Abstract
Background
Immunotherapy represents a promising option for treatment of hepatocellular carcinoma (HCC) in cirrhotic patients but its efficacy is currently inconsistent and unpredictable. Locoregional therapies inducing immunogenic cell death, such as transarterial chemoembolization (TACE) or selective internal radiation therapy (SIRT), have the potential to act synergistically with immunotherapy. For the development of new approaches combining locoregional treatments with immunotherapy, a better understanding of the respective effects of TACE and SIRT on recruitment and activation of immune cells in HCC is needed. To address this question, we compared intra-tumor immune infiltrates in resected HCC after preoperative treatment with TACE or SIRT.
Methods
Data fromr patients undergoing partial hepatectomy for HCC, without preoperative treatment (SURG, n = 32), after preoperative TACE (TACE, n = 16), or preoperative SIRT (n = 12) were analyzed. Clinicopathological factors, tumor-infiltrating lymphocytes (TILs), CD4+ and CD8+ T cells, and granzyme B (GZB) expression in resected HCC, and postoperative overall and progression-free survival were compared between the three groups.
Results
Clinicopathological and surgical characteristics were similar in the three groups. A significant increase in TILs, CD4+ and CD8+ T cells, and GZB expression was observed in resected HCC in SIRT as compared to TACE and SURG groups. No difference in immune infiltrates was observed between TACE and SURG patients. Within the SIRT group, the dose of irradiation affected the type of immune infiltrate. A significantly higher ratio of CD3+ cells was observed in the peri-tumoral area in patients receiving < 100 Gy, whereas a higher ratio of intra-tumoral CD4+ cells was observed in patients receiving > 100 Gy. Postoperative outcomes were similar in all groups. Irrespective of the preoperative treatment, the type and extent of immune infiltrates did not influence postoperative survival.
Conclusions
SIRT significantly promotes recruitment/activation of intra-tumor effector-type immune cells compared to TACE or no preoperative treatment. These results suggest that SIRT is a better candidate than TACE to be combined with immunotherapy for treatment of HCC. Evaluation of the optimal doses for SIRT for producing an immunogenic effect and the type of immunotherapy to be used require further evaluation in prospective studies.
Similar content being viewed by others
Background
Either for curative-intent or for palliative approaches, therapeutic management of hepatocellular carcinoma (HCC) in cirrhotic patients remains limited by the poor efficacy of currently available systemic therapies. In particular, potentially curative treatments, such as partial hepatectomy (PH) and destruction with radiofrequency (RF), are associated with high recurrence rates [1,2,3,4], strongly underlining the rationale for combining tumor-targeted approaches with effective systemic therapy. At the present, however, no neoadjuvant or adjuvant systemic treatment has been proven effective for reducing the risk of relapse when combined with PH or RF [5,6,7]. In this context, the use of immunotherapy appears to be an attractive option. Several studies have indicated that HCCs are immunogenic and immunosensitive tumors and promising results have been obtained with different types of immunotherapy, including adoptive immunotherapy and checkpoint inhibitors [8,9,10,11,12,13,14,15,16,17,18]. However, in individual patients, the overall results of immunotherapy remain inconsistent and outcomes are difficult to predict. To address this problem, it has been hypothesized that the reliability and robustness of response to different immunostimulating approaches could be enhanced by combination with loco-regional intra-arterial treatment, such as transarterial chemoembolization (TACE) or selective internal radiation therapy (SIRT). In fact, it has been shown that in situ cellular destruction, such as that induced by TACE, SIRT, or by thermic destruction with RF, may enhance tumor immunogenicity (so-called immunogenic cell death) by increasing the expression of tumor-associated antigens and the recruitment and diversity of tumor-infiltrating lymphocytes (TILs) [19,20,21,22,23,24,25]. In that sense, TACE and SIRT may potentially act synergistically with immunotherapy, both locally and for inducing a systemic anti-tumor immune response.
At this stage, both transarterial chemoembolization (TACE) and selective internal radiation therapy (SIRT) are potential candidates for use in such combined approaches. In current algorithms, TACE and SIRT are now similarly validated in the multimodal treatment of HCC, mainly as bridge therapy before transplantation or for palliation in patients not amenable to curative therapies [1]. However, the mechanisms of action of these two techniques are different, as TACE consists of intra-tumor deposition of particles loaded with chemotherapy combined with embolization of small tumor arteries, essentially leading to ischemic cell death, while SIRT consists of intra-tumor deposition of particles loaded with 90Yttrium (90Y), via smaller arterial branches, leading to radiation-induced cell death. Accordingly, a better understanding of the respective effects of TACE and SIRT on tumor immunogenicity and the tumor immune microenvironment represents a necessary first step for the design of new therapeutic protocols combining intra-arterial therapy and immunotherapy.
To evaluate this question, we analyzed tumor samples from patients who underwent PH for HCC after preoperative TACE or preoperative SIRT, and in patients who underwent surgery without preoperative treatment as a control. In these three groups, we compared immune infiltrates, such as TIL phenotypes and extent, and the intra-tumor expression of the cytotoxic molecule granzyme B (GZB).
Methods
Patients
We retrospectively analyzed three groups of patients who underwent PH for HCC, including patients who underwent surgery without preoperative treatment (SURG), and patients who underwent surgery after preoperative TACE (TACE) or after preoperative SIRT (SIRT). All patients had been previously declined for liver transplantation by multidisciplinary board decision. Selection criteria for PH included compensated Child-Pugh A cirrhosis, the absence of significant portal hypertension as defined by a portosystemic gradient ≤10 mmHg, the absence of extrahepatic tumors, resectable disease as defined by the surgical team, and the absence of any contraindication for general anesthesia and liver surgery.
Preoperative treatments
The decision to use preoperative treatment or not was determined according to the clinical protocols at the time of the patient’s treatment (period: 2012–2017). Patients treated with preoperative SIRT were included in a prospective trial to evaluate the feasibility and safety of SIRT before surgery for HCC in cirrhotic patients (ClinicalTrials.gov NCT01686880) [26]. Two modalities were used for TACE during the period of this study. In conventional TACE, an emulsion of doxorubicin (1 mg/kg) in lipiodol (iodinated poppy seed oil, Guerbet, France) was injected intra-arterially, followed by gelfoam embolization. For drug-eluting bead TACE, Dc Bead™ 100–300 μm (Biocompatibles UK Ltd) or LifePearl™ 200 μm (Terumo Europe NV, Leuven, Belgium) beads loaded with 75 mg doxorubicin were injected intra-arterially and followed by embolization with an embolic agent (gelfoam particles or Bead Block™, Biocompatibles, UK Ltd).
SIRT was performed as a 2-step procedure. First, a simulation was performed to assess the feasibility and safety of the treatment using the injection of 99mTc-labeled macro-aggregated albumin via supra-selective catheterization of the tumor-feeding segmental or lobar artery in a position determined according to pre-simulation contrast-enhanced angio-CT scan. SIRT was performed when the simulation showed tumor targeting and in the absence of significant pulmonary or gastrointestinal dissemination (pulmonary shunting ≤10%, according to safety requirements outlined by Lemaire et al.) [26]. In the second step, in the absence of contraindication, intra-arterial 90Yttrium (90Y) resin microspheres SIR-Spheres (Sirtex Medical Limited, Sidney, Australia) were injected supra-selectively into the position defined during SIRT simulation.
Surgery
In order to obtain a substantial biological effect of preoperative treatment and for radioprotection when the patients received SIRT, PH was planned at least 12 weeks after TACE or SIRT. PH was performed via laparoscopic or open approach according to technical considerations and surgeon’s choice. All resections were performed under intraoperative ultrasound guidance with the aim of achieving a tumor-free margin. Resections of three or more liver segments were defined as major hepatectomies. Postoperative complications were graded according to Clavien classification [27].
Pathology and evaluation of pathological response
HCCs were graded as well, moderately, or poorly differentiated. To evaluate the response to preoperative treatments, tumor necrosis was analyzed using hematoxylin eosin slides. Minor, moderate, and major pathological responses were defined when tumor necrosis was < 25%, ranging from 25 to 50%, and > 50%, respectively. No response and complete response were defined by the absence of necrosis and the absence of residual cancer cells, respectively.
Immunohistochemistry staining
Consecutive formalin-fixed paraffin-embedded tissue sections (4 μm) were immunohistochemically (IHC)-stained using a BenchMark XT IHC/ISH automated slide stainer (Ventana Mediated Systems) using the Ventana Benchmark technology-based detection system (Roche). Dual CD3/CD20, IHC stains were performed as previously described [28], using primary antibodies against CD3 (Abcam) and CD20 (DAKO). CD4, CD8, and GZB IHC were performed as single stains using monoclonal antibodies against CD4 (BioSB), CD8 (DAKO), and GZB (Abcam).
Image acquisition
Digital images were captured using the NanoZoomer 2.0- RS slide scanner (Hamamatsu, Japan) under 40x magnification.
Digital image analysis
Immunohistochemically stained sections were scanned at a magnification of 20x on a NanoZoomer slide scanner (Hamamatsu). Images were analyzed using VisiomorphDP software (Visiopharm) to quantify the CD3+, CD4+, CD8+ T cells, and GZB signals within the tumor and stromal areas defined by a pathologist for each digital image. The necrotic areas were manually excluded. All images were visually reviewed to remove staining artefacts and damaged tissue area. The total positively stained area(s) was scored as a percentage of the defined region.
Survival and correlation analyses
To investigate the potential effects of the type and extent of TILs and intratumoral expression of GZB, individual CD3+, CD4+, CD8+, and GZB data were correlated with disease-free survival (DFS), as defined by the time from surgery until the first documented progression of disease, and with overall survival (OS).
Lesion dosimetry
In patients treated with SIRT, lesion dosimetry was performed either on pre-therapeutic 99Tc-MAA SPECT/CT images or post-therapeutic 90Y-PET/CT using PMOD® (Technologies Ltd.; Zurich, Switzerland). Lesions were manually delineated on the anatomical images by an experienced physician and co-registered with either pre-therapeutic or post-therapeutic images.
Statistics
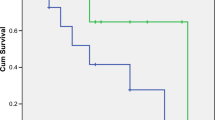
The data were analyzed using the SPSSv25 software. Clinicopathologic parameters were compared between SURG, TACE, and SIRT groups, using the ANOVA test for continuous data and the Chi-Square test for categorical variables. OS and DFS were defined as the time from the date of surgery to the date of death, from any cause, and to the date of the detection of recurrence or death, whichever occurred first, respectively. Survival curves were generated using the Kaplan-Meier method and the comparison between the three groups was performed using the Log-Rank test. The correlations between the extent of TIL and GZB intratumor expression and OS or PFS were evaluated using Cox regression analysis. In all tests, a p < 0.05 defined statistical significance.
Results
Patient and surgical characteristics and post-surgical outcomes
Overall, patient and tumor characteristics were similar in the three groups (Table 1). No differences were observed in demographics and causes/stages of cirrhosis between the SURG (n = 32), TACE (n = 16), and SIRT (n = 12) groups (Table 1). Patients were predominantly male, the median age of the entire population was 67.7 years (range: 27–88 years), and most of the patients had hepatitis C and alcohol-related cirrhosis. All patients were Child-Pugh A. The median tumor number was 1 in the three groups, and median tumor size was similar in the three groups, 40, 49.5, and 47.5 mm in SURG, TACE, and SIRT, respectively. No patients had macrovascular tumor invasion at imaging. Alfa-fetoprotein (AFP) levels varied widely but were not significantly different among the three groups. The median delta AFP level, as measured between dosage at diagnosis and preoperative dosage after TACE or SIRT, was similar in the TACE and SIRT groups (data not shown). The time interval between TACE or SIRT and surgery was similar, 14.4 and 15 weeks, respectively. Surgical approaches were similar in the three groups, consisting of laparoscopic resection in 34, 37, and 33% in SURG, TACE, and SIRT groups, respectively (Table 1). Significantly more patients underwent a major hepatectomy in the TACE group, representing 69%, as compared with 15 and 25% in the SURG and SIRT groups, respectively. One postoperative death was observed in the SURG group, 1 in the TACE group, and 0 in the SIRT group. Operative complication rates were similar in the three groups (Table 1).
Pathological data
The tumor histologic grades were similar in the three groups (Table 2). Significantly increased rates of tumor necrosis were observed in the TACE and SIRT groups as compared with spontaneous necrosis in the SURG group, including 28 and 17% complete responses, respectively (Table 2).
Intra-tumor infiltrating lymphocytes and granzyme B expression
Digital pathology was used to quantify TILs and granzyme B expression on scanned CD3, CD4/CD8, and GZB IHC-stained tissues. The resulting data demonstrated significant modifications of the immune infiltrates in SIRT patients as compared with TACE and SURG (Figs. 1 and 2). A significant increase in CD3+ TILs was observed in SIRT patients as compared with TACE and SURG patients, including a significantly increased ratio of both CD4+ T helper cells and CD8+ cytotoxic cells (Fig. 2). In contrast, preoperative TACE did not significantly modify TIL numbers and subsets as compared with the untreated condition in SURG patients (Fig. 2). Moreover, significant intra-tumoral expression of GZB was observed in SIRT as compared with SURG and TACE patients, while no modification was demonstrated between TACE and SURG groups (Fig. 2). Among SIRT patients, we compared TILs and GZB expression between patients receiving irradiation < 100 Gy (N = 6) and those receiving irradiation > 100 Gy (N = 6). A significantly higher ratio of CD3+ cells was observed in the peri-tumoral area in patients treated with lower doses (p = 0.004), whereas a higher ratio of intra-tumoral CD4+ cells was observed in patients treated with higher doses (p = 0.030) (data not shown). The other T cell populations and GZB expression were not significantly modulated according to different absorbed doses.
Representative images of dual CD4/ CD8 and Granzyme B staining on tumor tissues. Scans were imaged at 10x magnification using NDPview software (Hamamatsu). a TILs in a non-treated HCC patient, showing CD4+ (brown) and CD8+ (red) cells. b TILs in a preoperative SIRT-treated HCC patient, showing increased infiltrates with CD4+ (brown) and CD8+ (red) cells. c TILs expression in a preoperative TACE-treated HCC patient showing similar infiltrates with CD4+ (brown) and CD8+ (red) cells as observed in untreated patients but associated with significant areas of necrosis. d Granzyme B expression in a non-treated HCC patient (brown). e Granzyme B expression in a preoperative SIRT-treated HCC patient. f Granzyme B expression in a preoperative TACE-treated HCC patient
Increased TIL and Granzyme B expression in patients treated preoperatively with SIRT as compared with patients treated preoperatively with TACE and patients receiving no preoperative treatment. Comparison of CD3+, CD4+, CD8+, and Granzyme B in the three groups of patients. Each dot represents one individual. *: p < 0.05, ***: p < 0.01
Correlations between intra-tumoral infiltrates and survival
After a mean follow-up of 47, 42, and 35 months, no differences were observed in OS and DFS in the SURG, TACE, and SIRT groups, respectively. In the SURG, TACE, and SIRT groups, mean OS was 72 months (range: 54–93), 73.9 months (range: 50–98), and 74 months (range: 50–98), and mean DFS was 29 months (15–42), 40.5 months (range: 22–55), and 26.3 months (range: 7–47), respectively. To further analyze the potential effect of TILs and intra-tumoral expression of GZB, the percentages of these infiltrates, independently of preoperative treatment, were analyzed according to a Cox regression model. In these analyses, the percentages of CD3+ TILs (HR: 1.13, p = 0.32), CD4+ TILs (HR: 1.04, p = 0.15), CD8+ TILs (HR: 1.15, p = 0.15), and GZB (HR: 1.02, p = 0.84) were not correlated with DFS.
Discussion
There is a strong need to develop new therapeutic strategies for hepatocellular carcinoma in cirrhotic patients. In fact, in most cases, due to the frequency of occult intrahepatic metastases and to the pre-neoplastic nature of the whole cirrhotic liver, HCC should be considered to be a multicentric tumor. Therefore, besides liver transplantation, tumor-targeted approaches, such as PH and RF, and locoregional treatments, such as TACE, SIRT, or radiotherapy, are associated with high recurrence rates and poor long-term results. The combination of immunotherapy with local treatments may represent a new option for addressing this problem [29,30,31]. Different combinations are possible in this setting, both for the choice of the locoregional treatment and for the type of immunotherapy, and several of these strategies are currently being investigated [32,33,34,35,36,37]. Among locoregional treatments, both TACE and SIRT have the potential to induce local immunogenic cell death and to improve the efficacy of immunotherapy by revealing new tumor antigenic targets, creating acute inflammatory changes in the tumor microenvironment, and promoting the activation/recruitment of immune-active cells. In curative-intent approaches, it is also possible that the combination of preoperative intra-arterial treatments with immunotherapy may improve the long-term results of PH or RF by inducing a vaccinal-type effect and enhancing immune surveillance to prevent the development of micrometastases or of de novo HCC in the remnant cirrhotic liver.
The central objective of our study was to characterize the immunogenic effects of TACE and SIRT. To evaluate this question, we reviewed tumor samples in cirrhotic patients who underwent PH for HCC after preoperative TACE, preoperative SIRT, and without preoperative treatment. Our main finding is that SIRT, but not TACE, significantly enhances intra-tumor immune infiltrates in HCC as compared with the spontaneous infiltrates observed in patients who were untreated before tumor resection. In SIRT patients, we observed a significant increase in CD3+TILs, particularly of CD8+T cell subsets. Similarly, but to a lesser extent, a significant increase in CD4+TILs was observed in these cases but, as the phenotype of these cells was not characterized (including the relative proportions of regulatory FoP3+ and cytotoxic GZB+ among CD4+T cells), the impact of this phenomenon is difficult to interpret. Consistent with this finding, as CD8+T cells represent its major cellular source, a significant increase of GZB was observed in the SIRT group. Overall, these results confirm the recent observation from Chew et al. that showed that radioembolization increases anti-tumor immune responses in HCC [38]. Similarly, these authors showed that SIRT significantly increases CD8+T cell intra-tumoral infiltrates, but also other cellular populations involved in anti-tumor immunity, such as NK cells.
The mechanisms leading to immune activation after SIRT remain hypothetical. In fact, several observations have suggested that some of the clinical effects of radiation therapy could be related to stimulation of the antitumor immune response, including in the rare cases where a response is induced at distant sites after radiotherapy (the so-called abscopal effect) [39,40,41]. More specifically, it has been shown that tumor irradiation may increase the release of tumor antigens and the diversity and activity of TILs [42], suggesting potential synergistic activity with immunotherapy, such as immune checkpoint inhibitors [32].
Interestingly, we also observed that different doses of irradiation delivered during SIRT may differentially affect the type and extent of immune infiltrates and, in particular, that lower doses of irradiation could be more immunogenic. These preliminary observations should be further confirmed but are consistent with results obtained with external beam radiotherapy showing that immune responses are highly dependent on the administered radiation dose and fractioning [43].
In contrast to patients receiving preoperative SIRT, and despite significant amounts of tumor necrosis, no change in immune infiltrates was observed in patients treated with TACE. CD8+ and CD4+ TILs and GZB intra-tumor expression were not different in this group as compared with the spontaneous condition in untreated tumors, indicating that, in these conditions, TACE-related ischemic cell death does not generate significant modification of the inflammatory/immunogenic tumor microenvironment. This discrepancy between cellular necrosis and immune infiltrates in patients treated with TACE or SIRT could be related to several factors. First, the mechanisms leading to cell death are different in these two approaches. TACE uses larger microspheres (embolized at the arteriolar level) and produces ischemia-induced cell death, whereas SIRT uses smaller radioactive microspheres (embolized at the capillary level), and produces radiation-induced immunogenic cell death. Second, the kinetics of these two treatments may be different and it is possible that 15 weeks between intra-arterial treatment and surgery is not long enough for optimal visualization of significant tumor necrosis after SIRT [44, 45].
In the present study, confirming previous observations [26, 46,47,48], neither SIRT nor TACE were able to improve outcomes after PH as compared with patients receiving no preoperative treatment. Moreover, irrespective of the preoperative treatment, we did not observe any impact of the extent of TILs or of the intra-tumoral expression of GZB on recurrence rates and OS. While our study was underpowered to address this question, this may indicate that, under these conditions, locally-attracted immune cells may have not acquired full functionality, remaining unable to generate a robust anti-tumor response in the remnant liver. In fact, in HCC and in other tumors, the existence of non-redundant mechanisms of tumor resistance to radiation has been suggested by several observations, such as the variability of the responses and the extreme rarity of the abscopal effect [49, 50]. Interestingly, therapeutic combinations, such as radiotherapy and immunotherapy or dual checkpoint blockade may, at least partially, overcome these resistance mechanisms [51].
Conclusion
These results should be interpreted cautiously due to the limited number of patients and the retrospective nature of the study. Furthermore, as TILs in SIRT-treated patients have not been functionally investigated, and as no immunotherapy was given in these patients, the real immunogenic effect and potential synergy with checkpoint inhibitors or other immunomodulators remain to be verified. Yet, together with recent observations [38, 46], our results suggest that the combination of SIRT with immunotherapy, such as checkpoint blockade or dual checkpoint blockade, may represent an attractive therapeutic strategy for treatment of HCC, either in a preoperative setting, before PH or RF, or for palliation in patients not amenable to curative-intent treatment. The absence of immunogenic effects of TACE observed here suggests that SIRT should be tested preferentially in investigational protocols combining intra-arterial treatments with immunotherapy. This approach, and its further refinements, including the definition of the optimal dose of irradiation, the type of immunotherapy and the optimal schedule for sequential interventions, requires further evaluation in prospective studies.
Availability of data and materials
The datasets generated and analyzed during the current study are available from the authors on reasonable request.
Abbreviations
- 90Y:
-
90Yttrium
- AFP:
-
Alpha-fetoprotein
- GZB:
-
Granzyme B
- HBV:
-
Hepatitis B virus
- HCC:
-
Hepatocellular carcinoma
- HCV:
-
Hepatitis C virus
- IHC:
-
Immunohistochemistry
- MELD:
-
Model for end-stage liver disease
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- PH:
-
Partial hepatectomy
- RF:
-
Radiofrequency
- SIRT:
-
Selective internal radiation therapy
- TACE:
-
Transarterial chemoembolization
- TIL:
-
Tumor-infiltrating lymphocytes
References
European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol 2018;69:182–236. https://doi.org/10.1016/j.jhep.2018.03.019.
Bruix J, Sherman M, And the American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–2. https://doi.org/10.1002/hep.24199.
Gao J, Xie L, Yang WS, Zhang W, Gao S, Wang J, Xiang YB. Risk factors of hepatocellular carcinoma--current status and perspectives. Asian Pac J Cancer Prev. 2012;13:743–52.
Mazzaferro V, Lencioni R, Majno P. Early hepatocellular carcinoma on the procrustean bed of ablation, resection, and transplantation. Semin Liver Dis. 2014;34:415–26. https://doi.org/10.1055/s-0034-1394365.
Schwartz JD, Schwartz M, Mandeli J, Sung M. Neoadjuvant and adjuvant therapy for resectable hepatocellular carcinoma: review of the randomised clinical trials. Lancet Oncol. 2002;3:593–603.
Samuel M, Chow PK, Chan Shih-Yen E, Machin D, Soo KC. Neoadjuvant and adjuvant therapy for surgical resection of hepatocellular carcinoma. Cochrane Database Syst Rev. 2009;21:CD001199. https://doi.org/10.1002/14651858.CD001199.pub2.
Bruix J, Takayama T, Mazzaferro V, Chau GY, Yang J, Kudo M, Cai J, Poon RT, Han KH, Tak WY, Lee HC, Song T, Roayaie S, Bolondi L, Lee KS, Makuuchi M, Souza F, Berre MA, Meinhardt G, Llovet JM; STORM investigators. Adjuvant sorafenib for hepatocellular carcinoma after resection or ablation (STORM): a phase 3, randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2015;16:1344–54. https://doi.org/10.1016/S1470-2045(15)00198-9.
Breous E, Thimme R. Potential for immunotherapy for hepatocellular carcinoma. J Hepatol. 2011;54:830–4. https://doi.org/10.1016/j.jhep.2010.10.013.
Prieto J, Melero I, Sangro B. Immunological landscape and immunotherapy of hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol. 2015;12:681–700. https://doi.org/10.1038/nrgastro.2015.
Greten TF, Sangro B. Targets for immunotherapy of liver cancer. J Hepatol. 2017;68:157–66. https://doi.org/10.1016/j.jhep.2017.09.007.
Yao W, He JC, Yang Y, Wang JM, Qian YW, Yang T, Ji L. The prognostic value of tumor-infiltrating lymphocytes in hepatocellular carcinoma: a systematic review and meta-analysis. Sci Rep. 2017;7:7525. https://doi.org/10.1038/s41598-017-08128-1.
Lué A, Serrano MT, Bustamante FJ, Iñarrairaegui M, Arenas JI, Testillano M, Lorente S, Gil C, de la Torre M, Gomez A, Sangro B. Neutrophil-to-lymphocyte ratio predicts survival in European patients with hepatocellular carcinoma administered sorafenib. Oncotarget. 2017;8:103077–86. https://doi.org/10.18632/oncotarget.21528.
Yoong KF, McNab G, Hübscher SG, Adams DH. Vascular adhesion protein-1 and ICAM-1 support the adhesion of tumor-infiltrating lymphocytes to tumor endothelium in human hepatocellular carcinoma. J Immunol. 1998;160:3978–88.
Unitt E, Marshall A, Gelson W, Rushbrook SM, Davies S, Vowler SL, Morris LS, Coleman N, Alexander GJ. Tumour lymphocytic infiltrate and recurrence of hepatocellular carcinoma following liver transplantation. J Hepatol. 2006;45:246–53.
Wada Y, Nakashima O, Kutami R, Yamamoto O, Kojiro M. Clinicopathological study on hepatocellular carcinoma with lymphocytic infiltration. Hepatology. 1998;27:407–14.
Sangro B, Gomez-Martin C, de la Mata M, Iñarrairaegui M, Garralda E, Barrera P, Riezu-Boj JI, Larrea E, Alfaro C, Sarobe P, Lasarte JJ, Pérez-Gracia JL, Melero I, Prieto J. A clinical trial of CTLA-4 blockade with tremelimumab in patients with hepatocellular carcinoma and chronic hepatitis C. J Hepatol. 2013;59:81–8. https://doi.org/10.1016/j.jhep.2013.02.022.
Duffy AG, Ulahannan SV, Makorova-Rusher O, Rahma O, Wedemeyer H, Pratt D, Davis JL, Hughes MS, Heller T, ElGindi M, Uppala A, Korangy F, Kleiner DE, Figg WD, Venzon D, Steinberg SM, Venkatesan AM, Krishnasamy V, Abi-Jaoudeh N, Levy E, Wood BJ, Greten TF. Tremelimumab in combination with ablation in patients with advanced hepatocellular carcinoma. J Hepatol. 2017;66:545–51. https://doi.org/10.1016/j.jhep.2016.10.029.
El-Khoueiry AB, Sangro B, Yau T, Crocenzi TS, Kudo M, Hsu C, Kim TY, Choo SP, Trojan J, Welling TH Rd, Meyer T, Kang YK, Yeo W, Chopra A, Anderson J, Dela Cruz C, Lang L, Neely J, Tang H, Dastani HB, Melero I. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet. 2017;389:2492–502. https://doi.org/10.1016/S0140-6736(17)31046-2.
Kroemer G, Galluzzi L, Kepp O, Zitvogel L. Immunogenic cell death in cancer therapy. Annu Rev Immunol. 2013;31:51–72. https://doi.org/10.1146/annurev-immunol-032712-100008.
Mizukoshi E, Nakamoto Y, Arai K, Yamashita T, Sakai A, Sakai Y, Kagaya T, Yamashita T, Honda M, Kaneko S. Comparative analysis of various tumor-associated antigen-specific t-cell responses in patients with hepatocellular carcinoma. Hepatology. 2011;53:1206–16. https://doi.org/10.1002/hep.24149.
Zerbini A, Pilli M, Laccabue D, Pelosi G, Molinari A, Negri E, Cerioni S, Fagnoni F, Soliani P, Ferrari C, Missale G. Radiofrequency thermal ablation for hepatocellular carcinoma stimulates autologous NK-cell response. Gastroenterology. 2010;138:1931–42. https://doi.org/10.1053/j.gastro.2009.12.051.
Ayaru L, Pereira SP, Alisa A, Pathan AA, Williams R, Davidson B, Burroughs AK, Meyer T, Behboudi S. Unmasking of alpha-fetoprotein-specific CD4(+) T cell responses in hepatocellular carcinoma patients undergoing embolization. J Immunol. 2007;178:1914–22.
Hansler J, Wissniowski TT, Schuppan D, Witte A, Bernatik T, Hahn EG, Strobel D. Activation and dramatically increased cytolytic activity of tumor specific T lymphocytes after radio-frequency ablation in patients with hepatocellular carcinoma and colorectal liver metastases. World J Gastroenterol. 2006;12:3716–21.
Golden EB, Apetoh L. Radiotherapy and immunogenic cell death. Semin Radiat Oncol. 2015;25:11–7. https://doi.org/10.1016/j.semradonc.2014.07.005.
Ali MY, Grimm CF, Ritter M, Mohr L, Allgaier HP, Weth R, Bocher WO, Endrulat K, Blum HE, Geissler M. Activation of dendritic cells by local ablation of hepatocellular carcinoma. J Hepatol. 2005;43:817–22.
Lemaire M, Lucidi V, Bouazza F, Katsanos G, Vanderlinden B, Levillain H, Delatte P, Garcia CA, Vouche M, Galdon MG, Demetter P, Deleporte A, Hendlisz A, Flamen P, Donckier V. Selective internal radiation therapy (SIRT) before partial hepatectomy or radiofrequency destruction for treatment of hepatocellular carcinoma in cirrhotic patients: a feasibility and safety pilot study. HPB. 2018;20:641–8. https://doi.org/10.1016/j.hpb.2018.01.006.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Buisseret L, Garaud S, de Wind A, Van den Eynden G, Boisson A, Solinas C, Gu-Trantien C, Naveaux C, Lodewyckx JN, Duvillier H, Craciun L, Veys I, Larsimont D, Piccart-Gebhart M, Stagg J, Sotiriou C, Willard-Gallo K. Tumor-infiltrating lymphocyte composition, organization and PD-1/ PD-L1 expression are linked in breast cancer. Oncoimmunology. 2017;6:e1257452. https://doi.org/10.1080/2162402X.2016.1257452.
Takayama T, Sekine T, Makuuchi M, Yamasaki S, Kosuge T, Yamamoto J, Shimada K, Sakamoto M, Hirohashi S, Ohashi Y, Kakizoe T. Adoptive immunotherapy to lower postsurgical recurrence rates of hepatocellular carcinoma: a randomised trial. Lancet. 2000;356:802–7.
Lee JH, Lee JH, Lim YS, Yeon JE, Song TJ, Yu SJ, Gwak GY, Kim KM, Kim YJ, Lee JW, Yoon JH. Adjuvant immunotherapy with autologous cytokine-induced killer cells for hepatocellular carcinoma. Gastroenterology. 2015;148:1383–91.e6. https://doi.org/10.1053/j.gastro.2015.02.055.
Cui J, Wang N, Zhao H, Jin H, Wang G, Niu C, Terunuma H, He H, Li W. Combination of radiofrequency ablation and sequential cellular immunotherapy improves progression-free survival for patients with hepatocellular carcinoma. Int J Cancer. 2014;134:342–51. https://doi.org/10.1002/ijc.28372.
A Study of the Safety and Antitumoral Efficacy of Nivolumab After SIRT for the Treatment of Patients With HCC (NASIR-HCC). ClinicalTrials.gov Identifier: NCT03380130.
A Global Study to Evaluate Transarterial Chemoembolization (TACE) in Combination With Durvalumab and Bevacizumab Therapy in Patients With Locoregional Hepatocellular Carcinoma (EMERALD-1). ClinicalTrials.gov Identifier: NCT03778957.
Combine TACE and Autologous Tcm Immunotherapy Versus TACE Alone for HCC With MVI After Radical Resection. ClinicalTrials.gov Identifier: NCT03575806.
Sequential TransArterial Chemoembolization and Stereotactic RadioTherapy With Immuno Therapy for Downstaging Hepatocellular Carcinoma for Hepatectomy (START-FIT). ClinicalTrials.gov Identifier: NCT03817736.
Stereotactic Body Radiotherapy (SBRT) Followed by Immunotherapy in Liver Cancer. ClinicalTrials.gov Identifier: NCT03203304.
Tremelimumab With Chemoembolization or Ablation for Liver Cancer. ClinicalTrials.gov Identifier: NCT01853618.
Chew V, Lee YH, Pan L, Nasir NJM, Lim CJ, Chua C, Lai L, Hazirah SN, Lim TKH, Goh BKP, Chung A, Lo RHG, Ng D, Filarca RLF, Albani S, Chow PKH. Immune activation underlies a sustained clinical response to Yttrium-90 radioembolisation in hepatocellular carcinoma. Gut. 2019;68:335–46. https://doi.org/10.1136/gutjnl-2017-315485.
Grass GD, Krishna N, Kim S. The immune mechanisms of abscopal effect in radiation therapy. Curr Probl Cancer. 2016;40:10–24. https://doi.org/10.1016/j.currproblcancer.2015.10.003.
Barcellos-Hoff MH, Park C, Wright EG. Radiation and the microenvironment - tumorigenesis and therapy. Nat Rev Cancer. 2005;5:867–75.
Chino F, Pollis KE, Choi S, Salama JK, Palta M. Stereotactic Body Radiation Therapy-Induced Abscopal Effect on Hepatocellular Carcinoma After Treatment for Lung Cancer: A Case Report. Hepatology. 2018;68:1653–5.
Twyman-Saint Victor C, Rech AJ, Maity A, Rengan R, Pauken KE, Stelekati E, Benci JL, Xu B, Dada H, Odorizzi PM, Herati RS, Mansfield KD, Patsch D, Amaravadi RK, Schuchter LM, Ishwaran H, Mick R, Pryma DA, Xu X, Feldman MD, Gangadhar TC, Hahn SM, Wherry EJ, Vonderheide RH, Minn AJ. Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer. Nature. 2015;520:373–7. https://doi.org/10.1038/nature14292.
Burnette B, Weichselbaum RR. The immunology of ablative radiation. Semin Radiat Oncol. 2015;1:40–5. https://doi.org/10.1016/j.semradonc.2014.07.009.
Vouche M, Habib A, Ward TJ, Kim E, Kulik L, Ganger D, Mulcahy M, Baker T, Abecassis M, Sato KT, Caicedo JC, Fryer J, Hickey R, Hohlastos E, Lewandowski RJ, Salem R. Unresectable solitary hepatocellular carcinoma not amenable to radiofrequency ablation: multicenter radiology-pathology correlation and survival of radiation segmentectomy. Hepatology. 2014;60:192–201. https://doi.org/10.1002/hep.27057.
Salem R, Mazzaferro V, Sangro B. Yttrium 90 radioembolization for the treatment of hepatocellular carcinoma: biological lessons, current challenges, and clinical perspectives. Hepatology. 2013;58:2188–97. https://doi.org/10.1002/hep.26382.
Zhou WP, Lai EC, Li AJ, Fu SY, Zhou JP, Pan ZY, Lau WY, Wu MC. A prospective, randomized, controlled trial of preoperative transarterial chemoembolization for resectable large hepatocellular carcinoma. Ann Surg. 2009;249:195–202. https://doi.org/10.1097/SLA.0b013e3181961c16.
Yoo H, Kim JH, Ko GY, Kim KW, Gwon DI, Lee SG, Hwang S. Sequential transcatheter arterial chemoembolization and portal vein embolization versus portal vein embolization only before major hepatectomy for patients with hepatocellular carcinoma. Ann Surg Oncol. 2011;18:1251–7. https://doi.org/10.1245/s10434-010-1423-3.
Si T, Chen Y, Ma D, Gong X, Yang K, Guan R, Peng C. Preoperative transarterial chemoembolization for resectable hepatocellular carcinoma in Asia area: a meta-analysis of random controlled trials. Scand J Gastroenterol. 2016;51:1512–9.
Barry A, Knox JJ, Wei AC, Dawson LA. Can stereotactic body radiotherapy effectively treat hepatocellular carcinoma? J Clin Oncol. 2016;34:404–8. https://doi.org/10.1200/JCO.2015.64.8097.
Ohba K, Omagari K, Nakamura T, Ikuno N, Saeki S, Matsuo I, Kinoshita H, Masuda J, Hazama H, Sakamoto I, Kohno S. Abscopal regression of hepatocellular carcinoma after radiotherapy for bone metastasis. Gut. 1998;43:575–7.
Wehrenberg-Klee E, Goyal L, Dugan M, Zhu AX, Ganguli S. Y-90 radioembolization combined with a PD-1 inhibitor for advanced hepatocellular carcinoma. Cardiovasc Intervent Radiol. 2018;41:1799–802. https://doi.org/10.1007/s00270-018-1993-1.
Acknowledgements
The authors acknowledge the contribution of a medical writer, Sandy Field, PhD, to preparation of this manuscript.
Funding
This work was supported by “Les Amis de Bordet”.
Author information
Authors and Affiliations
Contributions
LC designed the study, performed the experiments and wrote the manuscript, RDW and PD performed the experiments, VL, AB, SM, FB, MV, IT and GV treated the patients and collected the data, SG, CN, MGG and KWG performed the experiments, AH designed the study, IDD, PF and DL performed the experiments and wrote the manuscript, VD designed the study and wrote the manuscript. All authors have read and accepted the manuscript in its present from.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received Institutional Review Board, (Institut Jules Bordet, Université Libre de Bruxelles, Brussels, Belgium) approval. Patients undergoing preoperative SIRT were included after written informed consent had been obtained (NCT011686880).
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Craciun, L., de Wind, R., Demetter, P. et al. Retrospective analysis of the immunogenic effects of intra-arterial locoregional therapies in hepatocellular carcinoma: a rationale for combining selective internal radiation therapy (SIRT) and immunotherapy. BMC Cancer 20, 135 (2020). https://doi.org/10.1186/s12885-020-6613-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-020-6613-1