Abstract
Background
Breast cancer screening and improving imaging techniques have led to an increase in the detection rate of early, nonpalpable breast cancers. For early breast cancer, breast conserving surgery is an effective and safe treatment. Accurate intraoperative lesion localization during breast conserving surgery is essential for adequate surgical margins while sparing surrounding healthy tissue to achieve optimal cosmesis. Preoperative wire localization and radioactive seed localization are accepted standard methods to guide surgical excision of nonpalpable breast lesions. However, these techniques present significant limitations. Radiofrequency identification (RFID) technology offers a new, nonradioactive method for localizing nonpalpable breast lesions in patients undergoing breast conserving surgery. This study aims to evaluate the feasibility of RFID surgical guidance for nonpalpable breast lesions.
Methods
This multicenter prospective cohort study was approved by the Institutional Review Board of the University Medical Center Utrecht. Written informed consent is obtained from all participants. Women with nonpalpable, histologically proven in situ or invasive breast cancer, who can undergo breast conserving surgery with RFID localization are considered eligible for participation. An RFID tag is placed under ultrasound guidance, up to 30 days preoperatively. The surgeon localizes the RFID tag with a radiofrequency reader that provides audible and visual real-time surgical guidance.
The primary study outcome is the percentage of irradical excisions and reexcision rate, which will be compared to standards of the National Breast Cancer Organisation Netherlands (NABON)(≤ 15% irradical excisions of invasive carcinomas). Secondary outcomes include user acceptability/experiences, learning curve, duration and ease of the placement- and surgical procedure and adverse events.
Discussion
This study evaluates the feasibility of RFID surgical guidance for nonpalpable breast lesions. Results may have implications for the future localization techniques in women with nonpalpable breast cancer undergoing breast conserving surgery.
Trial registration
Netherlands National Trial Register, NL8019, registered on September 12th 2019.
Similar content being viewed by others
Background
Breast cancer screening and improving imaging techniques lead to an increase in the detection rate of early, nonpalpable breast cancers [1]. For early breast cancer, breast conserving surgery is an effective and safe treatment [2]. Accurate intraoperative lesion localization during breast conserving surgery is essential for adequate surgical margins while sparing surrounding healthy tissue to achieve optimal cosmesis.
Various lesion localization methods are currently used. Preoperative wire placement under image guidance was first described in 1965 by Dodd and has been the standard localization method since [3,4,5]. This technique requires careful logistical planning as the wire needs to be placed on the day of surgery, which can lead to significant workflow inefficiencies and operative delays. Furthermore, there is little time left for the surgeon to evaluate the imaging after wire placement and to communicate with the radiologist. The wire entry site may differ from the ideal surgical approach. Other disadvantages of wire localization are the risk of migration or dislodgement and patient anxiety caused by the wire protruding from the patient’s skin.
Radioactive I-125 seed localization was designed to overcome these limitations and has shown non-inferiority to wire localization in surgical outcomes including surgical margins, reexcision and reoperation rates, specimen size and cosmetic result [4, 6, 7]. However, the use of radioactive seeds is constrained by stringent nuclear regulatory issues. Obtaining and maintaining proper licensing and meticulous tracking of the radioactive seed is mandatory. These regulatory disadvantages have limited the widespread adoption of this technique and have prompted research and development of nonradioactive, non-wire localization methods [8,9,10].
Radiofrequency identification (RFID) technology may offer an alternative method for localizing nonpalpable breast lesion in patients undergoing breast surgery. The RFID system consists of a RFID tag and a handheld reader. The RFID tag contains a microchip with a unique identification number and an antenna that responds to the radiofrequency signal send by the reader. The tag alters and reemits the signal to the reader, which responds with an audio signal and displays the tag’s unique identification number and the distance to the nearest end of the tag. The audible and visual feedback provide the surgeon with real-time guidance during the excision procedure.
Although data on the use of RFID localization is limited, resulting from a proof-of-concept study [11], some small, single-center cohort studies [12,13,14,15], and one retrospective cohort analysis [16], all authors conclude that RFID tags are safe and effective in localizing nonpalpable breast lesions. Further clinical research in a prospective multicenter cohort is necessary to substantiate these first reports. Therefore, the RFID Localizer 1 Trial aims to evaluate the feasibility of RFID surgical guidance for nonpalpable breast lesions in a prospective multicenter cohort study.
Methods and analysis
Study design and setting
This prospective multicenter cohort study was designed to evaluate feasibility of RFID surgical guidance for nonpalpable breast lesions in two non-academic hospitals that acted as early adopters of RFID localization. The standard localization technique was wire-localizaton in one hospital and radioactive I-125 seed localization in the other. The primary study outcome is the percentage of irradical excisions and reexcision rate. Secondary outcomes include user acceptability/experiences, learning curve, duration and ease of the placement- and surgical procedure and adverse events.
Study population and recruitment
Women, ≥ 18 years of age, with nonpalpable, histologically proven in situ or invasive breast cancer, who can undergo breast conserving surgery with RFID localization are considered eligible for participation (Table 1). All cancer subtypes may be included, provided that the lesion is visible on ultrasound imaging to enable RFID placement procedure under ultrasound guidance. Women with a lesion located deeper than 7 cm from the skin when lying supine cannot undergo RFID localization due to the maximum reach of the RFID reader of 7 cm. Women who are pregnant or lactating, women with multicentric breast cancer and women who are unable to understand and sign the study specific informed consent form after the nature of the study has been fully explained are excluded.
In participating centers with access to I-125 seed localization, patients undergoing neoadjuvant treatment will be excluded because in these patients a single procedure using I-125 seed is preferred over two procedures (using a marker during neoadjuvant treatment followed by preoperative RFID tag placement). Study participants are recruited from the surgical outpatient clinic of the participating hospitals. Eligibility criteria are assessed during multidisciplinary meetings. Patient characteristics, including breast cup size, are recorded. Written informed consent is obtained from all study participants.
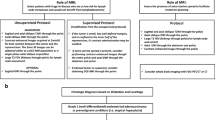
Study procedures (Fig. 1)
Preoperative placement of an RFID tag is performed by an experienced breast radiologist, using ultrasound guidance, up to 30 days prior to surgery. The passive RFID tag is composed of a coil and a microchip that stores a unique identification number. The RFID tag is approximately 11 mm long and 2 mm in diameter. A polypropylene cap prevents migration in tissue. The RFID tag is inserted percutaneously through a small skin incision with a preloaded 12-gauge sterile needle applicator after injection of a local anaesthetic (lidocaine 2%). In tumors > 1 cm the RFID tag is placed intralesional, in lesions ≤ 1 cm the RFID tag is placed directly next to the tumor. The VAS pain score of the patient is recorded. A 2-view mammography (CC and MLO) is obtained to confirm correct position of the RFID tag. Successful placement is recorded, which is defined as 0-5 mm distance between any point of the tag to any point of the tumor measured on the post-placement imaging. Directly after the placement procedure the radiologist completes a questionnaire on the duration and ease of the procedure (Table 2).
All surgical procedures are performed by an experienced oncology breast surgeon or an experienced surgical resident under direct supervision. At breast conserving surgery the surgeon localizes the RFID tag using the handheld, portable, battery-operated reader device (Fig. 2). The reader is bagged in a sterile drape for use in the sterile field. The reader has a loop probe with a detection range of up to 7 cm, and an attachable single-use sterile pencil probe (8 mm tip diameter) with a detection range up to 3.5 cm, intended for highly specific localization. The reader provides an audible signal that increases in pitch and volume when the probe is moved closer to the RFID tag. The reader also displays the distance from the probe to the tag in millimeters and the unique identification number of the RFID tag. The audible and visual feedback provide precise, real-time guidance during the excision procedure. Specimen radiography is performed to confirm successful retrieval of the RFID tag. Directly following the surgical procedure the surgeon completes a questionnaire on the duration and ease of the procedure.
RFID LOCalizer system (Hologic). The RFID LOCalizer system (Hologic) consists of a preloaded 12-gauge sterile needle applicator (A) containing the RFID tag (B), a handheld, portable, battery-operated reader device (C) with a loop probe with a detection up to 7 cm of depth (D), and an attachable sterile pencil probe with a detection range up to 3.5 cm (E)
Histopathological analysis is performed following routine standard of care, including assessment of surgical margins. Surgical margins are classified as radical, focally irradical and irradical according to the Dutch breast cancer guideline [17] (Fig. 3). Irradical excision and indication for reexcision is recorded.
Classification of surgical margins [17]. Radical excision is defined as no tumor at inked cut edges in an adequately processed specimen. Focally irradical excision is defined as one limited area (≤ 4 mm) of tumor (invasive carcinoma and/or DCIS) at inked cut edges. Irradical excision is defined as a larger area (> 4 mm) of tumor or multiple areas of tumor at inked cut edges [17]
Any adverse events potentially related to the RFID localization procedure, noted by the involved study radiologist, surgeon, pathologist, or other health care providers, are recorded. Post-operative wound infections, noted during post-operative follow-up visits as usual, are collected from the medical records 30 days after surgery by a study team member.
After completion of inclusion all users of the RFID localization system are invited to complete a questionnaire on system usability using the validated 10-item System Usability Scale [18]. All data is collected using Castor Electronic Data Capture.
Statistical analysis
Data will be analyzed using SPSS and RStudio. Descriptive statistical analysis will include the calculation of means, medians and interquartile ranges of the obtained data. The percentage of irradical excisions will be calculated by dividing the number of irradical excisions by the total number of excisions, with the corresponding 95% confidence interval (CI). The reexcision rate will be calculated by dividing the total number of reexcisions by the total number of excisions, with the corresponding 95% CI. Questionnaire data is evaluated using the five-level Likert scale.
Sample size considerations
We aim to include a minimum of 200 patients over a study period of one year. This sample size is based on the primary study outcome of the percentage of irradical excisions and reexcision rate, which will be compared to standards of the National Breast Cancer Organisation Netherlands (NABON). The NABON standards set a maximum of irradical excisions of invasive carcinomas at 15% [19]. Based on earlier data we expect that with a study population of 200 women, approximately 174 will have invasive breast cancer [19]. To show that with RFID surgical guidance the upper boundary of the 95% CI of the percentage of radical excisions does not exceed the NABON standard of 15%, with 174 cases of invasive breast cancer, a maximum percentage of irradical excisions of 9% in our study population is needed. Therefore, a sample size of 200 women is considered feasible and sufficient to show a statistically and clinically relevant outcome.
Discussion
The landscape of localization techniques is evolving fast in the search for the ideal method [4, 8,9,10]. Besides the RFID system, other novel, non-wire non-radioactive alternatives for lesion localization are under investigation, including SAVI SCOUT Radar localization and magnetic marker implantation (Magseed or MaMaLoc). Each technique comes with its own challenges.
The SAVI SCOUT system involves a 12-mm-long electromagnetic wave reflector that is activated by infrared light from a detector handpiece and a console that gives audible feedback to provide real-time guidance [20]. The magnetic resonance imaging (MRI) compatible radar reflector can be placed up to 5 cm in depth and up to 7 days before surgery using ultrasound or mammographic guidance. SAVI SCOUT is reported to be a reliable and effective alternative method but interaction with electrocautery can disrupt the signal or disable the reflector [21,22,23].
The Magseed system involves a 5-mm-long magnetic seed that can be placed up to 30 days preoperatively using ultrasound or mammographic guidance [24]. The Magnetic Marker Localization (MaMaLoc) is an experimental 3.5-mm-long magnetic marker [25]. The main challenge of using magnetic markers is the interference of metal surgical instruments with the detection of the marker, necessitating the use of special nonferromagnetic instruments. Magnetic marker localization is reported to be a reliable, effective and safe non-radioactive alternative to current localization techniques [24,25,26,27].
For both the SAVI scout and magnetic marker localization, as well as the RFID system, a downside is the need for two localization systems (two probes and two consoles) for breast conserving surgery requiring sentinel lymph node biopsy. This leads to a fuller operation field and requires the surgeon to switch between two techniques. Future registration for the use of novel localization methods in the axilla could resolve this. Further innovation should also focus on longer-term marker placement in patients undergoing neoadjuvant treatment. The current limited term that nonradioactive non-wire devices may be in place complicates its use in patients undergoing neoadjuvant treatment. In addition, the significant signal void artifacts on MRI from magnetic markers and RFID tags make response assessment on MRI virtually impossible (Supplemental material 1).
In conclusion, the field of localization techniques for nonpalpable breast lesions is moving fast and further research on novel approaches is essential to determine which are the localization techniques of the future. The RFID Localizer I trial will evaluate the feasibility of RFID surgical guidance for nonpalpable breast lesions in a prospective multicenter cohort study. Results may impact the future of localization techniques for nonpalpable breast cancer.
Availability of data and materials
The datasets generated during the study will be available from the authors on reasonable request.
Abbreviations
- CC:
-
Craniocaudal
- CI:
-
Confidence Interval
- MLO:
-
Mediolateral Oblique
- MRI:
-
Magnetic Resonance Imaging
- NABON:
-
Nationaal Borstkanker Overleg Nederland, National Breast Cancer Organisation Netherlands
- RFID:
-
Radiofrequency Identification
References
Welch HG, Prorok PC, O’Malley AJ, Kramer BS. Breast-cancer tumor size, overdiagnosis, and mammography screening effectiveness. N Engl J Med. 2016;375(15):1438–47.
Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002;347(16):1227–32.
Jensen SR, Luttenegger TJ. Wire localization of nonpalpable breast lesions. Radiology. 1979;132(2):484–5.
Chan BK, Wiseberg-Firtell JA, Jois RH, Jensen K, Audisio RA. Localization techniques for guided surgical excision of non-palpable breast lesions. Cochrane Database Syst Rev. 2015;12:CD009206.
G. D, K. F, W. D. Pre-operative localization of occult carcinoma of the breast. Nealon TF Management of the patient with cancer Philadelphia: WB Saunders Co;. 1965;88–113.
Stelle L, Schoenheit T, Brubaker A, Tang X, Qu P, Cradock K, et al. Radioactive seed localization versus wire localization for nonpalpable breast lesions: a two-year initial experience at a large community hospital. Ann Surg Oncol. 2018;25(1):131–6.
Xu XJ, Li JJ, Ji WB. An updated meta-analysis of radioactive seed localization versus wire-guided localization in the treatment of nonpalpable breast lesions. Breast J. 2018;24(4):673–5.
Hayes MK. Update on preoperative breast localization. Radiol Clin North Am. 2017;55(3):591–603.
Jeffries DO, Dossett LA, Jorns JM. Localization for breast surgery: the next generation. Arch Pathol Lab Med. 2017;141(10):1324–9.
Gunn JMS. Current trends in localization techniques for non-palpable breast lesions: making the invisible visible. Curr Breast Cancer Rep. 2017;9:165–71.
Reicher JJ, Reicher MA, Thomas M, Petcavich R. Radiofrequency identification tags for preoperative tumor localization: proof of concept. AJR Am J Roentgenol. 2008;191(5):1359–65.
Dauphine C, Reicher JJ, Reicher MA, Gondusky C, Khalkhali I, Kim M. A prospective clinical study to evaluate the safety and performance of wireless localization of nonpalpable breast lesions using radiofrequency identification technology. AJR Am J Roentgenol. 2015;204(6):W720–3.
DiNome ML, Kusske AM, Attai DJ, Fischer CP, Hoyt AC. Microchipping the breast: an effective new technology for localizing non-palpable breast lesions for surgery. Breast Cancer Res Treat. 2019;175(1):165–70.
Malter W, Holtschmidt J, Thangarajah F, Mallmann P, Krug B, Warm M, et al. First reported use of the Faxitron LOCalizer Radiofrequency Identification (RFID) System in Europe - A feasibility trial, surgical guide and review for non-palpable breast lesions. In Vivo. 2019;33(5):1559–64.
Wazir U, Tayeh S, Perry N, Michell M, Malhotra A, Mokbel K. Wireless breast localization using radio-frequency identification tags: the first reported European experience in breast cancer. In Vivo. 2020;34(1):233–8.
McGugin C, Spivey T, Coopey S, Smith B, Kelly B, Gadd M, et al. Radiofrequency identification tag localization is comparable to wire localization for non-palpable breast lesions. Breast Cancer Res Treat. 2019;177(3):735–9.
Richtlijn Borstkanker. https://www.oncoline.nl/mammacarcinoom: Nationaal Borstkanker Overleg Nederland; 2018.
Brooke J. SUS - A quick and dirty usability scale. London: Usability evaluation in industry. Taylor & Francis; 1996. p. 189–94.
DICA. NABON Breast Cancer Audit Year Report 2017. 2018.
Cox CE, Garcia-Henriquez N, Glancy MJ, Whitworth P, Cox JM, Themar-Geck M, et al. Pilot study of a new nonradioactive surgical guidance technology for locating nonpalpable breast lesions. Ann Surg Oncol. 2016;23(6):1824–30.
Cox CE, Russell S, Prowler V, Carter E, Beard A, Mehindru A, et al. A prospective, single arm, multi-site, clinical evaluation of a nonradioactive surgical guidance technology for the location of nonpalpable breast lesions during excision. Ann Surg Oncol. 2016;23(10):3168–74.
Falcon S, Weinfurtner RJ, Mooney B, Niell BL. SAVI SCOUT(R) localization of breast lesions as a practical alternative to wires: outcomes and suggestions for trouble-shooting. Clin Imaging. 2018;52:280–6.
Srour MK, Kim S, Amersi F, Giuliano AE, Chung A. Comparison of wire localization, radioactive seed, and Savi scout((R)) radar for management of surgical breast disease. Breast J. 2020;26(3):406–13. https://doi.org/10.1111/tbj.13499. Epub 2019 Aug 25.
Harvey JR, Lim Y, Murphy J, Howe M, Morris J, Goyal A, et al. Safety and feasibility of breast lesion localization using magnetic seeds (Magseed): a multi-centre, open-label cohort study. Breast Cancer Res Treat. 2018;169(3):531–6.
Schermers B, van der Hage JA, Loo CE, Vrancken Peeters M, Winter-Warnars HAO, van Duijnhoven F, et al. Feasibility of magnetic marker localisation for non-palpable breast cancer. Breast. 2017;33:50–6.
Zacharioudakis K, Down S, Bholah Z, Lee S, Khan T, Maxwell AJ, et al. Is the future magnetic? Magseed localisation for non palpable breast cancer. A multi-centre non randomised control study. Eur J Surg Oncol. 2019;45(11):2016–21.
Price ER, Khoury AL, Esserman LJ, Joe BN, Alvarado MD. Initial Clinical experience with an inducible magnetic seed system for preoperative breast lesion localization. AJR Am J Roentgenol. 2018;210(4):913–7.
Acknowledgements
The authors acknowledge the contribution of H.M. Verkooijen in the first phase of study design.
Funding
This work was supported by Hologic, grant number 1257. Hologic is not involved in the design of the study and collection, analysis, interpretation of data, writing the manuscript and in the decision to publish study results.
Author information
Authors and Affiliations
Contributions
BMD, AC, TD, LMJ, MS, AD and RMP were involved in the study design. BMD and AC drafted the manuscript, TD, LMJ, MS AD and RMP revised the manuscript. All authors have read and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board of the University Medical Center Utrecht. Written informed consent is obtained from all participants. The RFID Localizer 1 Trial is conducted in accordance with the Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects (Fortaleza, Brazil, October 2013).
Consent for publication
Written informed consent was obtained for publication of individual person’s imaging.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
den Dekker, B.M., Christenhusz, A., van Dalen, T. et al. A multicenter prospective cohort study to evaluate feasibility of radio-frequency identification surgical guidance for nonpalpable breast lesions: design and rationale of the RFID Localizer 1 Trial. BMC Cancer 22, 305 (2022). https://doi.org/10.1186/s12885-022-09394-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-09394-7