Abstract
Background
There is no evidence whether it is best to stop drinking alcohol at all or whether it is okay to drink a little in that light-to-moderate alcohol use was associated with low cardiovascular disease (CVD) compared to non-drinker among colorectal cancer (CRC) survivors, who are regarded as vulnerable to CVD. Therefore, we evaluated the association between alcohol consumption and incident CVD among long-term survivors of CRC.
Methods
This population-based, retrospective cohort study utilized data from the Korean National Insurance Service of 20,653 long-term survivors of CRC diagnosed between 2006 and 2012. Participants were followed up to the date of CVD, death, or December 31, 2018. All patients were categorized according to their daily alcohol consumption (g/day). The outcomes were incident CVD, including ischemic heart disease (IHD) and ischemic and hemorrhagic stroke, analyzed using the Cox proportional hazards regression after adjusting for cardiovascular risk factors and history of chemotherapy and radiotherapy.
Results
There was no association between alcohol consumption and incident CVD among long-term survivors of CRC. Additionally, hazardous alcohol consumption (≥ 40 g/day in male patients and ≥ 20 g/day in female patients) was associated with increased CVD, ischemic stroke, and hemorrhagic stroke (adjusted hazard ratio [95% confidence interval]: 1.51 [1.15–1.97], 1.60 [1.03–2.48], and 2.65 [1.25–5.62], respectively) compared with non-drinkers.
Conclusion
No discernable protective association was found between alcohol consumption and incident CVD for even light-to-moderate drinking among long-term survivors of CRC. Alcohol consumption ≥40 g/day in male patients and ≥ 20 g/day in female patients was associated with an increased risk of stroke compared with non-drinkers. These novel results provide useful evidence when advising survivors of CRC regarding alcohol use.
Similar content being viewed by others
Background
Colorectal cancer (CRC) is the third most diagnosed cancer worldwide [1] and the second among South Korean adults [2]. Although the global CRC mortality is still high, some countries, including the United States, United Kingdom, and South Korea, report high 5-year survival rates for CRC [3]. Early detection, progress in national cancer screening, and advances in therapeutics facilitated the decrease in cancer mortality that, in turn, increased active life expectancy [4]. Accordingly, long-term survivors of CRC are now faced with other health problems, including obesity, hypertension, diabetes, dyslipidemia, and cardiovascular disease (CVD).
Usually, 5 years after diagnosis and treatment of CRC, patients are informed of 5-year survival and recommended self-management with community care. For this reason, the lifestyle of long-term CRC survivors tends to return to the initial state before diagnosis, particularly alcohol habit. However, there is no evidence whether it is best to stop drinking alcohol at all or whether it is okay to drink a little in that light-to-moderate alcohol use was associated with low ischemic heart disease (IHD) and stroke mortality compared to non-drinker [5]. Therefore, we investigated the association between alcohol use and CVD among long-term survivors of CRC.
Methods
Study overview and patient population
The Korean National Health Insurance Service (NHIS) is a mandatory health insurance system for all citizens, including detailed data on demographics, lifestyle behaviors, outpatient department visits, hospitalizations, pharmacological prescriptions, surgical and adjuvant treatments, and laboratory examinations [6]. All citizens aged 40 years or older are eligible for a biannual screening that involves self-reported questionnaires regarding medical history, behavioral characteristics, anthropometric measurements, and laboratory findings [7]. In the Korean NHIS, critical codes for cancer were implemented in 2004. Therefore, patients with cancer are offered additional critical condition codes that are adopted only when a diagnosis of cancer is confirmed [8]. These codes provide reimbursement benefits for cancer-associated management costs based on the household incomes of patients. The diagnosis of CRC was made within the dataset by the attending physicians who recorded a primary diagnosis according to the International Classification of Diseases, Tenth Revision (ICD-10) codes.
This population-based, retrospective cohort study utilized data from the Korean NHIS. The inclusion criteria were patients with new-onset CRC who survived at least 5 years and had available demographic characteristics, follow-up information, and clinical data. Patients with CVD before the index date, defined as the date of 5-year survival for each participant, and those with missing values for covariates were excluded. All patients were followed up from the index date to the date of CVD, death, or December 31, 2018 (see Figure S1 in a supplementary file). This study was approved by the Institutional Review Board of Seoul National University (approval number E-2004-191-1119). The requirement for informed consent was waived by the review board, as the NHIS database is anonymized by strict confidentiality guidelines.
Among the 33,483 patients who were diagnosed with CRC (ICD-10 codes, C17–C21) and received health examinations, we excluded 5869 patients with CRC before 2006 to restrict the study population to only those patients with newly diagnosed CRC. To reconcile the starting point of observation and detect new-onset CVD, we excluded 5905 patients who had CVD prior to the index date. In addition, 1056 patients who had missing values for covariates were excluded. The final study population included 20,653 patients with CRC who survived ≥5 years after the initial diagnosis.
Exposure, outcomes, and covariates
Information on alcohol consumption was collected and included weekly drinking frequency (times per week) and daily consumption (standard drinks per day). One standard drink was defined as 10 g of alcohol. Alcohol-related classification followed the standards of the World Health Organization (WHO) [9]. A working definition from the WHO standards describes hazardous drinking as a regular, average alcohol consumption of ≥40 g/day for males and ≥ 20 g/day for females. Therefore, high alcohol consumption for male and female participants in this study was designated as ≥40 g/day and ≥ 20 g/day, respectively. CVD was the primary outcome and was defined as ≥2 days of hospitalization due to IHD or stroke. Before admission, the attending physician recorded a primary diagnosis according to the ICD-10 codes. The ICD-10 codes for CVD (I20–I25 and I60–I69), IHD (I20–I25), stroke (I60–I69), ischemic stroke (I63), and hemorrhagic stroke (I61–I62) were derived from the guidelines of the American Heart Association [10].
A self-reported questionnaire was used to obtain data on household income; history of dyslipidemia, hypertension, and diabetes mellitus; smoking status; alcohol consumption (as defined above); and physical activity. Physiological and serological measurements were collected at a health examination performed within 2 years prior to the 5-year survival date and included body mass index, waist circumference, blood pressure, fasting serum glucose, total cholesterol, and liver function tests. The Charlson Comorbidity Index (CCI) was calculated in accordance with a previous study [11]. Before hospital admission for a CVD event, the attending physician recorded a primary diagnosis using the ICD-10 codes for CVD as described above.
Statistical analyses
Continuous and categorical variables are presented as the median (interquartile range) and number (%), respectively. The hazard ratio (HR) and 95% confidence interval (CI) for the risks of CVD, IHD, stroke, ischemic stroke, and hemorrhagic stroke were evaluated using Cox proportional hazards regression after adjusting for age (continuous: years); sex (categorical: male, female); household income (categorical: 4 quartiles); body mass index (continuous: kg/m2); systolic blood pressure (continuous: mmHg); fasting serum glucose (continuous: mg/dL); total cholesterol (continuous: mg/dL); smoking (categorical: never and ever); physical activity, including walking and moderate or vigorous physical activity (categorical: 0, 1–2, 3–4, and ≥ 5 days per week); CCI (continuous); history of chemotherapy (categorical: yes, no); and history of radiotherapy (categorical: yes, no). The proportional hazards assumption was tested graphically based on the scaled Schoenfeld residuals, and we detected no violation in the assumption for proportionality. Alcohol consumption was coded using a restricted cubic spline function with four knots located at the 5th, 33rd, 67th, and 95th percentiles based on the amount of alcohol intake presented using the penalized B-spline function. Patients with no alcohol consumption were set as the reference group. A P value of less than 0.05 was considered reflective of statistical significance. All statistical analyses and data collection were carried out using the SAS Enterprise Guide 7.1 (SAS Institute, Cary, NC, USA).
Results
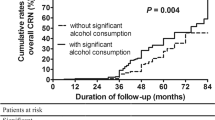
Table 1 shows the general characteristics of the study population according to sex. The proportion of non-drinkers was higher in female patients than in male patients. The median follow-up period was 3.2 years, and the longest follow-up period was 8.0 years. Figure 1 depicts the association of alcohol consumption with the risk of CVD. Alcohol consumption of ≥40 g/day in male patients and ≥ 20 g/day in female patients was associated with increased CVD compared with the non-drinking group after adjusting for the variables described above, whereas the lowest risks were found in the 10–19.9 g/day group for male patients and the < 5 g/day group for female patients. The quantitative values for the adjusted HR (aHR) for CVD, IHD, and stroke for male and female participants are presented in Tables 2 and 3, respectively.
Restricted cubic spline used for evaluating the association between alcohol consumption and cardiovascular diseases. Alcohol consumption was coded using a restricted cubic spline function with four knots located at the 5th, 33rd, 67th, and 95th percentiles based on the amount of alcohol intake and was presented with the penalized B-spline function. The upper cut-offs for the amount of alcohol intake were ≥ 40 and ≥ 20 g/day for male and female participants, respectively. The confidence intervals are presented with dashed lines. Hazard ratios were calculated using Cox proportional hazards regression analysis after adjusting for age, household income, systolic blood pressure, body mass index, fasting serum glucose, total cholesterol, smoking, walking, moderate-to-vigorous physical activity, Charlson comorbidity index, history of chemotherapy, and history of radiotherapy. a Cardiovascular disease risk in male participants. b Cardiovascular disease risk in female participants
To confirm if the association between alcohol consumption and CVD risk was homogeneous regardless of patient characteristics among male participants, subgroup analyses were performed (see Table S1 in a supplementary file). There was no beneficial amount of drinking in any of the stratified subgroups. By contrast, consuming 10–19.9 g/day significantly worsened the prognosis of patients with dyslipidemia (aHR, 7.47; 95% CI, 1.90–29.37; P = 0.004) in terms of CVD. In subgroup analyses of female participants, alcohol consumption was not significantly associated with CVD (see Table S2 in a supplementary file). Female patients who consumed ≥20 g/day of alcohol maintained significant increases in CVD risk in most subgroups and 10–19.9 g/day was significantly harmful in patients with diabetes mellitus (aHR, 8.38; 95% CI, 1.62–43.22; P = 0.011).
When stratified according to the WHO criteria, moderate alcohol consumption (males, < 40 g/day; females, < 20 g/day) did not increase or decrease the risk for CVD, IHD, total stroke, ischemic stroke, and hemorrhagic stroke (Table 4). However, hazardous alcohol consumption (males, ≥ 40 g/day; females, ≥ 20 g/day) significantly elevated the risk for CVD, which was mainly attributed to stroke, including both ischemic and hemorrhagic stroke. The subgroup analyses by sex, age, body mass index, chronic disease, comorbidity, smoking, or physical activity demonstrated similar tendencies as those revealed in the main results (Table S3 in a supplementary file).
Discussion
In this large, retrospective cohort study, no discernable protective association was found between alcohol consumption and CVD incidence, even after light-to-moderate drinking, among long-term survivors of CRC. Alcohol consumption of ≥40 g/day in male patients and ≥ 20 g/day in female patients was associated with increased CVD, which was mainly attributed to stroke rather than IHD. To the best of our knowledge, this is the first study to investigate the association between alcohol consumption and CVD among long-term (minimum of 5 years) survivors of CRC. Our results may provide important and useful evidence when communicating with cancer survivors regarding alcohol use.
The protective effects of light-to-moderate alcohol consumption on the development of CVD have been extensively investigated, although mainly among healthy adults [5, 12]. The protective mechanisms were regarded as improving CV risk factors, such as increasing high-density lipoprotein cholesterol and improving insulin resistance [13, 14]; changing hemostatic factors, such as decreasing fibrinogen, platelet activation, and its aggregation [15]; and altering inflammation and oxidative stress [16]. However, we found that there were no protective effects of alcohol consumption on CVD developments among long-term survivors of CRC. Similar results were found when unadjusted or only adjusted for age and household income for each male and female long-term CRC survivors.
One recent study on the effects of moderate alcohol consumption provides clues as to why there was no favorable effect of light-to-moderate alcohol consumption in our study. This systematic review and meta-analysis reported that there were immediate toxic effects on the cardiovascular system following moderate alcohol consumption, but protective effects were observed after 24 h [17]. The acute changes included increased heart rate and blood pressure resulting from activation of the renin-angiotensin system, increased vascular reactivity, and inhibition of endothelial nitric oxide production [18]. Another study demonstrated that an acute, negative inotropic effect by alcohol in isolated myocardium resulted in weakened heart contractions [19].
Survivors of cancer per se are potentially vulnerable to CVD due to cardiotoxic cancer therapeutics, including chemotherapy and radiotherapy [20]. In particular, 5-fluorouracil is one of the most widely used chemotherapeutic agents for CRC and has been reported to induce cardiotoxicity and long-term cardiovascular sequelae [21]. Furthermore, survivors of cancer are more likely to have CVD risk factors than are individuals without cancer. One large, retrospective cohort study reported that cancer survivors had significantly higher weights and rates of hypertension and dyslipidemia than did non-cancer controls [22]. Another epidemiological study suggested that common CVD risk factors play more prominent roles in CVD development in cancer survivors than in non-cancer controls [23]. Accordingly, the vascular vulnerability of survivors of CRC may lead to a lower capacity to buffer the acute adverse effects of alcohol and may possibly aggravate the adverse effects of alcohol. In our study, we found that the incidence of both ischemic and hemorrhagic stroke was elevated in the hazardous alcohol consumption group than in the abstainer group among survivors of CRC, and the magnitude was higher for hemorrhagic than for ischemic stroke. Key risk factors for hemorrhagic stroke are hypertension and atherosclerosis in the small vessels of the brain [24]. Therefore, survivors of CRC are vulnerable not only to ischemic changes but also to rapidly increasing blood pressure, which could be induced by alcohol consumption. Further studies are needed to understand the effects of alcohol consumption on the cardio- and cerebrovascular systems of cancer survivors.
Several limitations of this study should be noted. First, hospitalization for more than 2 days for IHD or stroke was used to define CVD incidence (based on ICD-10 codes). This may have resulted in the underestimation of chronic IHD that required no hospitalization. However, the accuracy of ICD-10 codes for CVD is greater than 80% [25]. Second, the approach to defining alcohol consumption was challenging. We could not distinguish the types of alcoholic beverages consumed, e.g., beer, soju (Korean distilled beverage), wine, or makgeolli (traditional Korean alcohol). According to a report on the trends of total alcoholic beverage consumption in Korea [26], approximately 40.2% was beer, 31.0% was soju, 16.2% was makgeolli, and 4.4% was wine. Instead of differentiating alcoholic beverages, we tried to unify the amount of ethanol consumed (g/day) considering the average alcohol concentration and quantity of one drink of each alcohol type. Third, the follow-up period was a median of 3.2 years and may have been too short to determine an accurate incidence of CVD associated with alcohol consumption. Conversely, because CRC per se is a risk factor for CVD, early incident IHD or stroke during follow-up may have been related to the CRC experience and not alcohol consumption. Nevertheless, the findings from a sensitivity analysis of the main results, excluding participants diagnosed CVD with the first follow-up, were also in line with those from the main results. Fourth, CVD risks of CRC survivors who reduced or stopped drinking due to severe illness and life-long non-drinkers were not evaluated. However, considering that the study population comprised patients diagnosed with CRC, it may not significantly affect our results, which requires further studies for validation. In addition, the results of the subgroup analyses should be considered as information for future studies, for which caution should be taken when interpreting primary findings considering insufficient justification and evaluation supported by the interaction with alcohol consumption. Another important concern is the use of thrombocyte aggregation inhibitors or other anticoagulants and the presence of thrombocytopenia or myeloproliferative disease that may have acted as confounders, which remains to be confirmed. Lastly, due to the retrospective study design, we did not fully capture the details of chemotherapy and radiotherapy; as an alternative, we focused on one type of cancer. Despite these limitations, the present study fills a gap in the literature and suggests that long-term survivors of CRC should consider abstaining from alcohol consumption to prevent CVD as well as CRC recurrence.
Conclusion
In this large, retrospective cohort study, no discernable protective association was found between alcohol consumption and incident CVD, not even for light-to-moderate drinking, among long-term survivors of CRC. Alcohol consumption ≥40 g/day in men and ≥ 20 g/day in women was associated with increased CVD, which was attributed mostly to stroke rather than to IHD. Considering that CRC is an alcohol-related cancer and that both its development and mortality are increased by alcohol consumption, long-term survivors with CRC should moderate and, if possible, abstain from drinking alcohol to prevent CVD and CRC recurrence. The results from this study may provide useful evidence when advising survivors of cancer regarding alcohol use.
Availability of data and materials
The datasets generated and/or analysed during the current study are available in the Institutional Review Board of Korean National Health Insurance Service repository, https://nhiss.nhis.or.kr.
Abbreviations
- aHR:
-
Adjusted hazard ratio
- CCI:
-
Charlson Comorbidity Index
- CI:
-
Confidence interval
- CRC:
-
Colorectal cancer
- CVD:
-
Cardiovascular disease
- HR:
-
Hazard ratio
- ICD-10:
-
International Classification of Diseases, Tenth Revision
- IHD:
-
Ischemic heart disease
- NHIS:
-
National Health Insurance Service
- WHO:
-
World Health Organization
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
Korea Central Cancer Registry, National Cancer Center. Annual report of cancer statistics in Korea in 2016. In: Ministry of Health and Welfare; 2018.
Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M, et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391(10125):1023–75. https://doi.org/10.1016/S0140-6736(17)33326-3.
Shapiro CL. Cancer survivorship. N Engl J Med. 2018;379(25):2438–50. https://doi.org/10.1056/NEJMra1712502.
Piano MR. Alcohol’s effects on the cardiovascular system. Alcohol Res. 2017;38(2):219–41.
Cheol Seong S, Kim YY, Khang YH, Heon Park J, Kang HJ, Lee H, et al. Data Resource Profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017;46(3):799–800. https://doi.org/10.1093/ije/dyw253.
Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017;46(2):e15. https://doi.org/10.1093/ije/dyv319.
Kim K, Choi S, Park SM. Association of fasting serum glucose level and type 2 diabetes with hepatocellular carcinoma in men with chronic hepatitis B infection: a large cohort study. Eur J Cancer. 2018;102:103–13. https://doi.org/10.1016/j.ejca.2018.07.008.
Organization WH. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines, vol. 67; 1992.
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139(10):e56–e528. https://doi.org/10.1161/CIR.0000000000000659.
Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57(12):1288–94. https://doi.org/10.1016/j.jclinepi.2004.03.012.
de Gaetano G, Costanzo S. Alcohol and health. J Am Coll Cardiol. 2017;70(8):923–5. https://doi.org/10.1016/j.jacc.2017.07.710.
Vu KN, Ballantyne CM, Hoogeveen RC, Nambi V, Volcik KA, Boerwinkle E, et al. Causal role of alcohol consumption in an improved lipid profile: the atherosclerosis risk in communities (ARIC) study. PLoS One. 2016;11(2):e0148765. https://doi.org/10.1371/journal.pone.0148765.
Greenfield JR, Samaras K, Hayward CS, Chisholm DJ, Campbell LV. Beneficial postprandial effect of a small amount of alcohol on diabetes and cardiovascular risk factors: modification by insulin resistance. J Clin Endocrinol Metab. 2005;90(2):661–72. https://doi.org/10.1210/jc.2004-1511.
Salem RO, Laposata M. Effects of alcohol on hemostasis. Am J Clin Pathol. 2005;123(Suppl):S96–105.
Piano MR, Phillips SA. Alcoholic cardiomyopathy: pathophysiologic insights. Cardiovasc Toxicol. 2014;14(4):291–308. https://doi.org/10.1007/s12012-014-9252-4.
Mostofsky E, Chahal HS, Mukamal KJ, Rimm EB, Mittleman MA. Alcohol and immediate risk of cardiovascular events: a systematic review and dose-response meta-analysis. Circulation. 2016;133(10):979–87. https://doi.org/10.1161/CIRCULATIONAHA.115.019743.
Marques-Vidal P, Arveiler D, Evans A, Amouyel P, Ferrieres J, Ducimetiere P. Different alcohol drinking and blood pressure relationships in France and Northern Ireland: the PRIME Study. Hypertension. 2001;38(6):1361–6. https://doi.org/10.1161/hy1101.095328.
Danziger RS, Sakai M, Capogrossi MC, Spurgeon HA, Hansford RG, Lakatta EG. Ethanol acutely and reversibly suppresses excitation-contraction coupling in cardiac myocytes. Circ Res. 1991;68(6):1660–8. https://doi.org/10.1161/01.RES.68.6.1660.
Okwuosa TM, Anzevino S, Rao R. Cardiovascular disease in cancer survivors. Postgrad Med J. 2017;93(1096):82–90. https://doi.org/10.1136/postgradmedj-2016-134417.
Sara JD, Kaur J, Khodadadi R, Rehman M, Lobo R, Chakrabarti S, et al. 5-fluorouracil and cardiotoxicity: a review. Ther Adv Med Oncol. 2018;10:1758835918780140.
Armenian SH, Xu L, Ky B, Sun C, Farol LT, Pal SK, et al. Cardiovascular disease among survivors of adult-onset cancer: a community-based retrospective cohort study. J Clin Oncol. 2016;34(10):1122–30. https://doi.org/10.1200/JCO.2015.64.0409.
Armstrong GT, Oeffinger KC, Chen Y, Kawashima T, Yasui Y, Leisenring W, et al. Modifiable risk factors and major cardiac events among adult survivors of childhood cancer. J Clin Oncol. 2013;31(29):3673–80. https://doi.org/10.1200/JCO.2013.49.3205.
Sierra C, Coca A, Schiffrin EL. Vascular mechanisms in the pathogenesis of stroke. Curr Hypertens Rep. 2011;13(3):200–7. https://doi.org/10.1007/s11906-011-0195-x.
Park JK, Kim KS, Kim CB, Lee TY, Lee KS, Lee DH, et al. The accuracy of ICD codes for cerebrovascular diseases in medical insurance claims. Korean J Prev Med. 2000;33(1):76–82.
Ministry of Agriculture FaRA, Korea Agro-Ficheries & Food Trade Corporation: A report on alcoholic beverage consumption trends of 2017 in Korea. 2017 https://www.atfis.or.kr/fip/article/M000010300/view.do?articleId=3582.
Acknowledgments
This study used data from the Korean NHIS (NHIS-2019-1-589). Seogsong Jeong and Sung Min Kim received grants from the BK21-plus education program provided by the National Research Foundation of Korea. None of the sponsors had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Funding
None received.
Author information
Authors and Affiliations
Contributions
SMP had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. GL and SJ contributed equally. GL, SJ, SC, and SMP participated in the conceptualization and design of the study. All authors contributed to the acquisition, analysis, and interpretation of data. SJ performed the statistical analysis. GL, SJ, and SMP drafted the manuscript. All authors critically revised the manuscript for important intellectual content. SMP supervised the study. SJ, SMK, and SMP provided administrative, technical, or material support. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted according to the guidelines in the Declaration of Helsinki and approved by Seoul National University’s Institutional Review Board (approval number: E-2004-191-1119). The requirement for informed consent was waived by the review board, as the NHIS database is anonymized by strict confidentiality guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Figure S1. Study design. Table S1. Subgroup analysis on the association of alcohol consumption with the risk of cardiovascular disease among men with long-term colorectal cancer survivors. Table S2. Subgroup analysis on association of alcohol consumption with the risk of cardiovascular disease among women with long-term colorectal cancer survivors. Table S3. Subgroup analysis on association of alcohol consumption with CVD according to the World Health Organization classification.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lee, G., Jeong, S., Choi, S. et al. Associations between alcohol consumption and cardiovascular disease among long-term survivors of colorectal cancer: a population-based, retrospective cohort study. BMC Cancer 21, 710 (2021). https://doi.org/10.1186/s12885-021-08436-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-021-08436-w