Abstract
Background
Sexual wellbeing is a critical yet often overlooked aspect of overall wellbeing for women across cancer diagnoses.
Objective
We identified profiles of women cancer survivors by sexual and psychosocial outcomes and compared groups for differences in relevant outcomes and individual characteristics.
Methods
Partnered women treated for cancer (n = 226; M age = 51.1 (12.6); 54% breast cancer; 86% White) completed a cross-sectional survey assessing sexual and psychosocial wellbeing. K-means cluster analysis modeled subgroups (clusters) with similar response patterns on measures of sexual wellbeing (sexual function, distress, sexual communication, and self-efficacy for communication), psychosocial wellbeing (quality of life (QOL), anxiety and depressive symptoms), and time since treatment. ANOVAs with Tukey post-hoc analyses and chi-square analyses tested cluster mean differences.
Results
Three distinct clusters of women differed by levels of adjustment in sexual and psychosocial wellbeing: higher-adjustment (32.7%), intermediate (37.6%), and lower-adjustment (29.6%). Significant differences among the clusters were found for all outcomes, with largest effect sizes for sexual distress (η2p = 0.66), sexual communication (η2p = 0.51), sexual satisfaction (η2p = 0.44), and anxiety and self-efficacy for communication (η2p = 0.32). The intermediate adjustment group was characterized by lower adjustment on measures of sexual and relationship function, and better adjustment on measures of QOL and mood.
Conclusions
Findings suggest that for women cancer survivors, measures of sexual and psychosocial wellbeing can model distinct profiles to inform targeted interventions to meet women’s needs. Evidence-based targeted interventions could lead to better sexual function, and ultimately to better QOL and overall wellbeing.
Implications for practice
A stepped intervention approach to sexual health care for women with cancer, where content and format depend on degree of sexual and psychosocial adjustment after cancer, may be most appropriate. Interdisciplinary teams may address sexual, emotional, and relationship functioning.
Similar content being viewed by others
There are approximately 8.8 million women with a history of invasive cancer in the United States [1], many of whom experience long term sexual sequelae of their treatment [2, 3]. Sexual wellbeing is an important part of quality of life for women across different cancers or treatment types [4], ages [5], and menopausal statuses [6]. Cancer treatment may cause physical, emotional, and relational changes that negatively affect sexual function and intimacy in relationships. Despite evidence that women want these issues addressed [7, 8], few oncology clinicians feel they have the time, expertise, comfort level, or referral resources to address women’s sexual wellbeing [9, 10]. Thus, women’s sexual wellbeing after cancer treatment is largely unaddressed [11].
Sexual wellbeing is a multidimensional concept [12], comprised of physical, emotional, and interpersonal components as evidenced by the relationship of sexual function with mood, relationship quality, self-efficacy, and communication [13, 14]. While prior research has shown that women’s sexual and relationship function, mood, and QOL are inter-related, studies have not specifically examined whether women could be grouped, or profiled, according to their responses on these outcome measures. Identifying profiles based on scores on outcomes of sexual, relationship, and psychosocial well-being could assist women and/or their clinicians in the selection of existing interventions, or inform the development of interventions to best address women’s sexual health needs to improve their overall well-being. For instance, it is possible that some women could experience sexual dysfunction and distress concurrently with distressed mood and relationship quality, whereas others may experience mild concerns, with limited or no concomitant effects seen for their mood or relationship quality. This individual variation in experiences may call for different approaches to education, support and treatment. Therefore, the goal of the present study was to explore sexual and psychosocial wellbeing of adult women treated for cancer, and to characterize subgroups (profiles) of women via cluster analysis based on standardized measures of sexual and psychosocial outcomes.
Methods
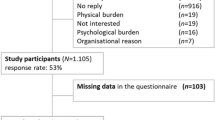
This manuscript describes a secondary analysis of cross-sectional data collected from 226 women with a cancer history who participated in an instrument evaluation study [14]. The goal of the original study was to assess the psychometric performance of the newly developed Self-Efficacy to Communicate about Sex and Intimacy (SECSI) scale which is intended to assess a woman’s confidence in her ability to communicate with her intimate partner about sex and intimacy. The university institutional review board approved the study (IRB #2016B0341). Adult women treated for any type of cancer who had a male partner were eligible. Women were recruited through local media (flyers, newsletters, oncology clinic postings), and ResearchMatch®, a NIH-sponsored national database of health research volunteers. Interested women were sent a link to complete informed consent, and to respond to standardized measures and questions about sexual behaviors, sociodemographic, and cancer characteristics via a one-time online survey.
Measures
Sexual Function. The Female Sexual Function Index (FSFI) is a widely used 19-item self-report scale, with higher scores indicating better sexual functioning [15] that has significant research supporting its use in women with cancer [16]. The FSFI had high internal consistency reliability in the present sample (Cronbach’s alpha = 0.97 for the total scale, and 0.85 - 0.98 for the subscales).
Sexual Distress. The Female Sexual Distress Scale Revised (FSDS-R) is a 13-item scale assessing sexually-related personal distress in women [17] that has been used successfully in women with cancer [18, 19]. The FSDS had high internal consistency reliability in this sample (Cronbach’s alpha = 0.96).
Sexual Behaviors. This 10-item questionnaire covered sexual behaviors (sex or intimate act) over the last 4 weeks [14]. They were asked if they had interest in or engaged in sexual activity (yes/no); if they or their partner had avoided or declined sexual advances, and if their partner had any limitations to perform sexual activity (yes/no)’ frequency of kissing and intercourse (frequency scale from none to more than once per day), and which partner initiated these activities most of the time; and to rate their sex life currently from ‘could not be better’ to ‘could not be worse’.
Relationship Satisfaction. Relationship satisfaction was measured using the 7-item abbreviated version of the Dyadic Adjustment Scale (DAS-7), which has been shown to correlate strongly with the original measure [20]. Higher scores indicate better relationship quality and satisfaction. The DAS-7 had good internal consistency reliability in the present sample (Cronbach’s alpha = 0.83).
Sexual Communication. The 13-item Dyadic Sexual Communication Scale (DSCS) has demonstrated good internal consistency reliability (Cronbach’s alpha = 0.81), test-retest reliability (r = 0.89), and discriminant validity between people with and without sexual problems (p < .01) [21, 22]. Higher scores indicate better perceived quality of communication. The DSCS had excellent internal consistency reliability in the present sample (Cronbach’s alpha = 0.90).
Self-Efficacy for Sexual Communication. The Self-Efficacy to Communicate about Sex and Intimacy (SECSI) scale is a 10-item scale assessing the extent of confidence to communicate with a romantic partner about changes in sex and intimacy after cancer treatment, with higher sum scores indicating greater self-efficacy [14]. The SECSI scale had high internal consistency reliability (Cronbach’s alpha = 0.94) and good test-retest reliability (r = 0.82) in the reported study.
Health-Related Quality of Life. Health-related quality of life was measured by the widely used Functional Assessment of Cancer Therapy–General (FACT-G) instrument [23] which contains 27 items assessing four domains of wellbeing: physical, social/family, emotional, and functional. Higher scores signify higher perceived quality of life. The FACT-G had very good to excellent internal consistency reliability in the present sample (Cronbach’s alpha = 0.93 for the total scale, and 0.84 – 0.88 for subscales).
Anxiety and Depression. Anxiety and depression symptoms were measured using the Generalized Anxiety Disorder (GAD-7) [24] scale and Patient Health Questionnaire (PHQ-8) scale [25]. Higher scores indicate greater symptom burden. Both scales had very good to excellent internal consistency reliability in the present sample (Cronbach’s alpha = 0.91 for the GAD-7 and 0.87 for the PHQ-8).
Data analysis
Degree and patterns of data missingness was evaluated by variable. Standardized scales with 5% missing data or less were assumed to be missing at random, and therefore missing values were imputed for analysis. We used multiple imputation methods to model missing data for GAD-7, PHQ-8, FSDS, SECSI, DAS-7, and DSCS. It appeared that women with missing FACT-G data (7.5-15.5% missing data by subscale) and FSFI data (25.7%) appeared to be missing not at random and therefore cases were retained in models but missing data was not imputed.
K-means cluster analysis was used to model subgroups with similar response patterns on measures of sexual wellbeing (sexual function, distress, sexual communication, and communication self-efficacy), psychosocial wellbeing (quality of life (QOL), anxiety and depressive symptoms), and time since treatment. Main study variables initially entered were subsequently reduced until there were several technically viable cluster solutions. K-means cluster analysis generated several technically viable cluster solutions that included two, three, and four derived clusters. The three-cluster model is presented in Table 2. The three-cluster solution best-balanced technical, conceptual, and practical considerations, incorporating the anticipated clinical and research uses of the results.
Once the clusters were identified, we tested for significant differences in cluster means. For interval and ratio variables, we first evaluated group differences with one-way analysis of variance (ANOVA) followed by post-hoc Tukey analysis for control of Type I error. Then partial eta-squared (η2p) values were computed to examine the relative effect sizes of mean scores differences between clusters on modeled variables. For categorical variables, chi-square tests of proportions (χ2) were used to examine group differences. Discriminant function analysis was performed to validate cluster analysis results.
Results
The mean age in this study was 51 years old (SD 12.6). Women were together with their partner an average of 20 years (SD 13.8). Most women (86.3) identified as white and highly educated with 53.5% having experienced breast cancer (Table 1). Sixty-eight percent of participants participated in sexual or intimate activity in the last 4 weeks.
K-means cluster analysis generated several technically viable cluster solutions that included two, three, and four derived clusters of women’s sexual and psychosocial wellbeing. The three-cluster model was the best representation of conceptual and practical considerations (Table 1). Overall, cluster 1 (32.7% of the sample) is characterized by better scores on sexual and psychosocial outcome measures, cluster 3 (29.6%) is characterized by worse scores on these measures, and cluster 2 (37.6%) is characterized by scores intermediate to these two groups on either extreme. The mean distance of cases in relation to the cluster centroid is an indicator of within-group homogeneity. The mean distances (with standard deviation) that were computed for the present sample to describe homogeneity within clusters are 16.7 ± 5.9 for cluster 1, 17.4 ± 4.8 for cluster 2, and 20.9 ± 6.2 for cluster 3.
There were statistically significant mean score differences between the three clusters for all variables except for time since treatment and time since diagnosis (Table 2). Effect sizes for statistically significant differences in variables between clusters range from small partial eta-squared (η2p) effects for age and years with partner (.03), medium η2p for physical QOL and relationship satisfaction (.13), to large η2p effects for the remainder of the modeled variables (.17 to .66). Most variables had a large effect size (Ƞ2 > 0.14): FACT-G Social (0.26), Emotional (0.20), Functional (0.17), and Total (0.26) scores; GAD-7 (0.32); PHQ-8 (0.28); FSFI Desire (0.23), Arousal (0.26), Lubrication (0.17), Orgasm (0.19), Satisfaction (0.44), Pain (0.17) and Total (0.29) scores; FSDS (0.66); SECSI (0.32); and DSCS (0.51). The largest effect size for difference between cluster means was for sexual distress with η2p of 0.66. The clusters of women also differed significantly on several sexual behaviors over the last 4 weeks (p-values.05-.01): interest in sexual activity (yes/no), engagement in sexual activity (yes/no), whether they avoided or declined sexual advances from their partner (yes/no), frequency of kissing, frequency of intercourse or equivalent activity, and ratings of their sex life.
In a stepwise discriminant function analysis (for a review of clustering methods and validation techniques, see Aldenderfer and Blashfield [27], the model retained FSDS, DSCS, and GAD-7, and removed the other variables. Canonical discriminant functions are plotted with cases assigned to clusters (Fig. 1). Cluster centroids are included to illustrate cluster distribution and homogeneity. Classification results showed that the predictive model would correctly assign cases to cluster 1 with an accuracy of 86.8%, cluster 2 with an accuracy of 97.3%, and cluster 3 with an accuracy of 94.9%.
Discussion
Whereas most prior quantitative studies have examined correlations between and predictors of sexual wellbeing, mood and QOL [28, 29], this study is unique in examining distinct subgroups of women who may share certain sexual and psychosocial factors. The cluster analytic approach used in the present study allows us to extend previous findings by characterizing subgroups (profiles) of women who differ in their sexual and psychosocial wellbeing and risk factors.
Overall, study findings are consistent with prior research in women with cancer showing that women reporting higher versus lower sexual well-being tend to differ in their physical and psychological health outcomes [30]. For instance, prior qualitative studies have demonstrated that women report a range of experiences in response to cancer survivorship, from significant negative consequences of treatment on women’s sexual function and relationship to growing closer together with a partner and finding new ways for experiencing intimacy [31, 32]. Our findings are also consistent with results of prior quantitative studies demonstrating that mood, sexual wellbeing and relationship quality are generally correlated for women after cancer [33, 34]. In this vein, a number of studies have found that cancer survivors who have better sexual communication are more responsive to each other’s needs, may engage in more effective coping, and experience less distress, better sexual functioning, and report better relationship satisfaction [29, 35, 36] than women with poor sexual communication.
A key finding that extends previous research was that three distinct subgroups of women treated for cancer emerged that differed in their reports of sexual and psychosocial wellbeing. Slightly over one-third of the sample fell into cluster 1, the higher-adjustment group, which was characterized by better sexual adjustment and relationship adjustment, mood, and quality of life. Women in this cluster were also distinguished by greater self-efficacy, or confidence, in communicating with their partners about changes in sex and intimacy after cancer treatment. In sum, they were doing very well in a range of domains of sexual and overall health. The largest group, however, was cluster 2, the intermediate adjustment group, which was characterized by lower adjustment on measures of sexual and relationship function, but better adjustment on measures of QOL and mood. The findings for this group are intriguing because they indicate that the lower adjustment in the sexual wellbeing outcomes for women in this group seem independent of their mood or QOL. Women in this group may be engaging in coping skills that prevent their sexual problems from impairing their mood or QOL. Another possibility is thatthey may have had high premorbid mood, which could have acted as a buffer against the impact of sexual problems on their overall wellbeing. Finally, women in cluster 3, the lower-adjustment group, reported worse sexual wellbeing, worse mood, and worse quality of life compared to the other two subgroups of women, suggesting that women in this group may be struggling with many aspects of recovery and survivorship extending beyond their sexual lives. This is the group that may have the least amount of resources, whether in terms of their mood or relationship, to call upon to buffer against their sexual problems, leading to worse overall outcomes, although this is conjecture.
One noteworthy finding was that sexual distress had the largest effect size difference between groups, signifying that it was the measure that best distinguished the clusters of women. The fact that this measure tracked most closely with the levels of adjustment represented by the clusters may be partly explained by the nature of sexual distress as capturing a higher-level appraisal of the sexual problems women are experiencing [37, 38]. For instance, whereas some women may experience low desire and feel distressed as a result, others may experience the same low desire without singificant distress. Indeed, distress constitutes an important component of sexual disorders and one that clinical guidelines in oncology recommend should be assessed when screening for sexual function problems. Our findings are in line with these clinical recommendations and suggest that sexual distress may serve as a useful barometer for women’s overall cancer-related sexual adjustment [39].
When differences between clusters in demographic characteristics were examined, there appeared to be some patterns that may be helpful to describe the groups. Both age (cluster 1 members more likely to be older than cluster 3 members, p = 0.04) and years in relationship with their partner (cluster 2 members more likely to be in a longer relationship than cluster 3 members, p = 0.04) differed significantly between groups. Other differences in demographics by cluster were not significant, but trends may bear examining, such as the larger proportion of women in cluster 3 in the lower education and income categories. Further research is warranted to understand how social and economic factors influence psychological and sexual adjustment after cancer.
Results of this secondary data analysis should be interpreted in light of the study’s strengths and limitations. The findings are generalizable to a relatively broad cancer survivor population in the U.S., as participants represented a wide age range and types of cancer. This is a strength because most prior studies have tended to focus on survivors of breast and gynecologic cancer [2, 40]. Yet, individuals diagnosed with non-reproductive cancers can rate sex as equally important as those with cancers affecting the reproductive organs (e.g., breast and gynecologic cancers) [29], supporting the premise that sexual wellbeing should be studied in women across a range of cancer diagnoses. A limitation of the sexual function (FSFI) scoring is that women who are not sexually active will have low scores (e.g., items about arousal, orgasm, or pain scored as ‘0’), though they may be sexually inactive for many reasons, including limitations of their partner to participate in sexual activity. Future studies should consider ways of addressing this issue, whether by limiting enrollment based on sexual activity status, using measures that can assess sexual function irrespective of sexual activity status, or including additional questions about reasons for sexual inactivity and potentially considering these responses in analyses.
Although we took into account both conceptual and practical considerations when selecting the three-cluster analysis model for interpretation, alternative cluster solutions and interpretations may also be viable. There are multiple potential guidelines suggesting sample size for cluster analysis, and our full sample may have been underpowered. The sample size was not such that we could do subgroup analyses and this study should be replicated in a larger sample. In addition, because the original study was a cross-sectional survey of women with widely variable time since treatment, it is not possible to determine whether women’s characteristics, and thus the differences between clusters, represent pre-cancer personal and relationship characteristics or effects of cancer treatment. All participants were partnered, so inferences should be limited to partnered survivors. In addition to replication of findings in larger samples, we also suggest replication studies in samples with more socioeconomic and racial/ethnic diversity. Further research is needed to design and test the efficacy, effectiveness, and costs of tailored interventions based on level or degree of need. While many studies have focused on sexual health and fertility in younger cancer survivors, the largest – and growing – age group of cancer survivors are older adults. As fatigue, diabetes, and poorer self-rated health are found to be associated with decline in sexual wellbeing for older adults, assessing and intervening for sexual wellbeing in this patient population is also warranted [41]. Finally, we did not examine partner factors such as sexual function or mood, which could have a bearing on women’s sexual adjustment and should be examined in future studies.
Clinical implications
These results have important clinical implications. Findings suggest that many women report positive psychosocial and sexual adjustment after cancer, which may come as welcome news to clinicians. For instance, clinicians may wish to incorporate the message that many women can still enjoy satisfying relationships and wellbeing even in the face of sexual difficulties with their patients, who may find this encouraging news. In addition, findings suggest that a stepped approach to sexual health care for women with cancer may be most appropriate and that such an approach could include different interventions, both in terms of content and format (e.g., duration, intensity), depending on the profile of adjustment. For example, whereas all women after cancer should receive assessment of cancer-related sexual concerns and education on effects of treatment on sexual function [42], a relatively small number of women will likely require intensive and complex sexual health treatment or sex and relationship therapy. Specifically, results of this study suggest that particular attention could be paid to efforts at assessing and managing sexual issues for women in the lower adjustment group, given how wide-ranging the impact of their cancer seems to be on various facets of their well-being. Clinicians may find it useful to consider whether a patient’s sexual difficulties are co-occurring with difficulties in mood and relationship quality, as this could suggest that an interdisciplinary approach addressing not only the patient’s sexual concerns, but also aspects of their emotional and relationship functioning could be beneficial. By contrast, we suspect that the women experiencing sexual difficulties but who report largely positive adjustment otherwise, could potentially benefit from a focused sexual wellbeing intervention. More work needs to be done to examine the content and format of interventions that would best meet the needs of each of these groups.
Conclusion
Sexual difficulties are common and distressing after treatments for a range of cancers. While such difficulties are widely prevalent, the results of this study suggest they can be found both alongside and independent of other psychosocial difficulties, indicating a range of experiences for women. Examining profiles of response across a range of measures of wellbeing may help determine paths forward to intervention and ultimately enhance quality of life for women after cancer.
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
American Cancer Society. Cancer Treatment & Survivorship Facts & figures 2019-2021. Atlanta: American Cancer Society; 2019.
Sadovsky R, Basson R, Krychman M, Morales AM, Schover L, Wang R, et al. Cancer and sexual problems. J Sex Med. 2010;7(1 Pt 2):349–73.
Bober SL, Varela VS. Sexuality in adult Cancer survivors: challenges and intervention. J Clin Oncol. 2012;30(30):3712–9.
Reese JB, Shelby RA, Keefe FJ, Porter LS, Abernethy AP. Sexual concerns in cancer patients: a comparison of GI and breast cancer patients. Support Care Cancer. 2010;18(9):1179–89.
Lindau ST, Schumm LP, Laumann EO, Levinson W, O'Muircheartaigh CA, Waite LJ. A study of sexuality and health among older adults in the United States. N Engl J Med. 2007;357(8):762–74.
Lindau ST, Anderson D, Gavrilova N. Sexual morbidity in very long-term survivors of vaginal and cervical Cancer: a comparison to National Norms. Gynecol Oncol. 2007;106(2):413–8.
Flynn KE, Reese JB, Jeffery DD, Abernethy AP, Lin L, Shelby RA, et al. Patient experiences with communication about sex during and after treatment for cancer. Psycho-Oncology. 2012;21(6):594–601.
Gilbert E, Perz J, Ussher JM. Talking about sex with health professionals: the experience of people with cancer and their partners. Europ J Cancer Care. 2014.
Park ER, Norris RL, Bober SL. Sexual health communication during cancer care: barriers and recommendations. Cancer J. 2009;15(1):74–7.
Dyer K, das Nair R. Why don't healthcare professionals talk about sex? A systematic review of recent qualitative studies conducted in the United Kingdom. J Sex Med. 2013;10(11):2658–70.
Reese JB, Sorice K, Beach MC, Porter LS, Tulsky JA, Daly MB, et al. Patient-provider communication about sexual concerns in cancer: a systematic review. J Cancer survivorship : research and practice. 2017;11(2):175–88.
Gilbert E, Ussher JM, Perz J. Sexuality after gynaecological cancer: a review of the material, intrapsychic, and discursive aspects of treatment on women's sexual-wellbeing. Maturitas. 2011;70(1):42–57.
Brotto LA, Yule M, Breckon E. Psychological interventions for the sexual sequelae of cancer: a review of the literature. J Cancer Survivorship: Research and Practice. 2010;4(4):346–60.
Arthur EK, Wills CE, Browning K, Overcash J, Menon U. The self-efficacy to communicate about sex and intimacy (SECSI) scale: psychometric assessment in women treated for cancer. Support Care Cancer. 2019.
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The female sexual function index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex & Marital Ther. 2000;26(2):191–208.
Baser RE, Li Y, Carter J. Psychometric validation of the female sexual function index (FSFI) in cancer survivors. Cancer. 2012;118(18):4606–18.
Derogatis RR, Leiblum S, Burnett A, Heiman J. The female sexual distress scale (FSDS): initial validation of a standardized scale for assessment of sexually related personal distress in women. J Sex Marital Ther. 2002;28(4):317–30.
Brotto LA, Erskine Y, Carey M, Ehlen T, Finlayson S, Heywood M, et al. A brief mindfulness-based cognitive behavioral intervention improves sexual functioning versus wait-list control in women treated for gynecologic cancer. Gynecol Oncol. 2012;125(2):320–5.
Classen CC, Chivers ML, Urowitz S, Barbera L, Wiljer D, O'Rinn S, et al. Psychosexual distress in women with gynecologic cancer: a feasibility study of an online support group. Psycho-Oncology. 2013;22(4):930–5.
Spanier GB. Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. J Marriage Fam. 1976;38(1):15–28.
Catania J. Dyadic sexual communication scale. In: Fisher TD, Davis CM, Yarber WL, Davis SL, editors. Handbook of sexuality-related measures. Thousand Oaks: SAGE Publications, Inc.; 1998. p. 129–31.
Catania J, Pollack L, McDermott LJ, Qualls SH, Cole L. Help-seeking behaviors of people with sexual problems. Arch Sex Behav. 1990;19(3):235–50.
Webster K, Cella D, Yost K. The functional assessment of chronic illness therapy (FACIT) measurement system: properties, applications, and interpretation. Health Qual Life Outcomes. 2003;1:79.
Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1-3):163–73.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988.
Aldenderfer M, Blashfield R. Cluster analysis. Thousand Oaks, California1984. Available from: https://methods.sagepub.com/book/cluster-analysis.
Carter J, Stabile C, Seidel B, Baser RE, Gunn AR, Chi S, et al. Baseline characteristics and concerns of female cancer patients/survivors seeking treatment at a female sexual medicine program. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer. 2015;23(8):2255–65.
Perz J, Ussher JM, Gilbert E, Australian C, Sexuality Study T. Feeling well and talking about sex: psycho-social predictors of sexual functioning after cancer. BMC Cancer. 2014;14:228.
Rowlands IJ, Lee C, Beesley VL, Webb PM. Australian National Endometrial Cancer Study G. predictors of sexual well-being after endometrial cancer: results of a national self-report survey. Supportive Care in Cancer: official journal of the multinational association of. Support Care Cancer. 2014;22(10):2715–23.
Ussher PJ, Gilbert E. Women's sexuality after Cancer: a qualitative analysis of sexual changes and renegotiation. Women Ther. 2014;37:205–21.
Canzona MR, Fisher CL, Ledford CJW. Perpetuating the cycle of silence: the intersection of uncertainty and sexual health communication among couples after breast cancer treatment. Support Care Cancer. 2019;27(2):659–68.
Levin AO, Carpenter KM, Fowler JM, Brothers BM, Andersen BL, Maxwell GL. Sexual morbidity associated with poorer psychological adjustment among gynecological Cancer survivors. Int J Gynecol Cancer. 2010;20(3):461–70.
Bradford A, Fellman B, Urbauer D, Gallegos J, Meaders K, Tung C, et al. Assessment of sexual activity and dysfunction in medically underserved women with gynecologic cancers. Gynecol Oncol. 2015;139(1):134–40.
Badr H, Acitelli LK, Taylor CLC. Does talking about their relationship affect couples' marital and psychological adjustment to lung cancer? J Cancer Survivorship: Research and Practice. 2008;2(1):53–64.
Yu Y, Sherman KA. Communication avoidance, coping and psychological distress of women with breast cancer. J Behav Med. 2015;38(3):565–77.
Stephenson KR, Meston CM. When are sexual difficulties distressing for women? The selective protective value of intimate relationships. J Sex Med. 2010;7(11):3683–94.
Santos-Iglesias P, Mohamed B, Walker LM. A systematic review of sexual distress measures. J Sex Med. 2018;15(5):625–44.
Tevaarwerk A, Denlinger CS, Sanft T, Ansbaugh SM, Armenian S, Baker KS, et al. Survivorship, version 1.2021. J Natl Compr Cancer Netw. 2021;19(6):676–85.
Candy B, Jones L, Vickerstaff V, Tookman A, King M. Interventions for sexual dysfunction following treatments for cancer in women. The. Cochrane Database Syst Rev. 2016;2:CD005540.
Syme ML, Klonoff EA, Macera CA, Brodine SK. Predicting sexual decline and dissatisfaction among older adults: the role of partnered and individual physical and mental health factors. J Gerontol B Psychol Sci Soc Sci. 2013;68(3):323–32.
Carter J, Lacchetti C, Rowland JH. Interventions to address sexual problems in people with Cancer: American Society of Clinical Oncology clinical practice guideline adaptation summary. J Oncol Pract. 2018;14(3):173–9.
Acknowledgements
The authors would like to acknowledge Carl Brown for his assistance in manuscript preparation.
Funding
Funding for the original research study was provided in part by the Oncology Nursing Society Foundation Endowment 2017 ONS Foundation Dissertation Research Grant and by a Sigma Theta Tau International Epsilon Chapter Dissertation Grant. Data were collected in partial fulfillment of the requirements for a PhD in nursing.
Author information
Authors and Affiliations
Contributions
EA led the project, including conceptualization, methodology, data analysis, manuscript preparation and editing, and funding acquisition. UM contributed to conceptualization, manuscript review and editing, funding acquisition, and project supervision. JBR and KR contributed to manuscript review and editing. KB and JO contributed to project conceptualization, manuscript review and editing. CW contributed to project conceptualization, methodology, data analysis, manuscript review and editing, funding acquisition, and project supervision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The questionnaire and methodology for this study was approved by the Human Research Ethics committee of The Ohio State University (Ethics approval number for parent study: 2016B0341; for data repository: 2017B0139). All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Arthur, E.K., Menon, U., Reese, J.B. et al. Profiles of women’s adjustment after cancer based on sexual and psychosocial wellbeing: results of a cluster analysis. BMC Cancer 22, 1003 (2022). https://doi.org/10.1186/s12885-022-10093-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-10093-6