Abstract
Background
The modified nutritional geriatric risk index (mGNRI) was developed as a novel index and provides a more appropriate prognostic index than the original GNRI, which was reported to be a useful index for predicting prognoses for various malignancies. This study investigated the prognostic significance of the mGNRI compared with that of the GNRI in patients with pancreatic cancer and the association with psoas muscle volume (PMV) for survival outcomes.
Methods
This retrospective study included 137 patients who had undergone pancreatectomy for pancreatic cancer. The enrolled patients were grouped as high mGNRI (≥ 85.3) or low mGNRI (< 85.3), and high GNRI (≥ 92) or low GNRI (< 92) for prognostic analysis based on cutoff values. A propensity-matched analysis was performed in this study.
Results
The 5-year overall survival of patients in the high mGNRI group or high GNRI group was significantly longer than those in the low mGNRI group or low GNRI group. Statistically significant differences for the 5-year OS were observed in the three groups with respect to the combination of mGNRI and PMV. Patients with low mGNRI/low PMV had a worse 5-year OS rate compared with patients with high GNRI/high PMV or those with high GNRI or high PMV, but not both. The concordance index of the mGNRI to predict the 5-year overall survival was greater than that of the GNRI or the combination of the GNRI and PMV, but lower than that of the combination of the mGNRI and PMV. Multivariate analysis revealed that the mGNRI was an independent prognostic factor for patients with pancreatic cancer (P = 0.005).
Conclusions
The mGNRI might be a more useful prognostic factor than the GNRI for patients with pancreatic cancer, and might predict prognostic outcomes more accurately when combined with PMV.
Similar content being viewed by others
Background
The nutritional status and systemic inflammatory response of patients have a striking influence on the development and progression of cancer, and a negative correlation exists between nutrition status and inflammation. Among various nutritional indicators, the geriatric nutritional risk index (GNRI) consisting of serum albumin level, and patient height and body weight was originally developed to assess the risks of mortality and morbidity in older hospitalized patients [1]. However, in the last decade, the GNRI has gained attention as a simple nutritional indicator to predict the prognosis of patients with cancer and several studies with a cohort including not only older patients but also non-older patients reported that the GNRI was a useful prognostic factor in lung cancer, esophageal cancer, gastric cancer, and pancreatic cancer [2,3,4,5]. Furthermore, we previously investigated the relationship between the GNRI and psoas muscle volume (PMV) for survival outcomes in patients with pancreatic cancer because skeletal muscle wasting was closely associated with a poor prognosis in patients with cancer. We reported that the combination of the GNRI and PMV was more useful than the GNRI alone as a prognostic factor for patients with pancreatic cancer [6].
Recently, the modified GNRI (mGNRI) incorporating C-reactive protein (CRP), a well-known acute-phase reactant in inflammatory responses, instead of serum albumin was reported to be useful for the prediction of the early recurrence and prognosis in patients with esophageal cancer [7]. Additionally, they reported that the mGNRI was a more appropriate prognostic index than the GNRI or other nutritional or inflammatory markers in esophageal cancer. However, the prognostic influence of the mGNRI in patients with pancreatic cancer remains unclear.
Therefore, instead of the GNRI, this study evaluated the significance of the mGNRI alone as a prognostic factor and the relationship between the mGNRI and PMV for prognosis prediction in patients with pancreatic cancer using propensity score-matched analysis.
Methods
Patients
This study included 137 patients with histologically confirmed pancreatic ductal adenocarcinoma who had undergone pancreatectomy at our hospital between July 2005 and December 2019. The resectability status of patients enrolled in this study was resectable pancreatic cancer in 135 patients and borderline resectable pancreatic cancer in 2 patients. No patient had distant metastasis in this study. The clinicopathological findings of the patients were collected from their medical records. Histopathological findings, including tumor size, lymph node involvement, and histological differentiation were classified in accordance with the 8th edition of the International Union Against Cancer Tumor-Node-Metastasis classification system [8]. All patients in this study were of Japanese ethnicity.
Modified Geriatric Nutritional Risk Index and Geriatric Nutritional Risk Index
In accordance with a previous report, the mGNRI was calculated using the following formula: mGNRI = [14.89/CRP (mg/dL)] + [41.7 × actual body weight/ideal body weight]. The serum CRP level was set as 0.3 mg/dL when a patient’s serum CRP level was less than 0.3 mg/dL because the normal upper limit of serum CRP is 0.3 mg/dL [7].
The following formula reported by Bouillanne et al. was used to calculate the GNRI: GNRI = [14.89 × serum albumin level (g/dL)] + [41.7 × actual body weight/ideal body weight]. In accordance with their report, the cutoff value of GNRI in this study was set as 92 [1].
The values of preoperative serum CRP level, preoperative serum albumin level, and patient height and body weight obtained within 1 week prior to surgery were used in this study. The value of a patient’s actual body weight divided by the ideal body weight was set as 1 when the patient’s weight exceeded the ideal body weight [1].
Measurement and assessment of PMV
According to our previous report, the total PMV (mm3) for each patient was calculated by the analysis of preoperative computed tomography images using SYNAPSE VINCENT (Fujifilm, Tokyo, Japan). Then, it was divided by the height cubed (m3) to produce normalized PMV values (mm3/m3). The optimal cutoff values for PMV were set to 61.5 mm3/m3 for men and 44.1 mm3/m3 for women [6].
Statistical analysis
Chi-squared or Fisher’s exact probability tests for categorical variables, and the Mann–Whitney U-test for continuous variables were used to evaluate differences between two groups. A propensity score was estimated using a logistic regression model using the following covariates: age, sex, carbohydrate antigen 19–9 (CA19-9), tumor size, presence or absence of lymph node involvement, presence or absence of neoadjuvant chemotherapy, and presence or absence of adjuvant chemotherapy. Propensity score-matched analysis was performed with a caliper width of 0.25 multiplied by the standard deviation of values calculated by a logistic regression model. The 5-year overall survival (OS) curves were constructed using the Kaplan–Meier method, and differences between survival curves were examined by the log-rank test. Receiver operating characteristic analysis was used to determine the cutoff value of the mGNRI. The concordance index (C-index) was used to evaluate the mGNRI alone, the GNRI alone, and the combination of the mGNRI and PMV or GNRI and PMV to predict the 5-year OS. Univariate and multivariate analyses were performed using Cox proportional hazard regression models to determine factors with prognostic significance for OS. Variables with a P-value < 0.05 were included in the multivariate analysis. P-values less than 0.05 were considered statistically significant. All statistical analyses were performed using IBM SPSS Statistics for Windows (version 24; IBM, Armonk, NY, USA).
Results
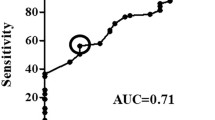
The median follow-up period in this study was 27.9 months (range: 1.7–177.4 months). The mean mGNRI of the patients in this study was 82.6 ± 14.2. The cutoff value of mGNRI was set at 85.3 using receiver operating characteristic curve analysis to predict the 5-year OS. Based on the cutoff value of mGNRI, the patients were divided into high mGNRI or low mGNRI groups.
Table 1 shows comparisons of the clinicopathological characteristics between the high mGNRI and low mGNRI groups before and after matching. After matching, 72 out of 137 enrolled patients remained. Significant correlations were observed between the high mGNRI group and low mGNRI group with respect to the body mass index, presence of lymph node involvement, preoperative albumin level, and preoperative lymphocyte count before matching, whereas no significant correlation was observed between the two groups with respect to the presence of lymph node involvement after matching.
The 5-year OS curves, stratified according to the mGNRI and GNRI before matching, are shown in Fig. 1a, b. The 5-year OS rate and median survival time (MST) were significantly higher in the high mGNRI group (38.7% and 41.1 months) compared with those in the low mGNRI group (16.1% and 16.4 months; P < 0.001, Fig. 1a). Regarding the GNRI, the 5-year OS rates in the high GNRI group were significantly higher than those in the low GNRI group (5-year OS rate: 35.9% vs 13.0%, MST: 39.3 months vs 14.8 months, respectively; P < 0.001, Fig. 1b). Similarly, after matching, the 5-year OS curves in the high mGNRI or high GNRI groups were significantly higher than those in the low mGNRI or low GNRI groups (mGNRI; P = 0.014, GNRI; P = 0.019, Fig. 2a, b). Furthermore, according to a combination of the mGNRI and PMV, we stratified the 72 patients into three groups after matching: A, patients with high mGNRI and high PMV (n = 25); B, patients with high mGNRI or high PMV (but not both) (n = 26); and C, patients with low mGNRI and low PMV (n = 21). We also stratified patients into three groups according to a combination of the GNRI and PMV: D, patients with high GNRI and high PMV (n = 36); E, patients with high GNRI or high PMV (but not both) (n = 24); and F, patients with low GNRI and low PMV (n = 12). Figure 3 shows the 5-year OS curves for the combination of mGNRI and PMV or the combination of GNRI and PMV. A statistically significant 5-year OS was observed for the three groups with respect to the combination of mGNRI and PMV (P = 0.003, Fig. 3a). However, for the combination of GNRI and PMV, the 5-year OS of patients in group D tended to be more favorable than that of patients in group E or F, although this did not reach statistical significance (P = 0.051, Fig. 3b). Figure 4 shows the C-index for the prediction of the 5-year OS of the mGNRI alone, GNRI alone, combination of mGNRI and PMV, and combination of GNRI and PMV using the area under the curve by ROC analysis. The C-index of mGNRI alone (0.620) was greater than that of GNRI alone (0.554) or the combination of GNRI and PMV (0.610). However, when mGNRI was combined with PMV, the C-index (0.652) was higher than that of mGNRI alone (0.620).
Overall survival curves in patients with pancreatic cancer compared between the combination of the mGNRI and PMV (a) and the combination of the GNRI and PMV (b) after matching. Group A, patients with high mGNRI/high PMV; group B, patients with high mGNRI or high PMV (but not both); group C, patients with low mGNRI/low PMV; Group D, patients with high GNRI/high PMV; group E, patients with high GNRI or high PMV (but not both); and group F, patients with low GNRI/low PMV. Abbreviations: mGNRI, modified geriatric nutritional risk index; PMV, psoas muscle volume; GNRI, geriatric nutritional risk index
After matching, multivariate analysis revealed that the mGNRI was an independent prognostic factor (hazard ratio [HR]: 2.359; 95% confidence interval [CI]: 1.291–4.311; P = 0.005), as well as sex (HR: 2.499; CI: 1.288–4.849; P = 0.007), lymph node metastasis (HR: 3.953; CI: 1.723–9.066; P = 0.001), and American Society of Anesthesiologists physical status (ASA-PS) (HR: 2.187; CI: 1.069–4.476; P = 0.032) in patients with resected pancreatic cancer (Table 2).
Discussion
This study demonstrated that mGNRI is a simple tool, which is superior to GNRI alone and the combination of GNRI and PMV for predicting the prognosis of patients with pancreatic cancer.
Pancreatic cancer patients with a low GNRI had significantly poorer prognostic outcomes than patients with high GNRI [2] [9]. Serum albumin, a protein used in clinical tests to assess nutritional condition, has been used to evaluate the morbidity and mortality of patients indicated for surgical treatment or as a prognostic predictive factor of various diseases including malignancies [10,11,12]. However, the American Society for Parenteral and Enteral Nutrition recently reported that serum albumin is an inflammatory marker associated with nutritional risk during nutritional assessments, and therefore, should not be used as a nutritional marker [13]. As an alternative, the GNRI is an inflammatory index, which was reported originally as a nutritional assessment tool. CRP is an acute protein involved in systemic inflammation, which can be also used as an indicator to predict survival in patients with cancer [14, 15]. A negative correlation was reported between the production of CRP and albumin, although both proteins are synthesized by hepatocytes [16, 17]. The mGNRI developed by Kouzu et al. is a novel prognostic index that uses inverse CRP instead of albumin, which is based on the reported negative correlation [7]. Furthermore, they suggested that the mGNRI was an independent prognostic factor for patients with esophageal cancer. However, the relationship between the mGNRI and prognostic outcomes in pancreatic cancer patients remains unclear. Therefore, the present study was conducted to evaluate the prognostic usefulness of the mGNRI compared with that of the GNRI in patients with pancreatic cancer. Our results found that patients with a high mGNRI had a significantly better prognosis than those with a low mGNRI and that the mGNRI was a predictive prognostic factor for patients with resected pancreatic cancer. Furthermore, the mGNRI was indicated to be more appropriate than the original GNRI when predicting the prognosis of patients with resected pancreatic cancer.
Interleukin (IL)-6 and other proinflammatory cytokines, including tumor necrosis factor, are released by inflammatory cells in the tumor microenvironment in response to tissue necrosis and the presence of tumor cells [18]. These cytokines, especially IL-6, were also shown to promote tumorigenesis by regulating multiple signaling pathways related to apoptosis, proliferation, angiogenesis, invasiveness, and metastasis [19]. Moreover, the synthesis of CRP is promoted in hepatocytes via activation by IL-6. Subsequently, CRP returns to the tumor microenvironment and promotes the autocrine growth of malignant tumors as an opsonin [18]. Therefore, serum CRP levels in patients with cancer might represent the biological behavior of cancer tissues because of the close relationship between IL-6 and CRP. In contrast, the reduced synthesis of albumin in the liver of patients with cancer is caused by the combined effects of inflammation and non-inflammatory factors such as inadequate protein and caloric intake; therefore, albumin may not reflect cancer progression as accurately as CRP in patients with cancer. Indeed, in renal cell carcinoma, CRP had a higher area under the curve for predicting OS compared with albumin [20]. These findings support the results observed in the current study.
In addition, we found that the mGNRI alone was superior to the combination of GNRI and PMV for predicting the prognosis of patients with pancreatic cancer. Body composition should also be considered to have an important role in survival outcomes in patients with cancer. We previously demonstrated that a combination of the GNRI and PMV, which are nutritional markers with distinct origins, might better predict prognosis in older patients with pancreatic cancer compared with the GNRI or PMV alone [6]. This study included older patients and non-older patients, which might have influenced these results. However, the combined mGNRI with skeletal muscle is superior to the mGNRI alone for predicting survival outcomes in patients with pancreatic cancer. These results presume that the mGNRI is more sensitive than the GNRI when reflecting prognostic outcomes in patients with pancreatic cancer.
There were several limitations in this study. It was a retrospective study with a small population of patients of East Asian ethnicity, and therefore, the findings might be biased with limited generalizability. The cutoff value of the mGNRI in this study was set at 85.3 by ROC analysis. However, the optimal cutoff value in patients with pancreatic cancer remains unclear. A large prospective study involving individuals of various ethnicities is necessary to confirm our findings.
Conclusions
The mGNRI might be a more useful prognostic factor than the original GNRI in patients with pancreatic cancer. Furthermore, the combination of mGNRI and PMV is superior to the mGNRI alone with respect to predicting the prognosis of patients with pancreatic cancer.
Availability of data and materials
The datasets generated during and analyzed during the current study are not publicly available, because they contain information that could compromise the privacy of research participants, but they are available from the corresponding author on reasonable request.
Abbreviations
- GNRI:
-
Geriatric nutritional risk index
- mGNRI:
-
Modified geriatric nutritional risk index
- PMV:
-
Psoas muscle volume
- CRP:
-
C-reactive protein
- OS:
-
Overall survival
- RFS:
-
Recurrence-free survival
- C-index:
-
Concordance index
- MST:
-
Median survival time
- IL-6:
-
Interleukin-6
References
Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent JP, Nicolis I, et al. Geriatric nutritional risk index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. 2005;82(4):777–83.
Hu SP, Chen L, Lin CY, Lin WH, Fang FQ, Tu MY. The prognostic value of preoperative geriatric nutritional risk index in patients with pancreatic ductal adenocarcinoma. Cancer Manage Res. 2020;12:385–95.
Sugawara K, Yamashita H, Urabe M, Okumura Y, Yagi K, Aikou S, et al. Geriatric nutrition index influences survival outcomes in gastric carcinoma patients undergoing radical surgery. JPEN J Parenter Enteral Nutr. 2021;45(5):1042–51.
Takahashi M, Sowa T, Tokumasu H, Gomyoda T, Okada H, Ota S, et al. Comparison of three nutritional scoring systems for outcomes after complete resection of non-small cell lung cancer. J Thorac Cardiovasc Surg. 2021;162(4):1257-1268.e1253.
Yamana I, Takeno S, Shimaoka H, Yamashita K, Yamada T, Shiwaku H, et al. Geriatric nutritional risk index as a prognostic factor in patients with esophageal squamous cell carcinoma -retrospective cohort study. Int J Surg. 2018;56:44–8.
Sakamoto T, Yagyu T, Uchinaka E, Miyatani K, Hanaki T, Kihara K, et al. The prognostic significance of combined geriatric nutritional risk index and psoas muscle volume in older patients with pancreatic cancer. BMC Cancer. 2021;21(1):342.
Kouzu K, Tsujimoto H, Sugasawa H, Ishibashi Y, Hase K, Kishi Y, et al. Modified geriatric nutrition risk index as a prognostic predictor of esophageal cancer. Esophagus. 2021;18(2):278–87.
Brierley JD, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumours. Hoboken: Wiley; 2017.
Koga F, Kawaguchi Y, Shimokawa M, Murayama K, Nakashita S, Oza N, et al. Gemcitabine plus nab-paclitaxel in older patients with metastatic pancreatic cancer: A post-hoc analysis of the real-world data of a multicenter study (the NAPOLEON study). J Geriatr Oncol. 2022;13(1):82–7.
Akirov A, Gorshtein A, Adler-Cohen C, Steinmetz T, Shochat T, Shimon I. Low serum albumin levels predict short- and long-term mortality risk in patients hospitalised to general surgery wards. Intern Med J. 2020;50(8):977–84.
Arques S. Human serum albumin in cardiovascular diseases. Eur J Intern Med. 2018;52:8–12.
Gupta D, Lis CG. Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr J. 2010;9:69.
Evans DC, Corkins MR, Malone A, Miller S, Mogensen KM, Guenter P, et al. The use of visceral proteins as nutrition markers: An ASPEN position paper. Nutr Clin Pract. 2021;36(1):22–8.
Allin KH, Nordestgaard BG. Elevated C-reactive protein in the diagnosis, prognosis, and cause of cancer. Crit Rev Clin Lab Sci. 2011;48(4):155–70.
Shrotriya S, Walsh D, Bennani-Baiti N, Thomas S, Lorton C. C-reactive protein is an important biomarker for prognosis tumor recurrence and treatment response in adult solid tumors: A systematic review. PLoS ONE. 2015;10(12):e0143080.
Lin H, Fan Y, Wieser A, Zhang J, Regel I, Nieß H, et al. Albumin might attenuate bacteria-induced damage on kupffer cells for patients with chronic liver disease. Cells. 2021;10(9):2298.
Sheinenzon A, Shehadeh M, Michelis R, Shaoul E, Ronen O. Serum albumin levels and inflammation. Int J Biol Macromol. 2021;184:857–62.
Groblewska M, Mroczko B, Sosnowska D, Szmitkowski M. Interleukin 6 and C-reactive protein in esophageal cancer Clinica chimica acta; Inte J Clin Chemi. 2012;413((19 20)):1583–90.
Kumari N, Dwarakanath BS, Das A, Bhatt AN. Role of interleukin-6 in cancer progression and therapeutic resistance. Tumour Biol : Journal Int Soc Oncodev Biol Med. 2016;37(9):11553–72.
Mountzias A, Hultdin J, Hlodan J, Kröger Dahlin BI, Johansson M, Ljungberg B. Inflammatory response markers and survival prediction in patients with renal cell carcinoma. Scand J Urol. 2022;56(1):47–52. https://doi.org/10.1080/21681805.2021.1983016.
Acknowledgements
We thank J. Ludovic Croxford, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Funding
There was no funding source.
Author information
Authors and Affiliations
Contributions
Study conception: T. Sakamoto; study design: T. Sakamoto; data acquisition: T. Sunaguchi, K. Goto; quality control of data and algorithms: T. Hanaki and K. Kihara; data analysis and interpretation: T. Sakamoto and K. Miyatani; statistical analysis: M. Morimoto, Y. Murakami, and Y. Shishido; manuscript preparation: T. Sakamoto; manuscript editing: T. Matsunaga, M. Yamamoto, and N. Tokuyasu; manuscript review: Y. Fujiwara; final approval of the article: all authors. read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional review board of ethics committee and national research committee with the 1964 Helsinki declaration and its later amendments. The Tottori University Hospital Ethics Committee approved this study (No. 21A125) and informed consent was waived by the Tottori University Hospital Ethics Committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sakamoto, T., Sunaguchi, T., Goto, K. et al. Modified geriatric nutritional risk index in patients with pancreatic cancer: a propensity score-matched analysis. BMC Cancer 22, 974 (2022). https://doi.org/10.1186/s12885-022-10071-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-10071-y