results of a Multicenter Cohort Study. Front Oncol. 2021;11.
Acknowledgements
This work would not have been possible without the staff of the registries involved, whose knowledge, skill and dedication leads to assimilation and analysis of data provided by patients and collected by the health service as part of their care and support and which results in outputs such as paper. This research has been conducted using data from the Northern Ireland Cancer Registry (NICR) which is funded by the Public Health Agency, Northern Ireland, the Netherlands Cancer Registry (NCR) maintained by the Netherlands Comprehensive Cancer Organization, and the New Zealand Cancer Registry (NZCR) maintained by the Ministry of Health. However, the interpretation and conclusions of the data are the sole responsibility of the author(s).
Funding
The Northern Ireland Cancer Registry is funded by the Public Health Agency of Northern Ireland. This uses data collected by health services as part of their care and support functions.
Author information
Authors and Affiliations
Contributions
Original idea, supervision and drafting -AG, analysis and drafting of manuscript text- HM, original data collection, analysis and primary collation - JMcL, provision of data - OV, EM, review and editing of manuscript – HM, DB, EM, OV, TL, AG & JMcL.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
This study was conducted on aggregate anonymised data in with data sharing agreements in place with New Zealand and the Netherlands and data is presented in accordance with Northern Ireland Cancer Registry (NICR) Confidentiality and Data Protection Policies and New Zealand’s Privacy Act 2020, the Health Information Privacy Code 2020. The NICR has ethical approval from the Office for Research Ethics Committees of Northern Ireland (ORECNI) (Ref: 20/NI/0132, IRAS project ID: 288121), for the collection and use of routinely collected data, relating to cancer patients, within the fields of health and social care research. As such, specific ethical approval and informed consent from the data subjects were not required for this study. All methods were subject to scientific critique and all data processing and analysis was conducted in accordance with the ORECNI conditions for ethical approval to use this data. The data from New Zealand was provided at an aggregated level in adherence to New Zealand’s Privacy Act 2020, the Health Information Privacy Code 2020, and the Health Information Governance Guidelines Ministry of Health, HISO 10064:2017: health information governance guidelines. Wellington, New Zealand: Ministry of Health; 2017. As such, ethical approval was not required from an ethics committee in New Zealand and the aggregate anonymous data was approved for use in line with Te Aho o Te Kahu Confidentiality and Data Protection Policies. In the Netherlands, this study did not require approval from an ethics committee according to the Central Committee on Research involving Human Subjects (CCMO). The Privacy Review Board of the Netherlands Cancer Registry approved the use of anonymous data for this study.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mitchell, H., Mclean, J., Gavin, A.T. et al. Impact of COVID-19 control on lung, breast, and colorectal pathological cancer diagnoses. A comparison between the Netherlands, Aotearoa New Zealand, and Northern Ireland. BMC Cancer 23, 700 (2023). https://doi.org/10.1186/s12885-023-11216-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-11216-3