Abstract
Background
Long-term prospective patient-reported outcomes (PRO) after breast cancer adjuvant radiotherapy is scarce. TomoBreast compared conventional radiotherapy (CR) with tomotherapy (TT), on the hypothesis that TT might reduce lung-heart toxicity.
Methods
Among 123 women consenting to participate, 64 were randomized to CR, 59 to TT. CR delivered 50 Gy in 25 fractions/5 weeks to breast/chest wall and regional nodes if node-positive, with a sequential boost (16 Gy/8 fractions/1.6 weeks) after lumpectomy. TT delivered 42 Gy/15 fractions/3 weeks to breast/chest wall and regional nodes if node-positive, 51 Gy simultaneous-integrated-boost in patients with lumpectomy. PRO were assessed using the European Organization for Research and Treatment of Cancer questionnaire QLQ-C30. PRO scores were converted into a symptom-free scale, 100 indicating a fully symptom-free score, 0 indicating total loss of freedom from symptom. Changes of PRO over time were analyzed using the linear mixed-effect model. Survival analysis computed time to > 10% PRO-deterioration. A post-hoc cardiorespiratory outcome was defined as deterioration in any of dyspnea, fatigue, physical functioning, or pain.
Results
At 10.4 years median follow-up, patients returned on average 9 questionnaires/patient, providing a total of 1139 PRO records. Item completeness was 96.6%. Missingness did not differ between the randomization arms. The PRO at baseline were below the nominal 100% symptom-free score, notably the mean fatigue-free score was 64.8% vs. 69.6%, pain-free was 75.4% vs. 75.3%, and dyspnea-free was 84.8% vs. 88.5%, in the TT vs. CR arm, respectively, although the differences were not significant. By mixed-effect modeling on early ≤2 years assessment, all three scores deteriorated, significantly for fatigue, P ≤ 0.01, without effect of randomization arm. By modeling on late assessment beyond 2 years, TT versus CR was not significantly associated with changes of fatigue-free or pain-free scores but was associated with a significant 8.9% improvement of freedom from dyspnea, P = 0.035. By survival analysis of the time to PRO deterioration, TT improved 10-year survival free of cardiorespiratory deterioration from 66.9% with CR to 84.5% with TT, P = 0.029.
Conclusion
Modern radiation therapy can significantly improve long-term PRO.
Trial registration
Trial registration number ClinicalTrials.govNCT00459628, April 12, 2007 prospectively.
Similar content being viewed by others
Background
Breast cancer is the most common cancer among women worldwide, and the second most frequent cause of cancer death in more developed regions [1]. It is a major contributor to the high overall cancer disability-adjusted life-years in very high Human Development Index countries, with quite a large contribution of years spent with a disability [2]. Radiotherapy improves tumor control and survival in breast cancer [3, 4]. With improved survival, quality of life (QOL) is becoming increasingly important. Treatment toxicities adversely affect QOL, and radiation therapy has been specifically associated with increased risks of heart disease and radiation pneumonitis [5]. As radiation techniques evolve continuously [6], there is need to evaluate whether breast cancer patients can benefit from new technologies.
Tomotherapy is a treatment system which provides intensity modulated and volumetric image guidance radiation therapy (IMRT-IGRT) [7, 8]. The irradiation is delivered helicoidally providing highly conformal shaping of dose distribution. Integrated imaging improves the accuracy of the treatment, allowing to treat tumors yet sparing critical structures. TomoBreast is a randomized clinical trial that investigates whether the technical advantage of tomotherapy translates into a substantial reduction of pulmonary and cardiac toxicities, as compared with conventional radiotherapy [9]. Previous reports of the trial have shown that tomotherapy improved the homogeneity of the dose to targets, decreased the dose to the heart and ipsilateral lung, and reduced the pooled all-grades lung-heart toxicity [10]. Subsequent analyses of the trial’s data established that lung function declined during the initial 3 months more markedly in the conventional radiotherapy arm and continued to decline thereafter [11]. Thus, at the very least, the trial already showed that lung toxicity is detectable early on and is affected by the choice of radiation technique. Previous preliminary analysis of the trial’s QOL data at 2 years further suggested an improvement of global health status and faster recovery from fatigue with tomotherapy [12]. With continued follow-up that reached 10 years, the present study seeks to assess the long-term impact of the trial on respiratory-related patient-reported outcomes (PRO).
Methods
Study design and patients
TomoBreast is a single center phase III randomized controlled trial comparing accelerated adjuvant radiotherapy with the tomotherapy system (TT), versus conventional post-surgery radiotherapy (CR) for breast cancer. The trial was conducted in 2007–2011 at the Universitair Ziekenhuis Brussel (UZ Brussel), Belgium. The trial tested the hypothesis that TT treatment, as compared with CR, could substantially reduce the incidence of pulmonary and cardiac toxicities (primary outcome), without increase of recurrences (secondary outcome). Pulmonary and cardiac toxicities were to be assessed by medical imaging and functional tests. Medical imaging was not implemented for lack of funding. Functional assessment was implemented under the form of five parallel modules: 1) echocardiographic evaluation under cardiologist guidance [13]; 2) pulmonary function test managed by the pneumology department [11]; 3) shoulder-arm physical evaluation managed by the physiotherapy unit [14]; 4) oncologist’s recording of clinical toxicities using the Late Effects Normal Tissues - Subjective, Objective, Management, Analytic (LENT-SOMA), and the Radiation Therapy Oncology Group (RTOG) scores [15]; and 5) patient-reported outcomes (PRO) as will be detailed in the next section. Analyses of the echocardiography, pulmonary function, physical evaluation, and clinician’s assessed toxicities limited to five-years curated data are on-going. The present study assesses exclusively the cardiopulmonary-related PRO extending over 10 years.
Eligible patients were women ≥18 years old with histologically proven stage I or II (T1-3N0 or T1-2N1 M0) invasive breast carcinoma [16], who had surgery (lumpectomy or mastectomy) with clear resection margins. Exclusion criteria were prior breast or thoracic radiotherapy, pregnancy, lactation, psychiatric or addictive disorders, and fertile patients without effective contraception. Patients who gave written informed consent were randomized to either CR (control arm), or TT (experimental arm). CR used the UZ-Brussel standard procedure of tangential chest fields, with an additional supraclavicular field in the case of nodal involvement, with a dose-fractionation of 50 Gy in 25 fractions/5 weeks, and a sequential electron boost of 16 Gy in 8 fractions/2 weeks in the case of breast-conserving surgery. CR planning used forward field-in-field intensity-modulated radiation treatment. TT used the Tomotherapy system. Target areas (breast for conservative surgery, thorax wall for mastectomy, plus nodal areas in node-positive patients) were treated with a dose-fractionation of 42 Gy in 15 fractions/3 weeks, and with a simultaneous integrated boost of 0.6 Gy/fraction in the case of breast-conserving surgery. TT-planning used the procedure “Tomo supine” for helical tomotherapy [17].
The study size required a minimum of 118 patients, computed on the hypothesis that TT would reduce the incidence of lung-heart any-grade toxicity from 25% with CR to 5% with TT, by two-sided testing with a power of 0.80 at a significance level of 0.05. Randomization was balanced by nodal status, type of surgery, and chemotherapy sequence using Efron’s biased coin method [18]. The randomization was conducted by a data manager independently of the clinicians. The patients and the clinical staff were not blinded to the allocation but had no influence on the random drawing process.
QOL assessments
PRO measures were assessed using the European Organization for Research and Treatment of Cancer (EORTC) core questionnaire (QLQ-C30). The breast module QLQ-BR23 was collected but not used in the present study. The present study retained the QLQ-C30’s five multi-item functional scales (physical, role, cognitive, emotional, and social), and three symptom scales (fatigue, pain, and dyspnea), as well as a global health scale [19]. The items were rated by patients using a seven-point response from 1 (“very poor”) to 7 (“excellent”) for global health status items #29 and #30, and a four-point response from 1 (“not at all”) to 4 (“very much”) for other items. The scale and item scores were linearly transformed to a 0–100 range. Functional and symptom scales were recoded such that a higher score represented a better level of functioning and symptom-free state. An overall summary measure labelled “C30 summary”, was also computed [20].
The Dutch or the French version of the QLQ-C30 printed questionnaire was used, in accordance with each patient’s preference. The questionnaires were collected before radiotherapy (baseline), at the last session of radiotherapy, at 1–3 months after completion of radiotherapy, and thereafter once yearly until February 2019.
Statistical analyses
The linear mixed effects model and specific PRO deterioration free survival were used for the PRO data analyses, as detailed below.
The linear mixed effects model fitted the PRO measures expressed as percent change from each patient’s baseline PRO. Time was modeled as a random effect and therapy as a fixed group effect. Coefficients were estimated through maximum likelihood [21]. The linear mixed effects were modeled on the full follow-up, then further modeled by period, early (assessments ≤2 years from randomization), and late (> 2 years from randomization).
Specific PRO survival estimates considered the time to event, in which event was defined as the degradation of a QOL scale to below 10% from baseline [22]. The 10% cutoff is analogous to the minimally important difference (MID) [23,24,25,26,27]. However, the data at hand was not used to determine a MID. The rationale is to apply a common cutoff applicable to future studies comparing the PRO to echocardiography and pulmonary function tests, taking into consideration that 10% change is concordant with the variable precision of these exams [13, 28]. The time-to-deterioration values for each individual patient were computed with the constraint that the linear regression of the patient’s QOL degradation over time should be significant at a 0.05 level. The patients were censored at the last follow-up time or at time of death. The Kaplan-Meier method and log-rank tests were applied [22]. In addition to the pre-defined QOL scales, a post-hoc “cardiorespiratory-related” composite event was defined as deterioration in any of the dyspnea, physical functioning, fatigue, and/or pain measures.
All analyses were done by intent-to-treat. No patient was excluded. Computations used R version 3.5.2 [29]. The specific R packages and functions used were: “tableone” for tables’ layout, using the Student’s t-test for the comparison of means and the chi-square test for the comparison of proportions; “PROscorerTools” for computation of the QOL scales; “survival” for the implementation of the Kaplan-Meier time-to-event analysis and the log-rank test [30]; the function “kmplot” for survival plot layout; and “lme4” for the linear mixed effects model [21]. Implementation of time-to-deterioration used an in-house script, available on request. Missing data were handled by listwise deletion.
Ethical statement
This trial complied fully with guidelines for Good Clinical Practice and the Declaration of Helsinki. Written informed consent was obtained from each patient. The trial was approved by the ethics committee of the Universitair Ziekenhuis Brussel (UZ-Brussel), and was registered on ClinicalTrials.gov, number NCT00459628.
Results
Baseline characteristics
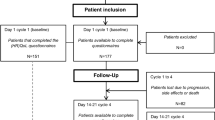
The trial, conducted at the UZ-Brussel, started in May 2007 and closed in July 2011 when the accrual was reached. A total of 123 women consented to participate (Fig. 1). Of these, 64 (52%) were randomized to CR and 59 (48%) to TT. Of the 64 patients allocated to CR, 2 received TT by request. Of the 59 patients allocated to TT, 3 received CR, 1 because of an appointment scheduling error, 2 because tomotherapy was unsuitable due to the patient’s body size exceeding the system’s limits.
The patients’ characteristics showed some imbalances between the two arms. There were non-significantly more smokers, more nodal disease, more concurrent chemo-radiation, and significantly more axillary lymph node dissection (P = 0.043), and HER2 overexpression and trastuzumab therapy (P = 0.055) in the TT group (Table 1).
As of February 4, 2020, the median follow-up of patients alive was 10.4 years. A total of 95 patients had no disease-related events and 28 had one or more events: 15 deaths, 1 local recurrence, 0 nodal recurrence, 14 metastases (either from a primary breast tumor or from a new primary tumor), and 13 new primary tumors. The locations of the new primary tumors were: 4 contralateral breast, of which 3 were invasive and 1 was non-invasive; 3 colorectal; 1 bladder; 1 kidney; 1 ovary; 1 lung; 1 skin basal cell carcinoma; and 1 skin basal cell and squamous cell carcinoma. The overall survival and the disease-free survival did not differ between the two groups, P = 0.971 and P = 0.569, respectively (Supplementary eFigure F1).
Completeness of assessments
The QOL questionnaires were continuously collected yearly. The patients returned on average 9 questionnaires (median = 10, inter-quartile range = 8–11). The time span covered by the collected questionnaires ranged from 0.5 to 11.3 years from randomization, averaging 8.1 years (median 8.5, inter-quartile range 7.2–9.9 years) (Supplementary eFigure F2). The overall percentage of missing items within the collected questionnaires was 3.4% and the rate of completed items was 96.6%. Number of questionnaires, follow-up duration, and pattern of missing data did not differ by randomization arm (Supplementary eFigure F3).
QOL outcomes
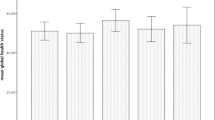
The patients presented with a deteriorated baseline QOL. The average score was below 100 by more than 10 points in all measures. The low baseline values –attributable to the post-surgery status– were comparable between the two randomization arms (Table 2).
Rapid improvement over the first 1–3 years was observed in almost all QOL measures, most notably in global health status, role and social functioning, fatigue, and pain (figure not shown). Most measures appeared to plateau thereafter.
Fitting the PRO with the linear mixed effects models showed an improvement with time in all measures (Supplementary eTable T2). In addition, tomotherapy as compared with conventional radiotherapy was associated with a trend towards lower rates of dyspnea (4.1%), P = 0.090. Modeling the mixed effects according to the early (≤2 years from randomization) and late (> 2 years from randomization) period of assessment showed that the largest improvements in PROs occurred early. Regarding the time effect, significant or nearly significant improvements were observed in the early period in global health status (P = 0.018), physical functioning (P = 0.091), role functioning (P = 0.001), social functioning (P = 0.004), and fatigue (P = 0.006) (Table 3, column Time Early effect). There were no significant time effects in the late period. Regarding the randomization group effect, tomotherapy was associated with a significantly poorer global health status in the early period (P = 0.032), but not in the late period. Better freedom from dyspnea was significantly associated with tomotherapy in the late period, P = 0.035 (Table 3, column TT Late effect). Tomotherapy was also associated with better cognitive functioning, P < 0.001 (Table 3, column TT Late effect).
Specific QOL deterioration free survival found a poorer survival free from dyspnea in the CR group as compared with TT, log-rank test P = 0.098 (Table 4). The 10–year dyspnea free survival estimate was 85.9% (95%CI: 77.7–94.9%) in the CR arm, as compared with 94.9% (89.5–100.0%) in the TT arm. Specific survival free from deterioration of the Global health status was significantly poorer in the CR group, 93.6% at 10 years, as compared with 100% in the TT arm, P = 0.052. Despite lack of significance in the other QOL scales, the survival plots showed moreover a trend of deterioration free survival in favor of TT, notably regarding Cognitive functioning, Social functioning, and Pain free (Fig. 2).
In the post-hoc analysis using the composite QOL outcome combining the pain measure with any of dyspnea, physical functioning, or fatigue scales, the specific survival free from deterioration in the composite outcome was significantly improved with TT arm, log-rank P = 0.029. Survival plot showed a clear separation in favor of TT (Fig. 3). The estimated 10-year survival free of deterioration was 84.5% (95%CI: 75.7–94.4%) in the TT arm, as compared with 66.9% (95%CI: 56.2–79.6%) in the CR arm.
Discussion
The improved long-term cardiorespiratory-related outcome in the tomotherapy arm is a key finding of the study, remarkably considering the high proportion of patients receiving concurrent chemotherapy and trastuzumab, and the high number of patients who were current or ex-smokers receiving lymph node irradiation. Previously, the diffusing capacity of the lung for carbon monoxide (DLCO) at 3 years was shown to be significantly better with tomotherapy [10, 31]. At 12 years follow-up, the respiratory-sparing effect of tomotherapy has been borne out through patient-reported outcome measures. These observations have an important implication: toxicity is detectable early, the impact can be long lasting, applying advanced radiotherapy techniques to spare the lungs and heart is of foremost concern.
Why should lung and heart toxicities be considered together, and why should fatigue and pain be included with dyspnea as cardiopulmonary outcomes? Both the lungs and heart are central to oxygen uptake and transport. Physical fitness requires an adequate supply of oxygen, which is dependent on a coordinated chain of processes that include ventilation, pulmonary blood flow, gas exchange, and cardiac output [32]. Disturbances in these processes due to cardiac or pulmonary impairment, aging, or disease, iatrogenic or not, could manifest as symptoms of decreased exercise tolerance, or increased fatigue and breathlessness [33]. Dyspnea is the most prevalent symptom among patients with cardiac and respiratory diseases [34]. However, dyspnea can be masked. Self-reported breathlessness can decrease with age, sensitivity to alteration of lung function can differ among patients, and the perception of dyspnea can be blunted in the course of respiratory and heart diseases [35].
Next to dyspnea, chest pain is a chief complaint in acute and long-term heart disease and is also common in patients with lung disease [36]. However, the chest is not the sole pain location. Non-chest pain is prevalent in patients with myocardial infarction and in heart failure [37] . Likewise, a high prevalence of bodily pain has been reported in chronic obstructive pulmonary disease [38].
TomoBreast used a composite lung and heart outcome in light of the trial size and the pragmatic consideration that cardiac events in modern radiotherapy are rare. The choice is validated by physiology, clinical pathology, and the well-documented overlap of cardiopulmonary symptoms. Furthermore, the combination of pain, fatigue, physical functioning, and dyspnea measures derived from the QLQ-C30 mirrors specific instruments for the measurement of lung and heart outcomes [39]. None of the symptoms is specific. Pain arising in a breast cancer can have many causes, not only from the breast, muscles, nerves, bone, but also from heart or lung. There is no specificity. Nevertheless, combined with other symptoms, the constellation improves the sensitivity to detect a substantial impact on patient quality of life. To our knowledge, this study is the first that explores the QLQ-C30 items in a cardiopulmonary perspective.
The study has limitations. The small number of patients allowed no subgroup analysis; neither by chemotherapy nor by regional nodal irradiation. Stratification did not consider trastuzumab treatment. The linear mixed models were not established in advance. The criteria of QOL deterioration were not prespecified. The study did not consider the precision of the QOL measurements. Single-item symptom scales were limited to a range of 1 to 4 possible responses. Conversion to a 0–100 range translates to only four possible values, 0, 33.3, 66.7, and 100, far from the precision implied by the need to detect 10% changes. Cardiopulmonary-related symptoms were not complemented with additional specific patient-reported lung or heart outcome measures such as cough and sputum, edema, palpitations, dizziness, or syncope. Tomotherapy patients reported less deterioration in measures of fatigue, pain, and dyspnea. We ascribe this to better lung-heart sparing. However, we cannot exclude that the favorable tomotherapy outcome could result from non-cardiopulmonary mechanisms.
Counterbalancing the limitations, the study argues against practice bounds to the development of breast radiotherapy. Conventional radiotherapy of the breast is still the preferred technique, advanced radiation is discouraged from reimbursement [9]. The present study is the counterpoint. It shows that an advanced technique can provide a meaningful long-term improvement in patient-reported outcomes.
The control arm and the experimental arm fractionation schedules differed, which might be perceived as a confounding weakness – if one discards all current evidence of large prospective randomized trials showing that moderate hypofractionation does not affect the outcome of breast cancer [40, 41]. Using normofractionation in the control arm maintained continuity with the majority of historic trials that demonstrated a survival advantage with breast radiotherapy [42]. Using hypofractionation in the experimental arm bridges with today’s practice. With hindsight, TomoBreast was designed against obsolescence of fractionation.
In summary, improved cardiorespiratory-related outcome in tomotherapy patients is a proof of concept that advanced radiation techniques can have a substantial clinical impact. The reduction of lung and heart toxicities is detectable early [31]. In the long-term, this translates into a significant advantage in patient self-reported outcome. Investing in lung/heart-sparing techniques do yield a benefit. Currently many approaches are available [43]. The challenge will be to choose the most cost-effective technique applicable to the largest number of patients.
Conclusions
Hypofractionated tomotherapy was associated with significantly better long-term survival-free from cardiorespiratory-related deterioration. The study is a proof of concept that patient-reported outcome might be improved using advanced radiation techniques.
Availability of data and materials
Data are available on request to Hilde Van Parijs, email Hilde.VanParijs@uzbrussel.be, and Vincent Vinh-Hung, email vh@onco.be. Protocol uploaded with manuscript.
Abbreviations
- CR:
-
control arm
- DLCO:
-
diffusing capacity of the lung for carbon monoxide
- EORTC:
-
European Organization for Research and Treatment of Cancer
- IMRT-IGRT:
-
intensity modulated and volumetric image guidance radiation therapy
- PRO:
-
patient-reported outcome
- QLQ-BR23:
-
breast module
- QLQ-C30:
-
core questionnaire
- QOL:
-
quality of life
- TT:
-
experimental arm
- UZ-Brussel:
-
Universitair Ziekenhuis Brussel
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–86. https://doi.org/10.1002/ijc.29210.
Ginsburg O, Bray F, Coleman MP, Vanderpuye V, Eniu A, Kotha SR, et al. The global burden of women's cancers: a grand challenge in global health. Lancet. 2017;389(10071):847–60. https://doi.org/10.1016/S0140-6736(16)31392-7.
Van de Steene J, Soete G, Storme G. Adjuvant radiotherapy for breast cancer significantly improves overall survival: the missing link. Radiother Oncol. 2000;55(3):263–72. https://doi.org/10.1016/S0167-8140(00)00204-8.
Vinh-Hung V, Verschraegen C. The breast conserving surgery project. Breast-conserving surgery with or without radiotherapy: pooled-analysis for risks of ipsilateral breast tumor recurrence and mortality. J Natl Cancer Inst. 2004;96(2):115–21. https://doi.org/10.1093/jnci/djh013.
Carver JR, Shapiro CL, Ng A, Jacobs L, Schwartz C, Virgo KS, et al. American Society of Clinical Oncology clinical evidence review on the ongoing care of adult cancer survivors: cardiac and pulmonary late effects. J Clin Oncol. 2007;25(25):3991–4008. https://doi.org/10.1200/JCO.2007.10.9777.
Verellen D, Ridder MD, Linthout N, Tournel K, Soete G, Storme G. Innovations in image-guided radiotherapy. Nat Rev Cancer. 2007;7(12):949–60. https://doi.org/10.1038/nrc2288.
Mackie TR, Kapatoes J, Ruchala K, Lu W, Wu C, Olivera G, et al. Image guidance for precise conformal radiotherapy. Int J Radiat Oncol Biol Phys. 2003;56(1):89–105. https://doi.org/10.1016/s0360-3016(03)00090-7.
Storme G, Verellen D, Soete G, Linthout N, Van De SJ, Voordeckers M, et al. From linac to tomotherapy: new possibilities for cure? AdvExpMedBiol. 2006;587:303–8. https://doi.org/10.1007/978-1-4020-5133-3_23.
Heymann S, Dipasquale G, Nguyen NP, San M, Gorobets O, Leduc N, et al. Two-level factorial pre-TomoBreast pilot study of Tomotherapy and conventional radiotherapy in breast cancer: post hoc utility of a mean absolute dose deviation penalty score. Technol Cancer Res Treat. 2020;19:1533033820947759. https://doi.org/10.1177/1533033820947759.
Van Parijs H, Miedema G, Vinh-Hung V, Verbanck S, Adriaenssens N, Kerkhove D, et al. Short course radiotherapy with simultaneous integrated boost for stage I-II breast cancer, early toxicities of a randomized clinical trial. Radiat Oncol. 2012;7(1). https://doi.org/10.1186/1748-717x-7-80.
Verbanck S, Hanon S, Schuermans D, Van Parijs H, Vinh-Hung V, Miedema G, et al. Mild lung restriction in breast cancer patients after hypofractionated and conventional radiation therapy: a 3-year follow-up. Int J Radiat Oncol Biol Phys. 2016;95(3):937–45. https://doi.org/10.1016/j.ijrobp.2016.02.008.
Versmessen H, Vinh-Hung V, Van Parijs H, Miedema G, Voordeckers M, Adriaenssens N, et al. Health-related quality of life in survivors of stage I-II breast cancer: randomized trial of post-operative conventional radiotherapy and hypofractionated tomotherapy. BMC Cancer. 2012;12(1). https://doi.org/10.1186/1471-2407-12-495.
Kerkhove D, Fontaine C, Droogmans S, De Greve J, Tanaka K, Van De Veire N, et al. How to monitor cardiac toxicity of chemotherapy: time is muscle! Heart. 2014;100(15):1208–17. https://doi.org/10.1136/heartjnl-2013-303815.
Adriaenssens N, Vinh-Hung V, Miedema G, Versmessen H, Lamote J, Vanhoeij M, et al. Early contralateral shoulder-arm morbidity in breast cancer patients enrolled in a randomized trial of post-surgery radiation therapy. Breast Cancer : Basic and Clinical Research. 2012;6:79–93. https://doi.org/10.4137/bcbcr.s9362.
Cox JD, Stetz J, Pajak TF. Toxicity criteria of the radiation therapy oncology group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995;31(5):1341–6. https://doi.org/10.1016/0360-3016(95)00060-C.
Sobin LH, Wittekind C. TNM classification of malignant Tumours. 6th ed. New-York: Wiley; 2002. https://doi.org/10.1002/0471463752.
Reynders T, Tournel K, De Coninck P, Heymann S, Vinh-Hung V, Van Parijs H, et al. Dosimetric assessment of static and helical TomoTherapy in the clinical implementation of breast cancer treatments. Radiother Oncol. 2009;93(1):71–9. https://doi.org/10.1016/j.radonc.2009.07.005.
Efron B. Forcing a sequential experiment to be balanced. Biometrika. 1971;58(3):403–17. https://doi.org/10.1093/biomet/58.3.403.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–76. https://doi.org/10.1093/jnci/85.5.365.
Giesinger JM, Kieffer JM, Fayers PM, Groenvold M, Petersen MA, Scott NW, et al. Replication and validation of higher order models demonstrated that a summary score for the EORTC QLQ-C30 is robust. J Clin Epidemiol. 2016;69:79–88. https://doi.org/10.1016/j.jclinepi.2015.08.007.
Bates D, Mächler M, Bolker B, Walker S. Fitting Linear Mixed-Effects Models Using lme4. J Stat Softw. 2015;67(1):48. https://doi.org/10.18637/jss.v067.i01.
Awad L, Zuber E, Mesbah M. Applying survival data methodology to analyze longitudinal quality of life data. In: Mesbah M, Cole BF, Lee M-LT, editors. Statistical methods for quality of life studies: design, measurements and analysis. Dordrecht: Springer Science+Business Media; 2002. p. 231–43. https://doi.org/10.1007/978-1-4757-3625-0_18.
King MT. The interpretation of scores from the EORTC quality of life questionnaire QLQ-C30. Qual Life Res. 1996;5(6):555–67. https://doi.org/10.1007/BF00439229.
Osoba D, Rodrigues G, Myles J, Zee B, Pater J. Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol. 1998;16(1):139–44. https://doi.org/10.1200/JCO.1998.16.1.139.
Schunemann HJ, Akl EA, Guyatt GH. Interpreting the results of patient reported outcome measures in clinical trials: the clinician's perspective. Health Qual Life Outcomes. 2006;4(1):62. https://doi.org/10.1186/1477-7525-4-62.
Fiteni F, Ray IL, Ousmen A, Isambert N, Anota A, Bonnetain F. Health-related quality of life as an endpoint in oncology phase I trials: a systematic review. BMC Cancer. 2019;19(1):361. https://doi.org/10.1186/s12885-019-5579-3.
Gamper EM, Musoro JZ, Coens C, Stelmes JJ, Falato C, Groenvold M, et al. Minimally important differences for the EORTC QLQ-C30 in prostate cancer clinical trials. BMC Cancer. 2021;21(1):1083. https://doi.org/10.1186/s12885-021-08609-7.
Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948–68. https://doi.org/10.1183/09031936.05.00035205.
R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for statistical Computing; 2017.
Therneau TM, Grambsch PM. Modeling survival data: extending the Cox model (statistics for biology and health). New York: NY Springer-Verlag; 2000. https://doi.org/10.1007/978-1-4757-3294-8.
Verbanck S, Hanon S, Schuermans D, Van Parijs H, Vinh-Hung V, Miedema G, et al. Small airways function in breast cancer patients before and after radiotherapy. Breast Cancer Res Treat. 2012;135(3):857–65. https://doi.org/10.1007/s10549-012-2201-7.
Treacher DF, Leach RM. Oxygen transport-1. Basic principles BMJ. 1998;317(7168):1302–6. https://doi.org/10.1136/bmj.317.7168.1302.
Burtscher M. Exercise limitations by the oxygen delivery and utilization systems in aging and disease: coordinated adaptation and deadaptation of the lung-heart muscle axis - a mini-review. Gerontology. 2013;59(4):289–96. https://doi.org/10.1159/000343990.
Mahler DA, O'Donnell DE. Recent advances in dyspnea. Chest. 2015;147(1):232–41. https://doi.org/10.1378/chest.14-0800.
Petersen S, von Leupoldt A, Van den Bergh O. Geriatric dyspnea: doing worse, feeling better. Ageing Res Rev. 2014;15:94–9. https://doi.org/10.1016/j.arr.2014.03.001.
Brims FJ, Davies HE, Lee YC. Respiratory chest pain: diagnosis and treatment. Med Clin North Am. 2010;94(2):217–32. https://doi.org/10.1016/j.mcna.2010.01.003.
Park JS, Cha KS, Shin D, Lee DS, Lee HW, Oh JH, et al. Impact of non-chest pain complaint as a presenting symptom on door-to-balloon time and clinical outcomes in patients with acute ST-elevation myocardial infarction. Am J Cardiol. 2014;114(12):1801–9. https://doi.org/10.1016/j.amjcard.2014.09.017.
Chen YW, Camp PG, Coxson HO, Road JD, Guenette JA, Hunt MA, et al. Comorbidities that cause pain and the contributors to pain in individuals with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2017;98(8):1535–43. https://doi.org/10.1016/j.apmr.2016.10.016.
Hareendran A, Leidy NK. Measurement of Dyspnea in Clinical Trials. In: Mahler DA, O'Donnell DE, editors. Dyspnea: Mechanisms, Measurement, and Management. Third Edition ed. Boca Raton, FL: CRC Press, Taylor & Francis Group; 2014. p. 111–127.
Gupta A, Ohri N, Haffty BG. Hypofractionated whole breast irradiation is cost-effective-but is that enough to change practice? Transl Cancer Res. 2018;7(Suppl 4):S469–S72. https://doi.org/10.21037/tcr.2018.03.20.
Wang SL, Fang H, Song YW, Wang WH, Hu C, Liu YP, et al. Hypofractionated versus conventional fractionated postmastectomy radiotherapy for patients with high-risk breast cancer: a randomised, non-inferiority, open-label, phase 3 trial. Lancet Oncol. 2019;20(3):352–60. https://doi.org/10.1016/S1470-2045(18)30813-1.
Vinh-Hung V, Nguyen NP, Verschraegen C. Hypofractionated nodal irradiation for breast cancer: a case for caution. JAMA Oncol. 2019;5(1):13–4. https://doi.org/10.1001/jamaoncol.2018.5061.
Wang X, Fargier-Bochaton O, Dipasquale G, Laouiti M, Kountouri M, Gorobets O, et al. Is prone free breathing better than supine deep inspiration breath-hold for left whole-breast radiotherapy? A dosimetric analysis. Strahlenther Onkol. 2021;197(4):317–31. https://doi.org/10.1007/s00066-020-01731-8.
Acknowledgments
We are deeply grateful to the technologists, nurses, and physicists of the Brussels University Hospital for patient management, to Stephanie Fortier of the James, Ohio State University for revision help, to Claudia Copeland of Carpe Diem Biomedical Writing & Editing for scientific English editing, and, foremost, we are indebted to our patients for participating to TomoBreast. We are grateful to our colleagues of the Ohio State University Comprehensive Cancer Center, Columbus, OH, USA, who presented part of the study at the San Antonio Breast Cancer Symposium, December 10-14, 2019.
Consent to participate
All patients gave signed informed consent to participate.
Code availability
All codes are publicly available through The Comprehensive R Archive Network https://cran.r-project.org/
Funding
TomoBreast was supported in part by grant SCIE2006–30 Stichting tegen Kanker - Fondation contre le Cancer, Belgium. The funding bodies played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
Concept and design: VVH, GS, MDR, HVP. Data acquisition: HVP, CF, GS, NA. Data analysis and graph report: VVH, OG. Initial draft: HVP, VVH, CF, CV. Literature search: DMN, NPN, GS. Data interpretation, manuscript writing, final approval: all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received approval from the Institutional Review Board at the Universitair Ziekenhuis Brussel, Vrije Universiteit Brussel.
Consent for publication
Not applicable.
Competing interests
The Radiation Oncology department of the Universitair Ziekenhuis Brussel under the direction of Guy Storme and Mark De Ridder had a research agreement with Tomotherapy Inc., Madison, WI, unrelated to the present study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Van Parijs, H., Vinh-Hung, V., Fontaine, C. et al. Cardiopulmonary-related patient-reported outcomes in a randomized clinical trial of radiation therapy for breast cancer. BMC Cancer 21, 1177 (2021). https://doi.org/10.1186/s12885-021-08916-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-021-08916-z