Abstract
Background
The future of combined immunotherapy (a PD-1/PD-L1 plus a CTLA-4 antagonist) is very bright. However, besides improving efficacy, combined therapy increases treatment-related adverse events (TRAEs). Also, the clinical application is limited in some solid tumors.
Methods
This paper purports to investigate the TRAEs for the combined immunotherapy aiming for a more appropriate utilization of immune checkpoint inhibitors (ICIs) in clinical practice through a meta-analysis.
Results
A total of 17 eligible studies covering 2626 patients were selected for a meta-analysis based on specified inclusion and exclusion criteria. The incidence rates of any grade and grade 3 or higher TRAEs were 88% (95%CI, 84–92%) and 41% (95%CI, 35–47%), respectively. The overall incidence of any grade TRAEs leading to discontinuation of treatment was 20% (95%CI, 16–24%). The incidence rate of treatment related deaths was 4.3‰ (95%CI, 1.4‰-8.4‰). Analysis showed that NIVO1 + IPI3 cohort had higher incidences of grade 3 or higher TRAEs (RR = 1.77, 95%CI, 1.34–2.34, p < 0.0001) and any grade TRAEs leading to discontinuation of treatment (RR = 1.81, 95%CI, 1.08–3.04, P = 0.02), compared with NIVO3 + IPI1 regimen.
Conclusions
The combined therapy had high TRAEs. The TRAEs, especially grade 3 or higher, led to discontinuation of the treatment. Furthermore, the incidence of treatment-related deaths was rare. Moreover, the NIVO3 + IPI1 regimen, regardless of efficacy, is more recommended because of better tolerance and lower adverse events.
Similar content being viewed by others
Background
Immunotherapies that involve immune checkpoint inhibitors (ICIs) comprise cytotoxic T lymphocyte-associated protein-4 (CTLA-4), programmed cell death protein-1 and ligand-1 (PD-1 and PD-L1) monoclonal antibodies. The first ICI, ipilimumab, received the US Food and Drug Administration (FDA) approval in 2011 [1]. It was then approved for treatment of advanced melanoma. Since 2014, PD-1/PD-L1 inhibitors, especially nivolumab, became an established treatment option for a number of tumors, including melanoma [2], non-small cell lung cancer (NSCLC) [3], renal cell carcinoma (RCC) [4] and Hodgkin’s lymphoma [5]. Furthermore, the combined use of one CTLA-4 plus one PD-1/PD-L1 antagonist was rather more efficacious than the respective monotherapies in some solid tumors [6, 7].
Combination or sole use of ICI potentiates some form of toxicity profiles which were never observed previously [8, 9]. They are known as immune-related adverse events (irAEs) which include thyroid dysfunction, colitis, pneumonitis, dermatitis as well as hepatitis amongst others [8, 9]. The aetiology of these toxicities are autoimmune and are peculiarly different from toxicities observed with conventional cytotoxic chemotherapy. ICIs usually causes side effects associated with autoimmune diseases by altering immune-surveillance [9, 10]. There are a few meta-analyses on the incidences of irAEs to date, and most include articles observed monotherapy or one ICI combined with chemotherapy [11, 12]. In brief, although the combined immunotherapy (anti-PD-1/PD-L1 plus anti-CTLA-4) improves the efficacy, there is a prominent increase of side effects. Consequently, the clinical use of combined ICIs is challenged.
Although most of the combined immunotherapy has achieved encouraging results in an increasing number of published reports for various tumors [13, 14], no one has ever conducted a meta-analysis of the treatment-related adverse events (TRAEs) for anti-PD-1/PD-L1 plus anti-CTLA-4. As a matter of fact, the combined immunotherapy involves different treatment regimens. We conducted a systematic review and meta-analysis of trials of anti-PD-1/PD-L1 plus anti-CTLA-4 in patients with tumor and compared the incidence of TRAEs among the groups treated with different combination regimens. We believe this meta-analysis will help enhance awareness of the incidence and characteristics of TRAEs, which may lead to a more appropriate utilization of ICIs in clinical practice for combination therapy.
Methods
Search methods
The following databases were systematically searched for literatures about clinical trials of combined ICIs (anti-PD-1/PD-L1 and anti-CTLA-4): PubMed, EBSCO, Web of Science and Cochrane Library. The databases were searched for articles published on or before September 2018. The search terms used were: (“nivolumab”OR “BMS 936558” OR “BMS 936559” OR “MDX 1105” OR “pembrolizumab” OR “lambrolizumab” OR “MK 3475” OR “pidilizumab” OR “CT 011” OR “durvalumab” OR “MEDI 4736” OR “atezolizumab” OR “MPDL 3280a” OR “avelumab” OR “AMP 224”) AND (“ipilimumab” OR “tremelimumab”). Additionally, the reference lists of the selected articles were individually reviewed to obtain other potentially relevant articles. Original articles published with prospective clinical trials of the combined ICIs for patients with advanced solid tumors were selected, including adverse events. Selected publications were all in English language.
Study selection
For inclusion in this meta-analysis: (1) investigated the safety and efficacy of the combined ICIs for treatment of solid tumors; (2) clearly reported the adverse events in their safety data, with or without clinical severity grading. The exclusion criteria are listed as follows:(1) the combined ICIs regimens included other therapies, such as chemotherapy and targeted therapy; (2) two immune checkpoint blockade were not used concurrently; (3) the original articles were presented only as meeting abstracts without published full-text; (4) the trials also covered non-solid tumors, such as lymphoma. In the event of duplicates, ambiguity, or publications reporting on the same study population, only the most recent, relevant, and/or comprehensive publication was included in the analysis.
Data extraction
Data from each included study was extracted by two investigators and reviewed independently by a third investigator following the Preferred Reporting Items for Systematic Review and Meta-Analysis guidelines [15]. Any discrepancy in study selection was resolved by consensus. The number of patients treated with combined ICIs, the number of patients with any grade TRAEs, the number of patients with grade 3 or higher TRAEs, the number of patients with TRAEs leading to treatment discontinuation, the number of patients with grade 3 or higher TRAEs leading to treatment discontinuation, the number of patients with any grade treatment-related serious adverse events, the number of patients with each TRAEs, and the number of treatment-related deaths were extracted. The trial phases, tumor types, types of specific agents, dose, and frequency of drug administration were recorded. The incidence of TRAEs was characterized based on all grades and grade 3 or higher as reported by each trial using the definitions of National Cancer Institute’s Common Terminology Criteria for Adverse Events (CTCAE).
Statistical analysis
For each clinical trial, the number of patients treated and the number of patients with adverse events reported were recorded for each treatment arm and dose level. All models were fit using log/logit/arcsine/Freeman-Tukey Double arcsine transformation, respectively, and restricted maximum likelihood estimation using an offset of 0.5 for all 0 cells. According to the normal test results, select the appropriate transformation. Heterogeneity was evaluated using the Cochran Q statistic and I2 statistics for its proportion of the total variability. If p ≥ 0.1 and I2 ≤ 50%, there is homogeneity between the results of the study, and the fixed-effect model will be used for meta-analysis; if p < 0.1 and I2 < 50%, heterogeneity exists among the results within an acceptable range, and the fixed-effect model is still required; if p < 0.1 and I2 ≥ 50%, it indicates that there is substantial heterogeneity among the data, and that we should analyze the source of the heterogeneity in an alternative way. Only when there is no apparent clinical heterogeneity, can the random-effect model be used for meta-analysis cautiously. Publication bias was evaluated by Egger’s test, p < 0.1 was considered statistically significant. Egger’s test of publication bias was not performed on analysis subgroup with less than 10 studies because of low sensitivity of qualitative and quantitative tests. All analyses were performed in Revman 5.3 Software and R 3.4.3 (meta and metafor package).
Results
Eligible studies and characteristics
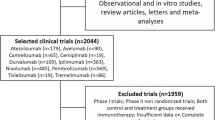
The search strategy originally generated 4342 relevant clinical trials from the databases. After screening and eligibility assessment, a total of 17 eligible studies [7, 13, 14, 16,17,18,19,20,21,22,23,24,25,26,27,28,29] were selected for this meta-analysis, including 2626 patients. The detailed search and study selection process is shown in Additional file 1: Figure S1. Tumor types tested in these studies included melanoma (n = 6), NSCLC (n = 3), RCC (n = 2), small cell lung cancer (n = 1), colorectal cancer (n = 1), glioblastoma (n = 1), esophagogastric cancer (n = 1), mesothelioma (n = 1) and sarcoma (n = 1) (Additional file 3: Table S1). Almost patients had an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1 in 14 studies, except for six patients. Patients had a Karnofsky performance status (KPS) score of at least 70% (in two studies) or at least 80% (in one study).
Therapeutic regimens of combination therapy
The regimens were categorized by class as: nivolumab plus ipilimumab cohort (n = 14) and other combination cohort (n = 3). The latter including pembrolizumab plus ipilimumab (n = 1) and durvalumab plus tremelimumab (n = 2). According to dose, and frequency of drug administration, the nivolumab plus ipilimumab cohort was further divided into three subgroups: NIVO1 + IPI3 cohort, NIVO3 + IPI1 cohort and other NIVO+IPI cohort. The regimens of NIVO1 + IPI3 cohort (n = 8) was nivolumab 1 mg/kg plus ipilimumab 3 mg/kg, every 3 weeks for 4 doses (induction phase), followed by nivolumab 3 mg/kg, every 2 weeks until disease progression or unacceptable toxicity incidence of TRAEs (maintenance phase). The regimens of NIVO3 + IPI1 cohort (n = 7) was nivolumab 3 mg/kg plus ipilimumab 1 mg/kg, every 3 weeks for 4 doses (induction phase), followed by nivolumab 3 mg/kg, every 2 weeks until disease progression or unacceptable toxicity incidence of TRAEs (maintenance phase). The regimens of other NIVO+IPI cohort (n = 4) were variable, as shown in Additional file 3: Table S1.
Incidence of TRAEs
16 articles reported any grade TRAEs, of which the incidence ranged from 72 to 100%, and the incidence rate was 88% (95%CI, 84–92%). The incidence was 95 and 76% in melanoma and NSCLC patients, respectively. The incidence was 92 and 86% in NIVO1 + IPI3 cohort and NIVO3 + IPI1 cohort, respectively. 17 articles reported grade 3 or higher TRAEs, the incidence ranged from 14 to 90%, and the overall incidence rate was 41% (95%CI, 35–47%). The incidence was 55 and 33% in melanoma and NSCLC patients, respectively. The incidence was 54 and 29% in NIVO1 + IPI3 cohort and NIVO3 + IPI1 cohort, respectively (Fig. 1 and Table 1).
Incidence of TRAEs leading to discontinuation of treatment and serious adverse events
Any grade TRAEs leading to discontinuation of treatment was reported by 17 articles, the incidence ranged from 7 to 39%, and the overall incidence was 20% (95%CI, 16–24%). The incidence was 30 and 18% in melanoma and NSCLC patients, respectively. The incidence was 27 and 14% in NIVO1 + IPI3 cohort and NIVO3 + IPI1 cohort, respectively. 10 articles reported grade 3 or higher TRAEs leading to discontinuation of treatment, the incidence ranged from 5 to 30%, and the overall incidence rate was 16% (95%CI, 12–23%). The incidence was 28 and 12% in melanoma and NSCLC patients, respectively. Besides, 10 of the articles reported any grade treatment-related serious adverse events, the incidence of which ranged from 23 to 70%, and the overall incidence rate was 32% (95%CI, 27–39%) (Fig. 2 and Table 1).
Incidence of treatment-related deaths
All included articles reported treatment-related deaths, and the incidence rate was 4.3‰ (95%CI, 1.4‰-8.4‰). A total of 29 deaths were related to study drugs. The most common causes were pulmonary events (n = 9) and cardiac events (n = 7). Pneumonitis was the most frequent cause of death in respiratory adverse drug reaction. Cardiac events included myocarditis, ventricular arrhythmia and cardiac tamponade. Other cause of deaths included hepatic necrosis, renal failure and myasthenia gravis. In addition, there were also some rare causes including hemo-phagocytic syndrome and tumor lysis syndrome (Additional file 2: Figure S2).
Incidence of common TRAEs
The most common any grade TRAEs were fatigue (38%), diarrhea (29%), pruritus (26%), rash (22%), and nausea (20%). The most common grade 3 or higher TRAEs were increased lipase (9%), colitis (6%), increased ALT (6%), increased AST (5%), and diarrhea (5%) (Table 1).
NIVO1 + IPI3 vs. NIVO3 + IPI1 regimens
4 studies investigated and compared the activity and safety of nivolumab combined with ipilimumab (NIVO1 + IPI3 vs. NIVO3 + IPI1). Analysis showed that NIVO1 + IPI3 cohort had more grade 3 or higher TRAEs (RR = 1.77, 95%CI, 1.34–2.34, p < 0.0001). Meanwhile, the any grade TRAEs leading to discontinuation of treatment was more likely to occur in patients with NIVO1 + IPI3 regimen too (RR = 1.81, 95%CI, 1.08–3.04, p = 0.02). Although not statistically significant, a slightly higher likelihood of any grade TRAEs was noted in patients with NIVO1 + IPI3 compared with NIVO3 + IPI1 cohort (RR = 1.07, 95%CI, 0.97–1.17, p = 0.18) (Fig. 3).
Discussion
To the best of our knowledge, this is the first meta-analysis to investigate the adverse drug events for combined ICIs (anti-PD-1/PD-L1 plus anti-CTLA-4). To date, most clinical trials of combination immunotherapy have chosen a treatment regimen of nivolumab combined with ipilimumab, namely NIVO1 + IPI3 or NIVO3 + IPI1 regimen [30]. One-third of the patients recruited for the clinical trial were with advanced melanoma in this article.
This study demonstrated the incidence of TRAEs among patients who had received combination therapy. Most patients had at least one any grade TRAEs during treatment course. Additionally, about half of the patients had higher grade TRAEs. Most importantly, a considerable number of patients discontinued the treatment because of TRAEs. In a word, patients with serious adverse events were not in the minority and TRAEs needed a more serious consideration.
With a frequency of up to 38%, fatigue was the most common adverse event. In contrast to the frequent occurrence, their severity was normally low (2% Grade 3 or higher). The findings were consistent with report by Sznol et al. [31]. Similarly, nearly one-third of cases had diarrhea, but most were not in poor condition except for those with colitis. Other common adverse events, such as pruritus, rash, nausea and so on, were relatively mild.
Increased lipase, with an overall incidence of approximately one-tenth, was the most common grade 3 or higher TRAEs. D’Angelo et al. reported that the most common treatment-related grade 3 or 4 adverse events were lipase elevation and diarrhea in combination therapy [32]. Su et al. summarized relevant clinical trials and found that combination treatment can significantly increase the risk of grade 3 or higher lipase elevation as well as any grade amylase elevation, compared with nivolumab or ipilimumab alone. However, neither monotherapy nor combination therapy are seen to potentiate the risk of immune-induced pancreatitis. The precise and specific mechanism for such observed differences are still unknown [33]. Consistent with previous results of Wang et al., about 6% patients had grade 3 or higher colitis [34]. Sznol et al. comprehensively analyzed a randomized clinical trial published recently and their results showed a higher rate of TRAEs leading to discontinuation of combination therapy than those with monotherapy of nivolumab or ipilimumab. The most common cause of discontinuation was colitis and diarrhea in all studies [31]. They were observed to be the primary immune-related gastrointestinal events and would have the same adverse drug reaction. Schadendorf et al. came to the conclusion that colitis was the most frequently reported TRAEs, which led to discontinuation rate of 10% [35]. Hepatotoxicity was also one of the important irAEs in immunotherapy. The current research showed that elevation of ALT and AST were only second to lipase elevation and colitis in grade 3 or higher TRAEs. Wang et al. reported that CTLA-4 inhibitors are linked to a higher risk of hepatotoxicity compared to PD-1 inhibitors [36].
In this study, the most common treatment-related deaths were caused by pneumonitis and cardiac causes. Baxi et al [37] found that the pneumonitis was the most common serious irAEs in monotherapy (PD-1/PD-L1 antagonist). However, our study shows that pneumonia was not the most common serious TRAEs but the most important cause of treatment-related deaths. Therefore, clinicians should pay great attention to pneumonia, especially of grade 3 or higher in immunotherapy. On the other hand, previous research had suggested that cardiac effects of ICIs were highly variable, but myocarditis was the most reported form of ICI-associated cardiotoxicity, as this cardiotoxicity is generally reversible with corticosteroids [38].
Generally, combination therapy had high incidence of TRAEs, including any grade TRAEs, grade 3 or higher TRAEs, and any grade treatment-related serious adverse events. In addition, any grade TRAEs, mainly about grade 3 or higher TRAEs, leading to discontinuation occurred in one in five patients. Thus, TRAEs, grade 3 or higher TRAEs in particular, became one of the major problems that could not be ignored in combination therapy. Meanwhile, it was also one of the most important factors limiting clinical application and reducing effects. However, the incidence of treatment-related deaths was low (< 1%), because the majority of events was reversible after the systemic use of glucocorticoids, then, well and safely managed. As described by Hassel et al., “in case of long-lasting and/or refractory immune-toxicities, organ- or case-specific escalation of immunosuppression was recommended” [30].
Notably, through subgroup analysis, it found that although any grade TRAEs of NIVO1 + IPI3 treatment regimen were similar to these of NIVO3 + IPI1, the former was associated with a higher incidence of grade 3 or higher TRAEs compared with the latter. Analogously, the analysis reinforced the fact that patients treated with NIVO1 + IPI3 had a higher risk of interruption due to any grade TRAEs than those treated with NIVO3 + IPI1. This is the first meta-analysis to report that NIVO3 + IPI1 regimen has a better tolerance than NIVO1 + IPI3 for clinical trials of combined ICIs (anti-PD-1/PD-L1 plus anti-CTLA-4).
Interestingly, Fujii et al. [39, 40] investigated the relationship between irAEs and response to the treatment. The results showed that irAEs had been associated with improved treatment outcomes, suggestive of an active immune status. So, the side effects of treatment needed to be reevaluated. Furthermore, the complexity of tumor microenvironment and also the intertwined tumor and immune cells interaction, it is however very hard to develop strong biomarkers that could help identify patients who may respond to immunotherapy [41].
Limitations
The limitations of this study should be stressed on. The heterogeneity among included studies cannot be ignored. Despite subgroup analysis, the heterogeneity persists. One of the important reasons is that the patient characteristics are quite different, such as race, geographic region, ECOG, tumor type, PD-L1 expression level and so on. Medication dose might be another important reason. More importantly, the combined immunotherapy regimens are mainly nivolumab plus ipilimumab, and therefore conclusions of this study cannot be applied to other ICIs.
Conclusions
This meta-analysis first evaluated TRAEs incidence of the combined therapy (anti-PD-1/PD-L1 plus anti-CTLA-4), and the regimen has a high incidence of TRAEs. Also, the TRAEs, especially grade 3 or higher, lead to treatment discontinuation. Pulmonary and cardiac toxicity were the leading causes of treatment-related death, but the incidence of treatment-related deaths was low. Last but not least, regardless of efficacy, the NIVO3 + IPI1 regimen is recommended as a combination treatment due to better tolerance and lower adverse events.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article.
Abbreviations
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- CI:
-
Confidence interval
- CTCAE:
-
Common Terminology Criteria for Adverse Events
- CTLA-4:
-
Cytotoxic T lymphocyte-associated protein-4
- ECOG:
-
Eastern Cooperative Oncology Group
- FDA:
-
Food and Drug Administration
- ICIs:
-
Immune checkpoint inhibitors
- irAEs:
-
Immune-related adverse events
- KPS:
-
Karnofsky performance status
- NSCLC:
-
Non-small cell lung cancer
- PD-1 and PD-L1:
-
Programmed cell death protein-1 and ligand-1
- RCC:
-
Renal cell carcinoma
- RR:
-
Relative risk
- TRAEs:
-
Treatment-related adverse events
References
Margolin K, Ernstoff MS, Hamid O, Lawrence D, McDermott D, Puzanov I, Wolchok JD, Clark JI, Sznol M, Logan TF, et al. Ipilimumab in patients with melanoma and brain metastases: an open-label, phase 2 trial. Lancet Oncol. 2012;13(5):459–65.
Weber JS, D'Angelo SP, Minor D, Hodi FS, Gutzmer R, Neyns B, Hoeller C, Khushalani NI, Miller WH Jr, Lao CD, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2015;16(4):375–84.
Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, Chow LQ, Vokes EE, Felip E, Holgado E, et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung Cancer. N Engl J Med. 2015;373(17):1627–39.
Motzer RJ, Escudier B, McDermott DF, George S, Hammers HJ, Srinivas S, Tykodi SS, Sosman JA, Procopio G, Plimack ER, et al. Nivolumab versus Everolimus in advanced renal-cell carcinoma. N Engl J Med. 2015;373(19):1803–13.
Ansell SM, Lesokhin AM, Borrello I, Halwani A, Scott EC, Gutierrez M, Schuster SJ, Millenson MM, Cattry D, Freeman GJ, et al. PD-1 blockade with nivolumab in relapsed or refractory Hodgkin's lymphoma. N Engl J Med. 2015;372(4):311–9.
Larkin J, Chiarion-Sileni V, Gonzalez R, Grob JJ, Cowey CL, Lao CD, Schadendorf D, Dummer R, Smylie M, Rutkowski P, et al. Combined Nivolumab and Ipilimumab or monotherapy in untreated melanoma. N Engl J Med. 2015;373(1):23–34.
Antonia SJ, Lopez-Martin JA, Bendell J, Ott PA, Taylor M, Eder JP, Jager D, Pietanza MC, Le DT, de Braud F, et al. Nivolumab alone and nivolumab plus ipilimumab in recurrent small-cell lung cancer (CheckMate 032): a multicentre, open-label, phase 1/2 trial. Lancet Oncol. 2016;17(7):883–95.
Santini FC, Rizvi H, Plodkowski AJ. Safety and Efficacy of Re-treating with Immunotherapy after Immune-Related Adverse Events in Patients with NSCLC. Cancer Immunol Res. 2018;6(9):1093–9.
Leonardi GC, Gainor JF, Altan M, Kravets S, Dahlberg SE, Gedmintas L, Azimi R, Rizvi H, Riess JW, Hellmann MD, et al. Safety of programmed Death-1 pathway inhibitors among patients with non-small-cell lung Cancer and preexisting autoimmune disorders. J Clin Oncol : official journal of the American Society of Clinical Oncology. 2018;36(19):1905–12.
Kahler KC, Eigentler TK, Gesierich A, Heinzerling L, Loquai C, Meier F, Meiss F, Pfohler C, Schlaak M, Terheyden P, et al. Ipilimumab in metastatic melanoma patients with pre-existing autoimmune disorders. Cancer Immunol Immunother : CII. 2018;67(5):825–34.
Bertrand A, Kostine M, Barnetche T, Truchetet ME, Schaeverbeke T. Immune related adverse events associated with anti-CTLA-4 antibodies: systematic review and meta-analysis. BMC Med. 2015;13:211.
Wu Y, Shi H, Jiang M, Qiu M, Jia K, Cao T, Shang Y, Shi L, Jiang K, Wu H. The clinical value of combination of immune checkpoint inhibitors in cancer patients: a meta-analysis of efficacy and safety. Int J Cancer. 2017;141(12):2562–70.
Hellmann MD, Rizvi NA, Goldman JW, Gettinger SN, Borghaei H, Brahmer JR, Ready NE, Gerber DE, Chow LQ, Juergens RA, et al. Nivolumab plus ipilimumab as first-line treatment for advanced non-small-cell lung cancer (CheckMate 012): results of an open-label, phase 1, multicohort study. Lancet Oncol. 2017;18(1):31–41.
Hodi FS, Chesney J, Pavlick AC, Robert C, Grossmann KF, McDermott DF, Linette GP, Meyer N, Giguere JK, Agarwala SS, et al. Combined nivolumab and ipilimumab versus ipilimumab alone in patients with advanced melanoma: 2-year overall survival outcomes in a multicentre, randomised, controlled, phase 2 trial. Lancet Oncol. 2016;17(11):1558–68.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9 w264.
Long GV, Atkinson V, Lo S, Sandhu S, Guminski AD, Brown MP, Wilmott JS, Edwards J, Gonzalez M, Scolyer RA, et al. Combination nivolumab and ipilimumab or nivolumab alone in melanoma brain metastases: a multicentre randomised phase 2 study. Lancet Oncol. 2018;19(5):672–81.
Tawbi HA, Forsyth PA, Algazi A, Hamid O, Hodi FS, Moschos SJ, Khushalani NI, Lewis K, Lao CD, Postow MA. Combined Nivolumab and Ipilimumab in Melanoma Metastatic to the Brain. N Eng J Med. 2018;379(8):722–30.
Wolchok JD, Chiarion-Sileni V, Gonzalez R, Rutkowski P, Grob JJ, Cowey CL, Lao CD, Wagstaff J, Schadendorf D, Ferrucci PF, et al. Overall survival with combined Nivolumab and Ipilimumab in advanced melanoma. N Engl J Med. 2017;377(14):1345–56.
Omuro A, Vlahovic G, Lim M, Sahebjam S, Baehring J, Cloughesy T, Voloschin A, Ramkissoon SH, Ligon KL, Latek R, et al. Nivolumab with or without ipilimumab in patients with recurrent glioblastoma: results from exploratory phase I cohorts of CheckMate 143. Neuro-oncology. 2018;20(5):674–86.
Janjigian YY, Bendell J, Calvo E, Kim JW, Ascierto PA, Sharma P, Ott PA, Peltola K, Jaeger D, Evans J, et al. CheckMate-032 Study: Efficacy and Safety of Nivolumab and Nivolumab Plus Ipilimumab in Patients With Metastatic Esophagogastric Cancer. J Clin Oncol : official journal of the American Society of Clinical Oncology. 2018;36(28):2836–44.
Hammers HJ, Plimack ER, Infante JR, Rini BI, McDermott DF, Lewis LD, Voss MH, Sharma P, Pal SK, Razak ARA, et al. Safety and efficacy of Nivolumab in combination with Ipilimumab in metastatic renal cell carcinoma: the CheckMate 016 study. J Clin Oncol : official journal of the American Society of Clinical Oncology. 2017;35(34):3851–8.
Overman MJ, Lonardi S, Wong KYM, Lenz HJ, Gelsomino F, Aglietta M, Morse MA, Van Cutsem E, McDermott R, Hill A, et al. Durable clinical benefit with Nivolumab plus Ipilimumab in DNA mismatch repair-deficient/microsatellite instability-high metastatic colorectal Cancer. J Clin Oncol : official journal of the American Society of Clinical Oncology. 2018;36(8):773–9.
D'Angelo SP, Mahoney MR, Van Tine BA, Atkins J, Milhem MM, Jahagirdar BN, Antonescu CR, Horvath E, Tap WD, Schwartz GK, et al. Nivolumab with or without ipilimumab treatment for metastatic sarcoma (Alliance A091401): two open-label, non-comparative, randomised, phase 2 trials. Lancet Oncol. 2018;19(3):416–26.
Motzer RJ, Tannir NM, McDermott DF, Aren Frontera O, Melichar B, Choueiri TK, Plimack ER, Barthelemy P, Porta C, George S, et al. Nivolumab plus Ipilimumab versus Sunitinib in advanced renal-cell carcinoma. N Engl J Med. 2018;378(14):1277–90.
Hellmann MD, Ciuleanu TE, Pluzanski A, Lee JS, Otterson GA, Audigier-Valette C, Minenza E, Linardou H, Burgers S, Salman P, et al. Nivolumab plus Ipilimumab in lung Cancer with a high tumor mutational burden. N Engl J Med. 2018;378(22):2093–104.
Callahan MK, Kluger H, Postow MA, Segal NH, Lesokhin A, Atkins MB, Kirkwood JM, Krishnan S, Bhore R, Horak C, et al. Nivolumab plus Ipilimumab in patients with advanced melanoma: updated survival, response, and safety data in a phase I dose-escalation study. J Clin Oncol : official journal of the American Society of Clinical Oncology. 2018;36(4):391–8.
Long GV, Atkinson V, Cebon JS, Jameson MB, Fitzharris BM, McNeil CM, Hill AG, Ribas A, Atkins MB, Thompson JA, et al. Standard-dose pembrolizumab in combination with reduced-dose ipilimumab for patients with advanced melanoma (KEYNOTE-029): an open-label, phase 1b trial. Lancet Oncol. 2017;18(9):1202–10.
Calabro L, Morra A, Giannarelli D, Amato G, D'Incecco A, Covre A, Lewis A, Rebelatto MC, Danielli R, Altomonte M, et al. Tremelimumab combined with durvalumab in patients with mesothelioma (NIBIT-MESO-1): an open-label, non-randomised, phase 2 study. Lancet Respir Med. 2018;6(6):451–60.
Antonia S, Goldberg SB, Balmanoukian A, Chaft JE, Sanborn RE, Gupta A, Narwal R, Steele K, Gu Y, Karakunnel JJ, et al. Safety and antitumour activity of durvalumab plus tremelimumab in non-small cell lung cancer: a multicentre, phase 1b study. Lancet Oncol. 2016;17(3):299–308.
Boutros C, Tarhini A, Routier E, Lambotte O, Ladurie FL, Carbonnel F, Izzeddine H, Marabelle A, Champiat S, Berdelou A, et al. Safety profiles of anti-CTLA-4 and anti-PD-1 antibodies alone and in combination. Nat Rev Clin Oncol. 2016;13(8):473–86.
Sznol M, Ferrucci PF, Hogg D, Atkins MB, Wolter P, Guidoboni M, Lebbe C, Kirkwood JM, Schachter J, Daniels GA, et al. Pooled analysis safety profile of Nivolumab and Ipilimumab combination therapy in patients with advanced melanoma. J Clin Oncol : official journal of the American Society of Clinical Oncology. 2017;35(34):3815–22.
D'Angelo SP, Larkin J, Sosman JA, Lebbe C, Brady B, Neyns B, Schmidt H, Hassel JC, Hodi FS, Lorigan P, et al. Efficacy and safety of Nivolumab alone or in combination with Ipilimumab in patients with mucosal melanoma: a pooled analysis. J Clin Oncol : official journal of the American Society of Clinical Oncology. 2017;35(2):226–35.
Su Q, Zhang XC, Zhang CG, Hou YL. Risk of Immune-Related Pancreatitis in Patients with Solid Tumors Treated with Immune Checkpoint Inhibitors: Systematic Assessment with Meta-Analysis. J Immunol Res. 2018;2018:1027323.
Wang DY, Ye F, Zhao S, Johnson DB. Incidence of immune checkpoint inhibitor-related colitis in solid tumor patients: a systematic review and meta-analysis. Oncoimmunology. 2017;6(10):e1344805.
Schadendorf D, Wolchok JD, Hodi FS, Chiarion-Sileni V, Gonzalez R, Rutkowski P, Grob JJ, Cowey CL, Lao CD, Chesney J, et al. Efficacy and safety outcomes in patients with advanced melanoma who discontinued treatment with Nivolumab and Ipilimumab because of adverse events: a pooled analysis of randomized phase II and III trials. J Clin Oncol : official journal of the American Society of Clinical Oncology. 2017;35(34):3807–14.
Wang W, Lie P, Guo M, He J. Risk of hepatotoxicity in cancer patients treated with immune checkpoint inhibitors: a systematic review and meta-analysis of published data. Int J Cancer. 2017;141(5):1018–28.
Baxi S, Yang A, Gennarelli RL, Khan N, Wang Z, Boyce L, Korenstein D. Immune-related adverse events for anti-PD-1 and anti-PD-L1 drugs: systematic review and meta-analysis. BMJ (Clinical research ed). 2018;360:k793.
Sury K, Perazella MA, Shirali AC. Cardiorenal complications of immune checkpoint inhibitors. Nat Rev Nephrol. 2018;14(9):571–88.
Fujii T, Naing A, Rolfo C, Hajjar J. Biomarkers of response to immune checkpoint blockade in cancer treatment. Crit Rev Oncol Hematol. 2018;130:108–20.
Fujii T, Colen RR, Bilen MA, Hess KR, Hajjar J, Suarez-Almazor ME, Alshawa A, Hong DS, Tsimberidou A, Janku F, et al. Incidence of immune-related adverse events and its association with treatment outcomes: the MD Anderson Cancer Center experience. Investig New Drugs. 2018;36(4):638–46.
Naing A. Being realistic and optimistic in curing cancer. J Immunother Precis Oncol. 2018;1(2):53–5.
Acknowledgements
Not applicable.
Funding
The authors have no financial support to declare.
Author information
Authors and Affiliations
Contributions
Each author contributed significantly to concept and development of the present paper. LG and MC designed this study. XL, HZ, XZ, and JP collected the data. LK and XW analyzed the data. PAK and MC drafted the manuscript. HS and LC interpreted and revised the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Figure S1. Flow diagram of study inclusion and exclusion. (DOCX 78 kb)
Additional file 2:
Figure S2. Forest plot of the incidence of treatment-related to deaths for combined immunotherapy (anti-PD-1/PD-L1 and anti-CTLA-4). (TIF 1446 kb)
Additional file 3:
Table S1. Characteristics of included trials in the meta-analysis. (DOCX 19 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Gu, L., Khadaroo, P.A., Su, H. et al. The safety and tolerability of combined immune checkpoint inhibitors (anti-PD-1/PD-L1 plus anti-CTLA-4): a systematic review and meta-analysis. BMC Cancer 19, 559 (2019). https://doi.org/10.1186/s12885-019-5785-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-019-5785-z