Abstract
Background
Research suggests having an oral and pharyngeal cancer (OPC) examination for early diagnosis can increase survival rate. However, the OPC screening rate is low in certain populations. To improve OPC screening rate, this study identified factors that are associated with having an OPC examination.
Methods
Participants with landlines and aged 25 years and older were recruited from six northern Florida counties. Bivariate and logistic regressions were used to predict the outcome of whether the participants had ever had an OPC examination as well as whether participants had ever heard of an OPC examination.
Results
Of 2260 participants with a mean age of 55.9 ± 15.0 years, the majority of participants never smoked (53.4%), self-identified as Whites (70.6%), and had some college or 2-year degree education (30.3%). Smokers were significantly less likely to have ever heard of an OPC examination than those who never smoked. Significant interaction between smoking status and race, and smoking status and social support interaction were found. Whites who never smoked were more likely to have had an OPC examination than non-Whites who never smoked. Former and current smokers with greater social support were more likely to have had an OPC examination than those with lower social support.
Conclusion
The findings from this study inform the need to enhance the awareness of having an OPC examination among smokers and to reduce barriers for racial minority populations to receive an OPC examination. Future research is warranted to develop interventions to target certain populations to improve the rate of OPC examination.
Similar content being viewed by others
Introduction
Oral and pharyngeal cancer (OPC) is a deadly disease and treatments are often disfiguring. According to data from the American Cancer Society, nearly 52,000 people were diagnosed with OPC and approximately 10,000 people died from OPC in 2018 in the United States [1]. On the other hand, OPC is highly preventable and early diagnosis can increase chances of survival [2]. Having an OPC examination early is key to detecting OPC at an earlier stage and preventing mortality [3, 4]. Nonetheless, OPC screening rates are low, especially in certain population subgroups, such as males aged between 45 and 64 years old, African Americans, and people with low socioeconomic status [5, 6]. To increase OPC examination rates and survival, it is important to understand what demographic and psychosocial factors are associated with having an OPC examination.
People who engage in risky behaviors such as excess consumption of alcohol and cigarette smoking and who have the presence of human papillomavirus type 16 (HPV-16) infection have been found to be at a higher risk of getting OPC and have a lower OPC survival rate [7,8,9,10,11,12]. Worldwide, cigarette smoking causes 20 to 30% of oral cancer [13]. Although the overall smoking rate among adults has steadily decreased in the past decades, 14% of adults are smokers in the United States according to 2017 data [14]. Studies have reported an associative relationship between the use of all forms of tobacco products, including direct and indirect use, and OPC [7, 15,16,17,18]. Smokers are at a higher risk of death caused by OPC than non-smokers, regardless of gender [7, 19]. According to data from the Behavioral Risk Factor Surveillance System although smokers are more likely to have oral health problems, their dental visit rates are lower compared to non-smokers, regardless of socioeconomic status and other health-related characteristics [20,21,22,23,24,25]. Dental visit rates are even lower among long-term and heavy smokers [20, 26]. Current smokers aged 40 years or older are at the highest risk of OPC, but are less likely to have an OPC examination than former smokers [5, 13]. The “inverse screening” suggests that people who engage in risky behaviors, such as heavy use of alcohol and tobacco, are less likely to take risk aversion behaviors such as dental attendance and cancer screening [12, 27, 28].
In addition to cigarette smoking, factors such as age, gender, socioeconomic status, race/ethnicity, and health behaviors are associated with OPC examination. People who are older, male, Black, heavy tobacco users, heavy alcohol users, and have low socioeconomic status and poor diet are at a higher risk of developing oral cancer [7, 15, 29, 30]. The results of a survey conducted in 2008 showed that 29.4% of people aged 18 years or older reported ever having an OPC examination in the United States [31]. People aged 18 to 39 years are less likely to have ever had an OPC examination than those aged 40 years or older [31]. Although OPC mortality among Blacks was found to be approximately twice as high as among Whites, the OPC examination rate among Blacks is lower than Whites [2, 32, 33]. Blacks are also at a higher rate of diagnosis with a later stage of OPC than Whites because of delays in OPC screening [34]. However, people who are at a higher risk of OPC are less likely to have regular dental examinations [35]. Barriers to oral cancer screening include lack of routine dental visits, insufficient patient-provider communication due to lack of knowledge, low social attention concerning OPC and risk factors, lack of resources to get an OPC examination, and fear/defensive avoidance [23, 36,37,38,39,40,41,42,43].
Prior research has demonstrated that smokers are at a higher risk of OPC and barriers to having an OPC examination in smokers have been identified. However, there is a lack of studies considering psychosocial factors such as perceived social support, as well as the interactions between demographic and psychosocial factors with smoking status when predicting whether a person has ever had an OPC examination. These interactions may play an important role in decision making related to having OPC screening, but research in this area is critically lacking in Florida. In this study, using a large sample from rural communities in Florida, we aimed to extend prior research by: (1) studying what factors predict the outcome of whether the participants had ever had an OPC examination; and (2) examining what factors predict whether participants had ever heard of an OPC examination. We hypothesized that we would be able to replicate the previous findings that people who had ever heard of an OPC examination were more likely to have had an OPC examination. Next, because evidence suggests that smokers are less likely to have had an OPC screening than non-smokers, we hypothesized that smoking status would be partially responsible for whether the participants had ever heard of OPC screening. In addition, we included psychosocial factors such as social support, comorbid conditions, perceived concerns of getting an OPC screening, and demographics as control variables in our analysis.
Methods
Study design
The participants were recruited using the computer-assisted telephone interviews (CATI) technique from April 2010 to February 2011 in six rural, northern Florida counties: Alachua, Bradford, Columbia, Gadsden, Jefferson, Leon, and Union. To ensure Blacks were adequately represented in our sample, we identified the rural census tracts that had populations greater than 30% Black within these counties and oversampled Blacks. The study was executed by professional interviewers at the University of Florida Bureau of Economic and Business Research Survey Center. Households with landlines were selected and only one participant was chosen from each household. The household was considered ‘uncontactable’ if no one had answered to any of 10 telephone calls. The oldest male within the household was prioritized during selection to maximize the participation of older men and balance representation of gender. A total of 16,000 telephone numbers was dialed, resulting in 2605 people aged 25 years and older who lived in the six rural counties participating in the current study.
Variables of interest
OPC examination
The main outcome variable of interest was whether the participants ever had an OPC examination. We asked the participants “Have you ever HAD a mouth or throat cancer examination?” Participants who responded No were coded as 0 and those who responded Yes were coded as 1.
Ever heard of an OPC examination
The second main outcome variable of interest was whether the participants ever heard of an OPC examination. We asked the participants “Have you ever HEARD of an examination for mouth or throat cancer examination?” Participants responding No were coded as 0 while those responding Yes were coded as 1.
Smoking status
We measured smoking status by asking two questions: “In your entire life, have you smoked at least 100 cigarettes, about 5 packs?” and “Do you now smoke cigarettes every day, some days, or not at all?” We categorized the participants into three groups: current smokers, former smokers, and never smoked (reference group). Participants who had smoked at least 100 cigarettes in their lifetime and reported smoking “everyday” or “some days” at the time of the survey were categorized as current smokers. Those who reported they had smoked at least 100 cigarettes over the course of their lifetime and identified themselves as not smoking at all currently were categorized as former smokers. People who never smoked refer to those who had never smoked at least 100 cigarettes in their lifetime and reported they did not smoke at all at the time of the survey.
Demographic and psychosocial variables
We collected sociodemographic variables, including age (continuous, range = 25–99 years), gender (dichotomous, men or women; women were the reference group), race (dichotomous, white or black; Blacks were the reference group), education (categorical, range = 1–6, higher numbers indicated higher educational attainment), and a financial security score. The financial security score was computed as the weighted average of the following two items: (1) “Which of these statements best describes your present financial status?” and (2) “If you were faced with an unexpected $500 medical bill that was not covered by insurance, how would you best describe your situation?” Possible scores for the first item ranged from 1 (I really cannot make ends meet) to 4 (money is not a problem, I can buy about whatever I want) and the possible scores for the second item ranged from 1 to 3, with higher scores reflecting being more able to comfortably pay the bill. The financial security score ranged from − 1 to 1; a higher score indicated a higher level of financial security. The question, “How concerned are you about getting mouth or throat cancer in the future?” was conducted to assess perceived concern of the participants. The item responses ranged from 1 (definitely not concerned) to 4 (very concerned) but were categorized into three groups (1 = not concerned, 2 = little concern, and 3 and 4 = very concerned). We measured health literacy by asking, “How often do you have a problem understanding the written materials about your medical condition?” and “How often do you have a problem understanding what is told to you about your medical condition?” (1 = rarely or none of the time, 4 = all of the time). Questions on chronic conditions were drawn from the Seattle Index of Comorbidity. We asked the participants, “Has a doctor or nurse has ever told you that you have any of the following problems?: cancer (excluding skin cancer), chronic lung disease or emphysema, asthma or bronchitis, congestive heart failure, diabetes, heart attack, pneumonia, stroke, arthritis, and chronic back pain.” Chronic conditions, ranging from one to ten, indicated the total number of coexisting chronic conditions. We categorized the participants into three groups: no chronic conditions, one chronic condition, and two or more than two chronic conditions. Social support was accessed using five items from a modified version of the medical Outcomes Social Support (MOSS) survey. The participants were asked to report how often, if needed, each of the following kinds of support was available to them: “someone to help with daily chores if you are sick,” “someone to turn to for suggestions about how to deal with a personal problem,” “someone to do something enjoyable with,” “someone to love and make you feel wanted,” and “someone to take you to the doctor if you needed it” (1 = none of the time, 5 = all of the time). We computed the average score of answered questions as the social support score. The score ranged from 0 to 4, a higher score indicated perceived greater social support [24, 44, 45].
Data analysis
Differences in demographic and psychosocial variables by smoking status were tested using survey-sample-weighted t tests (for continuous variables) or chi-squared tests (for categorical variables). We built survey-sample-weighted multiple logistic regression models to assess the association of the two outcome variables (whether the participants had ever had an OPC examination and whether participants had ever heard of an OPC examination and predictor variables including age, education, and financial security, gender, race, ever heard of an oral concern, health literacy, perceived concern, chronic conditions, social support, smoking status, and their interactions with smoking status. We used the survey procedure PROC SURVEYLOGISTIC of SAS version 9.4 (SAS Institute, Cary, NC) for the analysis.
Results
Participants’ characteristics
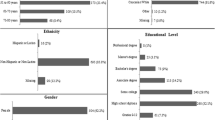
We summarized characteristics of the participants stratified by smoking status in Table 1. The mean age of the 2260 participants in the study was 55.9 ± 15.0 years. The majority of participants never smoked (n = 1206, 53.4%), self-identified as Whites (n = 1595, 70.6%), and had some college or 2-year degree (n = 684, 30.3%). There was a significant difference in the distribution of gender, race, education, age, and financial security score across people who never smoked, were former smokers, and current smokers (p < .0001). In addition, there were significant differences between groups with respect to ever having an OPC examination, ever hearing of an OPC examination, health literacy, concern, chronic conditions, social support, and depression (p < .001).
Predicting OPC examination
We summarized results from the logistic regression analysis predicting whether participants ever had an OPC examination in Table 2. In the analysis, we included age, education, financial security, gender, race, ever heard of an oral concern, health literacy, perceived concern, chronic conditions, social support, smoking status, and the interactions of these variables with smoking status as predictors. The results showed that older people were 1.09 times more likely than younger people to have had an OPC examination (odds ratio [OR] = 1.09; 95% confidence interval [CI] = 1.02–1.17; p = .018). Participants with a higher education level, a higher financial security score, and two or more than two chronic conditions were more likely to have had an OPC examination than those with a lower education level, a lower financial security score, and no chronic conditions (OR = 1.20; 95% CI = 1.11–1.31; p < .0001; OR = 1.68; 95% CI = 1.39–2.01; p < .0001; OR = 1.41; 95% CI = 1.11–1.79; p = .0046). In addition, people who were very concerned about getting OPC in the future and had ever heard of an oral examination were more likely to have had an OPC examination than those who were not concerned about getting OPC in the future and those who had never heard of an OPC examination (OR = 1.31; 95% CI = 1.01–1.70; p = .0456; OR = 3.73; 95% CI = 3.11–4.49; p < .0001). In predicting the outcome of “Ever had OPC examination”, former smokers were more likely to have had an OPC exam compared to never smokers (OR = 1.75; 95% CI = 1.11–2.76) or current smokers (OR = 2.27; 95% CI = 1.23–4.21), but only among Blacks. Smoking status is not predictive of OPC exam among Whites. The analysis revealed a significant smoking status by race interaction and smoking status by social support interaction. Whites who never smoked were 1.5 times more likely to have an OPC examination than non-Whites who never smoked (OR = 1.52; 95% CI = 1.16–2.00; p = .00026). Furthermore, former and current smokers with greater social support were more likely to have had an OPC examination than those with lower social support (OR = 1.22; 95% CI = 1.02–1.45; p = .0277; OR = 0.78; 95% CI = 0.62–0.98; p = 0.0339).
We summarized results from the logistic regression analysis predicting whether participants had ever heard of an OPC examination in Table 2. In the analysis, we included demographic variables, health literacy, perceived concern, chronic conditions, and smoking status as predictors. The results showed that Whites were 1.38 times more likely than non-Whites to have ever heard of an OPC examination (OR = 1.38; 95% CI = 1.13–1.69; p = .0017). Participants with a higher financial security score and a higher health literacy level were more likely to have ever heard of an OPC examination than those with a lower financial security score and a lower health literacy level (OR = 1.44; 95% CI = 1.22–1.70; p < .0001; OR = 1.23; 95% CI = 1.07–1.41; p = .0027). In addition, the analysis indicated that smokers were significantly less likely to have ever heard of an OPC examination than those who never smoked (OR = 0.77; 95% CI = 0.60–1.00; p = .049).
Discussion
Principal findings
This research aimed at exploring whether smoking status predicts the likelihood of ever having heard of an OPC examination as well as the likelihood of ever having had an OPC examination, taking into account interactions between smoking and demographic and psychosocial variables. We found that smokers were less likely to have heard of an OPC examination than non-smokers. In addition, among non-smokers, Whites were more likely to have an OPC examination than non-Whites. Former and current smokers with greater social support were more likely to have an OPC examination than those with lower social support. This is the first study, to our knowledge, that analyzed a large sample from rural communities in Florida to discover the factors associated with knowledge of OPC examinations, as well as factors associated with having ever had an OPC examination among smokers and non-smokers.
Our results showed that people who never smoked were more likely to have ever heard of an OPC examination than smokers. Furthermore, among Blacks, never smokers were less likely to have had an OPC exam than former smokers. One possible explanation of the lower rate of ever having heard of an OPC examination among smokers is that smokers are less likely to have regular dental visits [12, 20,21,22,23,24,25]. Previous studies have identified that dentists play an important role in informing patients and the public about the signs, symptoms, and knowledge about the etiology of OPC, and disseminating knowledge about the need to have an OPC examination [24, 46]. As a result of a lack of dental visits, smokers have been shown to be more likely to have a poorer oral health status than non-smokers, especially among low-income populations [20, 23, 24, 27, 42, 43]. In our survey, participants were asked to report whether they have ever heard of an OPC examination first then were asked to report whether they have ever had an OPC examination with a description of the exam procedure (e.g., dentist checking the inside of your mouth). It is possible that the former smokers may have not heard of an OPC examination but have had received an OPC examination during their dental visits provided by their health providers as former smokers are at a higher risk of OPC than never smokers [47]. As greater screening intention is associated with the recommendation provided by their healthcare providers; without regular dental visits, smokers may not receive any recommendations from their dentists and hence are less likely to have heard of an OPC screening [46]. Further research is warranted to understand the reasons for not having regular dental visits among smokers and interventions to motivate smokers to have regular dental visits should be developed.
The results of this study also showed that racial disparities had an impact on the relationship between smoking status and OPC examination. Whites who never smoked had a higher rate of OPC examination than non-Whites who never smoked. The lack of knowledge regarding the importance of having an OPC examination and lack of concern about getting OPC leads to never having had an OPC examination. Detecting OPC at an early stage may decrease its mortality rate. Research has identified that barriers to screening for OPC among non-Whites include lack of resources, defensive avoidance, as well as lack of knowledge and social attention [46]. Research has been focusing on delivering messages to increase the awareness of OPC through the media [2, 48,49,50]. People who have been exposed to the messages have increased concern about getting OPC, especially Blacks, and were more likely to have received their first OPC examination [2]. It is important to develop such kinds of interventions that target Black smokers and examine the long-term effects of the interventions.
Finally, our results indicated that former and current smokers with greater social support were more likely to have an OPC examination than former and current smokers with lower social support. This finding is consistent with previous studies that demonstrated personal coping resources, including social support, is one of the key factors that influence the likelihood of getting an OPC examination [51,52,53,54]. People with more coping resources are more receptive to potential undesirable health information than those with less coping resources [55].
Limitations
Results from this study should be interpreted within its limitations. This study may have sampling bias because the sample was drawn from people with landlines. However, our target population was older adults, among whom landlines are popular [56]. Another limitation is that this was a survey study and hence was subject to memory and recall bias. Some participants may not be able to recall whether they have received an OPC examination. The prevalence of people who had ever received ana OPC examination may be overestimated as a previous study showed that minorities often over-report having had an examination [57, 58]. Additionally, we only had data on cigarette smoking. Future studies should access the use of other tobacco products, such as chewing tobacco and cigars, which could also increase the risk of dental caries and oral cancer. Lastly, the current study only recruited the participants in rural north Florida and accessing whether the participants have ever received an OPC examination in the dental settings, the lack of more sampling and clinical sites limits the generalization of the findings.
Conclusions
This study provides data on whether people in a large population of rural communities in Florida have ever heard of an OPC examination and have ever had an OPC examination. Our results highlight the importance of advancing interventions targeting smokers to increase the awareness of having an OPC examination. Policies to reduce racial disparities to reduce the barriers to having an OPC examination should be established. In addition, future research is needed to develop interventions to improve social support for former and current smokers to increase the rate of OPC examination. While the findings from this study suggest that whether the respondents had ever heard of an OPC examination may be an important factor in changing the behavior of having an OPC examination, we cannot demonstrate causality. Future research is needed to understand the causal relationship and to develop interventions to improve the rate of OPC examination.
Availability of data and materials
The datasets supporting the conclusions of this article contain protected health information (PHI) such as names and addresses, so they are not available for public use. Please contact the corresponding author for further details.
Abbreviations
- CES-D:
-
Center for Epidemiologic Studies Depression
- CI:
-
Confidence interval
- HPV-16:
-
Human papillomavirus type 16
- MOSS:
-
Medical Outcomes Social Support
- OPC:
-
Oral and pharyngeal cancer
- OR:
-
Odds ratio
References
Cancer Facts & Figures 2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf. Accessed 17 Aug 2020.
Logan HL, Guo Y, Emanuel AS, Shepperd JA, Dodd VJ, Marks JG, et al. Determinants of first-time cancer examinations in a rural community: a mechanism for behavior change. Am J Public Health. 2015;105(7):1424–31. https://doi.org/10.2105/AJPH.2014.302516.
Holmes JD, Dierks EJ, Homer LD, Potter BE. Is detection of oral and oropharyngeal squamous cancer by a dental health care provider associated with a lower stage at diagnosis? J Oral Maxillofac Surg. 2003;61(3):285–91. https://doi.org/10.1053/joms.2003.50056.
Awan K. Oral cancer: early detection is crucial. J Int Oral Health JIOH. 2014;6(5):i–ii. https://pubmed.ncbi.nlm.nih.gov/25395811/.
Dodd VJ, Riley Iii JL, Logan HL. Developing an oropharyngeal cancer (OPC) knowledge and behaviors survey. Am J Health Behav. 2012;36(5):589–601. https://doi.org/10.5993/AJHB.36.5.2.
Logan HL, Guo Y, Marks JG. What a dentist should know about oral and pharyngeal cancer in Florida. Todays FDA. 2015;27(1):56–7 59.
Morse DE, Psoter WJ, Cleveland D, Cohen D, Mohit-Tabatabai M, Kosis DL, et al. Smoking and drinking in relation to oral cancer and oral epithelial dysplasia. Cancer Causes Control. 2007;18(9):919–29. https://doi.org/10.1007/s10552-007-9026-4.
Guo Y, Logan HL, Marks JG, Shenkman EA. The relationships among individual and regional smoking, socioeconomic status, and oral and pharyngeal cancer survival: a mediation analysis. Cancer Med. 2015;4(10):1612–9. https://doi.org/10.1002/cam4.509.
Elrefaey S, Massaro MA, Chiocca S, Chiesa F, Ansarin M. HPV in oropharyngeal cancer: the basics to know in clinical practice. Acta Otorhinolaryngol Ital. 2014;34(5):299–309.
Mork J, Lie AK, Glattre E, Hallmans G, Jellum E, Koskela P, et al. Human papillomavirus infection as a risk factor for squamous-cell carcinoma of the head and neck. N Engl J Med. 2001;344(15):1125–31. https://doi.org/10.1056/NEJM200104123441503.
Sturgis EM, Ang KK. The epidemic of HPV-associated oropharyngeal cancer is here: is it time to change our treatment paradigms? J Natl Compr Cancer Netw. 2011;9(6):665–73. https://doi.org/10.6004/jnccn.2011.0055.
Akinkugbe AA, Garcia DT, Brickhouse TH, Mosavel M. Lifestyle risk factor related disparities in oral cancer examination in the U.S: a population-based cross-sectional study. BMC Public Health. 2020;20(1):153.
Olson CM, Burda BU, Beil T, Whitlock EP. Screening for oral cancer: a targeted evidence update for the U.S. Preventive Services Task Force. Agency for Healthcare Research and Quality (US); 2013. http://www.ncbi.nlm.nih.gov/books/NBK132472/. Accessed 17 Apr 2021.
Jamal A, Phillips E, Gentzke AS, Homa DM, Babb SD, King BA, et al. Current cigarette smoking among adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(2):53–9. https://doi.org/10.15585/mmwr.mm6702a1.
Asthana S, Labani S, Kailash U, Sinha DN, Mehrotra R. Association of Smokeless Tobacco use and Oral Cancer: a systematic global review and meta-analysis. Nicotine Tob Res. 2019;21(9):1162–71. https://doi.org/10.1093/ntr/nty074.
Stanford-Moore G, Bradshaw PT, Weissler MC, Zevallos JP, Brennan P, Anantharaman D, et al. Interaction between known risk factors for head and neck cancer and socioeconomic status: the Carolina head and neck Cancer study. Cancer Causes Control. 2018;29(9):863–73. https://doi.org/10.1007/s10552-018-1062-8.
Gallaway MS, Henley SJ, Steele CB, Momin B, Thomas CC, Jamal A, et al. Surveillance for cancers associated with tobacco use - United States, 2010-2014. MMWR Surveill Summ. 2018;67(12):1–42. https://doi.org/10.15585/mmwr.ss6712a1.
Ward E, Jemal A, Cokkinides V, Singh GK, Cardinez C, Ghafoor A, et al. Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin. 2004;54(2):78–93. https://doi.org/10.3322/canjclin.54.2.78.
Chaturvedi P, Singh A, Chien C-Y, Warnakulasuriya S. Tobacco related oral cancer. BMJ. 2019;365:l2142.
Mucci LA, Brooks DR. Lower use of dental services among long term cigarette smokers. J Epidemiol Community Health. 2001;55(6):389–93. https://doi.org/10.1136/jech.55.6.389.
Wiener RC, Bhandari R, Trickett Shockey AK, Waters C. Dental care utilization among veterans by smoking status. Int J Dent. 2019;2019:8.
Klassen AC, Juon HS, Alberg AJ, Reid BC, Meissner HI. Opportunities for oral cancer screening among older African-American women. Prev Med. 2003;37(5):499–506. https://doi.org/10.1016/S0091-7435(03)00176-2.
Drilea SK, Reid BC, Li CH, Hyman JJ, Manski RJ. Dental visits among smoking and nonsmoking US adults in 2000. Am J Health Behav. 2005;29(5):462–71. https://doi.org/10.5993/AJHB.29.5.9.
Emanuel AS, Parish A, Logan HL, Dodd VJ, Zheng D, Guo Y. Dental visits mediate the impact of smoking on Oral health. Am J Health Behav. 2018;42(1):59–68. https://doi.org/10.5993/AJHB.42.1.6.
Viswanath A, Kerns TJ, Sorkin JD, Dwyer DM, Groves C, Steinberger EK. Self-reported oral cancer screening by smoking status in Maryland: trends over time. J Public Health Dent. 2013;73(4):261–70. https://doi.org/10.1111/jphd.12012.
Langevin SM, Michaud DS, Eliot M, Peters ES, McClean MD, Kelsey KT. Regular dental visits are associated with earlier stage at diagnosis for oral and pharyngeal cancer. Cancer Causes Control. 2012;23(11):1821–9. https://doi.org/10.1007/s10552-012-0061-4.
Alkhubaizi Q, Khalaf ME, Dashti H, Sharma PN. Oral Cancer screening among smokers and nonsmokers. J Int Soc Prev Community Dent. 2018;8(6):553–9. https://doi.org/10.4103/jispcd.JISPCD_197_18.
Csikar J, Kang J, Wyborn C, Dyer TA, Marshman Z, Godson J. The self-reported Oral health status and dental attendance of smokers and non-smokers in England. PLoS One. 2016;11(2):e0148700. https://doi.org/10.1371/journal.pone.0148700.
Conway DI, Petticrew M, Marlborough H, Berthiller J, Hashibe M, Macpherson LM. Socioeconomic inequalities and oral cancer risk: a systematic review and meta-analysis of case-control studies. Int J Cancer. 2008;122(12):2811–9. https://doi.org/10.1002/ijc.23430.
Auluck A, Walker BB, Hislop G, Lear SA, Schuurman N, Rosin M. Population-based incidence trends of oropharyngeal and oral cavity cancers by sex among the poorest and underprivileged populations. BMC Cancer. 2014;14(1):316. https://doi.org/10.1186/1471-2407-14-316.
Moyer VA. Force USPST. Screening for oral cancer: U.S. preventive services task force recommendation statement. Ann Intern Med. 2014;160(1):55–60. https://doi.org/10.7326/M13-2568.
Tomar SL, Loree M, Logan H. Racial differences in oral and pharyngeal cancer treatment and survival in Florida. Cancer Causes Control. 2004;15(6):601–9. https://doi.org/10.1023/B:CACO.0000036166.21056.f9.
Goodwin WJ, Thomas GR, Parker DF, Joseph D, Levis S, Franzmann E, et al. Unequal burden of head and neck cancer in the United States. Head Neck. 2008;30(3):358–71. https://doi.org/10.1002/hed.20710.
Guo Y, McGorray SP, Riggs CE Jr, Logan HL. Racial disparity in oral and pharyngeal cancer in Florida in 1991-2008: mixed trends in stage of diagnosis. Community Dent Oral Epidemiol. 2013;41(2):110–9. https://doi.org/10.1111/j.1600-0528.2012.00738.x.
Netuveli G, Sheiham A, Watt RG. Does the 'inverse screening law' apply to oral cancer screening and regular dental check-ups? J Med Screen. 2006;13(1):47–50. https://doi.org/10.1258/096914106776179836.
Vermeir P, Vandijck D, Degroote S, Peleman R, Verhaeghe R, Mortier E, et al. Communication in healthcare: a narrative review of the literature and practical recommendations. Int J Clin Pract. 2015;69(11):1257–67. https://doi.org/10.1111/ijcp.12686.
Blanch-Hartigan D, Chawla N, Moser RP, Finney Rutten LJ, Hesse BW, Arora NK. Trends in cancer survivors' experience of patient-centered communication: results from the health information National Trends Survey (HINTS). J Cancer Surviv. 2016;10(6):1067–77. https://doi.org/10.1007/s11764-016-0550-7.
Moore PM, Rivera Mercado S, Grez Artigues M, Lawrie TA. Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database Syst Rev. 2013;3:CD003751.
Licqurish SM, Cook OY, Pattuwage LP, Saunders C, Jefford M, Koczwara B, et al. Tools to facilitate communication during physician-patient consultations in cancer care: an overview of systematic reviews. CA Cancer J Clin. 2019;69(6):497–520. https://doi.org/10.3322/caac.21573.
Howell JL, Shepperd JA, Logan H. Barriers to oral cancer screening: a focus group study of rural black American adults. Psychooncology. 2013;22(6):1306–11. https://doi.org/10.1002/pon.3137.
Choi Y, Dodd V, Watson J, Tomar SL, Logan HL, Edwards H. Perspectives of African Americans and dentists concerning dentist-patient communication on oral cancer screening. Patient Educ Couns. 2008;71(1):41–51. https://doi.org/10.1016/j.pec.2007.11.011.
Bloom B, Adams PF, Cohen RA, Simile C. Smoking and oral health in dentate adults aged 18-64. NCHS Data Brief. 2012;85:1–8.
Blasi PR, Krakauer C, Anderson ML, Nelson J, Bush T, Catz SL, et al. Factors associated with future dental care utilization among low-income smokers overdue for dental visits. BMC Oral Health. 2018;18(1):183. https://doi.org/10.1186/s12903-018-0646-8.
Newell SM, Logan HL, Guo Y, Marks JG, Shepperd JA. Evaluating tablet computers as a survey tool in rural communities. J Rural Health. 2015;31(1):108–17. https://doi.org/10.1111/jrh.12095.
Riley JL, Pomery EA, Dodd VJ, Muller KE, Guo Y, Logan HL. Disparities in knowledge of mouth or throat cancer among rural Floridians. J Rural Health. 2013;29(3):294–303. https://doi.org/10.1111/jrh.12003.
Shepperd JA, Howell JL, Logan H. A survey of barriers to screening for oral cancer among rural black Americans. Psychooncology. 2014;23(3):276–82. https://doi.org/10.1002/pon.3415.
Anantharaman D, Muller DC, Lagiou P, Ahrens W, Holcatova I, Merletti F, et al. Combined effects of smoking and HPV16 in oropharyngeal cancer. Int J Epidemiol. 2016;45(3):752–61. https://doi.org/10.1093/ije/dyw069.
Watson J, Tomar S, Dodd V, Logan H, Choi Y. Effectiveness of a social marketing media campaign to reduce Oral Cancer racial disparities. J Natl Med Assoc. 2009;101(8):774–82. https://doi.org/10.1016/S0027-9684(15)31005-1.
Logan HL, Guo Y, Marks J. Disparities in survival patterns for Oral and pharyngeal Cancer in Florida: can we do anything about it? Todays FDA. 2015;27(4):58–9 61.
Logan H, Shepperd J, Pomery E, Guo Y, Muller K, Dodd V, et al. Increasing screening intentions for oral and pharyngeal cancer. AnnBehav Med. 2013;46(1):96–106. https://doi.org/10.1007/s12160-013-9480-z.
Ge S, Lu H, Li Q, Logan HL, Dodd VJ, Bian J, et al. Classification tree analysis of factors associated with Oral Cancer exam. Am J Health Behav. 2019;43(3):635–47. https://doi.org/10.5993/AJHB.43.3.16.
Riley JL 3rd, Dodd VJ, Muller KE, Guo Y, Logan HL. Psychosocial factors associated with mouth and throat cancer examinations in rural Florida. Am J Public Health. 2012;102(2):e7–14. https://doi.org/10.2105/AJPH.2011.300504.
Ford ME, Havstad S, Vernon SW, Davis SD, Kroll D, Lamerato L, et al. Enhancing adherence among older African American men enrolled in a longitudinal cancer screening trial. Gerontologist. 2006;46(4):545–50. https://doi.org/10.1093/geront/46.4.545.
Odedina FT, Campbell ES, LaRose-Pierre M, Scrivens J, Hill A. Personal factors affecting African-American men's prostate cancer screening behavior. J Natl Med Assoc. 2008;100(6):724–33. https://doi.org/10.1016/S0027-9684(15)31350-X.
Sweeny K, Melnyk D, Miller W, Shepperd JA. Information avoidance: who, what, when, and why. Rev Gen Psychol. 2010;14(4):340–53. https://doi.org/10.1037/a0021288.
Wireless Substitution: Early release of estimates from the National Health Interview Survey, 2018. https://www.cdc.gov/nchs/data/nhis/earlyrelease/wireless201906.pdf. Accessed 17 Aug 2020.
Lofters A, Vahabi M, Glazier RH. The validity of self-reported cancer screening history and the role of social disadvantage in Ontario, Canada. BMC Public Health. 2015;15(1):28. https://doi.org/10.1186/s12889-015-1441-y.
McPhee SJ, Nguyen TT, Shema SJ, Nguyen B, Somkin C, Vo P, et al. Validation of recall of breast and cervical cancer screening by women in an ethnically diverse population. Prev Med. 2002;35(5):463–73. https://doi.org/10.1006/pmed.2002.1096.
Acknowledgements
This work was conducted when the first author Tzu-Jung Wong was a PhD student in the Department of Behavioral Science and Community Health at University of Florida. Drs. Guo and Bian were funded in part by the National Institutes of Health (NIH)’s National Cancer Institute (NCI) R01CA246418, R21CA245858, R21CA253394, NIH’s National Institute on Aging (NIA) R21AG068717, and Centers for Disease Control and Prevention (CDC) U18DP006512. The authors wish to thank Ms. Safiyya Mohamed Ali for providing editorial support.
Funding
None.
Author information
Authors and Affiliations
Contributions
Tzu-Jung Wong and Yi Guo were responsible for the conception and design of the study, data analyses, interpretation of the findings, and manuscript writing. Virginia J. Dodd, Wei Wang, and Jiang Bian contributed to the design of the study and assisted in the writing. Qian Li performed the data analysis and assisted with the writing. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The University of Florida institutional review board approved all work for this study. All participants provided informed consent to participate in this study. All relevant ethical safeguards had been met in relation to patient or subject protection. We conducted the study in accordance to the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest in relation to this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wong, TJ., Li, Q., Dodd, V. et al. Oral cancer knowledge and screening behavior among smokers and non-smokers in rural communities. BMC Cancer 21, 430 (2021). https://doi.org/10.1186/s12885-021-08198-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-021-08198-5