Abstract
Background
In the phase III ALCYONE trial, daratumumab plus bortezomib/melphalan/prednisone (D-VMP) significantly improved overall response rate and progression-free status compared with VMP alone in transplant-ineligible patients with newly diagnosed multiple myeloma (NDMM). Here, we present patient-reported outcomes (PROs) from ALCYONE.
Methods
The European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire Core 30-item (EORTC QLQ-C30) and EuroQol 5-dimensional descriptive system (EQ-5D-5L) questionnaire were administered at baseline, every 3 months (year 1) and every 6 months (until progression). Treatment effects were assessed using a repeated-measures, mixed-effects model.
Results
Compliance with PRO assessments was comparable at baseline (> 90%) and throughout study (> 76%) for both treatment groups. Improvements from baseline were observed in both groups for EORTC QLQ-C30 Global Health Status (GHS), most functional scales, symptom scales and EQ-5D-5L visual analog scale (VAS). Between-group differences were significant for GHS (p = 0.0240) and VAS (p = 0.0160) at month 3. Improvements in pain were clinically meaningful in both groups at all assessment time points. Cognitive function declined in both groups, but the magnitude of the decline was not clinically meaningful.
Conclusions
Patients with transplant-ineligible NDMM demonstrated early and continuous improvements in health-related quality of life, including improvements in functioning and symptoms, following treatment with D-VMP or VMP.
Trial registration
ClinicalTrials.gov identifier NCT02195479, registered September 21, 2014
Similar content being viewed by others
Background
Treatment approaches for newly diagnosed multiple myeloma (NDMM) are chosen based on the patient’s fitness; those considered fit usually receive induction, high-dose chemotherapy and autologous stem cell transplant (ASCT) as standard of care [1]. In patients ineligible for ASCT, treatment with bortezomib, melphalan and prednisone (VMP) or lenalidomide plus low-dose dexamethasone is recommended [1]. Older patients and those who are transplant ineligible have significantly shorter relative survival than younger, fitter, transplant-eligible patients [2, 3]. In addition to age, factors such as frailty, performance status and comorbidities are important determinants of ASCT eligibility and treatment selection in the frontline setting [4,5,6].
MM can profoundly impact patients’ daily lives, imposing both physical (i.e. fatigue, mobility, pain and physical activity) and emotional (i.e. distress, anxiety, depression and effects on relationships) burdens [7, 8]. Maintaining health-related quality of life (HRQoL) during treatment is an important goal in MM, with a particular focus on understanding the long-term impact of disease and treatment on patients [9]. However, reports on HRQoL in the ASCT-ineligible population (in particular) are limited.
In May 2018, the US Food and Drug Administration approved daratumumab, an anti-CD38 humanized monoclonal antibody, for use in combination with VMP (D-VMP) in patients with NDMM who are ineligible for ASCT. This approval was based on the results of the multicenter, open-label, phase III ALCYONE trial (NCT02195479), which demonstrated significantly higher response rates, higher rates of minimal residual disease negativity, and lower risk of disease progression or death in patients who received D-VMP compared with those receiving VMP alone. Prespecified subgroup analyses showed the superiority of D-VMP over VMP in patients 75 years of age or older (29.9% of patients in the study) and those with poor prognosis [10]. Rates of grade 3/4 hematologic events, including neutropenia, thrombocytopenia and anemia, were higher in the D-VMP group than in the VMP group [10].
Here, we present analyses from the ALCYONE clinical trial evaluating the treatment effect of D-VMP on patient-reported outcomes (PROs).
Methods
Study design and patients
Details of the multicenter, randomized, open-label, active-controlled, parallel group ALCYONE trial have been previously published [10]. Cycle length for D-VMP and VMP was 6 weeks (cycles 1–9) and 4 weeks (cycle 10+), respectively. Eligible patients were randomized 1:1 to D-VMP (VMP [see below] plus intravenous daratumumab 16 mg/kg [once weekly in cycle 1, every 3 weeks in cycles 2–9 and every 4 weeks thereafter until disease progression or unacceptable toxicity]) or VMP (subcutaneous bortezomib 1.3 mg/m2 [cycle 1: twice weekly; cycles 2–9: 4 doses/cycle], melphalan 9 mg/m2 [days 1–4] and prednisone 60 mg/m2 [days 1–4]).
The study was conducted at 162 sites in 25 countries. Each study site’s local independent ethics committee or institutional review board approved the study protocol. This study was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki and the International Conference on Harmonisation Good Clinical Practice guidelines and adhered to CONSORT guidelines. All patients provided written informed consent.
PROs
PROs (a secondary objective of the ALCYONE trial) were assessed by the European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire Core 30-item (EORTC QLQ-C30) [11] and the EuroQol 5-dimensional descriptive system (EQ-5D-5L) [12]. The EORTC QLQ-C30 v3 is a validated, cancer-specific instrument that contains 30 items resulting in five functional scales (physical, role, emotional, cognitive and social functioning), one Global Health Status (GHS) scale, three symptom scales (fatigue, nausea and vomiting, and pain) and six single items (dyspnea, insomnia, appetite loss, constipation, diarrhea and financial difficulties) [11]. Higher scores represent greater GHS, better functioning and worse symptoms, respectively. The EQ-5D-5L, a generic measure of health status, assesses five domains including mobility, self-care, usual activities, pain/discomfort and anxiety/depression plus a visual analog scale (VAS) rating of “health today” [12].
PRO responses were collected using an electronic tablet device prior to any other study-related activities, at baseline (before randomization), every 3 months during the treatment phase and then every 6 months until disease progression. All patients were educated on the use of the electronic tablet. Interim results are presented for the first 36 months of treatment.
Statistical methods
The primary analysis population was the intent-to-treat (ITT) population (all randomized patients); the PRO data set was the ITT population of patients with a baseline and > 1 postbaseline PRO assessment. No imputation of missing data or adjustments for multiplicity were made. A sensitivity analysis was conducted using a pattern-mixture model.
PRO data were summarized using descriptive statistics, including number, mean, standard deviation, median, and minimum and maximum value by treatment group. Compliance was calculated at baseline and for each postbaseline PRO assessment visit as a percentage, with the number of PRO assessments received as the numerator and the number of PRO assessments expected at that time point (a clinical prediction of how many patients will be on treatment) as the denominator.
We assessed treatment differences using a repeated-measures, mixed-effects model with a missing-at-random data assumption. The model included the baseline PRO score, treatment group, time, treatment by time interaction and the stratification factors as fixed effects and subject as a random effect. A 2-sided 5% significance level was used to descriptively compare values for the exploratory PRO endpoints, which are derived from scale scores.
The proportion of patients achieving minimally important differences (MIDs) in each PRO instrument scale score, which indicate clinically meaningful changes, was summarized with odds ratios and 95% confidence intervals (CIs). Although there is no universal MID [13], there are multiple published MID thresholds ranging from 5 to 10 [14,15,16,17]. Here, MID thresholds to explore individual patient-level change were defined a priori as 10 points for the EORTC QLQ-C30 scale scores [18] and ≥ 7 points for EQ-5D-5L VAS [19].
We conducted exploratory subgroup analyses to determine if there were differences in EORTC QLQ-C30 GHS, functional and symptom scale scores by age, and Eastern Cooperative Oncology Group (ECOG) performance status. Exploratory analysis of time to worsening using survival curves and hazard ratios (HRs) by depth of clinical response and minimal residual disease (MRD) status were estimated for EORTC QLQ-C30 scores.
Results
Patients
Baseline patient demographics and population characteristics were similar between groups (D-VMP: n = 350; VMP: n = 356) (Table 1). Mean age was 71 years, there were approximately the same number of male and female patients, and approximately half of patients had a baseline ECOG performance status of 1. Baseline EORTC QLQ-C30 scores were similar between treatment arms for all functional and symptom scales (Table 1).
Compliance rates with PRO measures were high and similar across treatment groups. At baseline, 90.6 and 90.3% of patients subsequently assigned to the D-VMP group and 91.9 and 91.3% of patients randomized to the VMP group completed the EORTC QLQ-C30 and the EQ-5D-5L, respectively (supplementary Fig. 1). Compliance rates remained high (> 76%) throughout the study. The number of PRO assessments received was higher in the D-VMP group than in the VMP group, which is consistent with the greater numbers of patients staying on treatment with D-VMP compared with VMP. The PRO data sets for the D-VMP group were also larger owing to the longer treatment duration of these patients.
Treatment effect on EORTC QLQ-C30 scores
ITT population
Using a mixed-effects model with repeated measures, the least squares (LS) mean change in GHS score from baseline was 7.3 in the D-VMP group and 3.9 in the VMP group at 3 months (difference 3.4, p = 0.0240). Between-group differences were not significant at other assessment time points, but point estimates more often favored the D-VMP group than the VMP group. The LS mean change from baseline was clinically meaningful (i.e. ≥10 points) at months 9, 12, 18 and 30 for both treatment groups, as well as at month 24 in the VMP group and month 36 in the D-VMP group (Fig. 1a).
LS mean changes from baseline were not significantly different between treatment groups for the functional scales of the EORTC QLQ-C30. Point estimates favored the D-VMP group at all assessment time points for physical functioning (Fig. 1b) and most time points for role functioning, cognitive functioning and social functioning (supplementary Fig. 2a, c, d). The direction of the point estimates for between-group differences in change in emotional functioning fluctuated depending on the assessment time point, favoring D-VMP at months 6, 12, 30 and 36 and favoring VMP at months 3, 9, 18 and 24 (supplementary Fig. 2b). LS mean change from baseline in physical functioning scores was more often clinically meaningful in the D-VMP group than in the VMP group (6 vs 2 assessment time points). Clinically meaningful changes in role functioning scores were observed in the D-VMP group at all time points after month 3 and in the VMP group at all time points between month 3 and month 30. LS mean changes in emotional functioning scores were clinically meaningful in both treatment groups at all assessment time points after month 3. Scores for cognitive functioning declined from baseline in both groups, but the LS mean change from baseline was not clinically meaningful in either group at any assessment time point.
There were no significant between-group differences in LS mean change from baseline in scores for pain (Fig. 1c), fatigue (Fig. 1d) or nausea and vomiting (supplementary Fig. 2e). Point estimates generally favored D-VMP for these symptoms. Improvements in pain scores were clinically meaningful at all assessment time points for both treatment groups, but were not meaningful for either group at any time point for fatigue or nausea and vomiting. Although overall usage of concomitant medications was similar between groups (97.7 and 96.9% of patients in the D-VMP and VMP groups, respectively), greater proportions of patients in the D-VMP group than in the VMP group used analgesics (70.8% vs 57.9%) and anti-inflammatory agents (25.7% vs 14.4%).
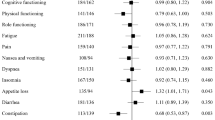
The proportions of patients with a clinically meaningful change (i.e. ≥10 points) in EORTC QLQ-C30 scores at month 36 are shown in Fig. 2. Differences between treatment groups were not statistically significant, but were numerically greater in the D-VMP group for all scales. The greatest proportion of patients experienced clinically meaningful changes in pain scores, with 75% of patients in the D-VMP group and 71% of patients in the VMP group reporting a mean change ≥10 points.
Subgroup analyses
In a subgroup analysis of EORTC QLQ-C30 GHS, physical functioning, pain and fatigue scores by age and ECOG performance status, similar patterns of increasing improvement in HRQoL were observed in all subgroups, including patients 75 years of age or older and those with poorer overall baseline functional status (ECOG performance status ≥2), with no significant difference between the D-VMP and VMP groups after 3 months (Table 2). Improvements were observed in all subgroups, but were generally greater in the younger (< 75 years) vs older (≥75 years) patients and in those with ECOG performance status of 2 vs those with ECOG performance status of 0 or 1.
Time to worsening of GHS, function and symptoms was generally longer with greater depth of clinical response (Table 3). Time to worsening was significantly longer for patients with a complete response and significantly shorter for patients with stable disease, both compared with patients with very good partial response/partial response on the EORTC QLQ-C30 GHS (hazard ratio = 0.72 and 1.75, respectively). Similarly, patients who reached MRD-negative status had significantly improved outcomes compared with MRD-positive patients on EORTC QLQ-C30 GHS and pain (hazard ratio = 0.70 and 0.60, respectively; p < 0.05).
Treatment effect on EQ-5D-5L scores
ITT population
At month 3, the LS mean difference from baseline in EQ-5D-5L VAS score was 7 in the D-VMP group and 3.8 in the VMP group (difference 3.1, p = 0.0160). Between-group differences were not significant at other assessment time points. Point estimates favored the D-VMP group at months 6, 9, 18 and 36 and favored the VMP group at months 12, 24 and 30 (Fig. 3a). The LS mean change was clinically meaningful in both groups at month 18, in the VMP group at month 24 and in the D-VMP group at month 36. The proportion of patients with a clinically meaningful improvement in VAS score was significantly greater in the D-VMP group at month 3 (54.8% vs 41.3%, odds ratio 1.72, p = 0.0025); between-group differences were not significant at other time points (Fig. 3b). The proportion of patients with clinically meaningful improvement in VAS score was numerically greater in the D-VMP group at all assessment time points except month 12.
Subgroup analyses
Similar to the subgroup analysis for EORTC QLQ-C30, increasing improvement over time was observed for EQ-5D-5L VAS scores in subgroups by age and ECOG performance status, with no significant difference between treatment groups after 3 months (Table 2). Improvements were greater in younger patients and those with an ECOG performance status of 2.
Discussion
MM is incurable and was responsible for 1.1% of all cancer deaths worldwide in 2018 [20], and patients with MM experience high levels of pain, fatigue and mood disturbances [21]. MM treatments are often associated with demanding administration and monitoring schedules, as well as adverse events. As a result, the burden of MM on patients’ HRQoL is substantial, and PROs should be an important consideration for evaluating new treatment strategies in these patients. This is particularly relevant for the subpopulation of patients with NDMM who are ineligible for transplant, as this group is typically older and often has comorbidities, including impaired renal and hepatic function, that may limit therapeutic options and/or increase susceptibility to adverse effects. Currently, data on HRQoL in this patient subpopulation are limited.
The results presented here provide clear evidence of the HRQoL benefits of D-VMP and VMP in patients with NDMM who are not eligible for transplant. These findings are consistent with a systematic review by Nielsen et al. [22], which reported clinically relevant improvement in HRQoL following treatment in this population. Our study is the first to examine HRQoL of patients treated with D-VMP, and the robustness of the results was supported by a sensitivity analysis using a pattern-mixture model.
Clinically meaningful improvements in GHS, function and symptoms were maintained in this patient population to at least 36 months, which corresponds to the median overall survival of the control group in the Myeloma Trialists’ Collaborative Group meta-analysis of 24 randomized MM trials [23], and is likely among the longest durations of follow-up reported in the first-line treatment of transplant-ineligible patients with MM. Baseline health status and burden of disease measured using the EORTC QLQ-C30 GHS, functional scales and symptom scales were worse for patients with NDMM compared with a population-based random sample of adults without cancer in Germany [24]. Nevertheless, post-treatment scores improved to a level approaching those of a noncancer population [25]. Improvements in cognitive functioning were lower than those reported for the other functional scales, but this is likely attributable to a ceiling effect, as the mean baseline scores for the cognitive functioning scale were the highest of the functional scales, leaving little additional room for improvement, especially in patients on active treatment. The improvements in pain and fatigue observed with both D-VMP and VMP may be particularly noteworthy. Prior studies have demonstrated that patients with NDMM tend to have more pain and fatigue than those with later-stage disease [26], and a study by Jordan et al. demonstrated that pain and fatigue are the strongest predictors of HRQoL [27]. Treatments that impact these symptoms may therefore have the largest impact on patients’ HRQoL.
Although improvements in the D-VMP group were statistically greater than those in the VMP group on some scores at some time points, between-group differences were largely nonsignificant. This observation needs to be considered in the context of the significant increase in clinical benefits observed with the D-VMP regimen [10]. One possible explanation for the lack of incremental benefit for D-VMP over VMP on HRQoL outcomes may be that this was an on-treatment analysis, in which PRO results are reported for patients remaining on treatment and do not reflect the impact of disease progression resulting in discontinuation of study treatment. A greater proportion of patients in the VMP group compared with the D-VMP group discontinued treatment owing to disease progression (13.3% vs 6.6%) [10]. A second explanation may be the substantial positive impact of bortezomib on HRQoL. The magnitude of symptom improvement observed in the present study is noticeably larger than has been observed in some other studies involving patients with NDMM who were transplant ineligible. For example, the magnitude of the mean changes in GHS, physical functioning, pain and fatigue observed in the D-VMP and VMP groups in the present trial is larger than those observed in the phase III FIRST study of lenalidomide plus low-dose dexamethasone vs melphalan/prednisone/thalidomide [28]. Although cross-trial comparisons need to be interpreted with caution, especially as patient inclusion criteria may differ, these observations suggest that owing to the large improvement in HRQoL with VMP alone and high baseline scores, there was little additional room for improvement in HRQoL upon further addition of daratumumab (i.e. ceiling effect). Especially when it comes to depth of remission, bortezomib-based regimens have consistently reported greater proportions of patients in compete response when compared with immunomodulatory drug–based combinations. In ALCYONE, response assessment was complemented by measurement of MRD rather than by pure International Myeloma Working Group uniform response criteria. In fact, patients who reached MRD-negative status had significantly improved outcomes compared with MRD-positive patients in terms of EORTC QLQ-C30 GHS and pain scores.
Although patients were not randomized by subgroup, and subgroup analyses should be interpreted with caution, results of these analyses were generally supportive of the findings in the overall population. Subgroup analyses also demonstrated symptom improvement with both D-VMP and VMP irrespective of age and functional status. Notably, improvements were observed in patients 75 years of age or older and those with poor overall function, indicating that the addition of daratumumab did not negatively affect HRQoL, even in frail and elderly patients who may have limited treatment options. The improvement in HRQoL in older patients is noteworthy, as elderly patients tend to have greater health impairment, including comorbidities, and so may have a lower likelihood of achieving treatment benefit; and transplant-ineligible patients tend to be older than those who are eligible for transplant [26]. A further subgroup analysis found that improvements in HRQoL were greater for patients achieving the greatest clinical response. This latter observation is consistent with the results of previous studies that have demonstrated an association between improved HRQoL outcomes and depth of clinical response in patients with MM [29, 30].
Other studies have also examined the impact of daratumumab as part of first-line treatment on HRQoL in patients with transplant-eligible and -ineligible MM. In the CASSIOPEIA study, daratumumab in combination with bortezomib, thalidomide, and dexamethasone was associated with significantly greater reductions in pain, less deterioration of cognitive functioning and greater improvements in emotional functioning vs bortezomib, thalidomide and dexamethasone alone in patients with transplant-eligible NDMM [31]. In the MAIA study, the combination of daratumumab with lenalidomide and dexamethasone was associated with faster and sustained improvement in HRQoL measures compared with lenalidomide and dexamethasone alone in patients with transplant-ineligible NDMM [32]. In both the CASSIOPEIA and MAIA studies, improvements in HRQoL were consistent with observed clinical benefit. Our results, the first in a study that includes an alkylator agent, add to these existing data and demonstrate that the combination of D-VMP improves HRQoL, with meaningful improvements in both functional and symptom scales in patients with transplant-ineligible NDMM.
As noted above, the improvements in PROs reported here complement the significant clinical benefits observed with D-VMP vs VMP, including a lower risk of disease progression and higher percentages of patients with MRD negativity. PROs provide the patient perspective on treatment, and use of clinical endpoints and PROs together best reflect the full spectrum of patients’ disease as well as the overall effectiveness of treatment. However, whereas the clinical assessments showed significant improvements with D-VMP vs VMP [10], including significant improvements in overall survival [33], differences in HRQoL between groups were modest and largely nonsignificant. In addition to the two explanations provided above, this disparity could be due to the use of generic PRO instruments in the ALCYONE trial. MM-specific PRO measures with greater sensitivity to changes in HRQoL, symptoms and impacts for comparing two treatments with multiple drugs may have been able to tease out the treatment differences with greater specificity, although the EORTC QLQ-C30 and EQ-5D-5L are validated tools that are widely used to assess HRQoL in patients with cancer.
One of the limitations of the present study is the open-label design, which may lead to biased treatment effects on PROs. As noted above, another limitation is that only on-treatment results are presented, as patients were censored from the analysis when they discontinued treatment, so HRQoL outcomes do not reflect disease progression (and more patients in the VMP group progressed and discontinued treatment). Furthermore, no reasons were documented for missing data, and some consequences of treatment may not have been identified. This study is also limited by the lack of control for the use of pain medication. Nonsteroidal anti-inflammatory drugs are not recommended in patients with MM because of renal toxicity [34], yet 25.7% of patients in the D-VMP group and 14.4% in the VMP group were treated with these agents, and the proportion of patients treated with analgesic, low-dose corticosteroid and anti-inflammatory medications was greater in the D-VMP group than in the VMP group. It is not possible to determine to what extent these medications may have contributed to the decreases in pain observed in the study, although the impact of systemic corticosteroids is likely minimal given the high cumulative dose of prednisone patients received as part of their study treatment. Furthermore, the difference in the proportion of patients treated with these agents while on study treatment may be explained, at least in part, by the fact that more patients remained on treatment in the D-VMP group.
In conclusion, patients with NDMM who were transplant ineligible demonstrated early and continuous improvements in HRQoL, including improvements in function and symptoms following treatment with D-VMP or VMP. Functional status and well-being were maintained in patients who remained in the study for both the D-VMP and VMP treatment groups, and support the clinical efficacy benefits already reported [10]. This analysis highlights the importance of measuring HRQoL and PROs to confirm the benefits of cancer therapy on the day-to-day aspects of patients’ lives, as well as their clinical prognoses.
Availability of data and materials
The data sharing policy of Janssen Pharmaceutical Companies of Johnson & Johnson is available at https://www.janssen.com/clinical-trials/transparency. As noted on this site, requests for access to the study data can be submitted through Yale Open Data Access (YODA) Project site at http://yoda.yale.edu.
Abbreviations
- ASCT:
-
Autologous stem cell transplant
- CI:
-
Confidence interval
- D-VMP:
-
Daratumumab plus bortezomib, melphalan and prednisone
- ECOG:
-
Eastern cooperative oncology group
- EORTC QLQ-C30:
-
European organisation for research and treatment of cancer quality of life
- EQ-5D-5L:
-
EuroQol 5-dimensional descriptive system
- GHS:
-
Global health status
- HR:
-
Hazard ratio
- HRQoL:
-
Health-related quality of life
- ITT:
-
Intent to treat
- LS:
-
Least squares
- MID:
-
Minimally important difference
- MM:
-
Multiple myeloma
- MRD:
-
Minimal residual disease
- NDMM:
-
Newly diagnosed multiple myeloma
- PRO:
-
Patient-reported outcome
- VAS:
-
Visual analog scale
- VMP:
-
Bortezomib, melphalan and prednisone
References
Moreau P, San Miguel J, Sonneveld P, Mateos MV, Zamagni E, Avet-Loiseau H, et al. Multiple myeloma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28(suppl 4):iv52–61.
Szabo K, Bodoki L, Nagy-Vincze M, Vincze A, Zilahi E, Szodoray P, et al. Effect of genetic and laboratory findings on clinical course of Antisynthetase syndrome in a Hungarian cohort. Biomed Res Int. 2018;2018:6416378.
Rodriguez-Otero P, Mateos MV, Martinez-Lopez J, Hernandez MT, Ocio EM, Rosinol L, et al. Predicting long-term disease control in transplant-ineligible patients with multiple myeloma: impact of an MGUS-like signature. Blood Cancer J. 2019;9(4):36. https://doi.org/10.1038/s41408-019-0176-x.
Moreau P, Attal M, Facon T. Frontline therapy of multiple myeloma. Blood. 2015;125(20):3076–84. https://doi.org/10.1182/blood-2014-09-568915.
Gandolfi S, Vekstein C, Laubach JP, O'Brien A, Masone K, Munshi NC, et al. The evolving role of transplantation in multiple myeloma: the need for a heterogeneous approach to a heterogeneous disease. Clin Adv Hematol Oncol. 2018;16(8):564–74.
Djebbari F, Sharpley FA, McLain-Smith S, Vallance G, Eyre TA, Kothari J, et al. Treatment-free interval as an additional measure of efficacy in a large UK dataset of transplant ineligible myeloma patients. PLoS One. 2020;15(2):e0229469. https://doi.org/10.1371/journal.pone.0229469.
Ramsenthaler C, Kane P, Gao W, Siegert RJ, Edmonds PM, Schey SA, et al. Prevalence of symptoms in patients with multiple myeloma: a systematic review and meta-analysis. Eur J Haematol. 2016;97(5):416–29. https://doi.org/10.1111/ejh.12790.
Baz R, Lin HM, Hui AM, Harvey RD, Colson K, Gallop K, et al. Development of a conceptual model to illustrate the impact of multiple myeloma and its treatment on health-related quality of life. Support Care Cancer. 2015;23(9):2789–97. https://doi.org/10.1007/s00520-015-2644-6.
Osborne TR, Ramsenthaler C, Siegert RJ, Edmonds PM, Schey SA, Higginson IJ. What issues matter most to people with multiple myeloma and how well are we measuring them? A systematic review of quality of life tools. Eur J Haematol. 2012;89(6):437–57. https://doi.org/10.1111/ejh.12012.
Mateos MV, Dimopoulos MA, Cavo M, Suzuki K, Jakubowiak A, Knop S, et al. Daratumumab plus bortezomib, melphalan, and prednisone for untreated myeloma. N Engl J Med. 2018;378(6):518–28. https://doi.org/10.1056/NEJMoa1714678.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–76. https://doi.org/10.1093/jnci/85.5.365.
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–36. https://doi.org/10.1007/s11136-011-9903-x.
King MT. A point of minimal important difference (MID): a critique of terminology and methods. Expert Rev Pharmacoecon Outcomes Res. 2011;11(2):171–84. https://doi.org/10.1586/erp.11.9.
Kvam AK, Fayers PM, Wisloff F. Responsiveness and minimal important score differences in quality-of-life questionnaires: a comparison of the EORTC QLQ-C30 cancer-specific questionnaire to the generic utility questionnaires EQ-5D and 15D in patients with multiple myeloma. Eur J Haematol. 2011;87(4):330–7. https://doi.org/10.1111/j.1600-0609.2011.01665.x.
Cocks K, King MT, Velikova G, de Castro GJ, Martyn St-James M, Fayers PM, et al. Evidence-based guidelines for interpreting change scores for the European organisation for the research and treatment of Cancer quality of life questionnaire Core 30. Eur J Cancer. 2012;48(11):1713–21. https://doi.org/10.1016/j.ejca.2012.02.059.
Cocks K, King MT, Velikova G, Fayers PM, Brown JM. Quality, interpretation and presentation of European Organisation for Research and Treatment of Cancer quality of life questionnaire core 30 data in randomised controlled trials. Eur J Cancer. 2008;44(13):1793–8. https://doi.org/10.1016/j.ejca.2008.05.008.
Cocks K, King MT, Velikova G, Martyn St-James M, Fayers PM, Brown JM. Evidence-based guidelines for determination of sample size and interpretation of the European organisation for the research and treatment of Cancer quality of life questionnaire Core 30. J Clin Oncol. 2011;29(1):89–96. https://doi.org/10.1200/JCO.2010.28.0107.
Wisløff F, Eika S, Hippe E, Hjorth M, Holmberg E, Kaasa S, et al. Measurement of health-related quality of life in multiple myeloma. Nordic myeloma study group. Br J Haematol. 1996;92(3):604–13. https://doi.org/10.1046/j.1365-2141.1996.352889.x.
Pickard AS, Neary MP, Cella D. Estimation of minimally important differences in EQ-5D utility and VAS scores in cancer. Health Qual Life Outcomes. 2007;5(1):70. https://doi.org/10.1186/1477-7525-5-70.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
Coleman EA, Goodwin JA, Coon SK, Richards K, Enderlin C, Kennedy R, et al. Fatigue, sleep, pain, mood, and performance status in patients with multiple myeloma. Cancer Nurs. 2011;34(3):219–27. https://doi.org/10.1097/NCC.0b013e3181f9904d.
Nielsen LK, Jarden M, Andersen CL, Frederiksen H, Abildgaard N. A systematic review of health-related quality of life in longitudinal studies of myeloma patients. Eur J Haematol. 2017;99(1):3–17. https://doi.org/10.1111/ejh.12882.
Myeloma Trialists' Collaborative Group. Interferon as therapy for multiple myeloma: an individual patient data overview of 24 randomized trials and 4012 patients. Br J Haematol. 2001;113(4):1020–34. https://doi.org/10.1046/j.1365-2141.2001.02857.x.
Schwarz R, Hinz A. Reference data for the quality of life questionnaire EORTC QLQ-C30 in the general German population. Eur J Cancer. 2001;37(11):1345–51. https://doi.org/10.1016/S0959-8049(00)00447-0.
Nolte S, Liegl G, Petersen MA, Aaronson NK, Costantini A, Fayers PM, et al. General population normative data for the EORTC QLQ-C30 health-related quality of life questionnaire based on 15,386 persons across 13 European countries, Canada and the unites states. Eur J Cancer. 2019;107:153–63. https://doi.org/10.1016/j.ejca.2018.11.024.
Robinson D Jr, Esseltine DL, Regnault A, Meunier J, Liu K, van de Velde H. The influence of baseline characteristics and disease stage on health-related quality of life in multiple myeloma: findings from six randomized controlled trials. Br J Haematol. 2016, 174;(3):368–81. https://doi.org/10.1111/bjh.14058.
Jordan K, Proskorovsky I, Lewis P, Ishak J, Payne K, Lordan N, et al. Effect of general symptom level, specific adverse events, treatment patterns, and patient characteristics on health-related quality of life in patients with multiple myeloma: results of a European, multicenter cohort study. Support Care Cancer. 2014;22(2):417–26. https://doi.org/10.1007/s00520-013-1991-4.
Delforge M, Minuk L, Eisenmann JC, Arnulf B, Canepa L, Fragasso A, et al. Health-related quality-of-life in patients with newly diagnosed multiple myeloma in the FIRST trial: lenalidomide plus low-dose dexamethasone versus melphalan, prednisone, thalidomide. Haematologica. 2015;100(6):826–33. https://doi.org/10.3324/haematol.2014.120121.
Delforge M, Dhawan R, Robinson D Jr, Meunier J, Regnault A, Esseltine DL, et al. Health-related quality of life in elderly, newly diagnosed multiple myeloma patients treated with VMP vs. MP: results from the VISTA trial. Eur J Haematol. 2012;89(1):16–27. https://doi.org/10.1111/j.1600-0609.2012.01788.x.
Dimopoulos MA, Palumbo A, Hajek R, Kropff M, Petrucci MT, Lewis P, et al. Factors that influence health-related quality of life in newly diagnosed patients with multiple myeloma aged ≥ 65 years treated with melphalan, prednisone and lenalidomide followed by lenalidomide maintenance: results of a randomized trial. Leuk Lymphoma. 2014;55(7):1489–97. https://doi.org/10.3109/10428194.2013.847933.
Roussel M, Moreau P, Attal M, Eisenmann JC, Laribi K, Jaccard A, et al. PS1377 improvement in health-related quality of life for newly diagnosed multiple myeloma transplant-eligible patients treated with daratumumab, bortezomib, thalidomide, and dexamethasone: CASSIOPEIA study. HemaSphere. 2019;3(suppl 1):630. https://doi.org/10.1097/01.HS9.0000563784.11014.52.
Perrot A, Facon T, Plesner T, Usmani SZ, Kumar S, Bahlis NJ, et al. Faster and sustained improvement in health-related quality of life (HRQoL) for newly diagnosed multiple myeloma (NDMM) patients ineligible for transplant treated with daratumumab, lenalidomide, and dexamethasone (D-Rd) versus Rd alone: MAIA. J Clin Oncol. 2019;37(15):8016. https://doi.org/10.1200/JCO.2019.37.15_suppl.8016.
Mateos MV, Cavo M, Blade J, Dimopoulos MA, Suzuki K, Jakubowiak A, et al. Overall survival with daratumumab, bortezomib, melphalan, and prednisone in newly diagnosed multiple myeloma (ALCYONE): a randomised, open-label, phase 3 trial. Lancet. 2020;395(10218):132–41. https://doi.org/10.1016/S0140-6736(19)32956-3.
Terpos E, Kleber M, Engelhardt M, Zweegman S, Gay F, Kastritis E, et al. European myeloma network guidelines for the management of multiple myeloma-related complications. Haematologica. 2015;100(10):1254–66. https://doi.org/10.3324/haematol.2014.117176.
Acknowledgements
We thank the patients who participated in this study, the staff members at the study sites, the data and safety monitoring committee and the staff members involved in data collection and analyses. We thank Polina Kaplan, MD, for her review of an early draft of this manuscript.
Funding
Funding for the ALCYONE (NCT02195479) study was provided by Janssen Research & Development, LLC. The sponsor and authors were jointly responsible for the conception and design, and data analysis. Medical writing support was provided by Linda Wychowski, PhD, and Corey Eagan, MPH, of Eloquent Scientific Solutions, and funded by Janssen Global Services, LLC. All the authors reviewed, revised, and approved the manuscript for submission. The sponsor and authors vouch for data accuracy and completeness.
Author information
Authors and Affiliations
Contributions
JW, SW, AK, KSG, and JF contributed to the conception and design, and data analysis and interpretation; SK, M-VM, MAD, KS, AJ, CD, PL, ZN, GU, LP, MC1, SG, AC, AML, PC, TS, S-SY, GI, TF, MG, JS-M, and MC2 contributed to the collection and assembly of data, and data analysis and interpretation; and all authors drafted and reviewed the manuscript, approved the final version for submission, and vouch for data accuracy and completeness.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki. The study protocol, informed consent forms, and other study-related documents were reviewed and approved by the local independent ethics committees and institutional review boards. Written informed consent was obtained from all patients.
Consent for publication
Not applicable.
Competing interests
Stefan Knop received honoraria from Amgen, Bristol-Myers Squibb, Celgene, Janssen and Takeda; served as a consultant or in an advisory role for Amgen, Bristol-Myers Squibb, Celgene, Janssen and Takeda; and received research funding from Amgen, Bristol-Myers Squibb, Celgene, Janssen and Takeda. Maria-Victoria Mateos has received honoraria from Adaptive Biotechnologies, Amgen, Celgene, Janssen Pharmaceuticals and Takeda; served on the Board of Directors or advisory committees for AbbVie, Amgen, Celgene, GenTech, GlaxoSmithKline, Janssen Pharmaceuticals, Mundipharma, PharmaMar, Roche and Takeda; served on data and monitoring committees for Amgen and Janssen Pharmaceuticals; and served on speakers bureaus for Amgen, Celgene, Janssen Pharmaceuticals and Takeda. Meletios A. Dimopoulos has received consulting fees, honoraria and research funding from Amgen, Celgene, Janssen and Takeda; and participated in advisory boards for Sanofi-Aventis. Kenishi Suzuki received honoraria from Bristol-Myers Squibb, Celgene, Janssen, Novartis, Ono, Takeda and Sanofi-Aventis; served as a consultant or in an advisory role for Bristol-Myers Squibb, Celgene, Janssen, Novartis, Ono, Takeda and Sanofi-Aventis; and is employed by SRL. Andrzej Jakubowiak received honoraria from AbbVie, Adaptive Biotechnologies, Amgen, Bristol-Myers Squibb, Celgene, Janssen, Karyopharm, SkylineDx and Takeda; and served as a consultant or in an advisory role for AbbVie, Adaptive Biotechnologies, Amgen, Bristol-Myers Squibb, Celgene, Janssen, Karyopharm, SkylineDx and Takeda. Chantal Doyen served as a consultant or in an advisory role for Janssen. Paulo Lucio received honoraria from Amgen, Celgene, Janssen and Takeda; and served as a consultant or in an advisory role for Amgen, Celgene, Janssen and Takeda. Mark Cook received honoraria from AbbVie, Amgen, Bristol-Myers Squibb, Celgene, GlaxoSmithKline, Janssen and Takeda; served as a consultant or in an advisory role for AbbVie, Amgen, Bristol-Myers Squibb, Celgene, GlaxoSmithKline, Janssen and Takeda; received research support from Celgene and Janssen; and served on a speakers bureau for Celgene and Janssen. Sebastian Grosicki received research funding from Affimed. Sung-Soo Yoon served as a consultant or in an advisory role for Amgen, Astellas, Celgene, Chugai, Janssen, Novartis and Takeda; received honoraria from Novartis; and received research funding from Kyowa Kirin, Roche-Genentech and Yuhan Pharmaceutical. Mamta Garg has received honoraria from Amgen and Janssen; research funding from Novartis; and travel accommodations and expenses from Amgen, Novartis and Takeda. Jianping Wang, Susan Wroblewski, Anupa Kudva, Katharine S. Gries and John Fastenau are employed by Janssen. Jesus San-Miguel received honoraria from Amgen, Bristol-Myers Squibb, Celgene, Janssen, Novartis, Roche and Sanofi. Michele Cavo has consulted for AbbVie, Amgen, Celgene and Janssen Pharmaceuticals; received honoraria from AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Janssen Pharmaceuticals and Takeda; and served on speakers bureaus for and received travel and/or accommodation expenses from Celgene and Janssen Pharmaceuticals. Zsolt Nagy, Ganna Usenko, Ludek Pour, Andre Crepaldi, Anna Marina Liberati, Philip Campbell, Tatiana Shelekhova, Genadi Iosava and Tomoaki Fujisaki have nothing to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Fig. 1
CONSORT patient flow diagram including completion of PRO questionnaires at baseline (ITT population).
Additional file 2: Supplementary Fig. 2
LS mean change from baseline in EORTC QLQ-C30. a – Role functioning. b – Emotional functioning. c – Cognitive functioning. d – Social functioning. e – Nausea and vomiting up to 36 months (ITT population).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Knop, S., Mateos, MV., Dimopoulos, M.A. et al. Health-related quality of life in patients with newly diagnosed multiple myeloma ineligible for stem cell transplantation: results from the randomized phase III ALCYONE trial. BMC Cancer 21, 659 (2021). https://doi.org/10.1186/s12885-021-08325-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-021-08325-2